Abstract
Background
Numerous studies in rats and a few other mammalian species, including man, have shown that the sinusoidal cells constitute an important part of liver function. In the pig, however, which is frequently used in studies on liver transplantation and liver failure models, our knowledge about the function of hepatic sinusoidal cells is scarce. We have explored the scavenger function of pig liver sinusoidal endothelial cells (LSEC), a cell type that in other mammals performs vital elimination of an array of waste macromolecules from the circulation.
Results
125I-macromolecules known to be cleared in the rat via the scavenger and mannose receptors were rapidly removed from the pig circulation, 50% of the injected dose being removed within the first 2–5 min following injection. Fluorescently labeled microbeads (2 μm in diameter) used to probe phagocytosis accumulated in Kupffer cells only, whereas fluorescently labeled soluble macromolecular ligands for the mannose and scavenger receptors were sequestered only by LSEC. Desmin-positive stellate cells accumulated no probes. Isolation of liver cells using collagenase perfusion through the portal vein, followed by various centrifugation protocols to separate the different liver cell populations yielded 280 × 107 (range 50–890 × 107) sinusoidal cells per liver (weight of liver 237.1 g (sd 43.6)). Use of specific anti-Kupffer cell- and anti-desmin antibodies, combined with endocytosis of fluorescently labeled macromolecular soluble ligands indicated that the LSEC fraction contained 62 × 107 (sd 12 × 107) purified LSEC. Cultured LSEC avidly endocytosed ligands for the mannose and scavenger receptors.
Conclusions
We show here for the first time that pig LSEC, similar to what has been found earlier in rat LSEC, represent an effective scavenger system for removal of macromolecular waste products from the circulation.
Background
Pig liver is frequently used to study liver transplantation and failure, and also serves as a source of cells for bioartificial livers [1]. On this background it is surprising that the knowledge about a central liver function, namely blood clearance, in the pig, has been insufficiently dealt with in the literature. The concept of the reticuloendothelial system (RES) was launched by Aschoff in 1924 [2]. A fact that is often forgotten nowadays is that Aschoff included both Kupffer cells (KC) and sinusoidal endothelial cells (LSEC) as equally important members of hepatic RES. However, with time, the liver RES came to be synonymous with the liver macrophage. In fact, all major text books of pathology used today describe the RES as consisting only of macrophages. Nevertheless, very recent studies on the biology of LSEC have shown that these cells in rodents, and the few other mammals that have been studied, represent the most important site of elimination of nearly all tested soluble waste macromolecules, spanning from the unphysiological colloidal vital stains used by Aschoff and his predecessors to a number of physiological macromolecular waste products such as major matrix components [3], serum components [4], lysosomal enzymes [5], and pathophysiological substances such as oxidized low density lipoprotein (LDL) [6] and advanced glycation end products [7]. Studies carried out to compare the scavenger function of KC and LSEC have shown that these two cell types contribute to the hepatic RES function in different yet complementary ways: KC eliminate large, insoluble waste fragments by phagocytosis, whereas LSEC are geared to non-phagocytic endocytosis of soluble macromolecules [3]. In line with this notion is the curious fact that most of the colloidal vital stain that Aschoff and his predecessors used to demonstrate the existence of a RES, was recently shown to be taken up exclusively by LSEC [8].
Thus, blood clearance of soluble waste macromolecules, a major liver function, resides largely in LSEC. It should be noted that these findings have been obtained using rats and some other rodents. Furthermore, it has been shown that most vertebrates carry their so-called scavenger endothelial cells (endothelial cells endowed with the same RES-function as rat LSEC) in organs other than liver [9]. These findings justify a careful study to determine whether the liver of pig is equipped with the same type of scavenger LSEC that is present in rat liver.
With the motivation to determine if pig liver contains LSEC that resemble rat LSEC, we set out to study the scavenger function of pig LSEC. Although some laboratories have reported on isolation of pig liver sinusoidal cells, those methods either yield very low purity or a very low cell number [10,11]. For this reason, we established a protocol consisting of collagenase perfusion, differential and density centrifugation, and centrifugal elutriation. This method yields both high purity and functionally intact pig liver sinusoidal cells that can be cultivated in monolayer cultures. Notably, the yield of sinusoidal cells was four orders of magnitude higher with the presently described method compared to a recently reported protocol [10]. With this method we show, for the first time, that pig LSEC are as endocytically active as their rat liver counterparts.
Results
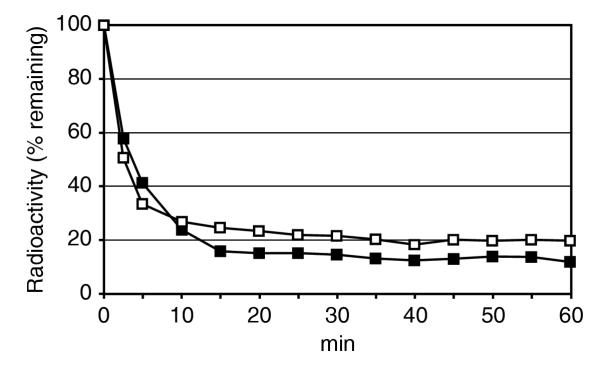
Rate of elimination and organ distribution of circulating formaldehyde-treated serum albumin (FSA) and α-mannosidase
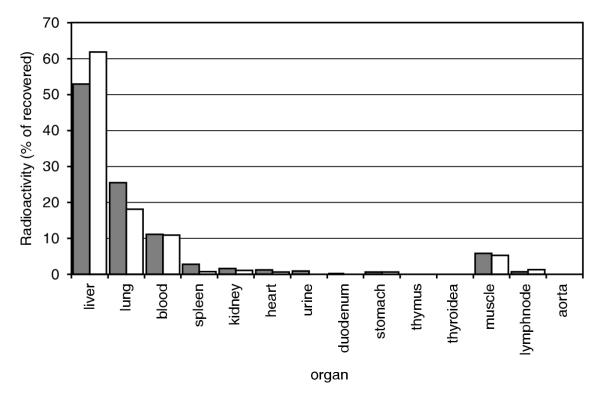
The circulatory survival of FSA and α-mannosidase was determined after intravenous administration of trace amounts of 125I-tyramine cellobiose-FSA (125I-TC-FSA) and 125I-α-mannosidase. Decay plots indicated efficient clearance of either probe, with 50% of injected dose being eliminated from the blood during 2–5 min (Fig. 1). The liver was the main site of uptake (Fig. 2), while a surprising finding was uptake in the lungs. Blood radioactivity after 15–20 min was 15–20% of injected dose. This equals the amount of unbound 125I after gel filtration through a PD-10 column of a sample of the intravenously administered ligands.
Figure 1.
Clearance kinetics. Approximately 100 × 106 cpm of 125I-tyramine cellobiose-formaldehyde-treated serum albumin (TC-FSA) and 125I-α-mannosidase were injected intravenously. Radioactivity in the blood sample collected immediately after injection was taken as 100%. Blood samples were collected every minute during the first 10 minutes, then every 5 minutes for one hour. (Open boxes: 125I-TC-FSA; n = 2, closed boxes: 125I-α-mannosidase; n = 1).
Figure 2.
Anatomical distribution. The animals used in the blood clearance studies (Fig. 1) were analyzed for anatomical distribution of radioactivity 1 h after injection. More than 90% of the injected doses were recovered in the organs listed. Results are expressed as percent total radioactivity recovered. (Grey bars: 125I-TC-FSA; n = 2, white bars: 125I-α-mannosidase; n = 1).
In vivo liver cell identification
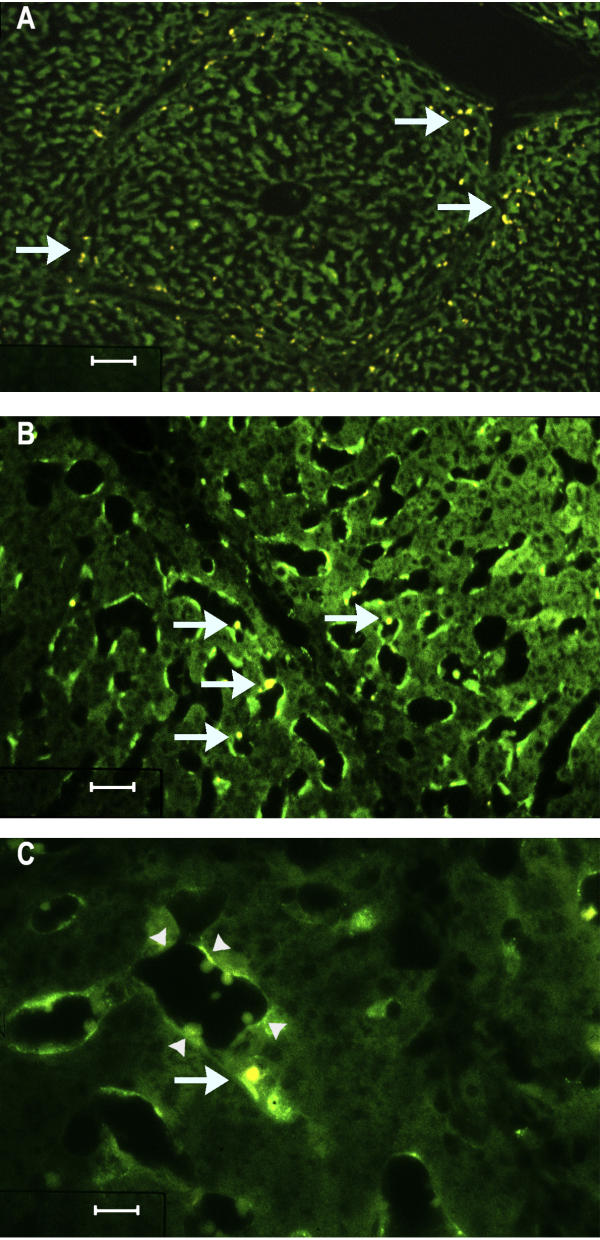
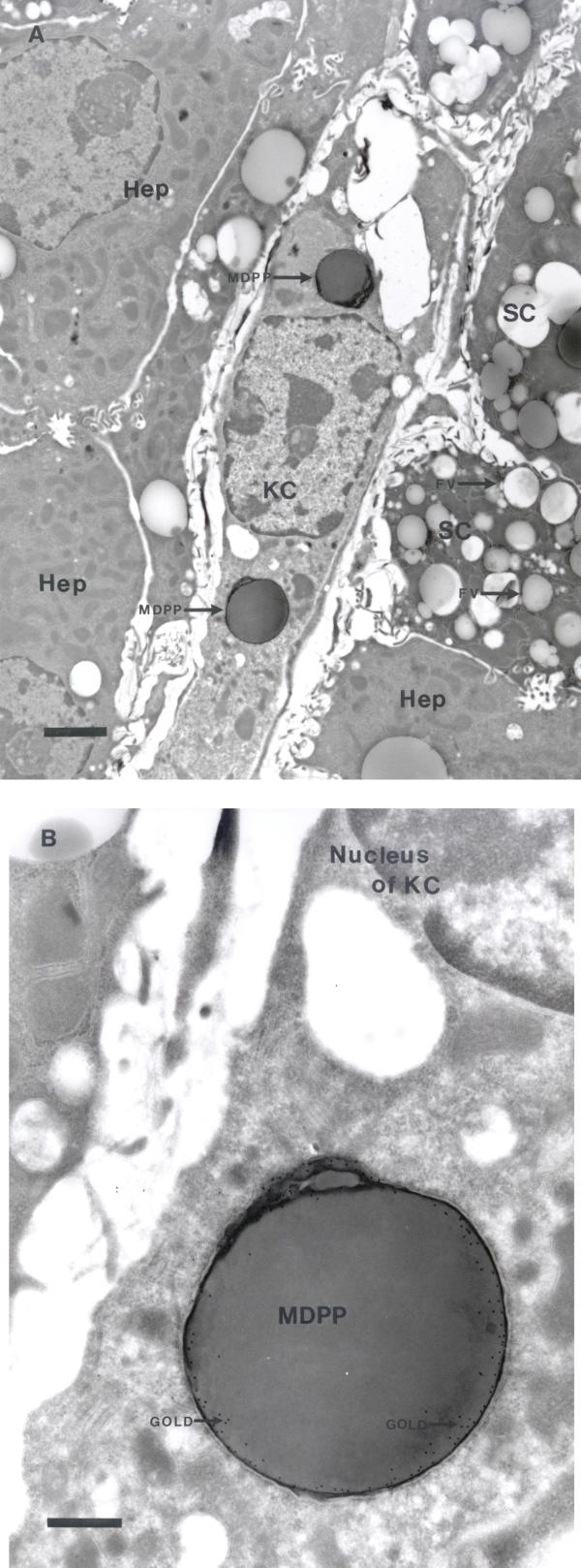
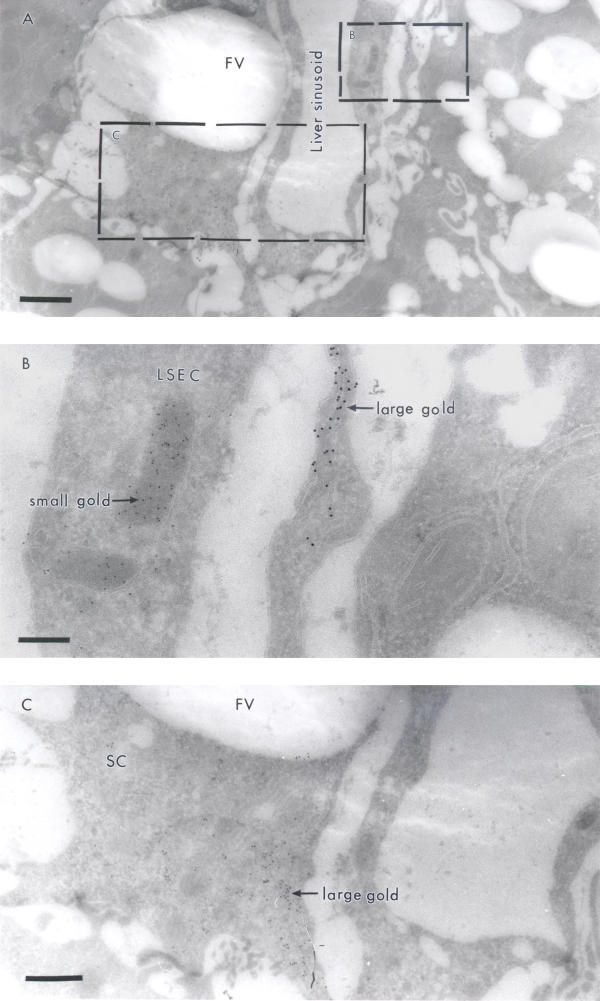
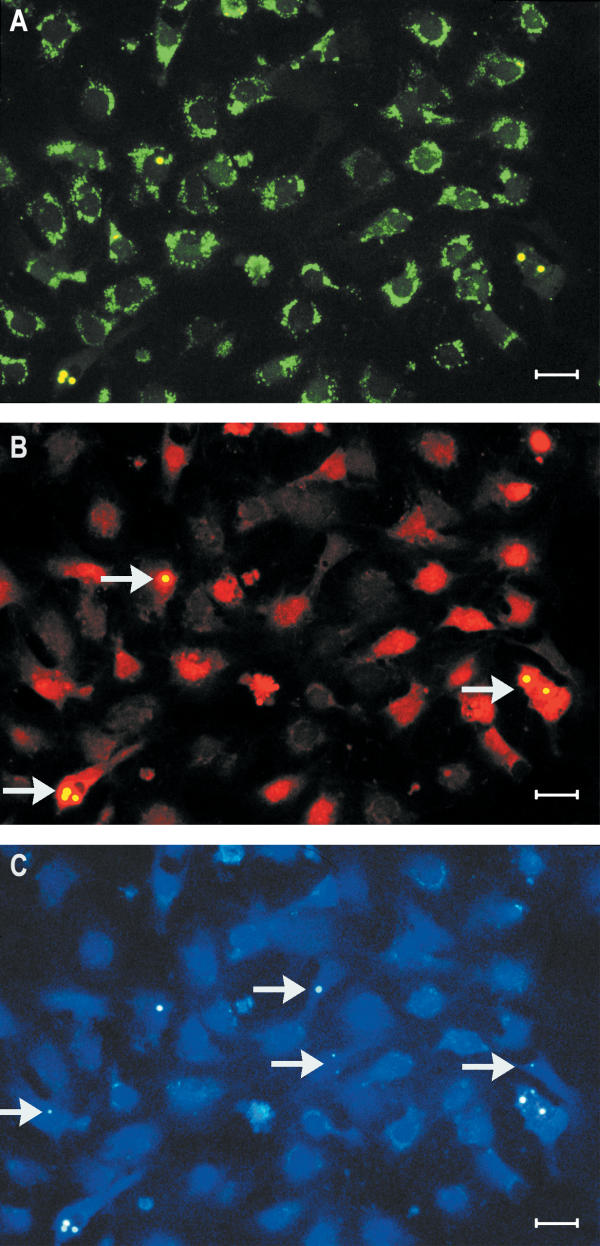
Intravenuosly administered TRITC-monodisperse polymer particles (MDPP) for identification of phagocytosing KC accumulated mainly periportally in liver acini (Figs. 3A, 3B, 3C). Immunoelectron microscopy of liver sections that had been reacted with anti-TRITC-antibodies and protein A-gold revealed the presence of gold particles along the periphery of the surface of the particles, allowing a reliable identification and intracellular location of TRITC-MDPP (Figs. 4A, 4B). In contrast to these particles, FITC-FSA was taken up exclusively in LSEC-like cells lining the liver sinusoids (Fig. 3B). To distinguish LSEC from stellate cells, double immunolabeling was performed to visualize FITC-FSA and desmin in transmission electron microscopy. FITC-FSA and desmin were observed in distinct cell types along the sinusoidal lining (Fig. 5). FITC-FSA was associated with organelles judged as lysosomes of LSEC.
Figure 3.
Fluorescence micrographs of liver section. Following intravenous administration of fluorescently labeled substances, sections were prepared as described in the Methods section. A heterogeneous distribution of yellow fluorescence from TRITC-labeled monodisperse polymer particles (MDPP) phagocytosed by Kupffer cells was located mainly in the periportal region of the liver acinus (arrows) (A). Green fluorescence along the lining of the liver sinusoids identifies endocytosed FITC-formaldehyde-treated serum albumin (FSA) by liver sinusoidal endothelial cells (LSEC), while the localization of phagocytosed MDPP is shown by arrows (B). Uptake of FITC-FSA (arrowheads) and MDPP (arrow) is shown more clearly at higher magnification in C. (Scale bars; A: 80 μm, B: 20 μm, C: 8 μm).
Figure 4.
Uptake of monodisperse polymer particles (MDPP) in Kupffer cells (KC). Following intravenous administration of fluorescently labeled substances, sections were prepared as described in the Methods section for transmission electron microscopy. MDPP are located intracellularly in Kupffer cells, as judged by their characteristic phagocytosis of the particles (A). Hepatocytes (Hep) contain numerous mitochondria. The cells that contain fat vacuoles (FV) may represent stellate cells (SC). To distinguish between vacuoles containing fat and phagocytosed MDPP, sections were immunolabeled with monoclonal anti-mouse TRITC-conjugate. Gold particles are located in the periphery of MDPP where the TRITC-molecules are attached (B). (Scale bars; A: 2 μm, B: 500 nm).
Figure 5.
Stellate cells (SC) and liver sinusoidal endothelial cells (LSEC). Following intravenous administration of fluorescently labeled substances, sections were prepared as described in the Methods section for transmission electron microscopy. Ultrathin sections were immunodouble labeled to visualize both FITC-labeled formaldehyde-treated serum albumin (FSA) in LSEC and desmin in SC. Figures B and C are higher magnification of segments of figure A. Cells lining the sinusoids (A) are LSEC as judged by the localization of small gold particles (5 nm, small arrow) in organelles taken as lysosomes (B). The cell containing large fatty vacuoles (FV) and large gold particles (10 nm, large arrow), was judged as a stellate cell (SC) (C). (Scale bars; A: 1 μm, B: 200 nm, C: 500 nm).
Cell separation
The number of non-parenchymal cells (NPC) obtained per liver following collagenase dispersion and isopycnic density separation in iodixanol was 280 × 107 (range 50–890 × 107) (weight of liver 237.1 g (43.6)) with a viability of 95.4% (2.5) as judged by trypan blue exclusion (Table 1). The corresponding figures for hepatocytes were 1880 × 107 (1110 × 107) and 94.1% (2.2). The cells obtained after iodixanol separation were subjected to centrifugal elutriation and collected in 4 fractions. The corresponding recoveries expressed as number of NPC and percentages of total are displayed in Table 2.
Table 1.
Parameters of liver perfusions, recovery of non-parenchymal cells (NPC), and viability (n = 10).
| Body wt (kg) | Liver wt (g) | Collagenase perfusion (min) | Portal-flow (mL·min-1) | Total NPC (×107) | Viability NPC (%) |
| 7.6 (0.6)* | 237.1 (43.6)* | 16.5 (3.2)* | 304.9 (47.4)* | 280 (50–890)# | 95.4 (2.5)* |
*The values are expressed as: mean (standard deviation). #The value is expressed as: mean (range).
Table 2.
Yield of non-parenchymal cells (NPC) from elutriation fractions (n = 4).
| Fraction | Flow rate (mL·min-1) | Number of NPC (×107) | % of total NPC |
| 1 | 18.5 (1.0) | 190 (68) | 69.2 |
| 2 | 32.0 (0.0) | 62 (12) | 23.0 |
| 3 | 37.0 (0.0) | 13 (8) | 5.0 |
| 4 | 45.0 (0.0) | 7 (2) | 2.7 |
The values are expressed as: mean (standard deviation).
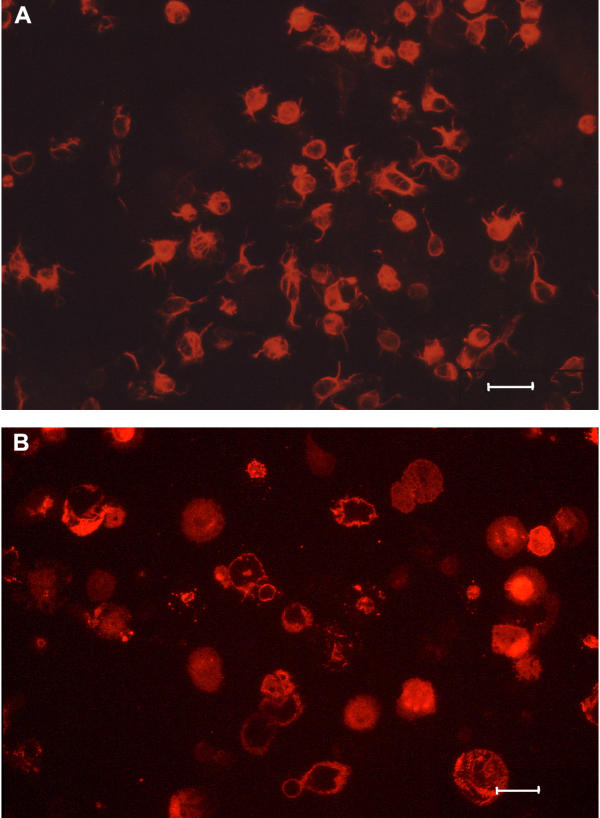
Identification of cultured cells
Cells, seeded on fibronectin-coated substrate, obtained from the elutriation fractions yielded LSEC cultures of varying purity (Table 3). We used in vivo (Fig. 6A) or in vitro administered FITC-FSA as a specific LSEC marker, positive reaction with anti-desmin antibodies as a specific marker of stellate cells (Fig. 7A), and a specific anti-pig macrophage antibody (Fig. 7B) or phagocytosis of TRITC-MDPP (Fig. 6B) as KC specific markers. Using these criteria, cultures resulting from elutriation fraction 1 were shown to contain 63.9% stellate cells; cultures established from fraction 2 contained 80.4% LSEC, and fractions 3 and 4 contained 66.2% and 61.0% LSEC. Cells that reacted with anti-pig-macrophage antibodies or phagocytosed TRITC-MDPP contained no FITC-FSA. Stellate cells were distinguished by immunolabeling with anti-desmin antibodies or by their content of characteristic autofluorescence from vitamin A droplets when irradiated with light of 328 nm of wavelength ([12]) (Fig. 6C).
Table 3.
Identification of cells after cultivation of elutriation fractions.
| Fraction | FITC – FSA | Desmin | KC | Hepatocytes |
| 1 | 32.1 (12.6) | 63.9 (15.4) | 4.0 (6.9) | 0.0 (0.0) |
| 2 | 80.4 (6.4) | 10.9 (9.2) | 7.0 (1.4) | 1.7 (1.6) |
| 3 | 66.2 (11.1) | 7.1 (3.8) | 15.2 (13.5) | 11.5 (17.5) |
| 4 | 61.0 (17.5) | 2.1 (1.7) | 10.9 (10.9) | 26.0 (19.4) |
Prior to isolation of cells, pigs received FITC-labeled formaldehyde-treated serum albumin (FSA) intravenously. Stellate cells stained with monoclonal mouse anti-human desmin antibody and Kupffer cells (KC) stained with anti-pig macrophage antibodies. Hepatocytes were identified by simple morphology. Values are percent of total number of cells per culture (n = 3). The values are expressed as: mean (standard deviation).
Figure 6.
Fluorescence micrographs of cultured liver sinusoidal endothelial cells (LSEC). Cultures were prepared as described in the Methods section. The cultures were fixed in 4% paraformaldehyde, after 6 h of incubation. FITC-labeled formaldehyde-treated serum albumin (FSA) and TRITC-labeled monodisperse polymer particles (MDPP) were administered intravenously prior to isolation of liver cells. Fluorescent microscopy reveals a homogeneous LSEC culture contaminated by a few cells with TRITC-MDPP and lipid containing vacuoles. The green fluorescence from endocytosed FITC-FSA demonstrates that most cells are LSEC, and that the probe is localized in cytoplasmic vacuoles (A), whereas the yellow fluorescence from phagocytosed TRITC-MDPP identifies Kupffer cells (arrows) (B). Autofluorescence from vitamin A identifies stellate cells (arrows) (C). (Scale bars; 20 μm).
Figure 7.
Fluorescent micrographs of cultured stellate cells and Kupffer cells. Cultures were prepared as described in Methods. The cultures were fixed in 4% paraformaldehyde, after 1 h of incubation. Micrographs of cultured stellate cells stained with monoclonal anti-desmin antibody (A) and cultured Kupffer cells stained with monoclonal anti-pig macrophage antibody (B). (Scale bars; 20 μm).
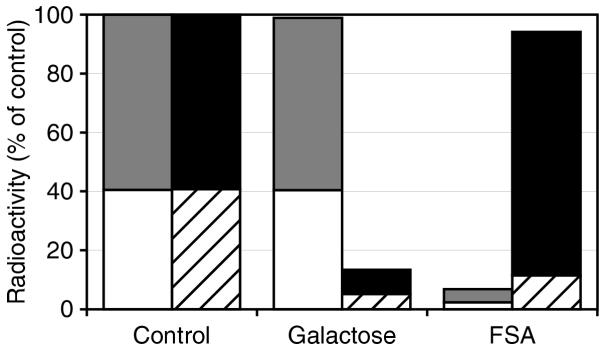
Specificity of endocytosis in cultured LSECs and hepatocytes
The specificity of endocytosis of 125I-FSA and 125I-asialo-orusomucoid protein (ASOR) in cultured LSEC and hepatocytes was studied by attempting to inhibit the uptake of trace amounts of radiolabeled ligands using excess amounts of unlabeled ligands. Incubation of LSEC cultures with 125I-FSA in the presence of excess amounts of unlabeled FSA (100 mg·mL-1) resulted in a 90% inhibition of uptake (Fig. 8). The presence of galactose (50 mmol·L-1) did not inhibit endocytosis of 125I-FSA by LSEC. Incubation of hepatocytes with 125I-ASOR in the presence of excess amounts of galactose (50 mmol·L-1) inhibited uptake by 85%. Unlabeled FSA did not inhibit endocytosis of 125I-ASOR by hepatocytes (Fig. 8).
Figure 8.
Specificity of endocytosis of 125I-formaldehyde-treated serum albumin (FSA) in cultured liver sinusoidal endothelial cells (LSEC) (grey and white bars), and 125I-asialo-orusomucoid protein (ASOR) in cultured hepatocytes (black and hatched bars). Monolayer cultures were incubated for 2 hrs, at 37°C, with trace amounts of labeled ligand alone (control) or together with excess amounts of unlabeled FSA (100 μg·mL-1) or galactose (50 mmol·L-1). The presence of unlabeled FSA inhibited effectively the endocytosis of 125I-FSA in LSEC, while galactose showed no such inhibitory effect. Galactose had an inhibitory effect on endocytosis of 125I-ASOR in hepatocytes, whereas unlabeled FSA showed no such inhibitory effect. Results, given as percent of control, are the means of triplicate experiments. Grey and white bars: 100% corresponds to 12.7% of added cpm, black and hatched bars: 100% corresponds to 14.6% of added cpm. White and hatched areas of bars represent % degraded ligand. Grey and black areas of bars represent % cell-associated ligand.
Discussion
Although it is assumed that pig LSEC perform the same physiological scavenger function as it has been observed in rat LSEC [3], it has actually never been shown. Since endothelial cells of the liver of most vertebrate species are associated with clearance activity [9], we wanted to study whether pig liver clearance function resides in the scavenger activity of LSEC in the same way as it has been shown in the rat. To this end, endocytosis of both foreign and physiological waste macromolecules in pig LSEC was studied in vivo and in vitro. For the in vitro studies we also developed a method for mass isolation and culture of pig LSEC.
Rate of elimination and organ distribution of FSA and α-mannosidase
First we studied the circulatory survival and anatomical distribution of FSA, a frequently used test ligand for the LSEC scavenger receptor in rat [13], and α-mannosidase, a physiological ligand for the mannose receptor of rat LSEC [14]. Studies in the rat and other vertebrates have shown that 125I-FSA is degraded very rapidly after uptake, resulting in rapid escape of radiotracer from the site of uptake. For this reason, FSA was labeled with 125I-TC, which is trapped in the lysosomes at the cellular site of uptake, thus preventing 125I escape from the uptake site [15]. Previous studies in the rat and other vertebrates showed that α-mannosidase, after its rapid uptake by the mannose receptor, accumulates within lysosomes and is reused for several hours before being degraded [5]. Therefore, α-mannosidase was labeled with 125I in a direct, conventional manner. Both 125I-TC-FSA and 125I-α-mannosidase were rapidly eliminated from the circulation, with 50% of the ligands being removed during the first 2–5 min after intravenous administration. This rapid removal suggested a very efficient uptake mechanism. Monitoring of radioactivity in the organs showed that the liver contained 53% (FSA) and 62% (α-mannosidase) of injected dose, suggesting that a cell type(s) in liver was responsible for clearance via the scavenger and mannose receptors. Surprisingly, as much as 26% FSA and 18% α-mannosidase were recovered in lungs. This is clearly different than in the rat, where uptake in the lungs of these and other soluble macromolecular waste products have not been observed [3]. A recent report [16] showed that ligands for studies of reticuloendothelial function were taken up in both lung and liver of pig, similarly to what we found using α-mannosidase and FSA. It was concluded from that study that 198Au colloidal particles and iron oxide particles were taken up in pulmonary intravascular macrophages. The possibility that these ligands might have been taken up by scavenger endothelial cells was not mentioned in that paper.
In vivo liver cell identification
To determine the role of different sinusoidal cells in the clearance function of pig liver, the cellular site of uptake of FITC-FSA was compared with that of TRITC-MDPP (a functional marker of phagocytosing KC), and immunoreactive desmin (a marker of stellate cells). Since light microscopy does not allow a clear distinction between particles that are truly internalized and those that are associated with the cell surface, liver tissue was prepared for electron microscopy. To enable a distinction between vitamin A-containing lipid droplets in stellate cells and internalized MDPP in KC, sections were first incubated with anti-TRITC-antibodies, then with protein A-gold. Observations of these sections revealed gold staining along the surface of the MDPP particles, corresponding to the surface localization of TRITC. Double immunolabeling showed that FITC-FSA (5 nm gold) was always associated with endothelial like lining cells that neither took up MDPP nor contained desmin (10 nm gold), indicating that the hepatic uptake in vivo of FSA was exclusively in LSEC, similar to what has been found in the rat [13].
Separation, cultivation, and characterization of cells in vitro
To allow a more detailed study of the tentative scavenger function of pig LSEC, we developed a protocol for isolation of sinusoidal cells. The protocol was modified as compared to rat [17] and mouse liver. According to the literature, rat and mouse liver sinusoidal cells can be isolated in high yield and purity using isopycnic separation. We found that this method was insufficient to isolate such cells from pig due to the high number of desmin-positive cells; therefore, we included centrifugal elutriation to separate the cells according to size. Using collagenase perfusion through the portal vein, followed by differential centrifugation, isopycnic centrifugation, and centrifugal elutriation we obtained 4 fractions, of which fraction 2, containing 62 × 107 (12 × 107) sinusoidal cells, gave monolayer cultures on fibronectin that were 80% pure in LSEC, as judged by uptake of intravenously administered FITC-FSA. The FITC-FSA positive LSEC did not react with anti-desmin or anti-pig macrophage antibodies. Conversely, only cells that took up TRITC-MDPP reacted with the anti-pig macrophage antibodies (about 11% of the plated cells).
Specific endocytosis of FITC-FSA was used successfully for vital-staining of LSEC either in vivo by intravenous injection, or by administration to LSEC-cultures in vitro. Since FITC-FSA is a highly stable molecule that can be easily and inexpensively prepared without special equipment, and stored for years in the freezer or refrigerator, we find this probe superior to other marker molecules launched as LSEC-specific functional markers (e.g., fluorescently-labeled acetylated LDL [18]) that are unstable and require expensive equipment for preparation. Although KC could be identified in vivo by their specific ability to phagocytose MDPP, this marker was disadvantageous for in vitro KC identification for the following two reasons: 1) KC that had phagocytosed intravenously administered MDPP exhibited significantly altered sedimentation properties on subseqent centrifugal elutriation; and 2) in vitro cultured KC did not phagocytose MDPP under the conditions used. These difficulties forced us to look for alternative ways of identifying the KC. Fortunately, an anti-pig-macrophage antibody kindly provided by Dr. A. Berndt, Germany, gave a specific staining of KC, but not of other types of liver cells; therefore this method was preferred as a method for identification of KC. The identification of stellate cells was at first based on demonstration of vitamin A-positive lipid droplets, that could be easily detected by autofluorescence when illuminated with light of 328 nm of wavelength. However, since vitamin A appeared to be present to a variable extent in stellate cells, we decided to employ immunostaining for desmin with a monoclonal antibody.
Specificity of endocytosis in cultured LSECs
The observation that uptake of 125I-FSA by cultured LSEC could be inhibited by excess amounts of FSA, but not by galactose, indicates that the cells express the same functional type of scavenger receptor as has been reported for rat LSEC [13]. The finding that FITC-FSA was taken up only in LSEC in vivo and in vitro is further evidence that the porcine and rat LSEC scavenger receptors are functionally similar. The finding that LSEC isolated and cultured according to the presently developed protocol, perform a highly active scavenger-receptor-mediated endocytosis proves that pig LSEC prepared according to our protocol have preserved their in vivo scavenger function.
Although several authors have reported the presence of LSEC in cultures of porcine liver cells, methods of identification of LSEC were unable to distinguish convincingly LSEC from other types of liver cells. In a study on isolation of NPC from piglets (1–15 days of age), Caperna et al. [19] used absence of uptake of 5 μm latex beads as a characteristic of LSEC. However, our observation that KC only rarely phagocytose particles in vitro, along with the fact that other liver cell types (i.e., stellate cells and lymphocytes) are unable to perform phagocytosis, suggest that absence of phagocytosis is not a valid way of distinguishing LSEC from other liver cells. In other studies, positive immune staining of von Willebrand factor has been used to identify pig LSEC [10,11]. However, the fact that this marker is widely used to identify vascular endothelial cells in general [20], together with other reports claiming that LSEC are devoid, or stain only weakly for this antigen, suggest that von Willebrand factor should not be used as a specific LSEC marker. Prostacyclin PGI2 generation has been used as a LSEC-specific marker [21]. However, PGI2 is a general endothelial marker, and can not be used as a LSEC-specific marker. Fluorescently labeled acetylated LDL has been used in much the same way as we used FITC-FSA as a vital stain to demonstrate the scavenger function of LSEC [22]. Nevertheless, it has been shown that this probe, in contrast to FITC-FSA, is taken up in brain microvessel endothelial cells [23], as well as in peripheral macrophages [24]).), suggesting that FITC-FSA is superior as a LSEC specific marker.
Conclusions
This study showed that pig LSEC are endowed with the same scavenger activity as rat LSEC. Although a method was recently reported for isolation of pig LSEC, with an average yield of 90 000 cells per liver [10], our method offers true mass isolation of LSEC, yielding 62 × 107 (12 × 107) purified LSEC per liver.
Methods
Antibodies and ligands
Monoclonal mouse anti-human desmin, clone D33, was from DAKO A/S, Denmark. Monoclonal goat anti-mouse IgG, TRITC-conjugate, was from Zymed, CA. Monoclonal rabbit anti-FITC was from DAKO A/S, Denmark. Monoclonal rabbit anti-TRITC was from Molecular Probes Inc., OR. Two mouse monoclonal antibodies (clones 2G6 and 2B10) against porcine macrophages were kindly provided by Dr. A. Berndt, Institute of Pathology, Friedrich Schiller University, Jena, Germany [25]. FSA was prepared as described [26]. ASOR was kindly provided by Dr. Trond Berg, University of Oslo, Norway. Bovine α-mannosidase was donated by Dr. O.K. Tollersrud, University of Tromsø, Norway.
Labeling procedures
Proteins were labeled with 125I (carrier free Na125I from Institute of Energiteknikk, Norway) either by a direct reaction employing Iodogen (Pierce, Rockford, IL) [27], or by conjugating the protein with 125I-labeled TC [15]. The iodinated proteins, with 125I attached to aromatic amino acids, were separated from free 125I on a PD-10 column (Sephadex G-25, Pharmacia, Sweden) equilibrated and eluted with PBS.
FSA (0.8 mg·mL-1) was incubated with FITC (Sigma-Aldrich, Norway) in sodium carbonate buffer (0.5 mol·L-1, pH 9.5) in a protein/dye weight ratio of 1:1 at 4°C overnight. Unreacted dye was removed by gel filtration through a PD-10 column equilibrated and eluted with PBS without Ca2+ or Mg2+.
Approximately 8.0 × 1010 MDPP, with a diameter of 2.0 μm (SINTEF, University of Trondheim, Norway) were incubated overnight in 1 mg·mL-1 TRITC (ICN Biomedicals Inc., CA) in sodium carbonate buffer (0.1 mol·L-1, pH 9.5) at 4°C. The TRITC-MDPP were washed three times in 70% ethanol, and finally in PBS to remove unbound TRITC.
Determination of anatomical distribution and serum t1/2
Serum half-life and organ distribution of intravenously administered radiolabeled FSA and α-mannosidase were determined as described [28]. Briefly, approximately 100 × 106 cpm 125I-TC-FSA or 125I-α-mannosidase were injected into the left jugular vein. Blood sampling was started immediately by collecting 2 mL blood samples from an intravenous catheter positioned in the right jugular vein. The organs were taken out after one hour, weighed and measured in a γ-counter (Cobra II, Packard Instrument Co., Inc., CT).
Surgical procedures
The experimental protocol was approved by the local steering committee of the Norwegian Experimental Animal Board. All animals received care according to the criteria outlined in the "Guide for the Care and Use of Laboratory Animals" prepared by the National Academy of Sciences and published by the National Institutes of Health (NIH publication 86–23 revised 1985). Castrated male pigs weighing 7.6 kg (0.6) (Sus scrofa domesticus, Norwegian strain) were fasted 18 hours with free access to water. Intramuscular ketamine (75 mg·kg-1) (Parke-Davis, Sweden) and atropine sulfate 1 mg (Nycomed Pharma, Norway) were used as premedication. The pigs were tracheostomized, intubated, and ventilated on a volume controlled ventilator (Servo 900, Elema-Schönander, Sweden). Anesthesia was maintained with continuous i.v. infusions of sodium pentobarbital (4 mg·kg-1·min-1) (Abbott Scandinavia, Sweden) and fentanyl (0.05 mg·kg-1·min-1) (Alpharma, Norway). A midline laparotomy was performed. The portal vein was mobilized and the portal bloodflow was measured with a flowprobe (CardioMed, Norway). Sodium heparin (3000 IU) (Leo, Denmark) was administered intravenously. FITC-FSA (40 mg) was administered intravenously via the left jugular vein, while some pigs received TRITC-MDPP injected via the portal vein as two boluses 30 and 5 minutes prior to perfusion. The hepatoduodenal ligament was ligated, and the portal vein was cannulated. Ca2+-free HEPES [29] solution at 37°C was perfused in vivo with a roller pump (Gambro, AK-10, Sweden) at the same rate as the portal blood flow. The liver was weighed, thereafter perfused ex vivo with a Ca2+-containing HEPES-solution with 0.02% Collagenase P (Roche Diagnostics, Norway) in a basin at 37°C.
The digested liver was transferred to a different basin containing RPMI 1640 medium with 1% BSA (4°C). After removing the stroma, the suspension was subsequently filtered through 1000 and 500 μm nylon mesh. The resulting cell suspension was subjected to centrifugation at 50 g to selectively sediment hepatocytes from NPC. The pellet of hepatocytes was resuspended, and subsequently washed two more times at 50 g. Cell viability was estimated from the percentage of cells which excluded 0.4% trypan blue.
Separation of NPC
The NPC in the first and second supernatants from the low-speed centrifugations were pelleted by high-speed centrifugation (1300 g) followed by resuspension in small volume before isopycnic centrifugation in a 12% iodixanol gradient (Nycomed, Norway) to generate a band of further enriched NPC. This fraction was washed in PBS and resuspended in HBSS, supplied with 4 mmol·L-1 EDTA, 1% FCS and 0.3% BSA, and loaded into the mixing chamber over 1 min. The NPC suspensions were fractionated in a J-21-B centrifuge fitted with a JE-6 elutriator rotor (Beckmann Instruments, Inc., CA). A pre-enrichment step was performed to further remove hepatocytes and cell aggregates with a pump flow rate of 30 mL·min-1 and rotorspeed at 1400 rpm. Four consecutive fractions, corresponding to pump flow rates of 18.5, 32, 37 and 45 mL·min-1, were collected from the rotor which was spun at a constant speed of 2500 rpm, at 15°C. The volume of effluent at each flow rate was 150, 250, 250 and 250 mL.
Immunolabeling and characterization of cultured cells
Monolayer cultures of hepatocytes and cells from each elutriation fraction were established on fibronectin-coated glass-coverslips inserted in 2 cm2 culture wells and maintained in serum-free RPMI 1640 medium in a CO2-incubator at 37°C. Cultures were fixed in 4% paraformaldehyde in PBS for 1 hour, after attachment and spreading.
Immunocytochemistry
To examine the distribution of FITC-FSA and TRITC-MDPP, small sections were taken at the periphery of the liver lobules during the washing perfusion, fixed in 4% paraformaldehyde, prepared and sectioned for fluorescence microscopy.
Sections and fixed cultures were embedded in antifade mounting medium (Dako Corp., CA). Examination of the mounted coverslips was performed in an Axiophot photomicroscope equipped with phase-contrast, fluorescence optics and a filter for excitation (wavelength 328 nm) of vitamin A (Zeiss Axiophot, Germany). Pictures were recorded on Kodak Ektachrome P1600X ASA (Kodak, Japan).
Whole livers were perfusion-fixed with McDowell's fixative (4% paraformaldehyde, 1% glutaraldehyde in PBS). Specimens for immunotransmission electron microscopy were prepared as described [30]. Briefly, small cubes were cut out of the liver tissue, and incubated in 2.3 mol·L-1 sucrose overnight before immersion in liquid nitrogen on aluminum pins. Ultrathin sections were cut using a diamond knife (Drukker international, The Netherlands). Before immunolabeling, sections were retrieved in sucrose and mounted on carbon coated grids. Sections were blocked for 15 minutes in 1% cold water fish skin gelatin (Sigma-Aldrich, Norway), followed by incubation with anti-TRITC (diluted in cold water fish skin gelatin), washing in PBS and incubation with protein A-gold (University of Utrecht, The Netherlands) [31] diluted in cold water fish skin gelatin for 15 minutes. Double labeling was performed in a sequential manner, using a fixative block (1% glutaraldehyde) between the first and second marker pair. The sections were then washed in PBS followed by washing in distilled water and dried in 1.8% methylcellulose and 0.3% uranyl acetate, and examined in a JEOL JEM 1010 transmission electron microscope (Tokyo, Japan) at 80 kV. Micrographs were recorded on Kodak electron microscope film, no. 4489 (Kodak, Tokyo, Japan).
Endocytosis studies in vitro
LSEC and hepatocyte cultures, established in 2 cm2 wells and maintained in serum-free RPMI 1640 medium, were washed and supplied with fresh medium containing 1% serum albumin and labeled proteins, 125I-FSA or 125I-ASOR (20 000 cpm per well). Specificity of endocytosis was studied by incubation with excess amounts of unlabeled FSA (100 μg·mL-1) or galactose (50 mmol·L-1). Incubations, carried out for 2 hours at 37°C to measure endocytosis, were terminated by transferring the media, along with one wash, to tubes containing 20% TCA, which precipitates only intact protein. The extent of degradation was determined by measuring the radioactivity in the pellet and supernatant that was obtained after centrifugation of the media. Cell-associated ligand was quantified by measuring the amount of radioactivity released by solubilizing the cultures in 1% (w/v) SDS. Radioactivity was measured in a γ-counter (Cobra II, Packard Instrument Co., Inc., Meridien, CT).
Statistics
The values are expressed as: mean (standard deviation) unless otherwise noted.
Authors' contributions
GIN and KHE designed and carried out the experiments. GIN drafted the manuscript. LMY contributed significantly to the animal preparation. RO carried out the electron microscopy studies. AR and BS coordinated the study and contributed to the text of the manuscript.
All authors have read and approved the final manuscript.
Acknowledgments
Acknowledgements
The authors would like to express their gratitude to Hege Hagerup, Ellinor Hareide, and Marna-Lill Kjæreng, Surgical Research Laboratory, University of Tromsø, for skilful technical assistance. The surgical assistance by Ebrahim Aghajani M.D., Odd-Petter Elvenes M.D. and Christian Korvald M.D. is greatly appreciated. The authors are grateful for the advice of Dr. Peter A. G. McCourt.
This work was supported by grants from the Norwegian Research Council.
Contributor Information
Geir I Nedredal, Email: Geir.Ivar.Nedredal@fagmed.uit.no.
Kjetil H Elvevold, Email: Kjetilhe@fagmed.uit.no.
Lars M Ytrebø, Email: Larsmy@fagmed.uit.no.
Randi Olsen, Email: randio@fagmed.uit.no.
Arthur Revhaug, Email: arthur.revhaug@unn.no.
Bård Smedsrød, Email: baards@fagmed.uit.no.
References
- Watanabe FD, Mullon CJ, Hewitt WR, Arkadopoulos N, Kahaku E, Eguchi S, Khalili T, Arnaout W, Shackleton CR, Rozga J, Solomon B, Demetriou AA. Clinical experience with a bioartificial liver in the treatment of severe liver failure. A phase I clinical trial. Ann Surg. 1997;225:484–491. doi: 10.1097/00000658-199705000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aschoff L. Ergeb Inn Med Kinderhk. 1924. pp. 1–118.
- Smedsrød B, Pertoft H, Gustafson S, Laurent TC. Scavenger functions of the liver endothelial cell. Biochem J. 1990;266:313–327. doi: 10.1042/bj2660313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hansen B, Melkko J, Smedsrød B. Serum is a rich source of ligands for the scavenger receptor of hepatic sinusoidal endothelial cells. Mol Cell Biochem. 2002;229:63–72. doi: 10.1023/A:1017919800347. [DOI] [PubMed] [Google Scholar]
- Smedsrød B, Tollersrud OK. Sinusoidal liver endothelial cells recruit lysosomal enzymes from the circulation by mannose-receptor mediated endocytosis. In: Wake K, Wisse E, Knook DL, editor. Cells of the hepatic sinusoid. Leiden, Kupffer Cell Foundation; 1995. pp. 180–183. [Google Scholar]
- Van Berkel TJ, De Rijke YB, Kruijt JK. Different fate in vivo of oxidatively modified low density lipoprotein and acetylated low density lipoprotein in rats. Recognition by various scavenger receptors on Kupffer and endothelial liver cells. J Biol Chem. 1991;266:2282–2289. [PubMed] [Google Scholar]
- Smedsrød B, Melkko J, Araki N, Sano H, Horiuchi S. Advanced glycation end products are eliminated by scavenger-receptor-mediated endocytosis in hepatic sinusoidal Kupffer and endothelial cells. Biochem J. 1997;322:567–573. doi: 10.1042/bj3220567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawai Y, Smedsrød B, Elvevold K, Wake K. Uptake of lithium carmine by sinusoidal endothelial and Kupffer cells of the rat liver: new insights into the classical vital staining and the reticulo-endothelial system. Cell Tissue Res. 1998;292:395–410. doi: 10.1007/s004410051069. [DOI] [PubMed] [Google Scholar]
- Seternes T, Sørensen KK, Smedsrød B. Scavenger endothelial cells of vertebrates: a nonperipheral leukocyte system for high-capacity elimination of waste macromolecules. Proc Natl Acad Sci USA. 2002;99:7594–7597. doi: 10.1073/pnas.102173299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerlach JC, Zeilinger K, Spatkowski G, Hentschel F, Schnoy N, Kolbeck S, Schindler RK, Neuhaus P. Large-scale isolation of sinusoidal endothelial cells from pig and human liver. J Surg Res. 2001;100:39–45. doi: 10.1006/jsre.2001.6224. [DOI] [PubMed] [Google Scholar]
- Cattan P, Zhang B, Braet F, Atia N, Conti F, Conjeaud H, Weill B, Chereau C, Houssin D, Calmus Y. Comparison between aortic and sinusoidal liver endothelial cells as targets of hyperacute xenogeneic rejection in the pig to human combination. Transplantation. 1996;62:803–810. doi: 10.1097/00007890-199609270-00018. [DOI] [PubMed] [Google Scholar]
- Knook DL, Seffelaar AM, de Leeuw AM. Fat-storing cells of the rat liver. Their isolation and purification. Exp Cell Res. 1982;139:468–471. doi: 10.1016/0014-4827(82)90283-x. [DOI] [PubMed] [Google Scholar]
- Eskild W, Kindberg GM, Smedsrød B, Blomhoff R, Norum KR, Berg T. Intracellular transport of formaldehyde-treated serum albumin in liver endothelial cells after uptake via scavenger receptors. Biochem J. 1989;258:511–520. doi: 10.1042/bj2580511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahl P, Six H, Rodman JS, Schlesinger P, Tulsiani DR, Touster O. Evidence for specific recognition sites mediating clearance of lysosomal enzymes in vivo. Proc Natl Acad Sci USA. 1976;73:4045–4049. doi: 10.1073/pnas.73.11.4045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittman RC, Carew TE, Glass CK, Green SR, Taylor CA, Jr, Attie AD. A radioiodinated, intracellularly trapped ligand for determining the sites of plasma protein degradation in vivo. Biochem J. 1983;212:791–800. doi: 10.1042/bj2120791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brain JD, Molina RM, DeCamp MM, Warner AE. Pulmonary intravascular macrophages: their contribution to the mononuclear phagocyte system in 13 species. Am J Physiol. 1999;276:L146–154. doi: 10.1152/ajplung.1999.276.1.L146. [DOI] [PubMed] [Google Scholar]
- Smedsrød B, Pertoft H. Preparation of pure hepatocytes and reticuloendothelial cells in high yield from a single rat liver by means of Percoll centrifugation and selective adherence. J Leukoc Biol. 1985;38:213–230. doi: 10.1002/jlb.38.2.213. [DOI] [PubMed] [Google Scholar]
- Pitas RE, Boyles J, Mahley RW, Bissell DM. Uptake of chemically modified low density lipoproteins in vivo is mediated by specific endothelial cells. J Cell Biol. 1985;100:103–117. doi: 10.1083/jcb.100.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caperna TJ, Failla ML, Kornegay ET, Richards MP, Steele NC. Isolation and culture of parenchymal and nonparenchymal cells from neonatal swine liver. J Anim Sci. 1985;61:1576–1586. doi: 10.2527/jas1985.6161576x. [DOI] [PubMed] [Google Scholar]
- Giddings JC, Banning AP, Ralis H, Lewis MJ. Redistribution of von Willebrand factor in porcine carotid arteries after balloon angioplasty. Arterioscler Thromb Vasc Biol. 1997;17:1872–1878. doi: 10.1161/01.atv.17.10.1872. [DOI] [PubMed] [Google Scholar]
- Matsuura T, Kawada M, Hasumura S, Nagamori S, Obata T, Yamaguchi M, Hataba Y, Tanaka H, Shimizu H, Unemura Y, Nonaka K, Iwaki T, Kojima S, Aizaki H, Mizutani S, Ikenaga H. High density culture of immortalized liver endothelial cells in the radial-flow bioreactor in the development of an artificial liver. Int J Artif Organs. 1998;21:229–234X. [PubMed] [Google Scholar]
- Gerlach JC, Ziemer RA, Spatkowski G, Zeilinger K, Neuhaus P. Visualization of liver sinusoidal endothelial cell repair behavior after preservation by in vitro time-lapse video microscopy. Transplantation. 1997;63:455–459. doi: 10.1097/00007890-199702150-00021. [DOI] [PubMed] [Google Scholar]
- Teifel M, Friedl P. Establishment of the permanent microvascular endothelial cell line PBMEC/C1-2 from porcine brains. Exp Cell Res. 1996;228:50–57. doi: 10.1006/excr.1996.0298. [DOI] [PubMed] [Google Scholar]
- Rommeswinkel M, Severs NJ, Koster M, Robenek H. Repression of the macrophage scavenger receptor in macrophage-smooth muscle cell heterokaryons. Arterioscler Thromb Vasc Biol. 1995;15:601–611. doi: 10.1161/01.atv.15.5.601. [DOI] [PubMed] [Google Scholar]
- Berndt A, Heller M, Methner U, Kosmehl H, Muller G. Monoclonal antibodies against porcine macrophages. Vet Immunol Immunopathol. 2000;74:163–177. doi: 10.1016/S0165-2427(00)00166-5. [DOI] [PubMed] [Google Scholar]
- Mego JL, McQueen JD. The Uptake and Degradation of Injected Labeled Proteins by Mouse-Liver Particles. Biochimica et Biophysica Acta. 1965;100:136–14. doi: 10.1016/0304-4165(65)90436-8. [DOI] [PubMed] [Google Scholar]
- Markwell MA. A new solid-state reagent to iodinate proteins. I. Conditions for the efficient labeling of antiserum. Anal Biochem. 1982;125:427–432. doi: 10.1016/0003-2697(82)90025-2. [DOI] [PubMed] [Google Scholar]
- Smedsrød B, Einarsson M. Clearance of tissue plasminogen activator by mannose and galactose receptors in the liver. Thromb Haemost. 1990;63:60–66. [PubMed] [Google Scholar]
- Alpini G, Phillips JO, Vroman B, LaRusso NF. Recent advances in the isolation of liver cells. Hepatology. 1994;20:494–514. [PubMed] [Google Scholar]
- Tokuyasu KT. Application of cryoultramicrotomy to immunocytochemistry. J Microsc. 1986;143:139–149. doi: 10.1111/j.1365-2818.1986.tb02772.x. [DOI] [PubMed] [Google Scholar]
- Slot JW, Geuze HJ. Sizing of protein A-colloidal gold probes for immunoelectron microscopy. J Cell Biol. 1981;90:533–536. doi: 10.1083/jcb.90.2.533. [DOI] [PMC free article] [PubMed] [Google Scholar]