Abstract
OBJECTIVE
To compare patients' and physicians' visit-specific satisfaction in an internal medicine outpatient setting, and to explain their respective views.
DESIGN
patients' and physicians' background characteristics were assessed prior to outpatient encounters. Immediately after the encounter, both patients and physicians completed a questionnaire assessing satisfaction with the visit.
SETTING
The outpatient division of an academic teaching hospital.
PARTICIPANTS
Thirty residents and specialists in general internal medicine, rheumatology, and gastroenterology, and 330 patients having a follow-up appointment with one of these physicians.
MEASUREMENTS AND MAIN RESULTS
patients' and physicians' visit-specific satisfaction was assessed using 5 Visual Analogue Scales (0 to 100). patients' overall satisfaction was higher than physicians' satisfaction (mean 81 vs. 66), and correlation of patients' and physicians' overall satisfaction with the specific visit was medium sized (r= .28, P < .001). patients' satisfaction ratings were associated with their previsit self-efficacy in communicating with their physician (P < .001) and with visiting a female physician (P < .01). Physicians' satisfaction was associated with patients' higher educational level (P < .05), primary language being Dutch (P < .001), better mental health (P < .05), and preference for receiving less than full information (P < .05).
CONCLUSIONS
In an outpatient setting, patients' visit-specific satisfaction ratings were substantially higher than, and only moderately associated with, physicians' ratings of the same visit. The dissimilar predictors explaining patients' and physicians' satisfaction suggest that patients and physicians form their opinion about a consultation in different ways. Hence, when evaluating outpatient encounters, physicians' satisfaction has additional value to patients' satisfaction in establishing quality of care.
Keywords: physician-patient relations, patient satisfaction, physician satisfaction, outpatients
In contemporary medicine, satisfaction is a widely used indicator of the quality of inpatient as well as outpatient care. In studies concerning quality of care, patient satisfaction is usually taken into account, while physicians' opinions are considered less often. Suchman et al.1 stated, though, that physician satisfaction offers important explanatory and evaluative insights into the patient-doctor relationship and the process of medical care. In addition, Fairhurst and May2 argue that “what is valuable about the consultation may be hidden from the patient (…).” Therefore, they suggest taking account also of the doctors' perspective on the interaction with their patients.
Although some studies have considered physicians' satisfaction with provided care,1,3–11 only a few have explicitly examined whether patients' and physicians' visit-specific satisfaction are congruent.12–15 The latter studies were conducted in general practice12–14 and an internal medicine outpatient clinic.15 In two studies,13,14 patients and physicians were both highly satisfied with the encounter, whereas in others, patients' satisfaction levels exceeded those of physicians.12,15 Even if both patients and doctors had high judgments on average, ratings were not necessarily correlated.13,14 In all but one study,12 however, questions for patients and physicians were not fully comparable.
The purpose of the current study was, first, to compare patients' and physicians' visit-specific satisfaction with the same consultation in an internal medicine outpatient setting. Second, we wanted to explain (dis)agreement by gaining insight into the factors predicting patients' and physicians' satisfaction.
The selection of predictors of satisfaction was mainly based on the literature on patient satisfaction,16–18 as few studies have investigated predictors of physicians' visit-specific satisfaction. Three types of predictors were considered. First, we looked at patient-related variables. Though studies show conflicting results, we hypothesized that satisfaction is associated with patient characteristics such as age and gender, educational level, ethnic background, and physical and mental health. Also, we included patients' preference for information, their preference for participation in decision making, and their self-efficacy (i.e., the confidence that one can successfully take appropriate and meaningful action) in communicating effectively with the physician. Second, we considered visit-specific characteristics. We hypothesized that the patient's acquaintance with the physician, waiting time before the consultation, and consultation length are possible predictors of satisfaction. In addition, the reason for this particular visit and the sequential number of the visit within the consultation schedule were taken into account. Third, associations between satisfaction and physician-related characteristics such as age and gender, physicians' professional attitudes toward patients, and perceptions of their ability to be communicatively responsive to their patients were explored.
METHODS
Design and Sample
This study took place at the outpatient division of an academic teaching hospital in Amsterdam, The Netherlands. All physicians working in the departments of general internal medicine, rheumatology, or gastroenterology were invited to participate between August 2001 and August 2002. Consecutive patients having a follow-up appointment with these physicians were contacted by letter 1 week prior to their scheduled appointment. Patients were eligible if they were able to speak, read, and write Dutch and were willing to provide written informed consent.
Participating physicians completed a baseline questionnaire on a single occasion, assessing their background characteristics. Participating patients were asked to complete a baseline questionnaire prior to the encounter. Immediately after the encounter both patients and physicians completed a short questionnaire. As we recruited patients who shared the same physician, assessments of patients were interdependent. This can be accounted for through multilevel analyses, which require at least 30 physicians to reliably estimate physician-related characteristics.19 Considering the number of predictors to be used, our aim was to recruit 10 patients per physician, resulting in a total of 300 cases.
Measures
Satisfaction
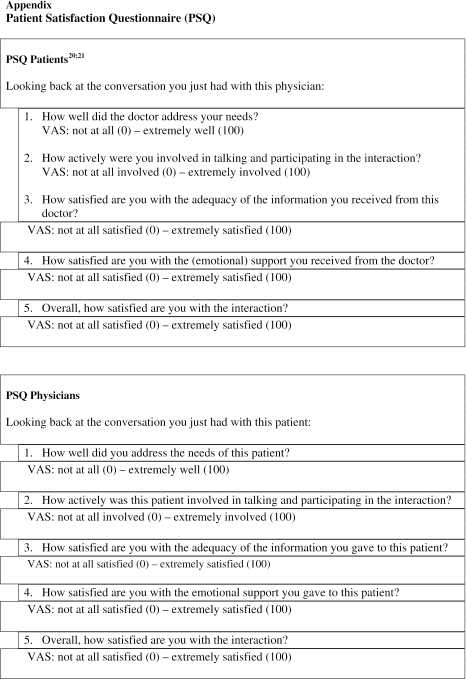
The Patient Satisfaction Questionnaire (PSQ)20,21 was used to measure patients' satisfaction following the consultation. It consists of 5 items measuring patients' satisfaction with 1) the way their needs were addressed, 2) their active involvement in the interaction, 3) information received, 4) emotional support received, and 5) the interaction in general. Answers were given on Visual Analogue Scales (VAS) ranging from 0 to 100 (see Appendix available online at http://www.jgim.org). An overall satisfaction score was obtained by averaging the responses to the 5 questions. Internal reliability (Cronbach's α) of the PSQ in this study was 0.90.
The questions of the PSQ were adapted to make them applicable as a measure of physician satisfaction. For example, the question “How well did the doctor address your needs?” was modified to “How well did you address the needs of this patient?” The Cronbach's α of this physician version of the PSQ was 0.87.
Corrected item-total correlations, indicative for internal validity, varied between 0.67 and 0.81 for patients' satisfaction and between 0.56 and 0.82 for physicians' satisfaction. Corrected item-total correlation of the item covering satisfaction with the interaction in general was high for both scales (0.81 and 0.82, respectively).
Patient Characteristics
patients' sociodemographic characteristics such as age, gender, education, primary language, and type of health insurance were included in the baseline questionnaire.
Preference for a certain level of detail in information was measured with a 10-point rating scale,22 ranging from 1 (“prefer as little information as possible”) to 10 (“prefer all information there is”). Given the skewness of the data, the scale was dichotomized. The first 9 response options were scored as “do not prefer as many details as possible,” the tenth as “prefer as many details as possible.”
patients' preferred level of participation in decision making was measured using four 5-point rating scales ranging from giving the physician full responsibility for decision making (1) to the patient wanting full responsibility themselves (5).23 The items covered preference for participation in decision making about treatment, diagnostic examination, life style, and self-monitoring of health. Principal component analysis showed that 1 factor accounted for 64% of the total variance. Hence, the 4 items were summed up, resulting in one overall score for the preference for participation in decision making (range 4 to 20, Cronbach's α 0.81).
patients' self-efficacy in obtaining medical information and physicians' attention to their medical concerns was assessed with the Perceived Efficacy in Patient-Physician Interactions (PEPPI).24 The PEPPI consists of 10 items, each beginning with “How confident are you in your ability to.…” Subjects responded to each question on a scale of 1 (“not at all confident”) to 5 (“very confident”). For the current study, the PEPPI was translated into Dutch, following a forward-backward procedure. The Cronbach's α coefficient in the present study was 0.95.
Health-related quality of life was assessed with the Dutch Standard Version of the Short-Form (SF-12) Health Survey,25 a validated instrument consisting of 12 items designed to assess the patients' views about their physical and mental state. Two subscales, concerning physical component score (PCS) and mental component score (MCS), are computed using standard algorithms.25
Visit Characteristics
Acquaintance with the physician was assessed by asking patients how many times they had visited this physician before. patients' reason for the encounter was assessed by asking them whether they attended the physician 1) for a routine visit, 2) to get results of an examination, 3) to evaluate treatment, 4) because of increased disease symptoms, and/or 5) for another reason. The sequential number of the visit within the consultation schedule was noted, because we hypothesized, for instance, that a physician may communicate differently with the 15th patient on his schedule compared with the 1st patient. Waiting time was determined by extracting the starting time of the encounter from the time the appointment was scheduled. Duration of the visit represents the number of minutes the patient was inside the consulting room.
Physician Characteristics
The physicians' baseline questionnaire included background characteristics such as age and gender, level of “seniority” (staff physician or resident), specialty, experience (number of years in practice, including years as a resident), workload (mean number of work hours per week), and current routine in outpatient encounters (number of visits per week).
Physicians' professional attitude was assessed with a shortened version of the Doctor-Patient Scale,26,27 the respondent expressing agreement or disagreement with statements on a 5-point scale. The scale was devised to measure physicians' attitudes toward patients and the doctor-patient relationship in terms of patient versus doctor centeredness.27 For reasons of practicality we reduced the original 48-item questionnaire to 10 items, on the basis of face validity. After reliability analysis 6 items were retained. The scales' Cronbach's α coefficient was 0.69.
Physicians' perception of their ability to be communicatively responsive in caring for their patients in general was measured by the Communicative Responsiveness Scale.28 The scale consists of 4 items, and responses were given on a 5-point Likert scale. The scale's Cronbach's α coefficient in this study was 0.70.
Statistical Analyses
To determine differences between participants and nonresponders, we used Fischer's exact tests for physicians, and χ2 tests and Student's t tests for patients. In the analysis of satisfaction, dependencies between patients who shared the same physician were accounted for by applying multilevel analyses. In this way we distinguished two levels of analyses: between- and within-physician level. First, we checked the need for two levels of analysis by comparing the fit of an empty model—without any explanatory variables included—using a fixed intercept with an empty model using a random intercept (χ2 test). Regarding patients' overall satisfaction, the amount of variance at the physician level was not significant. Hence, patient satisfaction appeared not to depend on the physician visited. For physicians' overall satisfaction, however, the amount of variance at the physician level was significant, indicating that physician ratings of satisfaction with their encounters with individual patients were not independent. For unity of presentation, both patient and physician satisfaction were analyzed using multilevel analysis.
Correlations between patients' and physicians' overall satisfaction were calculated to determine patient and physician agreement. Because of the multilevel structure of the data, there were two correlations, one at visit level and one at physician level. A positive correlation at visit level indicates that if a physician is more satisfied with a consultation, the patient is so as well, and vice versa. A positive correlation at physician level indicates that “on average” a more satisfied physician encounters “on average” more satisfied patients, and vice versa.
Multilevel regression modeling was used to determine predictors of patients' and physicians' overall satisfaction. Analyses were performed for patient and physician satisfaction separately. To reduce the number of predictors, we first carried out multiple regression analyses for the patient-related variables, using a backward selection method. A liberal level of significance of 0.15 was used, in order not to miss predictors that might turn out to be important in the final model. We did the same for visit-specific and physician-related variables. In this way we retained 4 possible predictors for the analysis of patient satisfaction and 10 for physician satisfaction. Subsequently, all preselected independent variables were added blockwise to the final model. For physician satisfaction we additionally checked the final model for random slopes, but the variance of the slopes consistently turned out to be not significant. The level of significance was set at 5%. Throughout, random effects and fixed effects were tested two-sided through likelihood ratio or deviance tests and Wald tests, respectively.29 Analyses were performed using SPSS for Windows 11.5.2 (SPSS Inc., Chicago, Ill)30 and MLwiN (London, UK).31
RESULTS
Participants
Of the 37 physicians invited to take part in the study, 30 (81%) consented. All nonparticipating physicians were staff members (100% vs. 50%; P = .03). No other differences between participating and nonparticipating physicians were found. Of the 30 participating physicians, 455 eligible patients were invited to participate, of whom 330 (73%) gave consent (mean 11 patients per physician; range 3 to 18). Nonparticipating patients did not differ from participants in age or gender, but were more likely to be attending the department of general internal medicine or rheumatology, and less likely to be attending the department of gastroenterology (nonresponse 31%, 32%, and 18%, respectively; χ2= 7.2, P = .03).
Forty-two percent of the participating patients were male; the average age was 53 years (Table 1). patients' self-reported diseases included conditions such as diabetes (n = 49), hypertension (n = 27), and rheumatic (n = 50) and gastrointestinal diseases (n = 89). Some of the patients (n = 71, 22%) reported they had not received a diagnosis yet. Characteristics of visits and participating physicians are displayed in Tables 2 and 3
Table 1.
Sample Characteristics: Patient Demographics (N = 330)*
| Number | Percentage/SD (Range) | |
|---|---|---|
| Gender | ||
| Male | 138 | 42% |
| Female | 194 | 58% |
| Mean age, y | 53 | SD 16 (17 to 87) |
| <25 | 11 | 3% |
| 25 to 39 | 58 | 18% |
| 40 to 65 | 172 | 52% |
| >65 | 89 | 27% |
| Education | ||
| Primary school/lower-level high school | 150 | 46% |
| Middle-level high school | 103 | 31% |
| Advanced vocational/ university | 69 | 21% |
| Primary language | ||
| Dutch | 293 | 89% |
| Other | 36 | 11% |
| Health insurance† | ||
| Sickness fund | 224 | 68% |
| Private health insurance | 105 | 32% |
| Mean “preference for information” | 9.6 | SD 1.1 (3 to 10) |
| Prefer as many details as possible | 257 | 78% |
| Do not prefer as many details as possible | 68 | 21% |
| Preference participation in decision making‡ | 11.2 | SD 2.8 (4 to 20) |
| Mean self-efficacy in medical interactions§ | 43.1 | SD .1 (10 to 50) |
| Mean physical health (SF-12: PCS)|| | 38.7 | SD 11.8 (11.6 to 58.6) |
| Mean mental health (SF-12: MCS)|| | 46.8 | SD 11.1 (17.9 to 68.2) |
Not all figures add up to 100%, due to missing data.
Sickness Fund: social insurance, mandatory for over 60% of the population, earning an income below a cutoff value (Euro 32,600 in 2004). Private health insurance: an available option for employees earning an income above the cutoff value of the Sickness Fund.
Higher scores indicate a higher preference for participation in medical decision making.
Higher scores indicate a higher self-efficacy regarding communication in medical interactions.
Higher scores indicate better perceived quality of life. Both PCS and MCS were calculated using standard U.S. scoring algorithms, which yield a mean score of 50 and a standard deviation of 10 in the U.S. general population.
SF-12, Short-Form Health Survey; PCS, physical component score; MCS, mental component score; SD, standard deviation.
Table 2.
Sample Characteristics: Visits (N = 330)*
| Number | Percentage/SD (Range) | |
|---|---|---|
| Department | ||
| General internal medicine | 175 | 53% |
| Rheumatology | 53 | 16% |
| Gastroenterology | 102 | 41% |
| Acquaintance: no of prior visits (with this physician): | ||
| None | 46 | 14% |
| 1 to 2 visits | 131 | 40% |
| 3 to 15 visits | 93 | 28% |
| >15 visits | 42 | 13% |
| Don't know/unknown | 18 | 5% |
| Reason for visit† | ||
| Follow-up/routine visit | 191 | 58% |
| Results of examination | 168 | 51% |
| Evaluation of treatment | 84 | 25% |
| Increase of disease symptoms | 46 | 14% |
| Other | 11 | 4% |
| Average waiting time, min | 10 | SD 16 (–50 to 115) |
| Average duration of visit, min | 13 | SD 5 (2 to 38) |
Not all figures add up to 100%, due to missing data.
Patients could indicate more than one reason for the visit.
SD, standard deviation.
Table 3.
Sample Characteristics: Physicians (N = 30)
| Number | Percentage/SD (Range) | |
|---|---|---|
| Gender | ||
| Male | 16 | 53% |
| Female | 14 | 47% |
| Mean age, y | 38 | SD 8 (26 to 58) |
| Mean years in practice (incl. years as a resident) | 8.6 | SD 8.3 (0.4 to 30.0) |
| Level of “seniority” | ||
| Staff physician | 15 | 50% |
| Resident | 15 | 50% |
| Attitude (6 to 30)* | 24.3 | SD 3.1 (10 to 28) |
| Communicative responsiveness (4 to 20)† | 14.1 | SD 1.9 (10 to 17) |
| “Practice” characteristics | ||
| Specialty | ||
| General internal medicine | 15 | 50% |
| Rheumatology | 5 | 17% |
| Gastroenterology | 10 | 33% |
| Mean work, hr/week | 49.7 | SD 7.6 (37 to 65) |
| Mean no. outpatient encounters/week | 32 | SD 21 (8 to 90) |
A higher score represents a more patient-centered attitude, a lower score represents a more doctor-centered attitude.
A higher score indicates higher perceived communicative responsiveness.
SD, standard deviation.
Patients and Physicians Satisfaction
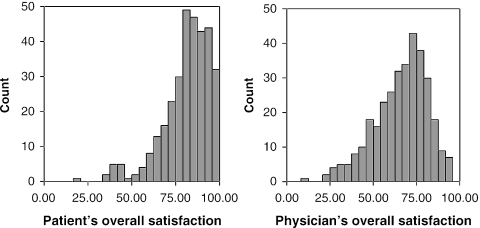
patients' and physicians' visit-specific satisfaction are presented in Table 4Figure 1. Physician satisfaction was substantially lower than patient satisfaction, both at item level and at overall satisfaction level. The correlation of patients' and physicians' overall satisfaction (n = 327) was 0.28 (P < .001), indicating a “medium-sized” association.32 The correlation at physician level (n = 30) was not significant, that is, the mean satisfaction of a physician was not associated with the mean satisfaction of his or her patients.
Table 4.
Visit-specific Satisfaction
| Satisfaction with | Patient Satisfaction Mean (SD)† | Physician Satisfaction Mean (SD)† | Correlation‡ |
|---|---|---|---|
| Needs addressed | 81 (16) | 63 (20) | 0.31* |
| Patient's involvement | 79 (16) | 69 (20) | 0.09 |
| Information given by physician | 83 (16) | 68 (18) | 0.16* |
| Emotional support | 80 (17) | 64 (18) | 0.21* |
| Interaction in general | 83 (15) | 67 (19) | 0.22* |
| Overall satisfaction§ | 81 (14) | 66 (15) | 0.28* |
P < .001.
0 to 100 scales. Due to missing data, n ranges from 325 to 328 (patient satisfaction) and from 329 to 330 (physician satisfaction).
Correlation between patient and physician satisfaction at visit level, accounting for the dependencies between patients of the same physicians.
patients' and physicians' average response on the 5 items.
FIGURE 1.
patients' and physicians' overall satisfaction with the outpatient encounter (N = 324).
Factors Predicting Satisfaction
Predictors of patient and physician satisfaction are shown in Table 5. Patients were more likely to be satisfied with the encounter when they perceived themselves to be more efficacious in obtaining medical information and physicians' attention to their medical concerns (P < .001). patients' satisfaction was not associated with background characteristics such as their age, gender, educational level, primary language, and physical or mental health. Also, patients' preference for information and for participation in medical decision making did not predict their satisfaction ratings. None of the visit-specific variables were associated with patient satisfaction, and neither were the physician-related variables except for physicians' female gender (P < .01). This model explained 27% of the variance in patients' satisfaction.
Table 5.
Predictors of Patient and Physician Satisfaction, Using Multilevel Multiple Regression Analysis
| Final model | Patient Satisfaction (n = 298) Coeff (SE) | Physician Satisfaction (n = 296) Coeff (SE) |
|---|---|---|
| Fixed effect | ||
| Intercept† | 39.51 (4.21) | 42.79 (6.41) |
| Patient variables | ||
| Age | Not selected | 0.10 (0.05) |
| Education | Not selected | 1.39 (0.62)* |
| Primary language (0.1)‡ | Not selected | −9.23 (2.60)*** |
| Physical health | Not selected | 0.14 (0.07) |
| Mental health | Not selected | 0.18 (0.07)* |
| Preference/info (0.1)§ | Not selected | 4.35 (1.96)* |
| Preference/decision making | Not selected | 0.50 (0.28) |
| Self-efficacy in communication | 0.88 (0.10)*** | Not selected |
| Visit-specific variables | ||
| Sequential number of visit | Not selected | −0.31 (0.24) |
| No. of prior visits (this physician) | 0.81 (0.43) | Not selected |
| Reason visit “increase of symptoms” (0.1)|| | −1.82 (1.88) | Not selected |
| Physician variables | ||
| Physician's gender (0.1)¶ | 4.17 (1.35)** | Not selected |
| Dept. (0.1; 1 = rheumatology) | Not selected | −6.23 (3.42) |
| Dept. (0.1; 1 = gastroenterology) | Not selected | −1.59 (2.73) |
| Random effect | ||
| Visit level (σ2e) | 132.31 (10.84) | 167.80 (14.53) |
| Physician level (σ2µ0) | 0.00 (0.00) | 25.11 (11.12) |
| R2 (visit level) | .27 | .19 |
| R2 (physician level) | — | .35 |
| Goodness of fit: χ2 (df)# | 93.7 (4)*** | 50.7 (10)*** |
The intercept can be interpreted as the average satisfaction of a (hypothetical) subject scoring 0 for each predictor in the model.
P < .05;
0 = Dutch, 1 = other.
P < .001.
0 = preference for all information possible, 1 = less than all information.
0 = no, yes = 1.
0 = male, 1 = female.
P < .01;
Improvement of fit compared to model 0 (empty model).
Higher physician satisfaction was associated with patients' higher educational level (P < .05), their primary language being Dutch (P < .001), better mental health (P < .05), and patients' preferences for receiving less than full information (P < .05). This model explained 19% of the visit level variance in physicians' satisfaction. Physician satisfaction was not predicted by patients' physical health, self-efficacy, or preference for participation in medical decision making. Furthermore, neither visit-specific variables nor physician-related variables were associated with physician satisfaction.
As the relationship between patients' satisfaction and their previsit self-efficacy was strong, we determined post hoc which variables were associated with patients' self-efficacy. Higher scores on self-efficacy were associated with patients' older age (r = .17, P < .01), better physical (r = .13, P < .05) and mental health (r = .27, P < .01), higher information need (r = .14, P < .05), and a higher number of prior visits with this physician (r = .13, P < .05). Two of these variables, age and number of prior visits, had significant bivariate correlation with patient satisfaction (r = .18, P < .01 and r = .13, P < .05, respectively).
DISCUSSION
This study compared patients' and physicians' visit-specific satisfaction in an internal medicine specialist setting. patients' satisfaction was considerably higher than physicians' satisfaction, and the correlation between patients' and physicians' ratings was medium-sized. patients' satisfaction was largely determined by their previsit self-efficacy in communicating with their physician and by physicians' gender, whereas physicians' satisfaction was mainly predicted by patients' educational level, primary language, mental health, and preference for information.
It appears that physicians were more critical of the quality of their communication than patients. This finding is consistent with other studies.3,10–12,15 The correlation between patients' and physicians' ratings was not high, which indicates that patients and physicians actually judged the consultation differently. Some other investigators have found no significant correlation between patients' and physicians' satisfaction ratings.13,14 Of interest, as mentioned in Methods, patient satisfaction was independent of the physician visited, whereas a physician's satisfaction ratings were not independent from each other. Patients may not have varied greatly in their ratings because they usually have little reference material to judge their physician, as patients see their physician infrequently and generally meet few different specialists. By contrast, physicians encounter many patients daily, which enables them to compare visits. Moreover, it is possible that there actually was little difference between physicians in their delivery of care. In that case all physicians were equally good (or bad), as reflected in the patients' ratings, but some physicians judged their encounters more critically than others.
We adapted the Patient Satisfaction Questionnaire to also measure physicians' satisfaction, in order to be able to compare patients' and physicians' ratings. Although internal reliability of both versions was high, physicians may have interpreted questions differently. For both the patients' and the physicians' scale, however, an underlying “satisfaction” dimension is suggested by the high corrected item-total correlation of the item about satisfaction with the interaction in general, indicating that both scales consider relevant aspects of satisfaction.
Patients and physicians may have different perceptions of the consultation process, as a result of different expectations and demands. In a study by Laine et al.,33 for example, patients and physicians agreed that the most crucial element of outpatient care is clinical skill, but they disagreed about the relative importance of other aspects of care; particularly, patients found provision of information far more important than physicians. Likewise, in a general practice setting, aspects of the doctor-patient relationship and provision of information were rated and ranked higher by patients than by doctors.11 The dissimilar predictors determining patients' and physicians' satisfaction in our study seem to confirm that patients and physicians actually form their opinion about a consultation using different criteria.
The higher patients perceived their self-efficacy in obtaining medical information and physicians' attention to their medical concerns, the more satisfied they were after the visit. patients' satisfaction as well as self-efficacy had a bivariate association with patients' age and number of prior visits to this physician. Although the associations were small, they might indicate that the well-known relationship between patients' satisfaction and age and patient-physician acquaintance is in part mediated by a higher confidence of these patients in their ability to communicate with the physician. As self-efficacy is an important predictor of actual behavior,34 it would be interesting to determine whether these patients actually communicate in a more participatory way with their physicians as compared to patients with lower self-efficacy. An additional line of inquiry would be to determine whether patient participation can be enhanced by enhancing self-efficacy.
Patient satisfaction was also related to physician gender. Some earlier studies also found patients of female physicians to be more satisfied,35–38 but other studies did not.14,39–41 A recent systematic review42 revealed that visits with female physicians tend to be longer than those with male physicians. In our study, however, the mean visit duration of both male and female physicians was 13 minutes. Furthermore, the review showed that female physicians tend to use more “patient-centered” behavior, such as active partnership behaviors, use of emotional talk, and active enlistment of patient input, than do male doctors. Whether these gender differences also occur in our study awaits further investigation.
In contrast with other studies, patient satisfaction was not associated with perceived physical or mental health state. This could be due to the timing of satisfaction assessment. Jackson et al.17 showed that patient satisfaction ratings immediately after a consultation were primarily affected by doctor-patient communication, whereas satisfaction ratings 2 weeks and 3 months after the consultation were related to medical outcome, such as health status. patients' previsit preference for participation in medical decision making in our study was also not associated with patients' satisfaction ratings. This is in line with findings of Gattellari et al.,43 whereas Golin et al.44 found that diabetic patients who desired greater participation in medical decision making were more satisfied with the visit.
Physicians seemed to be more comfortable seeing an “easy patient”: a person who is well-educated, whose primary language is Dutch, who does not want to be fully informed, and has good mental health. These latter associations are in accordance with Suchman et al.,1 who found patients' nondemanding, cooperative nature to be an independent component of physician satisfaction, and who found patients' emotional distress—as rated by the physician—to be associated with lower physicians' satisfaction. This may suggest that physicians fail to meet their own standards of care with lower-educated, demanding, or distressed patients. It would be worthwhile to pay further attention to physicians' difficulties in communicating with these specific groups of patients. Notably, physicians in our study appeared to find difficulty in communicating with patients whose primary language was not Dutch, generally being patients from a different ethnic background. Patients were only eligible for this study when they were able to speak, read, and write Dutch; thus only a selective, relatively skilled group of patients from a different ethnic background took part. Further research in the field of communication with these patients is warranted.
Visit characteristics such as waiting time, duration of the consultation, and the reason for visiting the physician were not associated with either patients' or physicians' satisfaction. This suggests that satisfaction reflects the patient-physician relationship more than the context of the visit. Some studies10,14 have found a significant relationship between patient satisfaction and waiting time. In these studies, however, waiting time was a self-reported variable, reflecting patients' perceptions of how long they had been waiting, whereas in the present study actual waiting time was used.
Physicians participating in this study were residents and specialists in general internal medicine and two subspecialties: rheumatology and gastroenterology. Hospital-based (general) internists in The Netherlands function more like specialists as compared to the general internists in the United States. On the other hand, Dutch (sub)specialists, such as rheumatologists and gastroenterologists, are also general internists and may have a more general view than U.S. subspecialists. Almost 60% of the visits in this study were routine follow-up visits, which may make findings generalizable to U.S. general internist visits.
Some limitations of the study should be noted. First, although questionnaires were filled out anonymously, satisfaction ratings might have been biased by response tendencies. Physicians had to judge their own behavior, and accordingly they may have been more critical, based on social desirability considerations. Patients, on the other hand, judged their physician, on whom they are dependent for receiving care. This is regarded as one of the reasons why high levels of patient satisfaction are a common finding in satisfaction research.18,45 Second, although the response rate of physicians in our study was satisfactory (81%), all nonresponding physicians were staff physicians, which could have influenced satisfaction ratings.
The explained variance in satisfaction in our study was high compared with other studies.17 Still, it is possible that other factors, particularly the interaction process, contributed to both patient and physician satisfaction. Several studies have shown that patients' satisfaction is related to verbal and nonverbal behaviors during the visit, but results have been conflicting.46–48 A next step will be to determine whether the interaction process influences both patient and physician satisfaction, controlling for the respective predictors mentioned above.
In the assessment of quality of care, experiences of both patients and their health care providers are of relevance. Ideally, all participating parties are satisfied with the care they receive or give, even if their opinions are based on different aspects of care. Yet, even though in recent years the number of studies using physician satisfaction with specific medical encounters has been growing, physicians' satisfaction has not regularly been used as an outcome measure. Our study shows that patients and physicians may differ in their satisfaction ratings regarding the same encounter, while the dissimilar factors influencing patients' and physicians' satisfaction suggest that patients and physicians indeed form their opinion about a consultation in different ways. Our findings underline that in quality of (outpatient) care research, the use of physicians' satisfaction has additional value to patients' opinions, and we suggest that this outcome measure be incorporated in research consistently.
Acknowledgments
We thank the patients and physicians who participated in the study. Furthermore, we greatly appreciate the hospitality of the receptionists and nurses at the outpatient clinic of Internal Medicine. Finally, we render thanks to the Board of Directors of the Academic Medical Center/University of Amsterdam, The Netherlands, who funded this study.
Appendix
REFERENCES
- 1.Suchman AL, Roter D, Green M, Lipkin MJ. Physician satisfaction with primary care office visits. Collaborative Study Group of the American Academy on Physician and Patient. Med Care. 1993;31:1083–92. doi: 10.1097/00005650-199312000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Fairhurst K, May C. Consumerism and the consultation: the doctor's view. Fam Pract. 1995;12:389–91. doi: 10.1093/fampra/12.4.389. [DOI] [PubMed] [Google Scholar]
- 3.Orden SR, Collette P, Souchek J, Masover L, Stamler J. Physician and patient assessment of ambulatory care in a university facility. J Community Health. 1978;4:23–32. doi: 10.1007/BF01349582. [DOI] [PubMed] [Google Scholar]
- 4.Lewis CC, Pantell RH, Sharp L. Increasing patient knowledge, satisfaction, and involvement: randomized trial of a communication intervention. Pediatrics. 1991;88:351–8. [PubMed] [Google Scholar]
- 5.Shore BE, Franks P. Physician satisfaction with patient encounters. Reliability and validity of an encounter-specific questionnaire. Med Care. 1986;24:580–9. [PubMed] [Google Scholar]
- 6.Roter DL, Stewart M, Putnam SM, Lipkin MJ, Stiles W, Inui TS. Communication patterns of primary care physicians. JAMA. 1997;277:350–6. [PubMed] [Google Scholar]
- 7.Hornberger J, Thom D, MaCurdy T. Effects of a self-administered previsit questionnaire to enhance awareness of patients' concerns in primary care. J Gen Intern Med. 1997;12:597–606. doi: 10.1046/j.1525-1497.1997.07119.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mann S, Sripathy K, Siegler EL, Davidow A, Lipkin M, Roter DL. The medical interview: differences between adult and geriatric outpatients. J Am Geriatr Soc. 2001;49:65–71. doi: 10.1046/j.1532-5415.2001.49011.x. [DOI] [PubMed] [Google Scholar]
- 9.Detmar SB, Muller MJ, Schornagel JH, Wever LD, Aaronson NK. Health-related quality-of-life assessments and patient-physician communication: a randomized controlled trial. JAMA. 2002;288:3027–34. doi: 10.1001/jama.288.23.3027. [DOI] [PubMed] [Google Scholar]
- 10.Kurata JH, Nogawa AN, Phillips DM, Hoffman S, Werblun MN. Patient and provider satisfaction with medical care. J Fam Pract. 1992;35:176–9. [PubMed] [Google Scholar]
- 11.Jung HP, Wensing M, Olesen F, Grol R. Comparison of patients' and general practitioners' evaluations of general practice care. Qual Saf Health Care. 2002;11:315–9. doi: 10.1136/qhc.11.4.315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rashid A, Forman W, Jagger C, Mann R. Consultations in general practice: a comparison of patients' and doctors' satisfaction. BMJ. 1989;299:1015–6. doi: 10.1136/bmj.299.6706.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Winefield HR, Murrell TG, Clifford J. Process and outcomes in general practice consultations: problems in defining high quality care. Soc Sci Med. 1995;41:969–75. doi: 10.1016/0277-9536(94)00403-g. [DOI] [PubMed] [Google Scholar]
- 14.Probst JC, Greenhouse DL, Selassie AW. Patient and physician satisfaction with an outpatient care visit. J Fam Pract. 1997;45:418–25. [PubMed] [Google Scholar]
- 15.Weinberger M, Greene JY, Mamlin JJ. The impact of clinical encounter events on patient and physician satisfaction. Soc Sci Med. 1981;15:239–44. doi: 10.1016/0271-5384(81)90019-3. [DOI] [PubMed] [Google Scholar]
- 16.Hall JA, Dornan MC. Patient sociodemographic characteristics as predictors of satisfaction with medical care: a meta-analysis. Soc Sci Med. 1990;30:811–8. doi: 10.1016/0277-9536(90)90205-7. [DOI] [PubMed] [Google Scholar]
- 17.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52:609–20. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 18.Sitzia J, Wood N. Patient satisfaction: a review of issues and concepts. Soc Sci Med. 1997;45:1829–43. doi: 10.1016/s0277-9536(97)00128-7. [DOI] [PubMed] [Google Scholar]
- 19.Kreft I, de-Leeuw J. Introducing Multilevel Modeling. x. Thousand Oaks, Calif: Sage Publications; 1998. p. 149. [Google Scholar]
- 20.Blanchard CG, Ruckdeschel JC, Fletcher BA, Blanchard EB. The impact of oncologists' behaviors on patient satisfaction with morning rounds. Cancer. 1986;58:387–93. doi: 10.1002/1097-0142(19860715)58:2<387::aid-cncr2820580233>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 21.Ong LML, Visser MRM, Lammes FB, de Haes JCJM. Doctor-patient communication and cancer patients' quality of life and satisfaction. Patient Educ Couns. 2000;41:145–56. doi: 10.1016/s0738-3991(99)00108-1. [DOI] [PubMed] [Google Scholar]
- 22.Cassileth BR, Zupkis RV, Sutton-Smith K, March V. Information and participation preferences among cancer patients. Ann Intern Med. 1980;92:832–6. doi: 10.7326/0003-4819-92-6-832. [DOI] [PubMed] [Google Scholar]
- 23.Sutherland HJ, Llewellyn-Thomas HA, Lockwood GA, Tritchler DL, Till JE. Cancer patients: their desire for information and participation in treatment decisions. J R Soc Med. 1989;82:260–3. doi: 10.1177/014107688908200506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maly RC, Frank JC, Marshall GN, DiMatteo MR, Reuben DB. Perceived efficacy in patient-physician interactions (PEPPI): validation of an instrument in older persons. J Am Geriatr Soc. 1998;46:889–94. doi: 10.1111/j.1532-5415.1998.tb02725.x. [DOI] [PubMed] [Google Scholar]
- 25.Ware JJ, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 26.de Monchy C, Richardson R, Brown RA, Harden RM. Measuring attitudes of doctors: the doctor-patient (DP) rating. Med Educ. 1988;22:231–9. doi: 10.1111/j.1365-2923.1988.tb00012.x. [DOI] [PubMed] [Google Scholar]
- 27.Batenburg V. Medical students' attitudes: attitude development in a medical school. 1997. PhD Thesis, Utrecht: Elinkwijk BV.
- 28.Miller KI, Stiff JB, Ellis BH. Communication and empathy as precursors to burn-out among human service workers. Commun Monogr. 1988;55:250–65. [Google Scholar]
- 29.Hox JJ. Multilevel AnalysisTechniques and Applications. London, UK: Lawrence Erlbaum Associates, Inc.; 2002. [Google Scholar]
- 30.SPSS Inc. SPSS 115 Syntax Reference Guide: Base System, Advanced Models, Regression Models. Chicago, Ill: SPSS Inc.; 2003. [Google Scholar]
- 31.Rasbash J, Browne W, Goldstein H, et al. A User's Guide to MLwiN. London, UK: University of London, Centre of Multilevel Modelling, Institute of Education; 2002. [Google Scholar]
- 32.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Rev. ed. xv. Hillsdale, NJ: Lawrence Erlbaum Associates; 1987. p. 474. [Google Scholar]
- 33.Laine C, Davidoff F, Lewis CE, et al. Important elements of outpatient care: a comparison of patients' and physicians' opinions. Ann Intern Med. 1996;125:640–5. doi: 10.7326/0003-4819-125-8-199610150-00003. [DOI] [PubMed] [Google Scholar]
- 34.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. xiii. Upper Saddle River, NJ: Prentice-Hall; 1986. p. 617. [Google Scholar]
- 35.Linn LS, Cope DW, Leake B. The effect of gender and training of residents on satisfaction ratings by patients. J Med Educ. 1984;59:964–6. doi: 10.1097/00001888-198412000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Delgado A, Lopez-Fernandez LA, Luna JD. Influence of the doctor's gender in the satisfaction of the users. Med Care. 1993;31:795–800. doi: 10.1097/00005650-199309000-00004. [DOI] [PubMed] [Google Scholar]
- 37.Bertakis KD, Helms LJ, Callahan EJ, Azari R, Robbins JA. The influence of gender on physician practice style. Med Care. 1995;33:407–16. doi: 10.1097/00005650-199504000-00007. [DOI] [PubMed] [Google Scholar]
- 38.Roter DL, Geller G, Bernhardt BA, Larson SM, Doksum T. Effects of obstetrician gender on communication and patient satisfaction. Obstet Gynecol. 1999;93:635–41. doi: 10.1016/s0029-7844(98)00542-0. [DOI] [PubMed] [Google Scholar]
- 39.Murphy-Cullen CL, Larsen LC. Interaction between the socio-demographic variables of physicians and their patients: its impact upon patient satisfaction. Soc Sci Med. 1984;19:163–6. doi: 10.1016/0277-9536(84)90283-1. [DOI] [PubMed] [Google Scholar]
- 40.Anderson LA, Zimmerman MA. Patient and physician perceptions of their relationship and patient satisfaction: a study of chronic disease management. Patient Educ Couns. 1993;20:27–36. doi: 10.1016/0738-3991(93)90114-c. [DOI] [PubMed] [Google Scholar]
- 41.Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–8. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–64. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 43.Gattellari M, Butow PN, Tattersall MH. Sharing decisions in cancer care. Soc Sci Med. 2001;52:1865–78. doi: 10.1016/s0277-9536(00)00303-8. [DOI] [PubMed] [Google Scholar]
- 44.Golin C, DiMatteo MR, Duan N, Leake B, Gelberg L. Impoverished diabetic patients whose doctors facilitate their participation in medical decision making are more satisfied with their care. J Gen Intern Med. 2002;17:857–66. doi: 10.1046/j.1525-1497.2002.20120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Williams B, Coyle J, Healy D. The meaning of patient satisfaction: an explanation of high reported levels. Soc Sci Med. 1998;47:1351–9. doi: 10.1016/s0277-9536(98)00213-5. [DOI] [PubMed] [Google Scholar]
- 46.Williams S, Weinman J, Dale J. Doctor-patient communication and patient satisfaction: a review. Fam Pract. 1998;15:480–92. doi: 10.1093/fampra/15.5.480. [DOI] [PubMed] [Google Scholar]
- 47.Mead N, Bower P. Patient-centred consultations and outcomes in primary care: a review of the literature. Patient Educ Couns. 2002;48:51. doi: 10.1016/s0738-3991(02)00099-x. [DOI] [PubMed] [Google Scholar]
- 48.Lewin SA, Skea ZC, Entwistle V, Zwarenstein M, Dick J. Interventions for providers to promote a patient-centered approach in clinical consultations. Cochrane Database Syst Rev. 2001 doi: 10.1002/14651858.CD003267. CD003267. [DOI] [PubMed] [Google Scholar]