Abstract
BACKGROUND
There is little evidence to support the widely accepted assertion that better physician-patient relationships result in higher rates of adherence with recommended therapies.
OBJECTIVE
To determine whether and which aspects of a better physician-patient relationship are associated with higher rates of adherence with antiretroviral therapies for persons with HIV infection.
DESIGN
Cross-sectional analysis.
SETTING
Twenty-two outpatient HIV practices in a metropolitan area.
PARTICIPANTS
Five hundred fifty-four patients with HIV infection taking antiretroviral medications.
MEASUREMENTS
We measured adherence using a 4-item self-report scale (α= 0.75). We measured core aspects of physician-patient relationships using 6 previously tested scales (general communication, HIV-specific information, participatory decision making, overall satisfaction, willingness to recommend physician, and physician trust; α > 0.70 for all) and 1 new scale, adherence dialogue (α= 0.92). For adherence dialogue, patients rated their physician at understanding and solving problems with antiretroviral therapy regimens.
RESULTS
Mean patient age was 42 years, 15% were female, 73% were white, and 57% reported gay or bisexual sexual contact as their primary HIV risk factor. In multivariable models that accounted for the clustering of patients within physicians' practices, 6 of the 7 physician-patient relationship quality variables were significantly (P < .05) associated with adherence. In all 7 models worse adherence was independently associated (P < .05) with lower age, not believing in the importance of antiretroviral therapy, and worse mental health.
CONCLUSIONS
This study showed that multiple, mutable dimensions of the physician-patient relationship were associated with medication adherence in persons with HIV infection, suggesting that physician-patient relationship quality is a potentially important point of intervention to improve patients' medication adherence. In addition, our data suggest that it is critical to investigate and incorporate patients' belief systems about antiretroviral therapy into adherence discussions, and to identify and treat mental disorders.
Keywords: patient compliance, HIV infections, physician-patient relations, HIV infections/drug therapy
The belief that good physician-patient relationships are associated with better adherence to antiretroviral regimens for HIV infection is widespread,1–4 and supported by several qualitative studies.5–9 However, only a few published empirical studies have examined this relationship,5,10–15 with mixed results. Two of these studies were conducted among a sample of prisoners,10,11 and thus have limited generalizability. Bakken et al.12 found that a scale measuring patients' engagement with their provider was significantly related to self-reported medication adherence, but their adherence measure did not specifically focus on antiretrovirals. The other four studies were done among diverse populations using a variety of methods, and did not find relationships between measures of physician-patient relationships and adherence.5,13–15 No large study that we are aware of has assessed which specific and mutable aspects of the physician-patient relationship produce better regimen adherence among those with HIV disease. Because accumulating evidence indicates that physicians' behaviors can be improved through training,16–26 targeting those specific aspects of the physician-patient relationship linked with greater adherence can serve to focus targeted, effective interventions.
To understand how the quality of various aspects or dimensions of provider-patient relationships is related to medication adherence in HIV disease, we surveyed a large and diverse sample of HIV-infected individuals cared for in 22 different providers' offices in Boston. We asked patients to report on the quality of their relationship with their primary HIV provider using 7 multi-item scales that assess distinct aspects of the physician-patient relationship likely to improve adherence with antiretroviral therapy. These included general communication,27 HIV-specific information,27 participatory decision making,28,29 overall satisfaction,30 willingness to recommend the physician to others,30 trust,31 and the quality of “adherence dialogue.”
METHODS
Subjects
All providers in the metropolitan Boston area caring for five or more patients with HIV disease were contacted by telephone between September 1997 and June 1998 to determine the size of their HIV panel. Nurse practitioners were included when they cared for patients without direct physician oversight. To develop this comprehensive sample, we contacted academic teaching hospitals, city hospitals, state hospitals, community hospitals, community health centers, university health services, a large staff model health maintenance organization (HMO), and private practices. Using this approach we identified 140 providers (137 physicians and 3 nurse practitioners). We invited only providers caring for 50 or more patients to participate (n = 29, 27 physicians and 2 nurse practitioners). Of these, 22 (76%, including 20 physicians and 2 nurse practitioners) agreed to participate. These 22 providers practiced at 11 different sites including academic teaching hospitals (n = 5), community hospitals (n = 2), community health centers (n = 2), and public hospitals (1 state hospital and 1 city hospital).
All patients in participating providers' practices who providers believed had normal cognitive function and could read English were eligible. At 9 sites patients were asked to participate through their physicians' office. Of 1,213 invited patients, 744 (61.3%) agreed to participate. Of these 744 participants, 620 (83.3%) returned questionnaires. All study protocols were approved by Institutional Review Boards at each of the study sites.
Data Collection
Data on adherence, interpersonal care, and sociodemographic characteristics were collected by patient surveys done between January 1999 and December 1999. Viral loads and CD4 counts were determined by medical record review.
Study Measures
Adherence
Adherence to antiretroviral therapy was the dependent variable. We conducted cognitive testing of several approaches to the assessment of self-reported adherence. After consultation with national adherence experts, we tested an interviewer-administered approach that was being used by many groups, including the AIDS Clinical Trials Group, which asked patients about each dose of each medicine on each of the last 3 days. Most patients could accomplish this complicated reporting task with the help of an interviewer, but the approach failed when we tried to adapt it to the pencil-and-paper format we needed for a mailed survey. We therefore opted to ask more global questions about antiretroviral adherence. Patients also reported in cognitive tests that it was easier to respond to questions with Likert-type response options than to questions that asked about percentages of doses skipped. We asked participants who were using antiretroviral medications 4 questions. The first 3 questions asked patients “During the past 4 weeks, how often did you do each of the following: make small changes from the antiretroviral drugs your doctor prescribed, make major changes from the antiretroviral drugs your doctor prescribed, or stop taking one or more of your antiretroviral medications because of side effects.” Response options were: many times, sometimes, a few times, or not at all. The fourth question asked “How often during the last 7 days were you able to take your antiretroviral medications exactly as your doctor or nurse told you?” Response options were: none of the time, a little of the time, some of the time, most of the time, and all of the time.
Confirmatory factor analysis using principal components confirmed that these 4 adherence items could be aggregated. To create an aggregate adherence score, we transformed each item linearly into a 0 to 100 scale (with 100 representing perfect adherence) and computed the mean of the nonmissing items. If 2 or more of the 4 items were missing, the score was considered missing. The Cronbach's α for the scale was 0.72. To assess item acceptability, we examined rates of missing responses. To validate this adherence measure we examined the relationship between the adherence score and viral loads. We used only cases when there was a viral load within 3 months of the adherence report (n = 392). We grouped the adherence score in clinically relevant groups as 0 to 60 (9.2%), 61 to 90 (25.9%), 91 to 99 (21.6%), and 100 (43.3%), and classified viral loads as detectable versus nondetectable. The strength of the relationship was tested using the χ2 test.
Quality of Physician-Patient Relationships
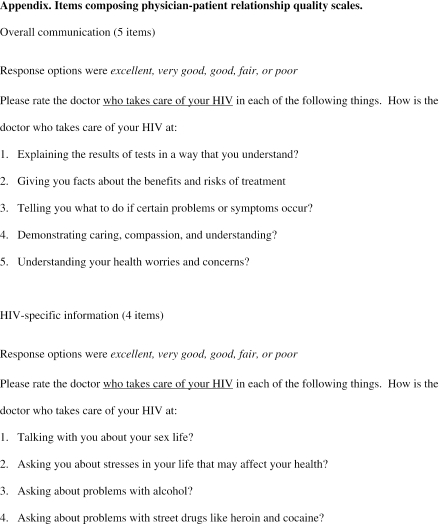
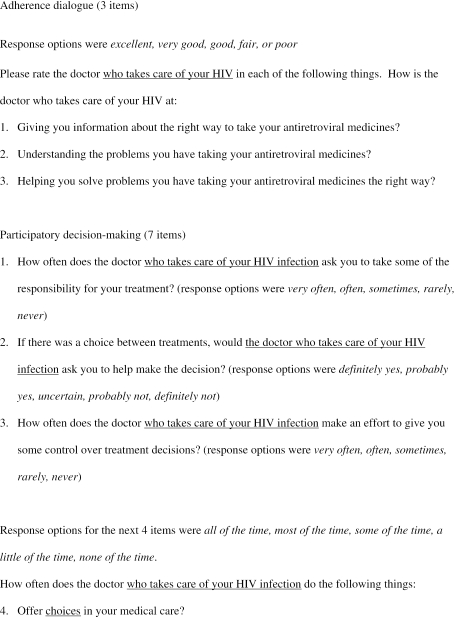
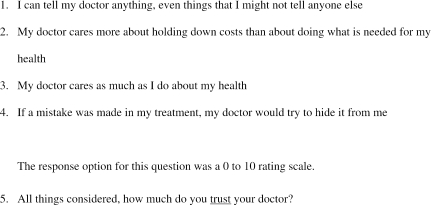
We used 6 previously tested multi-item scales to assess the quality of specific dimensions of the physician-patient relationship: general communication,27 provision of HIV-specific information,27 egalitarian decision-making style,28 overall satisfaction with care,30 willingness to recommend the physician to others,30 and trust in the physician (see Appendix available online at http://www.jgim.org).31 In addition, we developed a new scale for this study that assessed the quality adherence dialogue. Patients were asked, “How is the doctor who takes care of your HIV at: giving you information about the right way to take your antiretroviral medicines, understanding the problems that you have taking your antiretroviral medicines, and helping you solve problems you have taking your antiretroviral medicines the right way.” Response options were: excellent, very good, good, fair, or poor. Confirmatory factor analysis using principal components was used to verify that these items could be aggregated into a scale, and Cronbach's αs were determined.
Covariates
We assessed variables with demonstrated prior relationships to the quality of physician-patient relationships and adherence, including gender, race (white, African American, Hispanic, other), educational level, age, sexual orientation, unstable housing, history of injection drug use, and health insurance. To assess health status, we used the physical component score (PCS) and the mental component score (MCS) from the HIV Costs, Services, and Utilization Study developed by Hays et al.32 To assess beliefs about antiretroviral therapy, we asked patients how necessary it would be to take antiretroviral medications to get “the best quality HIV care,” with 5 response options ranging from very necessary to not at all necessary. For analyses, we dichotomized the scale between very necessary and quite necessary. We also examined the effects of other potential confounders, including the number of pills taken per day, the duration of physician-patient relationship, and whether patients had AIDS.
Statistical Analysis
Of the 620 survey respondents, 552 were using antiretrovirals and had a nonmissing adherence score, and constituted the analytic sample. The patient was the unit of analysis. To examine the bivariate relationships of independent variables and covariates to adherence, we used the Wilcoxon rank sum or Kruskal-Wallis tests for categorical variables and Spearman correlation coefficients for continuous variables. For race, we used analysis of variance to determine mean adherence scores for each racial group, but we used the Kruskal-Wallis test to determine whether differences between the groups were statistically significant.
To model the relationship between each of the physician-patient relationship quality scales and adherence we used multiple ordinal logistic regression. We categorized adherence into 20 levels, with each level representing an equal increment of 5 points in the original 100-point score. This approach insured the comparability of odds ratios between models. We used Hausman specification tests to verify the proportional odds assumption.33,34 We considered using linear regression for this analysis, but our analysis of the residuals from linear models showed considerable heteroskedasticity, making linear regression inappropriate. We also considered logistic regression, but did not believe it was appropriate to dichotomize our data at any particular point. For example, dichotomizing at 95 treats people with scores of 94, 50, and 20 as identical, which we do not believe is clinically correct.
Using separate multiple ordinal logistic regression, we analyzed the multivariable relationship of each of the 7 measures of interpersonal care to adherence. Covariates related to adherence at P values of .10 or less included age, gender, education, beliefs about antiretroviral therapy, MCS, and PCS, and these variables were included in all regression models. We transformed the odds ratios to represent a 10-point change in each of the physician-patient relationship quality scales. All multivariable models were adjusted for physician-level clustering. All analyses were conducted using Stata 7.0 (Stata Corporation, College Station, Tex).
To highlight the relative importance of physician-patient relationship quality variables, we determined the percent increment in variance in adherence explained by each physician-patient relationship quality variable, and compared it to the percent increment in variance explained by the mental health summary variable (MCS). We calculated the percent increment in variance explained as ([pseudo R2 of full model—pseudo R2 of model excluding the variable of interest] / pseudo R2 of the full model). We chose the MCS variable as a reference variable because it had the highest percent increment in the pseudo R2 in 6 of the 7 models (the one exception being the adherence dialogue model, in which adherence dialogue had a higher percent increment in pseudo R2).
RESULTS
Patient Characteristics
Participating physicians (n = 22) included 8 generalist physicians, 10 physicians with infectious disease training, 2 physicians with hematology-oncology training, and 2 nurse practitioners. Patient characteristics are shown in Table 1. The mean patient age was 42 years, 15% were women, 27% were nonwhite, and 88% had completed high school. Eighty-seven percent felt that antiretroviral therapy was important, and 70% of patients had been cared for by their current physician for more than 2 years. The mean physical and mental health component scores were 52.1 and 51.4, respectively. For reference, the mean PCS scores of patients nationally with Stage A, B, and C disease are 59, 52, and 46, respectively.32 The mean CD4 count was 432 cells/mm3 and 43% had nondetectable viral loads.
Table 1.
Patient Characteristics (N = 554)
| Characteristic | |
|---|---|
| Sociodemographic characteristics | |
| Mean age, y (SD) | 41.6 (7.7) |
| Female, % | 15.2 |
| Race, % | |
| White | 73.2 |
| African American | 14.5 |
| Hispanic | 6.9 |
| Other | 5.4 |
| High school graduates, % | 88.2 |
| HIV risk factor, % | |
| Male-to-male sexual contact only | 57.4 |
| Male-to-female sexual contact only | 6.0 |
| IDU only | 8.5 |
| Other (including combinations of risk factors) | 28.0 |
| No health insurance, % | 11.7 |
| Homeless/temporary housing, % | 5.5 |
| Duration of physician-patient relationship > 2 years, % | 70.0 |
| Beliefs about antiretroviral therapy | |
| Believes antiretroviral therapy is “very important,”% | 87.2 |
| Clinical characteristics | |
| Mean number of pills per day (SD) | 18.5 (10.1) |
| Mean physical health (SD) | 52.1 (8.3) |
| Mean mental health (SD) | 51.4 (8.9) |
| Mean CD4 cell count (cells/mm3) (SD) | 432 (264) |
| Viral load, % nondetectable | 43.4 |
Here we present viral load results only for patients who had a viral load <3 months before the study visit (n = 392). Viral loads were done in numerous laboratories, with no consistent definition of “nondetectable.” In most the definition was <50 copies/ml, but in some it was <400 copies/ml.
SD, standard deviation, IDU, injection drug use.
Mean physician-patient relationship quality scores ranged from 75 (HIV-specific information; Table 2) to 94 (willingness to recommend). The overall satisfaction and willingness to recommend scales were positively skewed, with 65.9% and 75.5% of participants scoring at the ceiling. With the exception of the trust scale (Cronbach's α= 0.71), all other scales had αs of 0.8 or greater.
Table 2.
Measures of Physician-Patient Relationship Quality and Adherence
| Percentiles | |||||||
|---|---|---|---|---|---|---|---|
| Measure | Items (#) | Cronbach's α | 25th | 50th | 75th | Mean (SD) | % at Ceiling |
| General communication | 5 | 0.93 | 75 | 95 | 100 | 86.9 (18.4) | 49.8 |
| HIV-specific information | 4 | 0.93 | 56.3 | 81.3 | 100 | 75.5 (26.7) | 38.9 |
| Participatory decision making | 7 | 0.86 | 71.4 | 85.7 | 96.4 | 81.5 (18.8) | 20.4 |
| Overall satisfaction | 4 | 0.92 | 87.5 | 100 | 100 | 91.9 (15.0) | 65.9 |
| Willingness to recommend | 2 | 0.81 | 100 | 100 | 100 | 93.6 (14.9) | 75.5 |
| Physician trust | 5 | 0.71 | 76 | 86 | 98 | 84.8 (13.9) | 24.7 |
| Adherence dialogue | 3 | 0.93 | 89 | 100 | 100 | 86.6 (19.6) | 57.0 |
| Adherence | 4 | 0.75 | 85.4 | 93.8 | 100 | 87.2 (18.6) | 43.3 |
SD, standard deviation.
Self-reported adherence in this sample was high, with a mean adherence score of 87 on a 0 to 100 scale (α= 0.75). Perfect adherence was reported by 43% of participants. The percent of patients with undetectable viral loads in adherence score groups of 1 to 60, 61 to 90, 91 to 99, and 100 were 21.1%, 40.0%, 48.4%, and 48.8%, respectively (P = .003 by χ2 test).
Bivariate Analyses
In bivariate analyses (Table 3), all 7 measures of interpersonal care were significantly associated with adherence, with Spearman correlation coefficients ranging from 0.13 (participatory decision-making style) to 0.21 (adherence dialogue). Patients with better physical health (r = .12, P = .007) and better mental health (r = .20, P < .0001) reported better adherence. Older patients reported better adherence (r = .15, P = .0004), and men reported somewhat better adherence than women (88.2 vs. 82.1, P = .03). Those who believed that antiretroviral therapy was important had better adherence than those who did not (88.6 vs. 79.6, P < .002). Race was not associated with adherence (P = .38).
Table 3.
Bivariate Relationships Between Adherence and Selected Covariates
| Variable | Correlation | Mean Adherence Score | P Value |
|---|---|---|---|
| Physician-patient relationship quality | |||
| General communication | 0.17 | — | <.0001 |
| HIV-specific information | 0.15 | — | .002 |
| Participatory decision making | 0.14 | — | .002 |
| Overall physician satisfaction | 0.17 | — | <.0001 |
| Willingness to recommend | 0.13 | — | .002 |
| Physician trust | 0.16 | — | .0002 |
| Adherence dialogue | 0.21 | — | <.0001 |
| Patient characteristics | |||
| Physical health | 0.12 | — | .007 |
| Mental health | 0.20 | — | <.0001 |
| Age, y | 0.15 | — | .0004 |
| Education* | 0.08 | .07 | |
| Gender | .03† | ||
| Male | 88.2 | ||
| Female | 82.1 | ||
| Beliefs about antiretroviral therapy, % | 0.002† | ||
| Important | 88.6 | ||
| Not important | 79.6 | ||
| Race | 0.37‡ | ||
| White | 88.3 | ||
| African American | 83.7 | ||
| Hispanic | 83.9 | ||
| Other | 87.2 |
Number of years of education was treated as a continuous variable.
P values are based on Wilcoxon rank-sum test.
The mean values are from an analysis of variance. The P value is from a Kruskal-Wallis test.
Multivariable Analyses
The results of the multiple ordinal logistic regression models are shown in Table 4. The odds ratios (ORs) in the table represent the odds of changing by 1 level in the 20-level ordinal adherence variable for each unit change in the independent variable. For the 7 interpersonal care variables (each of which used a 100-point scale), the OR represents a 10-point change in the independent variable. For general communication, the OR was 1.15 (P = .0001). That is, for each 10-point improvement in general communication, the odds of improving adherence by 1 level were increased by 15%. Similarly, HIV-specific information (OR, 1.09, P = .02), overall physician satisfaction (OR, 1.14, P = .004), willingness to recommend (OR, 1.09, P = .009), trust (OR, 1.10, P = .03), and adherence dialogue (OR, 1.20, P < .0001) were all significantly and independently associated with adherence. Participatory decision-making style (OR, 1.7, P = .11) showed a trend toward statistical significance.
Table 4.
Multivariable Relationship of Measures of Physician-Patient Relationship Quality to Adherence, Adjusted for Age, Gender, Education, Race, Physical Health, and Mental Health
| Physician-Patient Relationship Quality Measure | Odds Ratio* | 95% CI | P Value |
|---|---|---|---|
| General communication | 1.15 | 1.07 to 1.23 | .0001 |
| HIV-specific information | 1.09 | 1.01 to 1.16 | .02 |
| Participatory decision making | 1.07 | 0.99 to 1.15 | .12 |
| Overall physician satisfaction | 1.14 | 1.04 to 1.25 | .004 |
| Willingness to recommend physician | 1.09 | 1.02 to 1.15 | .009 |
| Physician trust | 1.10 | 1.01 to 1.21 | .03 |
| Adherence dialogue | 1.20 | 1.10 to 1.30 | <.0001 |
The 0 to 100 adherence variable was transformed into 20 equal ordinal categories of 5 points each for modeling. The odds ratio is therefore the odds of a 5-point change in adherence for a unit change in the independent variable. For each of the interpersonal care variables a unit change is 10 points on the 0- to 100-point scale.
Those who believed that it was important to take antiretroviral medications to get the best quality HIV care had better adherence in every model (ORs from 1.73 to 2.24, P < .05). Older patients had somewhat better adherence, with an OR for a 1-year increment in age in each model 1.04 (P < .01). That is, for each year of increasing age, the odds of improving adherence by 1 level were increased by 4%. Similarly, mental health was strongly associated with adherence (ORs for each 1-point increment in health 1.04 to 1.05, P < .001). Gender, education, race, and PCS were not associated with adherence.
The percent increment in explained variance associated with the MCS variable ranged from 16% to 19% in the 7 multivariable models. By comparison, the percent increment in explained variance associated with each of the physician-patient relationship quality variables was as follows: general communication (15%), HIV-specific information (10%), participatory decision making (4%), overall physician satisfaction (11%), willingness to recommend (4%), physician trust (4%), and adherence dialogue (25%).
DISCUSSION
We assessed 7 different measures of interpersonal care, and 6 of the 7 were independently associated with our measure of adherence. Of these, 4 (general communication, overall satisfaction, willingness to recommend, and physician trust) were generic measures; that is, they were developed for use in general patient populations. One (HIV-specific communication) was a condition-specific scale that focused on physician-patient communication about sexual behaviors and substance abuse. And 1 (adherence dialogue) focused more specifically on how physicians communicate with their patients about antiretroviral medications. The consistency of our findings across these different scales supports the assertion that better physician-patient relationships and physician-patient communication produce better adherence with antiretroviral therapies.
The magnitude of the relationships between these physician-patient relationship quality measures and antiretroviral medication adherence can be appreciated both through the relatively low correlation coefficients seen in bivariate tests (between 0.13 and 0.21), and through the odds ratios in the final models, which ranged from 1.08 to 1.20. Adherence with antiretrovirals is a highly complex behavior, and it has been difficult for researchers to find variables that are strongly and consistently related to adherence. Because of this, it is particularly important that providers understand every potentially modifiable risk factor for poor adherence. Although the relationship between these physician-patient relationship quality variables and adherence is only of moderate strength, for several of the variables the magnitude of the relationship was similar to that of mental health, the variable that in this analysis was most consistently and strongly associated with adherence.
How mutable or modifiable are physician-patient relationships? Studies from several clinical specialties, including general medicine,19,23,26,35–37 gynecology,21 pediatrics,22 oncology, and rehabilitation medicine24 suggest that both trainees and those who have finished training can be taught to behave in ways that are more patient centered. There is also good evidence that the improvements engendered by such training persist over time.38–40 However, no studies of which we are aware have directly examined whether such training improves medication adherence.
patients' beliefs about antiretroviral therapy were also statistically significantly associated with adherence in multivariate regression modeling. Our findings are consistent with those of others who have studied the relationship between patient beliefs and adherence in HIV10,11,41–43 or in other diseases.44 Trying to understand whether patients believe that taking antiretroviral medications will help them, and attempting to educate patients on the benefits and risks of highly active antiretroviral therapy, may improve adherence.
Consistent with previous data,5,14,45,46 we found that better mental health was associated with better adherence. Mental health problems are common in HIV disease,47–51 cause considerable morbidity,51 are highly treatable,52–54 and are often not detected by physicians.55–58 Our findings are another reminder to clinicians to be vigilant for symptoms of depression and other mental disorders in their patients with HIV.
This study had several important methodological strengths. We studied a diverse sample of persons with HIV cared for at 11 different care sites in a metropolitan area, and used multiple validated measures of interpersonal care. Nonetheless there were several relevant study limitations. First, we assessed adherence by report, and may have overestimated adherence rates.45,59 In addition, we used a Likert scale for adherence that cannot be directly translated into percent of prescribed doses taken or therapeutic coverage. However, this is a weakness of any self-report measure of adherence.
Second, it is theoretically possible that self-reports of adherence and patients' assessments of physician-patient relationship quality are both manifestations of a global positive or negative attitude that patients have about their physician and medical care, rather than truly independent measures. Future analyses of the association between physician-patient relationship quality and adherence would benefit from the use of an objective measure of adherence such as MEMS (Medication Event Monitoring System). Third, the generalizability of our findings may be limited by several factors. Because most of our respondents were contacted by mail, we suspect the types of nonresponse bias that are usually seen in mailed surveys,60,61 including fewer responses from nonwhites and those with low incomes, unstable housing, or active substance abuse. For example, only 8.5% of our patients reported injection drug use as their primary HIV risk factor. In addition, we sampled patients from practices of experienced HIV providers in one metropolitan area. However, national data suggest the most patients with HIV in this country are cared for by providers and in sites that have HIV expertise.62
Finally, although no cross-sectional study can unequivocally establish the direction of causal effects, it is unlikely that the direction of the causal relationships between physician-patient relationship quality and adherence was the reverse of that proposed. That is, it is unlikely that patients' reported adherence affects reports of physician-patient relationship quality. Whether improving physician-patient relationship quality can improve adherence can only be definitively addressed by an intervention trial. It is important to note, however, that intervention trials have clearly shown that improving physician-patient communication can result in better health outcomes.63–65 Our findings support the assertion that better adherence may have mediated these effects.
Few clinicians and even fewer researchers are familiar with the methods used to measure the quality of physician-patient relationships and to measure medication adherence. Our regression models describe how an increment of improvement in physician-patient relationship quality is associated with an increment of improvement in self-reported adherence, which we appreciate is not intuitive. However, these measurement and interpretation challenges are inherent in this field of research. The goal of this research was not to rigorously calibrate this relationship, but rather to present an empirical proof of the principal that higher quality physician-patient relationships are associated with better medication adherence. Because our results were both consistent across measures of physician-patient relationship quality and statistically significant, we believe that we have achieved this proof of principal.
This study shows that multiple dimensions of the physician-patient relationship are associated with medication adherence in persons with HIV infection. The observation that physicians can be trained to interact more effectively with their patients suggests that physician-patient relationship quality is a potentially important point of intervention for efforts to improve patients' medication adherence. In addition, our data suggest that it is critical to investigate and incorporate patients' belief systems about antiretroviral therapy into adherence discussions, and to identify and treat mental disorders.
Acknowledgments
This study was supported by the Robert Wood Johnson Foundation and the Lifespan/Tufts/Brown Center for AIDS Research (P30 AI42853). Dr. Schneider was funded by a grant from the General Clinical Research Center under grant M01-RR00054.
Appendix
REFERENCES
- 1.Becker MH. Patient adherence to prescribed therapies. Med Care. 1985;23:539–55. doi: 10.1097/00005650-198505000-00014. [DOI] [PubMed] [Google Scholar]
- 2.Lerner BH, Gulick RM, Dubler NN. Rethinking nonadherence: historical perspectives on triple-drug therapy for HIV disease. Ann Intern Med. 1998;129:573–8. doi: 10.7326/0003-4819-129-7-199810010-00012. [DOI] [PubMed] [Google Scholar]
- 3.Friedland GH, Williams A. Attaining higher goals in HIV treatment: the central importance of adherence. AIDS. 1999;13(suppl 1):S61–S72. [PubMed] [Google Scholar]
- 4.Mehta S, Moore RD, Graham NM. Potential factors affecting adherence with HIV therapy. AIDS. 1997;11:1665–70. doi: 10.1097/00002030-199714000-00002. Editorial. [DOI] [PubMed] [Google Scholar]
- 5.Holzemer WL, Corless IB, Nokes KM, et al. Predictors of self-reported adherence in persons living with HIV disease. AIDS Patient Care STDS. 1999;13:185–97. doi: 10.1089/apc.1999.13.185. [DOI] [PubMed] [Google Scholar]
- 6.Murphy DA, Roberts KJ, Martin DJ, Marelich W, Hoffman D. Barriers to antiretroviral adherence among HIV-infected adults. AIDS Patient Care STDS. 2000;14:47–58. doi: 10.1089/108729100318127. [DOI] [PubMed] [Google Scholar]
- 7.Laws MB, Wilson IB, Bowser DM, Kerr SE. Taking antiretroviral therapy for HIV infection: learning from patients' stories. J Gen Intern Med. 2000;15:848–58. doi: 10.1046/j.1525-1497.2000.90732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murphy DA, Roberts KJ, Hoffman D, Molina A, Lu MC. Barriers and successful strategies to antiretroviral adherence among HIV-infected monolingual Spanish-speaking patients. AIDS Care. 2003;15:217–30. doi: 10.1080/0954012031000068362. [DOI] [PubMed] [Google Scholar]
- 9.Malcolm SE, Ng JJ, Rosen RK, Stone VE. An examination of HIV/AIDS patients who have excellent adherence to HAART. AIDS Care. 2003;15:251–61. doi: 10.1080/0954012031000068399. [DOI] [PubMed] [Google Scholar]
- 10.Mostashari F, Riley E, Selwyn PA, Altice FL. Acceptance and adherence with antiretroviral therapy among HIV-infected women in a correctional facility. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;18:341–8. doi: 10.1097/00042560-199808010-00005. [DOI] [PubMed] [Google Scholar]
- 11.Altice FL, Mostashari F, Friedland GH. Trust and the acceptance of and adherence to antiretroviral therapy. J Acquir Immune Defic Syndr. 2001;28:47–58. doi: 10.1097/00042560-200109010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Bakken S, Holzemer WL, Brown MA, et al. Relationships between perception of engagement with health care provider and demographic characteristics, health status, and adherence to therapeutic regimen in persons with HIV/AIDS. AIDS Patient Care STDS. 2000;14:189–97. doi: 10.1089/108729100317795. [DOI] [PubMed] [Google Scholar]
- 13.Vincke J, Bolton R. Therapy adherence and highly active antiretroviral therapy: comparison of three sources of information. AIDS Patient Care STDS. 2002;16:487–95. doi: 10.1089/10872910260351267. [DOI] [PubMed] [Google Scholar]
- 14.Gordillo V, del Amo J, Soriano V, Gonzalez-Lahoz J. Sociodemographic and psychological variables influencing adherence to antiretroviral therapy. AIDS. 1999;13:1763–9. doi: 10.1097/00002030-199909100-00021. [DOI] [PubMed] [Google Scholar]
- 15.Golin CE, Liu H, Hays RD, et al. A prospective study of predictors of adherence to combination antiretroviral medication. J Gen Intern Med. 2002;17:756–65. doi: 10.1046/j.1525-1497.2002.11214.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roter DL, Hall JA. Doctors Talking with PatientsPatients Talking with Doctors. Westport, Conn: Auburn House; 1992. [Google Scholar]
- 17.Gordon GH, Rost K. Evaluating a faculty development course on medical interviewing. In: Lipkin M Jr, Putnam SM, Lazare A, editors. The Medical Interview: Clinical Care, Education, and Research. New York, NY: Springer-Varlag; 1995. pp. 436–47. [Google Scholar]
- 18.Thompson TL, Parrott R. Interpersonal communication and health. In: Knapp ML, Daly JA, editors. Handbook of Interpersonal Communication. Thousand Oaks, Calif: Sage Publications; 2002. pp. 680–725. [Google Scholar]
- 19.Roter DL, Cole KA, Kern DE, Barker LR, Grayson M. An evaluation of residency training in interviewing skills and the psychosocial domain of medical practice. J Gen Intern Med. 1990;5:347–54. doi: 10.1007/BF02600404. [DOI] [PubMed] [Google Scholar]
- 20.Levinson W, Roter D. The effects of two continuing medical education programs on communication skills of practicing primary care physicians. J Gen Intern Med. 1993;8:318–24. doi: 10.1007/BF02600146. [DOI] [PubMed] [Google Scholar]
- 21.van Dulmen AM, van Weert JC. Effects of gynaecological education on interpersonal communication skills. BJOG. 2001;108:485–91. doi: 10.1111/j.1471-0528.2001.00104.x. [DOI] [PubMed] [Google Scholar]
- 22.van Dulmen AM, Holl RA. Effects of continuing paediatric education in interpersonal communication skills. Eur J Pediatr. 2000;159:489–95. doi: 10.1007/s004310051316. [DOI] [PubMed] [Google Scholar]
- 23.Moral RR, Alamo MM, Jurado MA, de Torres LP. Effectiveness of a learner-centred training programme for primary care physicians in using a patient-centred consultation style. Fam Pract. 2001;18:60–3. doi: 10.1093/fampra/18.1.60. [DOI] [PubMed] [Google Scholar]
- 24.Sliwa JA, Makoul G, Betts H. Rehabilitation-specific communication skills training: improving the physician-patient relationship. Am J Phys Med Rehabil. 2002;81:126–32. doi: 10.1097/00002060-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Hulsman RL, Ros WJ, Winnubst JA, Bensing JM. The effectiveness of a computer-assisted instruction programme on communication skills of medical specialists in oncology. Med Educ. 2002;36:125–34. doi: 10.1046/j.1365-2923.2002.01074.x. [DOI] [PubMed] [Google Scholar]
- 26.Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians' interviewing skills and reducing patients' emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155:1877–84. [PubMed] [Google Scholar]
- 27.Wilson IB, Kaplan S. Physician-patient communication in HIV disease: the importance of patient, physician, and visit characteristics. J Acquir Immune Defic Syndr. 2000;25:417–25. doi: 10.1097/00042560-200012150-00006. [DOI] [PubMed] [Google Scholar]
- 28.Kaplan SH, Gandek B, Greenfield S, Rogers W, Ware JE. Patient and visit characteristics related to physicians' participatory decision-making style. Results from the Medical Outcomes Study. Med Care. 1995;33:1176–87. doi: 10.1097/00005650-199512000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Dukes KA, Kaplan SH, Sullivan RA, Silliman RA, D'Agostino RB, Greenfield S. The differential effect of physicians' egalitarian decision-making style on the health outcomes of women with type II diabetes. J Gen Intern Med. 1994;9:51. [Google Scholar]
- 30.Davies AR, Ware JE. GHAA's Consumer Satisfaction Survey and User's Manual. 2nd ed. Washington, DC: GHAA; 1991. [Google Scholar]
- 31.Safran DG, Kosinski M, Tarlov AR, et al. The Primary Care Assessment Survey: tests of data quality and measurement performance. Med Care. 1998;36:728–39. doi: 10.1097/00005650-199805000-00012. [DOI] [PubMed] [Google Scholar]
- 32.Hays RD, Cunningham WE, Sherbourne CD, et al. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV cost and services utilization study. Am J Med. 2000;108:714–22. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 33.Hausman J. Specification tests in econometrics. Econometrica. 1984;52:1219–40. [Google Scholar]
- 34.Hausman J. Specification tests in economics. Econometrica. 1978;46:1251–71. [Google Scholar]
- 35.Joos SK, Hickam DH, Gordon GH, Baker LH. Effects of a physician communication intervention on patient care outcomes. J Gen Intern Med. 1996;11:147–55. doi: 10.1007/BF02600266. [DOI] [PubMed] [Google Scholar]
- 36.Roter D, Rosenbaum J, de Negri B, Renaud D, DiPrete-Brown L, Hernandez O. The effects of a continuing medical education programme in interpersonal communication skills on doctor practice and patient satisfaction in Trinidad and Tobago. Med Educ. 1998;32:181–9. doi: 10.1046/j.1365-2923.1998.00196.x. [DOI] [PubMed] [Google Scholar]
- 37.Brown JB, Boles M, Mullooly JP, Levinson W. Effect of clinician communication skills training on patient satisfaction. A randomized, controlled trial. Ann Intern Med. 1999;131:822–9. doi: 10.7326/0003-4819-131-11-199912070-00004. [DOI] [PubMed] [Google Scholar]
- 38.Stillman PL, Sabers DL, Redfield DL. Use of trained mothers to teach interviewing skills to first-year medical students: a follow-up study. Pediatrics. 1977;60:165–9. [PubMed] [Google Scholar]
- 39.Maguire P, Fairbairn S, Fletcher C. Consultation skills of young doctors: I—Benefits of feedback training in interviewing as students persist. Br Med J (Clin Res Ed) 1986;292:1573–6. doi: 10.1136/bmj.292.6535.1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bowman FM, Goldberg DP, Millar T, Gask L, McGrath G. Improving the skills of established general practitioners: the long-term benefits of group teaching. Med Educ. 1992;26:63–8. doi: 10.1111/j.1365-2923.1992.tb00125.x. [DOI] [PubMed] [Google Scholar]
- 41.Smith MY, Rapkin BD, Morrison A, Kammerman S. Zidovudine adherence in persons with AIDS. The relation of patient beliefs about medication to self-termination of therapy. J Gen Intern Med. 1997;12:216–23. doi: 10.1046/j.1525-1497.1997.012004216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stone VE, Clarke J, Lovell J, et al. HIV/AIDS patients' perspectives on adhering to regimens containing protease inhibitors. J Gen Intern Med. 1998;13:586–93. doi: 10.1046/j.1525-1497.1998.00180.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Laws MB, Wilson IB, Bowser DM, Kerr SE. Taking antiretroviral therapy for HIV infection: learning from patients' stories. J Gen Intern Med. 2000;15:848–58. doi: 10.1046/j.1525-1497.2000.90732.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horne R, Weinman J. patients' beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res. 1999;47:555–67. doi: 10.1016/s0022-3999(99)00057-4. [DOI] [PubMed] [Google Scholar]
- 45.Paterson DL, Swindells S, Mohr J, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- 46.Singh N, Squier C, Sivek C, Nguyen MH, Wagener M, Yu VL. Determinants of nontraditional therapy use in patients with HIV infection. A prospective study. Arch Intern Med. 1996;156:197–201. [PubMed] [Google Scholar]
- 47.Holland JC, Tross S. The psychosocial and neuropsychiatric sequelae of the acquired immune deficiency syndrome and related disorders. Ann Intern Med. 1985;103:760–4. doi: 10.7326/0003-4819-103-5-760. [DOI] [PubMed] [Google Scholar]
- 48.Perry S. HIV-related depression. In: Price R, Perry S, editors. HIV, AIDS, and the Brain. New York, NY: Raven Press; 1993. pp. 233–8. [Google Scholar]
- 49.Lyketsos CG, Hutton H, Fishman M, Schwartz J, Treisman GJ. Psychiatric morbidity on entry to an HIV primary care clinic. AIDS. 1996;10:1033–9. doi: 10.1097/00002030-199610090-00015. [DOI] [PubMed] [Google Scholar]
- 50.Lyketsos CG, Federman EB. Psychiatric disorders and HIV infection: impact on one another. Epidemiol Rev. 1995;17:152–64. doi: 10.1093/oxfordjournals.epirev.a036171. [DOI] [PubMed] [Google Scholar]
- 51.Sherbourne CD, Hays RD, Fleishman JA, et al. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. Am J Psychiatry. 2000;157:248–54. doi: 10.1176/appi.ajp.157.2.248. [DOI] [PubMed] [Google Scholar]
- 52.Markowitz JC, Kocsis JH, Fishman B, et al. Treatment of depressive symptoms in human immunodeficiency virus-positive patients. Arch Gen Psychiatry. 1998;55:452–7. doi: 10.1001/archpsyc.55.5.452. [DOI] [PubMed] [Google Scholar]
- 53.Rabkin JG, Wagner GJ, Rabkin R. Fluoxetine treatment for depression in patients with HIV and AIDS: a randomized, placebo-controlled trial. Am J Psychiatry. 1999;156:101–7. doi: 10.1176/ajp.156.1.101. [DOI] [PubMed] [Google Scholar]
- 54.Zisook S, Peterkin J, Goggin KJ, Sledge P, Atkinson JH, Grant I. Treatment of major depression in HIV-seropositive men. HIV Neurobehavioral Research Center Group. J Clin Psychiatry. 1998;59:217–24. doi: 10.4088/jcp.v59n0502. [DOI] [PubMed] [Google Scholar]
- 55.Nielson AC, Williams TA. Depression in ambulatory medical patients: prevalence by self-report questionnaire and recognition by nonpsychiatric physicians. Arch Gen Psych. 1980;37:999–1004. doi: 10.1001/archpsyc.1980.01780220037003. [DOI] [PubMed] [Google Scholar]
- 56.Seller RH, Blascovich J, Lenkei E. Influence of stereotypes in the diagnosis of depression by family practice residents. J Fam Pract. 1981;12:849–54. [PubMed] [Google Scholar]
- 57.Goldberg D, Steele JJ, Johnson A, Smith C. Ability of primary care physicians to make accurate ratings of psychiatric symptoms. Arch Gen Psych. 1982;39:829–33. doi: 10.1001/archpsyc.1982.04290070059011. [DOI] [PubMed] [Google Scholar]
- 58.Kessler LG, Cleary PD, Burke JD. Psychiatric disorders in primary care: results of a follow-up study. Arch Gen Psych. 1985;42:583–7. doi: 10.1001/archpsyc.1985.01790290065007. [DOI] [PubMed] [Google Scholar]
- 59.Liu H, Golin CE, Miller LG, et al. A comparison study of multiple measures of adherence to HIV protease inhibitors. Ann Intern Med. 2001;134:968–77. doi: 10.7326/0003-4819-134-10-200105150-00011. [DOI] [PubMed] [Google Scholar]
- 60.Zaslavsky AM, Zaborski LB, Cleary PD. Factors affecting response rates to the Consumer Assessment of Health Plans Study survey. Med Care. 2002;40:485–99. doi: 10.1097/00005650-200206000-00006. [DOI] [PubMed] [Google Scholar]
- 61.Etter JF, Perneger TV. Analysis of non-response bias in a mailed health survey. J Clin Epidemiol. 1997;50:1123–8. doi: 10.1016/s0895-4356(97)00166-2. [DOI] [PubMed] [Google Scholar]
- 62.Landon BE, Wilson IB, Wenger NS, et al. Specialty training and specialization among physicians who treat HIV/AIDS in the United States. J Gen Intern Med. 2002;17:12–22. doi: 10.1046/j.1525-1497.2002.10401.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Greenfield S, Kaplan S, Ware JE., Jr Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 64.Greenfield S, Kaplan SH, Ware JE, Yano EM, Frank HJL. patients' participation in medical care: effects on blood sugar control and quality of life in diabetes. J Gen Intern Med. 1988;3:448–57. doi: 10.1007/BF02595921. [DOI] [PubMed] [Google Scholar]
- 65.Kaplan SH, Greenfield S, Ware JE., Jr . Impact of the doctor-patient relationship on the outcomes of chronic disease. In: Stewart M, Roter D, editors. Communicating with Medical Patients. Newbury Park, Calif: Sage Publications; 1989. pp. 228–45. [Google Scholar]