Abstract
OBJECTIVE
To compare collaborative care for treatment of depression in primary care with consult-liaison (CL) care. In collaborative care, a mental health team provided a treatment plan to the primary care provider, telephoned patients to support adherence to the plan, reviewed treatment results, and suggested modifications to the provider. In CL care, study clinicians informed the primary care provider of the diagnosis and facilitated referrals to psychiatry residents practicing in the primary care clinic.
DESIGN
Patients were randomly assigned to treatment model by clinic firm.
SETTING
VA primary care clinic.
PARTICIPANTS
One hundred sixty-eight collaborative care and 186 CL patients who met criteria for major depression and/or dysthymia.
MEASUREMENTS
Hopkins Symptom Checklist (SCL-20), Short Form (SF)-36, Sheehan Disability Scale.
MAIN RESULTS
Collaborative care produced greater improvement than CL in depressive symptomatology from baseline to 3 months (SCL-20 change scores), but at 9 months there was no significant difference. The intervention increased the proportion of patients receiving prescriptions and cognitive behavioral therapy. Collaborative care produced significantly greater improvement on the Sheehan at 3 months. A greater proportion of collaborative care patients exhibited an improvement in SF-36 Mental Component Score of 5 points or more from baseline to 9 months.
CONCLUSIONS
Collaborative care resulted in more rapid improvement in depression symptomatology, and a more rapid and sustained improvement in mental health status compared to the more standard model. Mounting evidence indicates that collaboration between primary care providers and mental health specialists can improve depression treatment and supports the necessary changes in clinic structure and incentives.
Keywords: depressive disorder, primary health care, veterans
Depression is a common chronic illness associated with major impairments in function.1–4 Most depression treatment is provided in primary care settings,5,6 where this condition continues to be underdetected and undertreated.7–11
Randomized trials have demonstrated that attempts to improve practice that rely upon a single aspect of care, such as patient screening, registries, provider education, or feedback, typically produce only minor improvements, if any.12 For example, the setting of the study that we report here, the General Internal Medicine Clinic (GIMC) of the Seattle Division of Department of Veterans Affairs Puget Sound Health Care System, had been a site in an earlier trial of academic detailing and continuous quality improvement. The intervention, largely focusing on depression screening and feedback, resulted in no difference in treatment process or outcomes.13,14
Collaborative care includes patient-, provider-, and system-level components based on a chronic illness model.15 It is a population-based approach in which multidisciplinary primary care teams assist the primary care provider in delivering evidence-based treatment.16,17 Studies evaluating such interventions have demonstrated success in improving both process and outcomes of depression care.18–22 It was not clear, however, whether the interventions tested in these settings would work equally well in the VA, which treats a primarily aging male population that is below average in socioeconomic resources and above average in comorbidity and functional disability.1,23,24 Such approaches have not been previously been tested in VA to our knowledge.
We adapted this collaborative care model to the patient population and treatment resources in a VA primary care setting and compared it with consult-liaison (CL) care. The study objectives were to compare the effects of the 2 models of care on depression symptom severity, health status, and satisfaction with care.
METHODS
Setting
The GIMC is organized into 4 firms,25 to which providers and their patient panels are assigned in an unsystematic manner. GIMC staff with independent patient panels during the study recruitment period (January 1998 until March 1999, with follow-up for an additional 9 months) included 19 attending physicians, 38 residents, 10 fellows, and 22 nurse practitioners. The clinic was supported by 1 full-time equivalent psychiatry resident, an attending psychiatrist who supervised the resident, clinical psychologists and interns, and 4 social workers and interns. Two of the 4 clinic firms were randomly assigned to the collaborative care intervention, and 2 to CL care.
Sample
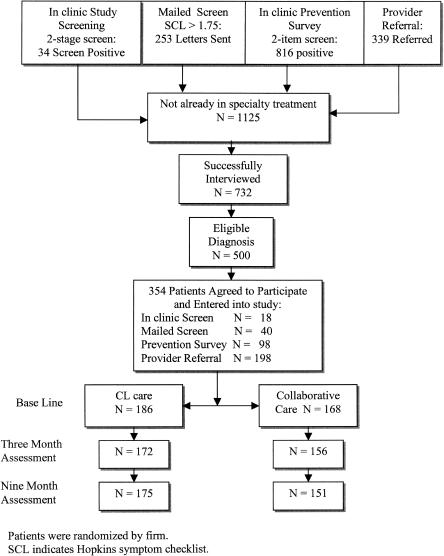
Several previous collaborative care studies evaluated patients for inclusion only after they had been identified by their primary care provider as being depressed, had been started on an antidepressant medication,19 and remained symptomatic.20 Because of the under-identification of depressed primary care patients reported in previous studies, we decided to include patients at an earlier stage in the process, i.e., patients who had not yet been recognized and who had not yet begun treatment. We used 4 screening methods: 1) patients with major depression or dysthymia (our targeted conditions) referred from an ongoing unrelated study conducting waiting room screening to identify patients with minor depression,26 2) mailed screening conducted for another ongoing study,27 3) a prevention survey conducted with all patients as part of the clinic check-in, and 4) referral by primary care providers (see Fig. 1). Although other methods generated more total referrals, this last method generated the most referred patients who were eligible for and entered the study. All procedures were reviewed by the Human Subjects Committee. No known adverse events occurred as a consequence of study activities.
FIGURE 1.
Recruitment and retention for collaborative care study.
After initial screening, we administered a computer-assisted structured interview to each prospective subject assessing depression severity, current or past use of medication or therapy, health status, current and past alcohol use, posttraumatic stress disorder symptoms, history of mental illness, and barriers to care. The assessment of depression and anxiety symptoms was based on the Primary Care Evaluation of Mental Disorders (PRIME-MD) questionnaire with additional questions taken from the Structured Clinical Interview for the Diagnostic and Statistical Manual of Mental Disorders–Fourth Edition (DSM-IV).11 Alcohol use was assessed with the CAGE, a quantity-frequency index, and questions about the patient's perception of substance use.28 A skilled psychology technician conducted the interview in person or by telephone. Previous studies have found high concordance between in-person and telephone structured depression assessment.29
Eligible patients had a current major depressive episode, dysthymia, or both. Exclusion criteria were as limited as possible to enhance the generalizability of the results. Patients who had made a recent visit to a mental health specialty clinic or who had scheduled a future appointment were excluded, because we did not want to interfere in ongoing intensive treatment. Patients who required treatment for substance abuse or posttraumatic stress disorder prior to initiating depression treatment were excluded and referred to appropriate specialty clinics (N = 53). Eleven other patients were excluded because of acute suicidality, psychosis, or other condition requiring immediate treatment. Estimates of statistical power performed prior to initiating the study indicated that a minimum group size of 168 was required to achieve adequate power. Because baseline assessment was blinded to group membership, recruitment continued until the sample size criterion was met for both groups, resulting in a final tally of 168 collaborative care and 186 CL patients.
Interventions
Provider Education
Primary care providers on both arms received 3 hours of instruction about depression assessment and treatment and clinic resources.30
Consult-liaison Care
CL care represented the traditional model in which the primary care provider was responsible for initiating treatment of depressive symptoms and coordinating the patient's overall care, with consultation from or referral to a specialist as deemed necessary. To ensure that the trial was not merely a test of more care versus less care, an explicit attempt was made to equate the amount of mental health resources available to each of the firms. The available time of the psychologist and social workers was evenly divided among the 4 firms. During the study period, the psychiatry resident's time was reserved for the CL firms, whereas the supervising psychiatrist participated in the collaborative care intervention but rarely met directly with patients. Providers in all firms were notified of the patient's diagnosis either via an entry into the electronic medical record or, if the provider had referred the patient, as part of the report of the consultant. Primary care providers in the CL care firms were able to refer patients to the psychiatry resident, psychologist, and/or social workers, all of whom were physically present in the GIMC. The CL mental health providers provided treatment directly during individual visits with patients who were deemed manageable in the primary care setting. More complicated patients were referred to specialty mental health clinics, facilitated by the study team.
Collaborative Care
Diagnosis and treatment
The collaborative care team consisted of a clinical psychologist, a psychiatrist, social workers, and a psychology technician. The team met weekly to develop treatment plans and to conduct a 6- and 12-week progress evaluation for each patient. The team decided on a treatment recommendation following VA Major Depression Guideline treatment recommendations, taking into account current and previous treatment and patient preferences.31 The team communicated with primary care providers using electronic progress notes. The system incorporated an alert and co-signature function that brought any new communication to the provider's attention and enabled the team to track receipt and acknowledgment of notes and follow-up. For recommendations that were questioned by the primary care provider, the team psychiatrist contacted the provider to achieve consensus on a treatment plan. The team also tracked pharmacy records. If agreed-upon prescriptions were not written in a timely fashion, the study team contacted the provider to discuss the recommendation. In 5 cases, the provider could not be contacted and the team psychiatrist wrote the prescription and followed up with the patient.
Treatment options
Depression treatment options were: begin, increase dosage of, or change antidepressant medication; add an adjuvant medication; enroll in a cognitive behavior therapy (CBT) group; schedule with the psychologist or psychiatrist; or refer to mental health specialty care. Options were selected in a stepwise fashion beginning with the least resource-intensive option consonant with previous treatments and the patient's preference. If the 6- and 12-week progress evaluations indicated the option was ineffective, a new or stepped-up option was recommended.
Cognitive behavior therapy
Previous studies have found that brief psychological therapy is effective12,32 and preferred to antidepressant medication by many patients.33 We designed a CBT group consisting of 6 sessions34 led by a psychologist or social worker.35
Patient education
A videotape36 and specially designed 3-part patient workbook were mailed to each patient during the course of treatment.
Patient support and progress evaluation
A social work staff member or student called each patient on a regular schedule to encourage adherence, address treatment barriers, and assess response.
Measures and Data Collection
Outcome measures were administered to all patients at baseline (within 1 week of enrollment) and 3 and 9 months later in a computer-assisted telephone interview. Interviewers were trained graduate students who were uninformed as to subjects' group membership. Depressive symptomatology was measured using the Hopkins Symptom Checklist (SCL-20) depression scale, consisting of the 20 depression items from the SCL-90.37 We report the average item score (range, 0 to 4.0). Health status was measured with the Veterans Short Form (SF)-36 Health Status Questionnaire.1,38 This assessment, like the MOS SF-36, can be scored as 8 subscales and as 2 scores: a physical component summary (PCS) score and a mental component summary (MCS) score.
We used the Sheehan Disability Scale,39 a 3-item questionnaire that examines how diminished health status interferes with work/school, family life, and social life and activities. We evaluated patient satisfaction with treatment using scales developed by Katon et al.19
Using the VA's electronic medical record system, we collected data for the year after baseline on the number and dosage of antidepressant prescriptions. We assessed the therapeutic adequacy of antidepressant prescriptions by adapting an algorithm from Simon et al.40 Prescriptions were classified as being of at least the minimum therapeutic dose or twice the minimum therapeutic dose recommended by Agency for Health Care Policy and Research guidelines32 and additional published sources for newer medications. We determined whether the 2 dosage ranges had been prescribed for at least 30 days or at least 90 days. This approach to assessing antidepressant treatment adequacy from pharmacy refill data compares favorably to data obtained from patients' reports.41
We used the VA version of the Chronic Disease Score (CDS),42,43 a measure of chronic medical illness based on medication data, to describe overall disease burden at enrollment. This measure has been found to have a high correlation with physician ratings of severity of illness and to predict hospitalization and mortality in the year following assessment after controlling for age, gender, and health care visits.43
Data Analysis
To compare patient characteristics at enrollment, we used t tests for normally distributed continuous variables, Wilcoxon tests for variables with skewed distributions, and Pearson's χ2 tests for categorical variables.
We analyzed SCL, SF-36 and Sheehan scores at 3 and 9 months after baseline using linear regression models. We employed both repeated measures regression methods (linear mixed models), and analysis of covariance (ANCOVA) using the baseline measure as a covariate. In all cases, these analyses yielded similar results and, for simplicity, we present only the ANCOVA results. The additional complexity of mixed models is most beneficial when there are many follow-up occasions and there is substantial missing data (attrition). However, in our study we had only 2 assessment times after baseline and obtained excellent follow-up. Analysis was by intent to treat, with all patients for whom data were available included in each analysis, regardless of final treatment status. We performed 3 sets of analyses: unadjusted; adjusted for provider clustering (using the SAS procedure MIXED; SAS Institute, Inc., Cary, NC); and adjusted for provider clustering, patient age, marital status, living situation (alone or not), race, gender, previous depression episodes, and CDS. Generally, all 3 analyses gave the same results, but we note exceptions where relevant. We present unadjusted means and standard deviations.
To evaluate clinically significant changes in depression, we analyzed 2 categorical outcomes using logistic regression: whether patients achieved a 50% reduction in their baseline SCL score and whether the follow-up SCL scores were above 1.75 (a standard threshold indicating major depression). Categorical analysis was performed using the GEE option44 of the SAS procedure GENMOD.
There is no potential conflict of interest that might bias the results of this work. The study sponsor had no role in the study design beyond initial review of the proposal for funding, and had no role in the collection, analysis, or interpretation of the data; in the writing of the report; or the decision to submit the report for publication. The authors had full data access and accept full responsibility for the integrity of the data and the accuracy of data analysis.
RESULTS
Patients in the collaborative care and CL care groups were similar except that the former were more likely to have had prior depressive episodes (Table 1). None of the variables used as study outcomes were significantly different between the treatment groups at baseline. There were also no significant baseline differences between the 32 patients (9%) for whom 9-month follow-up data could not be obtained and all other patients. Patients' referral sources were similar for the 2 groups. The proportion of patients retained in the study in both collaborative care and CL care was high at 3 (93% vs 92%) and 9 months (90% vs 94%) (Fig. 1).
Table 1.
Baseline Characteristics of Patients by Group
| Characteristics | Collaborative Care (n = 168) | Consult-liason Care (n = 186) |
|---|---|---|
| Mean age, y ± SD | 57.8 ± 13.5 | 56.6 ± 14.2 |
| Male, % | 95.2 | 95.7 |
| Married, % | 40.5 | 44.1 |
| Caucasian, % | 78.0 | 81.2 |
| >1 Y college, % | 57.5 | 56.8 |
| Living alone, % | 34.5 | 26.3 |
| Service-connected disability, % | 56.0 | 60.6 |
| With previous depression,* % | 59.5 | 48.4 |
| Both major depression and dysthymia, % | 58.9 | 62.2 |
| SF-36, mean ± SD | ||
| Subscales | ||
| Physical functioning | 40.07 ± 26.94 | 43.09 ± 25.67 |
| Role–physical | 43.75 ± 31.37 | 44.29 ± 27.77 |
| Bodily pain | 36.99 ± 26.39 | 36.55 ± 23.59 |
| General health | 38.63 ± 23.43 | 35.06 ± 21.79 |
| Energy/vitality | 24.98 ± 18.96 | 26.39 ± 18.68 |
| Social functioning | 37.01 ± 26.43 | 40.72 ± 27.01 |
| Role–emotional | 53.28 ± 29.17 | 58.24 ± 27.73 |
| Mental health | 43.00 ± 19.13 | 43.83 ± 20.83 |
| Summary scores | ||
| Physical Component Summary (PCS) | 33.37 ± 12.49 | 32.87 ± 11.06 |
| Mental Component Summary (MCS) | 33.74 ± 11.56 | 35.23 ± 11.89 |
| Sheehan Functional Status Summary | 5.75 ± 2.43 | 5.33 ± 2.45 |
| Symptom Check List (SCL) | 1.96 ± 0.65 | 1.83 ± 0.70 |
| Chronic Disease Score | 3.80 ± 3.20 | 3.40 ± 3.10 |
Significant difference between study arms using Wilcoxon nonparametric test (P < .05).
The components of the collaborative care intervention were generally implemented as planned. The team developed, revised, communicated, and helped implement treatment plans for all collaborative care patients. Patients were discussed in the team meeting on an average of 3 occasions (SD 2.0; range 2 to 9). Of the 3 to 5 social work follow-up calls that were scheduled during acute-phase treatment, patients received an average of 2.1 calls (SD 1.6; range 0 to 5). Three to five calls were planned for the maintenance phase, and an average of 1.2 calls (SD 1.3; range 0 to 6) were completed.
Our efforts to equalize the amount of treatment available to the 2 groups appeared successful. In the year following enrollment in the study, the patients in the 2 groups were equally likely to have made a mental health specialty care visit (36% in collaborative care versus 37% in CL care). Patients in the collaborative care group were more likely to have had a depression-related primary care visit than those in the CL care group (84% vs 57%), while CL patients were more likely to have seen a psychiatry resident in primary care than those in the collaborative care group (37% vs 4%). The total number of primary care visits for the 2 groups was very similar (8.9 visits for collaborative care group versus 8.5 visits for CL care group). No-shows or cancellations of scheduled outpatient visits were not significantly different between the 2 groups (44% collaborative care versus 40% CL care).
Effect on Depression
Patients in the collaborative care group experienced a significantly larger decrease in depressive symptomatology during acute-phase treatment than did patients in the CL group (Table 2). SCL scores decreased an average of 0.34 between baseline and month 3 in the collaborative care group and 0.14 in CL care (P < .025 adjusting for baseline). However, the differences at month 9 were not significantly different (0.41 vs 0.25; P = .17 adjusting for baseline).
Table 2.
Mean Difference in Treatment Outcomes
| Mean Change (SE) | Mean Difference (95% Cl) | |||
|---|---|---|---|---|
| Collaborative Care | Consult-liaison | Difference Between CC and CL, Unadjusted | Difference Between CC and CL, Adjusted | |
| Symptom Check List | ||||
| Baseline to 3 mo | −0.34 (0.05) | −0.14 (0.05) | −0.20 (−0.06 to −0.34)* | −0.17 (−0.31 to −0.03)† |
| Baseline to 9 mo | −0.41 (0.05) | −0.25 (0.06) | −0.16 (−0.01 to −0.31)* | −0.13 (−0.29 to 0.03) |
| Sheehan Disability Scale | ||||
| Baseline to 3 mo | −0.63 (0.21) | 0.09 (0.18) | −0.72 (−1.26 to −0.18)* | −0.53 (−1.04 to −0.02)† |
| Baseline to 9 mo | −0.55 (0.21) | 0.05 (0.20) | −0.60 (−1.17 to −0.03)* | −0.43 (−0.99 to 0.13) |
| SF-36 Mental Component Summary | ||||
| Baseline to 3 mo | 5.06 (1.00) | 1.71 (0.84) | 3.35 (0.79 to 5.91)* | 2.28 (−0.09 to 4.66) |
| Baseline to 9 mo | 5.69 (1.04) | 2.20 (0.97) | 3.49 (0.70 to 6.28)* | 2.37 (−0.45 to 5.19) |
| SF-36 Physical Component Summary | ||||
| Baseline to 3 mo | −0.41 (0.58) | −0.10 (0.51) | −0.31 (−1.82 to 1.20) | −0.08 (−1.57 to 1.41) |
| Baseline to 9 mo | −1.70 (0.67)* | −0.22 (0.59) | −1.48 (−3.23 to 0.27) | −1.20 (−2.83 to 0.43) |
Significantly different (P < .05), unadjusted.
Significantly different using SAS proc mixed, after adjusting for provider clustering, baseline score, age, martial status, living arrangements, race, gender, Chronic Disease Score, and previous episodes of depression.
CC, collaborative care; CL, consult-liason; 95% CI, 95% confidence interval.
Two commonly accepted methods were used to evaluate clinical significance of improvement in symptoms: a decrease of ≥50% from baseline value, and a reduction below a cut-point associated with diagnosis of major depression. With respect to these categorical outcomes, 17.2% of patients in the collaborative care group had SCL scores that were <50% of their baseline value at month 3 and 18.1% did so at month 9. These values were not significantly different from the 11.8% and 15.1% of CL care patients with such reductions at months 3 and 9, respectively. Using SCL scores of ≥1.75 as a cutoff for indication of major depression, 65% of collaborative care patients were depressed at baseline compared to 55% of the CL group. A stratified analysis showed that the only significant transition was that the collaborative care group patients who were depressed at baseline using this indication were less likely to continue to be depressed at 3 months (Mantel-Haenszel odds ratio, 1.64; 95% confidence interval [CI], 1.00 to 2.70). No significant differences were found at 9 months.
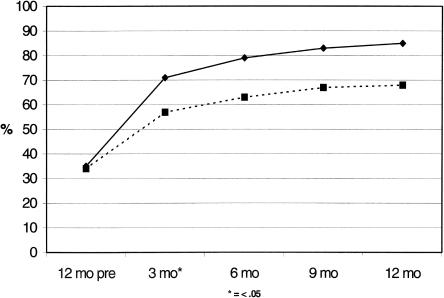
A total of 80% of collaborative care patients received prescriptions for antidepressants during the 9-month treatment trial, compared to 62% for CL care (P < .0001; Fig. 2). Of the patients who were on antidepressants, however, the adequacy of therapy was not significantly different between the 2 treatment groups (Table 3). During the acute-treatment phase, 22% of collaborative care patients attended a CBT group, compared to 0% for CL care.
FIGURE 2.
Antidepressant medications: patients with 1 or more prescriptions.
Table 3.
Antidepressant Medication Adequacy
| Adequacy Criterion | Collaborative Care, % (n = 135) | Consult-liason Care, % (n = 115) |
|---|---|---|
| Minimum dose for 30 d | 81.5 | 78.3 |
| Minimum dose for 90 d | 65.2 | 63.5 |
| Twice minimum for 30 d | 72.6 | 73 |
| Twice minimum for 90 d | 51.1 | 53 |
Effects on Health Status and Satisfaction
The collaborative care group improved significantly on the Sheehan Disability Scale from baseline to 3 months compared to the CL care group (Table 2), with no significant difference at 9 months. With respect to general health status (Veterans SF-36; Table 2), the collaborative care group demonstrated statistically and clinically significant improvements on the MCS compared to CL care at 3 months (difference in mean MCS change of 3.35; 95% CI, 0.79 to 5.91) and at 9 months (difference in mean MCS change of 3.49; 95% CI, 0.70 to 6.28), in unadjusted analyses. After adjustment for baseline MCS score, demographic variables, history of prior depressive episodes, and potential provider clustering, the estimated treatment effect is attenuated with a confidence interval for the 3 month comparison equal to −0.09 to 4.66 (P = .06) and for 9 months equal to −0.45 to 5.19 (P = .10). Difference in the number of prior depressive episodes appeared to account for most of this attenuation. A difference of one-half standard deviation (5 points) is considered clinically significant. A greater proportion of collaborative care patients exhibited an improvement in MCS score of ≥5 points from baseline to 9 months compared to CL care patients (45% vs 36%), and fewer collaborative care patients had a ≥5 point reduction (15% vs 25%). A test for trend comparing the percent of patients with +5, −5 to +5, and less than −5 is significant with P = .03. Change in MCS score was not related to referral source. We observed declines in the PCS score in both the collaborative and CL groups, with a statistically significant decrease in collaborative care PCS from baseline to 9 months.
Patients in both treatment groups were highly and equally satisfied with their primary care providers. Averages of the 5-item satisfaction scale were 86.2% for collaborative care and 84.4% for CL care at 3 months and 85.8% and 86.4%, respectively, at 9 months. Based on an overall measure of satisfaction with their treatment for depression, whether delivered by the primary care provider or other staff, 81.6% of collaborative care patients were satisfied at 3 months compared to 81.8% of CL care patients and 87.2% and 76.9%, respectively, were satisfied at 9 months, with no significant differences between groups.
DISCUSSION
Our collaborative care intervention resulted in more-rapid improvement in depression symptomatology and a more-rapid and sustained improvement in mental health status compared to a consult-liaison model that resembled the primary care–mental health relationship that exists in many primary care settings. Although there was some variability between the 2 groups in the amount of change in the SCL, SF-36 MCS, and Sheehan scales 3 and 9 months after enrollment, all significant differences favored collaborative care. Analyses adjusting for patient baseline characteristics remained significant with one exception.
To help put our findings into context, we can compare our results with the findings from a study also using the SF-36 MCS as a study outcome.45 This study of a general primary care population aged 18 to 64 compared the effectiveness of nortriptyline or 20 sessions of interpersonal psychotherapy with usual care. They found a mean change of 15 points on the SF-36 MCS in the treatment group and 9.7 in usual care, for a difference of means of 5.3. We found smaller changes and differences (mean changes of 5.69 points for collaborative care, and 2.20 for CL, for a difference of means of 3.49 points).
Our result was obtained in spite of the fact that the CL patients were screened for depression, their providers were notified of the diagnosis, and the CL providers received the same educational intervention as the collaborative care providers. In addition, the patients' access to mental health specialty care was facilitated by the study team, resulting in the CL patients having more face-to-face treatment with mental health specialists (psychiatry residents) than the collaborative care patients and exposure to mental health specialty clinic treatment equal to that of the collaborative care patients. In a different setting, in which mental health services were less-routinely available, the collaborative intervention that we tested might have had an even more favorable effect.
These positive results were also obtained despite our less-intensive collaborative care intervention, compared to those evaluated by Katon et al., upon which this intervention was originally based.19,20 The first of these19 evaluated an intervention in which psychiatrists met with and prescribed antidepressant medications directly to patients, rather than, as in this study, evaluating data collected by a psychology technician and offering treatment suggestions to the primary care provider without seeing the patient. In the second study by Katon et al.,20 clinical psychologists met with patients individually 4 to 6 times during treatment, as compared with our brief social work telephone calls and CBT group availability. The Katon et al. studies were also conducted in a staff model HMO with full-time primary care providers and a considerably different patient population. Patients in our study possessed a number of characteristics that have been shown to predict difficulties with treatment, such as older age (our patients are an average of 15 years older), less education, higher unemployment, a much greater prevalence of chronic illness (CDS of 3.57 vs 0.6), and more psychiatric comorbidity (e.g., coexistent posttraumatic stress disorder and alcohol abuse). Thus, our findings are important in demonstrating that relatively small changes in the organization and delivery of mental health services can provide measurable benefits, even for a very difficult patient population.
This study demonstrated significant differences in outcome; future studies of the intervention components will be necessary to establish their relative importance to collaborative care. However, the primary treatment differences between our 2 groups were the systematic formulation and communication of a treatment plan, and the systematic evaluation of patient progress and subsequent plan reformulation. Our results suggest that simply providing services without adequate communication, coordination, and follow-up does not produce optimal results.
An important factor in the effectiveness of collaborative care is the experience and involvement of primary care providers.46 Despite the fact that most attending physicians in this academic setting were present in the clinic only 20% to 30% of the time, they usually acknowledged and acted upon depression treatment information in a timely fashion, as did nurse practitioners. Residents, however, often required repeated communications before they acted. In 5 cases, the diagnostic alert never was acknowledged and the team psychiatrist met with the patient to begin treatment.
The results of this study add to and extend evidence from various settings that effective treatment of depression requires efficient collaboration between primary care providers and mental health specialists based on a chronic illness care model.15,17,47 Some health care systems, such as VA, have taken steps to implement such a model by establishing guidelines and performance measures to increase screening for depression in primary care and continuity of care following depression detection. Our experience is that clinic structure, relationships between general and specialty providers, and performance incentives are critical factors.
Given available resources, we would make 2 changes to our collaborative intervention to attempt to prolong its effects. First, we would strive for a greater degree of symptomatic improvement in the acute-treatment phase, since evidence suggests that this decreases the probability of relapse.48 Second, we would put most of our social work telephone follow-up resources into assisting with acute phase treatment. We think that intensifying and prolonging care management in the maintenance phase of treatment would help consolidate and protect symptomatic improvement in this chronic population.
After our research involvement was completed, our clinic continued to do systematic depression screening and evaluation and to support close collaboration between primary care and mental health disciplines. We have also undertaken several modifications designed in part to better sustain change in depression outcomes. Our multidisciplinary treatment team has become the standard of care and expanded to include the psychiatry residents who rotate through the clinic. An attending psychiatrist now has a part-time clinic within the primary care clinic to assist with the treatment of refractory depression. The team selectively monitors patients at high risk for relapse and uses the stepped-care model to refer patients who are not improving to mental health specialty clinics. In summary, we are attempting to use in-clinic and specialty mental health resources most effectively through a combination of in-clinic collaboration and coordinated referral.
Adopting population-based treatment care management through telephone follow-up can be difficult. One requirement is to identify the appropriate clinic staff to perform this function and then integrate this activity with other duties. Our experience and other studies22,49 suggest that staff performing this care management function need telephone assessment and triage skills but do not need to be psychotherapists or prescribers. Lack of system incentives in the form of workload credit or reimbursement is a major barrier.
A follow-up study50 based on the results of this study and others cited here is now in progress to address the major limitation of this study: the potential limitation in generalizability beyond this single clinic. This multisite program will provide collaborative care toolkits, improve informatics, and test methods of care management that will provide policy makers with data on which to base redesign of system incentives to support improved chronic illness care.
Acknowledgments
This report presents the findings and conclusions of the authors. It does not necessarily represent those of the VA or HSR&D Service.
The Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service supported this research.
REFERENCES
- 1.Kazis LE, Ren XS, Lee A, et al. Health status in VA patients: results from the Veterans Health Study. Am J Med Qual. 1999;14:28–38. doi: 10.1177/106286069901400105. [DOI] [PubMed] [Google Scholar]
- 2.Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52:11–9. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- 3.Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Results from the WHO Collaborative Study on Psychological Problems in General Health Care. JAMA. 1994;272:1741–48. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- 4.Wells KB, Golding JM, Burnam MA. Chronic medical conditions in a sample of the general population with anxiety, affective, and substance use disorders. Am J Psychiatry. 1989;146:1440–6. doi: 10.1176/ajp.146.11.1440. [DOI] [PubMed] [Google Scholar]
- 5.Katon W. The epidemiology of depression in medical care. Int J Psychiatry Med. 1987;17:93–110. doi: 10.2190/xe8w-glcj-kem6-39fh. [DOI] [PubMed] [Google Scholar]
- 6.Narrow WE, Regier DA, Rae DS, Manderscheid RW, Locke BZ. Use of services by persons with mental and addictive disorders. Findings from the National Institute of Mental Health Epidemiologic Catchment Area Program. Arch Gen Psychiatry. 1993;50:95–107. doi: 10.1001/archpsyc.1993.01820140017002. [DOI] [PubMed] [Google Scholar]
- 7.Coyne JC, Schwenk TL, Fechner BS. Nondetection of depression by primary care physicians reconsidered. Gen Hosp Psychiatry. 1995;17:3–12. doi: 10.1016/0163-8343(94)00056-j. [DOI] [PubMed] [Google Scholar]
- 8.Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED. Older age and the underreporting of depressive symptoms. J Am Geriatr Soc. 1995;43:216–21. doi: 10.1111/j.1532-5415.1995.tb07325.x. [DOI] [PubMed] [Google Scholar]
- 9.Magruder HK, Zung WW, Feussner JR, Alling W, Saunders WB, Stevens HA. Management of general medical patients with symptoms of depression. Gen Hosp Psychiatry. 1989;11:201–6. doi: 10.1016/0163-8343(89)90042-x. [DOI] [PubMed] [Google Scholar]
- 10.Simon GE, VonKorff M, Wagner EH, Barlow W. Patterns of antidepressant use in community practice. Gen Hosp Psychiatry. 1993;15:399–408. doi: 10.1016/0163-8343(93)90009-d. [DOI] [PubMed] [Google Scholar]
- 11.Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID): history, rationale, and description. Arch Gen Psychiatry. 1992;49:624–29. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 12.Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depression in primary care practice: an update of the Agency for Health Care Policy and Research Practice Guidelines. Arch Gen Psychiatry. 1998;55:1121–27. doi: 10.1001/archpsyc.55.12.1121. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg HI, Wagner EH, Fihn SD, et al. A randomized controlled trial of CQI teams and academic detailing: can they alter compliance with guidelines? Jt Comm J Qual Improv. 1998;24:130–42. doi: 10.1016/s1070-3241(16)30367-4. [DOI] [PubMed] [Google Scholar]
- 14.Horowitz CR, Goldberg HI, Martin DP, et al. Conducting a randomized controlled trial of CQI and academic detailing to implement clinical guidelines. Jt Comm J Qual Improv. 1996;22:734–50. doi: 10.1016/s1070-3241(16)30279-6. [DOI] [PubMed] [Google Scholar]
- 15.Wagner EH, Austin BT, Von Korff M. Improving outcomes in chronic illness. Manag Care Q. 1996;4:12–25. [PubMed] [Google Scholar]
- 16.Katon W, Von Korff M, Lin E, et al. Population-based care of depression: effective disease management strategies to decrease prevalence. Gen Hosp Psychiatry. 1997;19:169–78. doi: 10.1016/s0163-8343(97)00016-9. [DOI] [PubMed] [Google Scholar]
- 17.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 18.Hunkeler EM, Meresman JF, Hargreaves WA, et al. Efficacy of nurse telehealth care and peer support in augmenting treatment of depression in primary care. Arch Fam Med. 2000;9:700–8. doi: 10.1001/archfami.9.8.700. [DOI] [PubMed] [Google Scholar]
- 19.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines. Impact on depression in primary care. JAMA. 1995;273:1026–31. [PubMed] [Google Scholar]
- 20.Katon W, Robinson P, Von Korff M, et al. A multifaceted intervention to improve treatment of depression in primary care. Arch Gen Psychiatry. 1996;53:924–32. doi: 10.1001/archpsyc.1996.01830100072009. [DOI] [PubMed] [Google Scholar]
- 21.Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;56:1109–15. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 22.Wells KB, Sherbourne C, Schoenbaum M, et al. Impact of disseminating quality improvement programs for depression in managed primary care: a randomized controlled trial. JAMA. 2000;283:212–20. doi: 10.1001/jama.283.2.212. [DOI] [PubMed] [Google Scholar]
- 23.Randall M, Kilpatrick KE, Pendergast JF, Jones KR, Vogel WB. Differences in patient characteristics between Veterans Administration and community hospitals. Implications for VA planning. Med Care. 1987;25:1099–104. doi: 10.1097/00005650-198711000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Wolinsky FD, Coe RM, Mosely RR, Homan SM. Veterans' and nonveterans' use of health services. A comparative analysis. Med Care. 1985;23:1358–71. doi: 10.1097/00005650-198512000-00005. [DOI] [PubMed] [Google Scholar]
- 25.Cebul RD. Randomized, controlled trials using the metro firm system. Med Care. 1991;29:JS9–JS18. [PubMed] [Google Scholar]
- 26.Williams JW, Jr, Barrett J, Oxman T, et al. Treatment of dysthymia and minor depression in primary care: a randomized controlled trial in older adults. JAMA. 2000;284:1519–26. doi: 10.1001/jama.284.12.1519. [DOI] [PubMed] [Google Scholar]
- 27.McDonell M, Anderson S, Fihn S. The Ambulatory Care Quality Improvement Project: A Multi-Site Information System for Monitoring Health Outcomes. Washington, DC: Department of Veterans Affairs; 1998. Presented at the Annual Meeting of the Department of Veterans Affairs Health Services Research and Development Service, Washington DC, February 12–14, 1998. [Google Scholar]
- 28.Samet JH, Rollnick S, Barnes H. Beyond CAGE. A brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287–93. doi: 10.1001/archinte.156.20.2287. [DOI] [PubMed] [Google Scholar]
- 29.Simon GE, Revicki D, VonKorff M. Telephone assessment of depression severity. J Psychiatr Res. 1993;27:247–52. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- 30.Department of Veterans Affairs. Major Depressive Disorder Clinical Guidelines. Washington, DC: Department of Veterans Affairs; 1997. [Google Scholar]
- 31.Chilvers C, Dewey M, Fielding K, et al. Antidepressant drugs and generic counseling for treatment of major depression in primary care: randomized trial with patient preference arms. BMJ. 2001;322:772–75. doi: 10.1136/bmj.322.7289.772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Depression Guideline Panel. Depression in Primary Care: Clinical Practice Guideline. Rockville, Md: Agency for Health Care Policy and Research, US Department of Health and Human Services; 1993. Publication Nos. AHCPR 93–0550 and 93–0551. [Google Scholar]
- 33.Brody DS, Khaliq AA, Thompson TL. Patients' perspectives on the management of emotional distress in primary care settings. J Gen Intern Med. 1997;12:403–6. doi: 10.1046/j.1525-1497.1997.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Padesky CA, Greenberger D. Clinician's Guide to Mind Over Mood. New York: The Guilford Press; 1995. [Google Scholar]
- 35.Greenberger D, Padesky CA. Mind Over Mood. New York: The Guilford Press; 1995. [Google Scholar]
- 36.Depression. New York: Time-Life Medical Patient Educational Media; 1996. (Recurrent and Chronic) [videotape] [Google Scholar]
- 37.Derogatis LR, Lipman RS, Rickels R, Uhlenhuth EH, Covi L. The Hopkins Symptom Checklist, a measure of primary symptom dimensions. In: Pichot P, editor. Psychological Measurements in Psychopharmacology: Problems in Pharmacopsychiatry. 7th ed. Basil, Switzerland: Kargerman; 1974. pp. 79–110. [DOI] [PubMed] [Google Scholar]
- 38.Kazis LE. The Veterans SF-36 Health Status Questionnaire: Developments and Application in the Veterans Health Administration. Medical Outcomes Trust Monitor. 2000;5:1–14. [Google Scholar]
- 39.Lin EH, VonKorff M, Russo J, et al. Can depression treatment in primary care reduce disability?: A stepped care approach. Arch Fam Med. 2000;9:1052–58. doi: 10.1001/archfami.9.10.1052. [DOI] [PubMed] [Google Scholar]
- 40.Simon GE, Lin EH, Katon W, et al. Outcomes of “inadequate” antidepressant treatment. J Gen Intern Med. 1995;10:663–70. doi: 10.1007/BF02602759. [DOI] [PubMed] [Google Scholar]
- 41.Saunders K, Simon G, Grothaus L. Assessing the feasibility of using computerized pharmacy refill data to monitor antidepressant treatment on a population basis: a comparison of automated and self-report data. J Clin Epidemiol. 1998;51:883–90. doi: 10.1016/s0895-4356(98)00053-5. [DOI] [PubMed] [Google Scholar]
- 42.Malone DC, Billups SJ, Valuck RJ, Carter BL. Development of a chronic disease indicator score using a Veterans Affairs Medical Center medication database. IMPROVE Investigators. J Clin Epidemiol. 1999;52:551–57. doi: 10.1016/s0895-4356(99)00029-3. [DOI] [PubMed] [Google Scholar]
- 43.VonKorff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 44.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 2001;73:13–22. [Google Scholar]
- 45.Coulehan JL, Schulberg HC, Block MR, Madonia MJ, Rodriguez E. Treating depressed primary care patients improves their physical, mental, and social functioning. Arch Intern Med. 1997;157:1113–20. [PubMed] [Google Scholar]
- 46.Glasgow RE, Hiss RG, Anderson RM, et al. Report of the health care delivery work group: behavioral research related to the establishment of a chronic disease model for diabetes care. Diabetes Care. 2001;24:124–30. doi: 10.2337/diacare.24.1.124. [DOI] [PubMed] [Google Scholar]
- 47.Wagner EH, Glasgow RE, Davis C, et al. Quality improvement in chronic illness care: a collaborative approach. Jt Comm J Qual Improv. 2001;27:63–80. doi: 10.1016/s1070-3241(01)27007-2. [DOI] [PubMed] [Google Scholar]
- 48.Nierenberg AA, Wright EC. Evolution of remission as the new standard in the treatment of depression. J Clin Psychiatry. 1999;60(suppl 22):7–11. [PubMed] [Google Scholar]
- 49.Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320:550–4. doi: 10.1136/bmj.320.7234.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chaney EF, Rubenstein LV, Hedrick SC, Yano EM. Approaches to Guidelines Implementation: Primary Care Depression Treatment. Washington, DC: Department of Veterans Affairs; 2000. Presented at HSR&D Service 18th Annual Meeting, Washington, DC, March 20–24, 2000. [Google Scholar]