Abstract
BACKGROUND
Distrust of the health care system may be a significant barrier to seeking medical care, adhering to preventive health care and treatment regimens, and participating in medical research.
OBJECTIVE
To describe the development and psychometric testing of an instrument (the Health Care System Distrust Scale) to measure distrust of the health care system.
METHODS
Scale development involved 2 phases. In Phase 1, a pilot instrument was developed based on a conceptual model of health care-related distrust. Draft items were created using focus group sessions with members of the general public, literature review, and expert opinion. Draft items were pilot tested with 55 individuals waiting to be assigned to jury duty at the Municipal Court of Philadelphia. A priori, candidate items for elimination or revision included those with >5% missing data, extremely low or high interitem or item-total correlations, or those having a negative effect on the scale's internal consistency. In Phase 2, we conducted a survey of 400 prospective jurors to assess the reliability and validity of the final scale scores.
RESULTS
In Phase 1, a 10-item scale was constructed that included 4 items measuring honesty, 2 items measuring confidentiality, 2 items measuring competence, and 2 items measuring fidelity. The participants in Phase 2 had a mean age of 41 years. Forty-three percent were African-American, 45% white, and 4% Hispanic. Scores on the Health Care System Distrust scale ranged from 12 to 46 with a possible range from 10 to 50. The mean score was 29.4 with a standard deviation of 6.33. No item had over 5% missing data. Internal consistency (Cronbach's α) was 0.75. Item-total correlations ranged from 0.27 to 0.57. Principal components analysis revealed 1 general component accounting for 32% of the variance. Nine of the variables had loadings higher than 0.40. As predicted, distrust of the health care system was higher among African Americans than whites and was inversely correlated with trust in personal physicians.
CONCLUSIONS
Initial testing suggests that we developed an instrument with valid and reliable scores in order to measure distrust of the health care system. Future research is needed to evaluate the validity and reliability of the Health Care System Distrust scale among diverse populations. This instrument can facilitate the investigation of the prevalence, causes, and effects of health care system distrust in the United States.
Keywords: distrust, health care
American health care has undergone tremendous change over the past several decades. Some of these changes, such as the development of effective screening tests and treatments for various diseases, have the potential to greatly reduce the burden of disease in the United States. However, this potential is threatened by another major change: rising distrust of physicians and the health care system.1–4 Concern about the prevalence and impact of health care-related distrust has led to the rapid growth of research surrounding the constructs of trust and distrust. The ability to measure health care-related trust and distrust is an important contribution to this research effort.5,6
Defining trust and distrust is both complex and necessary for any measurement effort. Most scholars agree that trust requires several key components, including significant personal vulnerability of the truster, uncertainty about the future action of others (the trustee), and a specific object or issue that is entrusted to the trustee, e.g., my children, my health.1,6–13 In some definitions, distrust is conceptualized as the absence of trust, whereas others have suggested that distrust implies negative beliefs that the trustee will act in ways against the best interest of the truster.6 Trust is also categorized by the object of trust, with categories that can be very narrow, such as a single politician, or quite broad, such as politicians in general or government as a whole.8 In health care, these categorizations have been translated into distinctions between trust in specific individuals or institutions (e.g., trust in my primary care physician), trust in certain types of individuals or institutions (e.g., trust in physicians in general), and trust in the health care system as a whole (encompassing multiple health care-related institutions).1,6
Although several scales have been developed to measure trust of physicians,5,14–18 less attention has been paid to the development of measures of trust and distrust of types of health care institutions or the health care system. To our knowledge, only two published scales exist in this area—the Health Insurer Trust Scale and the Medical Mistrust Index (which focuses on hospitals).19,20 No scale currently exists to assess trust in the health care system as a whole. Furthermore, given the potential for distrust to include negative beliefs beyond an absence of trust, measures are needed that capture distrust as well as trust. To date, relatively little is known about distrust of the health care system, including how it may influence health and health care. The development of a scale measuring health care system distrust will facilitate studies investigating the prevalence, causes, and effects of distrust of the health care system in the United States, including the contribution of this type of distrust to racial disparities in health and health care in the United States. Thus, the goals of this study were to develop a scale to measure health care system distrust and to examine the scale's psychometric properties, including whether health care system distrust functioned as a unidimensional or multidimensional construct.
METHODS
Scale development, revision, and psychometric testing were accomplished in 2 phases, using an iterative process.21
Phase 1: Scale Development
We developed a conceptual model of health care-related trust and distrust to guide scale development. Based upon scholarship from multiple fields, we defined trust as the belief by an individual (the truster) that another entity (the trustee) would act in one's best interest in the future to prevent a potentially important negative outcome. In our model, distrust implies not just the absence of trust, but the presence of beliefs that the trustee will act in ways that are against one's best interest. We postulated that trust (or distrust) has 4 domains: fidelity, competence, confidentiality, and honesty/informed consent.6 Furthermore, we categorized the objects of trust as they relate to health care as individuals (i.e., doctors, nurses, etc.), individual entities (i.e., health insurer, hospital), and the health care system in general. We hypothesized that distrust of the health care system would be inversely related to trust in personal physicians. Furthermore, we hypothesized that distrust would be higher among ethnic minorities, because of the historical and current evidence of discrimination by the health care system. We had no reason to hypothesize a priori group differences for gender, age, or education, assuming equivalent race distributions.
Guided by this conceptual model, we developed pilot items based on 4 focus groups with members of the general public and review of prior health care-related trust scales.6,16–20 Focus group participants were recruited using advertisements in free local newspapers and posted flyers. Individuals were reimbursed $20 for participation and groups were held in easily accessible locations with refreshments. Sessions lasted approximately 90 minutes and were tape recorded. After a brief introduction, previously developed open-ended questions were asked to generate discussion about beliefs related to trust and distrust of the health care system.22,23 Thirty-eight individuals participated, of whom 20 were men, 19 were African American, 14 white, and 5 Asian American. Audiotape transcripts were independently reviewed by 3 investigators to identify distinct concepts/major themes and key phrases related to health care system distrust.
A total of 15 draft items were generated. Care was taken to ensure that draft items represented both trust and distrust, captured the postulated domains of distrust, and were both positively and negatively framed. To accomplish these goals, draft items included 2 items adapted from the Trust Subscale of the Primary Care Assessment Survey.18 These items assessed fidelity (“The health care system cares more about doing what is needed for my health than holding costs down”) and honesty (“If a mistake were made in my health care, the health care system would try to hide it from me”). Items were scored on a 5-point Likert scale ranging from “strongly agree” (5 points) to “strongly disagree” (1 point). After one-on-one review with volunteers, 4 items were dropped because they were difficult to understand and 11 items were assembled into a pilot instrument.
The pilot instrument was tested in a survey of 55 individuals recruited from women and men waiting to be assigned to jury duty at the Municipal Court of Philadelphia. In Philadelphia County, prospective jurors are selected from voter registration records and adult licensed drivers. A trained research assistant asked all prospective jurors waiting to be called for jury duty to complete a survey. Those who agreed to participate were told they would receive a candy bar upon completion. Participants were not told about the survey content prior to receiving it. The survey was administered in the juror selection waiting room. The sample size for the pilot survey was selected to allow 5 respondents per item.24 Although courthouse procedures prevent the calculation of an exact response rate, based on our experience with this method and other surveys, we estimate that approximately 70% of prospective jurors volunteer to participate and over 95% of individuals who volunteer complete the questionnaires.
Item revision and selection were accomplished in 3 steps. First, items were examined for missing data with a plan to discard items with more than 5% missing data. Second, item-item and item-total correlations were examined to insure that all items were positively related to one another, but not redundant. The goal was to have item-item correlations between 0.20 and 0.40 and item-total correlations above 0.20.21 Third, items were removed sequentially beginning with the item giving the lowest corrected item-total correlation. The internal consistency of each shortened scale was calculated. Items with low item-total correlations or where internal consistency increased when they were removed were either deleted or revised.
Phase 2: Evaluation of Final Instrument
The final instrument was administered by a trained research coordinator to 400 participants at the Municipal Court of Philadelphia using the same procedures described in Phase 1. As noted previously, we estimate that between 65% and 70% of eligible participants complete the survey. The survey packet contained, in order, the Health Care System Distrust Scale, the Trust Subscale from the Primary Care Assessment Survey,18 and demographics. The Trust Subscale from the Primary Care Assessment Survey is an established 8-item measure of trust in an individual's primary physician that includes domains of integrity, competence, and agency.18 The distributions of scores on the final items were examined to assess ceiling or floor effects (i.e., the majority of respondents choosing either extreme option) and characteristics of missing data, item-total correlations, and reliability were reassessed.21 Principal components analysis was used to examine construct validity by looking at the number and characteristics of the domains.25 Interpretation of the results of the principal component analysis was guided by examining the graphical plot of Eigenvalues (scree test) and the rotated loadings of the variables on the identified components.24,26 Concurrent validity (comparison to an existing criterion) was assessed by correlating scores on the Health Care System Distrust Scale and Trust Subscale and comparing means for demographic subgroups using independent sample t tests or one-way analysis of variance as indicated. Multivariate analyses were conducted using linear regression, with Health Care System Distrust scale scores as the dependent variable and demographic characteristics (race, age, gender, and education) as independent variables.27 Age was analyzed as a continuous variable and as an ordinal variable. Education was dichotomized into college degree and higher versus less than a college degree.
Dr. Armstrong is supported by an American Cancer Society Clinical Research Training Grant and a Robert Wood Johnson Generalist Faculty Scholar Award.
RESULTS
Phase 1
Content Validity.
Eleven draft items were developed. Based on the pilot test results, 3 items were removed, 4 items were revised, and 2 items were added to the pilot scale. One item (“My consent is always requested before my medical information is released”) was removed because it was highly correlated (0.68) with a similar item, “Health records are kept private so that information about my health cannot get into the wrong hands”. Two items were dropped because of low item-total correlations (< 0.2) and because their focus was on physicians rather than the health care system: “My doctors inform me of everything going on with my health” and “My doctors only order tests and prescribe medicine in my best interest.” Items were revised for multiple reasons: 1 item was revised because of low item-total correlations (< 0.2) and concern that positive framing of an item that mentioned cost was disconsonant: “The health care system cares more about doing what is needed for my health than holding costs down” became “The health care system cares more about holding costs down than it does about doing what is needed for my health”; 3 items were revised for clarity because of relatively low item-total correlations (0.1 to 0.2) and their effects on internal consistency: “Health records are kept private so that information about my health cannot get into the wrong hands” became “My medical records are kept private”; “When they take my blood, I don’t know what they are using it for” became “When they take my blood, they do tests they don’t tell me about”; “No one will have access to my medical information unless I approve of it” became “People can get access to my medical records without my approval.”
Two positively framed items were added because positive items had been removed: “I receive high-quality medical care from the health care system” and “The health care system puts my medical needs above all other considerations when treating my medical problems.” These items were derived from 2 other scales of trust in personal physicians, the Patient Trust Scale and the Trust in Physician Scale, respectively.16,17 The final 10-item scale is shown in Table 1. Four items (a, d, e, and j) were designed to measure honesty, 2 items (b and f) to measure confidentiality, 2 items to measure competence (c and h), and 2 items to measure fidelity (g and i).
Table 1.
Health Care System Distrust Scale*
| The next questions are about your opinion of the health care system in general. When we refer to the health care system, we mean hospitals, health insurance companies, and medical research. For each statement below, please check how strongly you agree or disagree. | |||||
|---|---|---|---|---|---|
| [5] Strongly Agree, % | [4] Agree, % | [3] Not Sure, % | [2] Disagree, % | [1] Strongly Disagree, % | |
| a. Medical experiments can be done on me without my knowing about it. | 13 | 27 | 13 | 22 | 25 |
| b. My medical records are kept private. | 20 | 27 | 24 | 23 | 5 |
| c. People die every day because of mistakes by the health care system. | 24 | 47 | 17 | 10 | 3 |
| d. When they take my blood, they do tests they don’t tell me about. | 10 | 20 | 34 | 27 | 9 |
| e. If a mistake were made in my health care, the health care system would try to hide it from me. | 11 | 31 | 37 | 17 | 5 |
| f. People can get access to my medical records without my approval. | 8 | 33 | 23 | 24 | 12 |
| g. The health care system cares more about holding costs down than it does about doing what is needed for my health. | 19 | 41 | 18 | 17 | 6 |
| h. I receive high-quality medical care from the health care system. | 13 | 41 | 20 | 21 | 5 |
| i. The health care system puts my medical needs above all other considerations when treating my medical problems. | 5 | 20 | 29 | 35 | 11 |
| j. Some medicines have things in them that they don’t tell you about. | 17 | 46 | 17 | 14 | 6 |
b, h, and i are reverse scored to measure distrust.
Phase 2
A total of 400 individuals completed the survey. Participants were 62% female with a mean age of 41 years and an age range from 19 to 73. Forty-three percent were African American, 45% were white, 4% Hispanic, 2% Asian American, and 6% other. The highest level of education attained was high school diploma for 25%, some college for 31%, a college degree for 20%, and some graduate school or higher for 17%. Five percent of participants had not completed high school.
Scores on the Health Care System Distrust scale ranged from 12 to 36, out of a possible 10 to 50, with higher scores indicating more distrust. The mean was 29.4, with a standard deviation of 6.33 (See Fig. 1). Responses to specific items are reported in Table 1.
FIGURE 1.
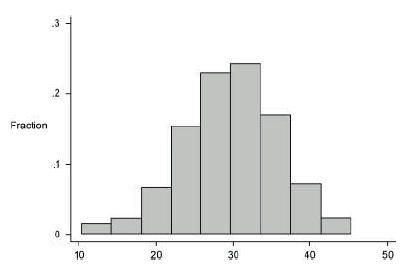
Distribution of Health Care System Distrust Scores (N = 400).
Missing Data.
No item had over 5% missing data. The amount of missing data ranged from 1.4% to 2.8%.
Ceiling and Floor Effects.
On an item level, there was little clustering at the upper or lower end of the scale. The highest or lowest response options were endorsed by no more than 25% of respondents for any given item. Moreover, for each item, all options were endorsed by some respondents.
Item-total Correlations.
Corrected item-total correlations for the scale ranged between 0.27 and 0.57.
Internal Consistency.
Cronbach's α coefficient for the scale was 0.75. Sequential item reduction trials did not increase the reliability of the scale scores.
Construct Validity.
As hypothesized, distrust scores were higher among African Americans than whites in both univariate and multivariate analyses (P = .002). In multivariate analyses, distrust scores were higher among participants with higher levels of education (P = .03 for some college or higher vs high school diploma or lower). Distrust was not associated with gender or age, although participants who were 51 to 60 had higher distrust scores than either younger or older participants. However, this difference did not reach statistical significance. (See Tables 2 and 3).
Table 2.
Unadjusted Associations with Distrust
| Distrust Score* | ||||
|---|---|---|---|---|
| N | Mean | SD | P Value | |
| Race | ||||
| African American | 156 | 30.4 | 6.30 | .002 |
| White | 178 | 28.3 | 6.06 | |
| Gender | ||||
| Women | 244 | 29.8 | 6.20 | .15 |
| Men | 147 | 28.8 | 6.65 | |
| Education | ||||
| ≤ H.S. diploma | 111 | 28.7 | 6.33 | .17 |
| ≥ Some college | 280 | 29.7 | 6.37 | |
| Age, y | ||||
| 19 to 30 | 105 | 29.2 | 6.11 | .24 |
| 31 to 40 | 89 | 29.6 | 6.73 | |
| 41 to 50 | 100 | 29.1 | 6.48 | |
| 51 to 60 | 53 | 31.2 | 6.13 | |
| 61 to 73 | 39 | 28.4 | 6.33 | |
Score is the simple sum of 10 questions from the Health Care System Distrust Scale after reversing 2 positively framed items. Possible range is from 10 to 50.
SD, standard deviation; H.S., high school.
Table 3.
Adjusted Associations with Distrust
| Mean Difference in Distrust Score | SE | P Value | |
|---|---|---|---|
| African-American | |||
| (vs white) | −1.96 | 0.69 | .005 |
| Women (vs men) | |||
| ≥ Some college | −0.66 | 0.68 | .33 |
| (vs ≤ high school diploma) | 1.65 | 0.77 | .03 |
| Age (vs 19 to 30 years) | |||
| 31 to 40 | −0.22 | 0.94 | .81 |
| 41 to 50 | 0.25 | 0.92 | .78 |
| 51 to 60 | −1.92 | 1.10 | .08 |
| 61 to 73 | 0.24 | 1.22 | .84 |
SE, standard error of mean.
Construct validity was also examined using principal components analysis. One component with an Eigenvalue of 3.17 was retained using the scree test.24–26 This component explained 32% of the total variance. For the 10 items, rotated loadings ranged between 0.38 and 0.73. Nine items had loadings above 0.40 and 7 had loadings higher than 0.50.
Concurrent Validity.
Scores on the Health Care System Distrust Scale were inversely correlated with scores on the Trust Subscale from the Primary Care Assessment Survey (Pearson Correlation Coefficient −0.34, P < .0005).
DISCUSSION
Health care-related distrust is widely believed to have grown significantly in the last several decades. This trend has been attributed to multiple causes including the emergence of managed care with restricted access to health care, disclosures of prior episodes of unethical medical research, publicity surrounding medical errors and malpractice, growing access to medical information outside of the physician's office, and less continuity and contact with personal physicians.1–6,28–32 The growth of distrust has potentially serious and negative consequences for many aspects of medical care, including physician–patient relationships, patient satisfaction, and patient acceptance and adherence to medical interventions.
We developed a 10-item instrument, the Health Care System Distrust Scale, to measure distrust of the health care system. This scale encompasses items assessing the primary domains of trust/distrust we postulated in our conceptual model: competence, confidentiality, honesty, and fidelity. In addition, the scale measures beliefs about specific practices in the health care system (e.g., doing blood tests), as well as general beliefs about the motives of the health care system (e.g., holding costs down). In a pilot test of a racially diverse group of over 400 individuals, this scale performed well, with evidence to support score construct validity and some concurrent validity. Although we hypothesized that the postulated domains of trust would be seen as multiple dimensions in the scale, principal component analysis identified a single factor, which explained over 90% of the variance. These results lend credence to the argument that the concept of health care system distrust is meaningful to members of the general public and that it can be measured as a single construct.6,8 Future work is needed to further validate this scale, including assessments of test-retest reliability, responsiveness to change, and understandability, as well as investigating the performance of the scale in different populations.
We believe that this scale offers an important addition to currently available measures of health care-related distrust. To our knowledge, there are 7 published scales of health care-related trust, 4 of which focus on trust in physicians and 3 of which focus on other specific components of the health care system. The 4 scales measuring physician trust assess trust in a specific physician or set of physicians and have generally been found to have high internal consistency (Cronbach's α ranging from 0.85 to 0.94). Several studies have used these scales to examine trust in physicians, finding that it is generally high and correlates with method of physician payment, continuity of the physician–patient relationship, satisfaction with physicians, and patient health.16,29,33–36 The other scales of health care-related distrust include the Distrust Index, which focuses on medical research, the Trust in Insurer Scale, which focuses on the individual's health insurance companies, and the Medical Mistrust Index, which focuses on hospitals.19,20,37 These scales have been less widely used to date. The choice of which scale to use in future studies depends largely on the question being asked. For studies that are focusing on a particular type of health care-related trust or interested in correlations among multiple types of trust or distrust, it is reasonable to include one or more of the more specific trust measures. For studies that are interested in the specific construct of distrust of the health care system or want to include a more general measure of health care-related distrust, the Health Care System Distrust scale may provide a reasonable and relatively parsimonious alternative.
The need to measure health care system distrust arises on several fronts. Although distrust is widely discussed as a critical threat to health care in the United States, there are very few data to support these claims. As noted above, most studies of health care-related trust or distrust to date have focused on trust in personal physicians and found relatively high levels of trust. Studies assessing the prevalence and distribution of other forms of health care-related trust and distrust, including distrust of the health care system, are needed to determine the existence and magnitude of this threat. Distrust of the health care system has been proposed as an important barrier to seeking medical care, adhering to preventive health care and treatment regimens, and participating in medical research.5,38 The availability of a scale to measure health care system distrust will facilitate testing these hypotheses. Furthermore, measurement of distrust of the health care system across racial and ethnic groups is likely to play an important role in understanding the causes of racial and ethnic disparities in health and health care in the United States.39 Although racist and unethical medical research practices are widely believed to have resulted in widespread health care-related distrust among ethnic/racial minorities, there is surprisingly little empiric evidence documenting differences in health care-related distrust among racial and ethnic groups.20,30,40–45 The availability of the Health Care System Distrust scale should facilitate research in this area. Finally, in the event that distrust of the health care system proves to be a prevalent and important barrier to health care, the Health Care System Distrust scale can facilitate the development and testing of interventions to reduce distrust.
In addition to testing the Health Care System Distrust scale, our pilot survey provides some early insights into the prevalence and correlates of health care system distrust. The majority of respondents reported that the health care system cares more about holding costs down than it does about doing what is needed for their health, that people die every day because of mistakes by the health care system, and that medicines have contents that are not revealed to patients. Over a third of respondents endorsed responses indicating distrust for other scale items. Although distrust of the health care system was higher among African Americans than whites, even after adjusting for education, this difference was relatively small (an effect size of 0.33), perhaps smaller than might have been predicted based on anecdotal reports. In multivariate analyses, distrust was higher among more educated individuals but was not significantly associated with age or gender. More research should be done to determine whether these patterns are generalizable outside of our study population and to explore their potential causes.
Our study has several limitations. We included individuals from a single metropolitan area with relatively few Hispanics or Asian Americans. Although prospective jurors are selected to be representative of the voter population, certain types of individuals, such as some professionals, may be underrepresented. Interestingly, the demographics of our sample correspond closely with those of the population of Philadelphia County, according to the 2000 U.S. Census. Our sample was 43% African American, 45% white, and 38% male with a mean age of 41 years. The adult population of Philadelphia County is 43% African-American, 45% white, and 34% male with a mean age of 41 years.46 Our assessment of construct validity was limited, focusing on association of Health Care System Distrust scores with a few sociodemographic characteristics and 1 other trust score. Furthermore, the correlation with the Trust Subscale of the Primary Care Assessment Survey may have been artificially elevated because the 2 scales have 2 similar items. We did not collect data on other participant characteristics, including prior experiences with the health care system, current utilization of health care services, health status, health insurance coverage, primary language, and immigration history, preventing us from assessing their associations with distrust or including these characteristics in our multivariate models. Our scale does not distinguish between attitudes about individual health care system components and may provide insufficient detail for studies focused on one particular component.
The development of a psychometrically sound measure of distrust of the health care system will facilitate future studies seeking to better understand the causes, prevalence, and consequences of health care-related distrust. Furthermore, the availability of this scale may allow this important construct to be added to studies in many other areas, including those exploring racial disparities, quality of medical care, and physician–patient communication. These studies represent an early step toward understanding and addressing the growth of health care-related distrust in the United States.
REFERENCES
- 1.Goold SD. Trust, distrust and trustworthiness: lessons from the field. J Gen Int Med. 2002;17:79–81. doi: 10.1046/j.1525-1497.2002.11132.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mechanic D. Changing medical organization and the erosion of trust. Milbank Q. 1996;74:171–89. [PubMed] [Google Scholar]
- 3.Gray BH. Trust and trustworthy care in the managed care era. Health Aff (Millwood) 1997;16:34–49. doi: 10.1377/hlthaff.16.1.34. [DOI] [PubMed] [Google Scholar]
- 4.McGary H. Distrust, social justice and health care. Mt Sinai J Med. 1999;66:236–40. [PubMed] [Google Scholar]
- 5.Pearson SD, Raeke LH. Patients’ trust in physicians. Many theories, few measures, and little data. J Gen Int Med. 2000;15:509–13. doi: 10.1046/j.1525-1497.2000.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hall MA, Dugan E, Zheng B, Mishra AK. Trust in physicians and medical institutions: what is it, can it be measured, and does it matter? Milbank Q. 2001;79:613–39. doi: 10.1111/1468-0009.00223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Barber B. The Logic and Limits of Trust. New Brunswick, NJ: Rutgers University Press; 1983. [Google Scholar]
- 8.Hardin R. Conceptions and explanations of trust. In: Cook K, editor. Trust in Society. vol. II. New York: Russell Sage Foundation; 2001. pp. 3–40. [Google Scholar]
- 9.Heimer C. Solving the problem of trust. In: Cook K, editor. Trust in Society. vol. II. New York: Russell Sage Foundation; 2001. pp. 40–89. [Google Scholar]
- 10.Sztompka P. In: Alexander J, Seidman S, editors. Cambridge, UK: Cambridge University Press; 1999. p. 214. [Google Scholar]
- 11.Earle T, Cvetkovich G. Social Trust: Toward a Cosmopolitan Society. New York: Praeger; 1995. [Google Scholar]
- 12.Bianco W. Uncertainty, appraisal, and common interest: the roots of constituent trust. In: Braithwaite V, Levi M, editors. Trust and Governance. vol. I. New York: Russell Sage Foundation; 1998. pp. 245–67. [Google Scholar]
- 13.Tyler T. Why do people rely on others? Social identity and social aspects of trust. In: Cook K, editor. Trust in Society. vol. II. New York: Russell Sage Foundation; 2001. pp. 285–307. [Google Scholar]
- 14.Anderson LA, Dedrick RF. Development of the Trust in Physician Scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol Rep. 1990;67:1091–100. doi: 10.2466/pr0.1990.67.3f.1091. [DOI] [PubMed] [Google Scholar]
- 15.Hall MA, Zheng B, Dugan E, et al. Measuring patients’ trust in their primary care providers. Med Care Res Rev. 2002;59:293–318. doi: 10.1177/1077558702059003004. [DOI] [PubMed] [Google Scholar]
- 16.Kao AC, Green DC, Davis NA, Koplan JP, Cleary PD. Patients’ trust in their physicians. J Gen Int Med. 1998;13:681–6. doi: 10.1046/j.1525-1497.1998.00204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Thom DH, Ribisl KM, Stewart AL, Luke DA. Further validation and reliability testing of the Trust in Physician Scale. The Stanford Trust Study Physicians. Med Care. 1999;37:510–7. doi: 10.1097/00005650-199905000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Safran DG, Kosinski M, Tarlow AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Zheng B, Hall MA, Dugan E, Kidd KE, Levine D. Development of a scale to measure patients’ trust in health insurers. Health Serv Res. 2002;37:187–202. [PubMed] [Google Scholar]
- 20.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African-American and white cardiac patients. Med Care Res Rev. 2000;57:146–61. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 21.Streiner D, Norman G. Health Measurement Scales: A Practical Guide to Their Use. Oxford: Oxford University Press; 1995. [Google Scholar]
- 22.Kitzinger J. Introducing focus groups. BMJ. 1995;311:299–302. doi: 10.1136/bmj.311.7000.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shamdajani SA. Focus Groups: Theory at Practice; Group Dynamics and Focus Group Research. Newbury Park, Calif: Sage Publications, Inc.; 1990. [Google Scholar]
- 24.Streiner D. Figuring out factors: the use and misuse of factory analysis. Can J Psychiatry. 1995;39:135–40. doi: 10.1177/070674379403900303. [DOI] [PubMed] [Google Scholar]
- 25.Stevens J. Applied Multivariate Statistics for the Social Sciences. Hillsdale, NJ: Erlbaum; 1986. [Google Scholar]
- 26.Cattell RB, Jaspars J. A general plasmode for factor analytic exercises and research. Multivariate Behavioral Research Monographs. 1967.
- 27.Harrell FE. Regression Modelling Strategies. New York: Springer; 2001. Springer Series in Statistics. [Google Scholar]
- 28.Mechanic D, Schlesinger M. The impact of managed care on patients’ trust in medical care and their physicians. JAMA. 1996;275:1693–7. [PubMed] [Google Scholar]
- 29.Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. The relationship between method of physician payment and patient trust. JAMA. 1998;280:1708–14. doi: 10.1001/jama.280.19.1708. [DOI] [PubMed] [Google Scholar]
- 30.Gamble VN. A legacy of distrust: African Americans and medical research. Am J Prev Med. 1993;9:35–8. [PubMed] [Google Scholar]
- 31.Durso TW. Health care inequities lead a mistrust research. Scientist. 1997;11:1. [Google Scholar]
- 32.Kohn LT, Corrigan JM, Donaldson MS. To Err Is Human: Building a Safer Health Care System. Washington, DC: Institute of Medicine. National Academy Press; 1999. pp. 22–41. Also available at: http://stills.nap.edu/html/to_err_is_human/. Accessed December 2, 2003. [Google Scholar]
- 33.Keating NLGD, Kao AC, Gazmararian JA, Wu VY, Cleary PD. How are patient's specific ambulatory care experiences related to trust, satisfaction, and considering changing physicians? J Gen Int Med. 2002;17:29–39. doi: 10.1046/j.1525-1497.2002.10209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thom DH The Stanford Trust Study Physicians. Physician behaviors that predict patient trust. J Fam Pract. 2001;50:323–8. [PubMed] [Google Scholar]
- 35.Safran DG, Taira DA, Rogers WH, et al. Linking primary care performance to outcomes of care. J Fam Pract. 1998;47:213–20. [PubMed] [Google Scholar]
- 36.Safran DG, Rogers W, Tarlov A, et al. Organizational and financial characteristics of health plans: are they related to primary care performance? Arch Int Med. 2000;160:69–76. doi: 10.1001/archinte.160.1.69. [DOI] [PubMed] [Google Scholar]
- 37.Corbie-Smith G, Thomas S, Geroge D. Distrust, race and research. Arch Int Med. 2002;162:2458–63. doi: 10.1001/archinte.162.21.2458. [DOI] [PubMed] [Google Scholar]
- 38.Hall W. The link between trust and physician satisfaction. ACP-ASIM Observer. 2001. p. 6.
- 39.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 40.Corbie-Smith G, Thomas S, Williams M, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. J Gen Int Med. 1999;14:537–46. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Freimuth VS, Quinn SC, Thomas SB, et al. African Americans’ views on research and the Tuskegee Syphilis Study. Soc Sci Med. 2001. p. 52. [DOI] [PubMed]
- 42.Randall VR. Slavery, segregation and racism: trusting the health care system ain’t always easy! An African American perspective on bioethics. Saint Louis University Public Law Review. 1996;15:191–235. [PubMed] [Google Scholar]
- 43.Talone P. Establishing trust after Tuskegee. Int J Radiat Oncol Biol Phys. 1998;40:3–4. doi: 10.1016/s0360-3016(97)00832-8. [DOI] [PubMed] [Google Scholar]
- 44.Hoover F. Blacks and health: a legacy of distrust. Columbus Dispatch. 1999. pp. 23–7.
- 45.Gamble VN. Under the shadow of Tuskegee: African Americans and health care (Public health then and now) Am J Public Health. 1997;87:1773–8. doi: 10.2105/ajph.87.11.1773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.US Census. Available at: http://www.fedstats.gov/qf/states/42/42101.html. Accessed December 2, 2003.


