Abstract
OBJECTIVE
Determine relationships between age, self-reported health, and satisfaction in a large cohort of hospitalized patients.
DESIGN
Cross-sectional survey.
SETTING
Thirty-one hospitals in a large Midwestern metropolitan area.
PATIENTS/PARTICIPATION
Randomly selected medical and surgical patients (N = 64,900; mean age, 61 years; 56% female; 84% white) discharged during specific time periods from July 1990 to March 1995 who responded to a mailed survey (overall response rate, 48%).
MEASUREMENTS AND MAIN RESULTS
Patients' overall ratings of hospital quality and satisfaction with 5 aspects of care (physician care, nursing care, information provided, discharge instructions, and coordination of care) were measured by a validated survey, which was mailed to patients after discharge. Analyses compared satisfaction in 5 age groups (18 to 35, 36 to 50, 51 to 65, 66 to 80, and > 80 years). Scores for the 5 aspects of care initially increased with age (P < .001) and then declined (P < .001). A similar relationship was found in analyses of the proportion of patients who rated overall quality as “excellent” or “very good.” Satisfaction was also higher in patients with better self-reported health (P < .001). In analyses of patients with poor to fair health, satisfaction scores peaked at age 65 before declining. However, for patients with good to excellent health, scores peaked at age 80. Moreover, declines in satisfaction in older patients were lower in patients with better health. These findings were consistent in multivariable analyses adjusting for potential confounders.
CONCLUSIONS
Satisfaction exhibits a complex relationship with age, with scores increasing until age 65 to 80 and then declining. This relationship was consistent across individual satisfaction scales, but was modified by health status. The results suggest that age and health status should be taken into account when interpreting patient satisfaction data.
Keywords: patient satisfaction, age, health status, quality of health care
Patient satisfaction is a widely used measure of health care quality that has been linked to other outcome measures and to patients' behavioral intentions. For example, patients who are more satisfied with their care are more likely to be compliant with various aspects of treatment1–3 and to return to providers for additional care.4–6 Furthermore, hospitals with higher patient satisfaction scores also have higher ratings of quality, as assessed by physicians and hospital employees.7 For these reasons, patient satisfaction is increasingly being used to evaluate the performance of individual physicians, hospitals, and health plans.6,8,9
However, in addition to the above attributes of care, patient satisfaction has also been shown to vary according to specific demographic and clinical characteristics.10–13 Although prior studies have often yielded conflicting results with respect to the magnitude and direction of associations between patient satisfaction and individual variables, the 2 most consistent and strongest associations have been noted for age and health status. In general, satisfaction appears to be higher in older patients2,4,11–17 and in patients with better overall health.11–15,18 However, most prior studies that have examined relationships between age and satisfaction have examined all patients over a specific age (e.g., 65 years) together and have not distinguished between the “young old” and older cohorts. Moreover, most studies have not examined whether relationships between age and satisfaction may be modified by health status. Given that health status tends to decline in older patients, such interaction effects are likely.
Understanding how patients' baseline characteristics affect patient satisfaction is critical to interpreting patient satisfaction data and to making correct inferences about the effectiveness of specific interventions and the performance of individual providers. Because the elderly are the fastest growing segment of the population and account for a disproportionate share of health care encounters, age-related differences in satisfaction are increasingly relevant. Thus, the current analysis was conducted to more definitively determine relationships between age, self-reported health, and satisfaction in a large cohort of hospitalized patients.
METHODS
Study Design
The study was designed as a cross-sectional, secondary analysis of data collected through the Cleveland Health Quality Choice Program, a regional initiative designed to measure hospital performance in Northeast Ohio that publicly disseminated comparative hospital data for patient satisfaction and several other outcome measures.19,20
Patients
The sample included randomly selected medical and surgical patients aged 18 years and older who were discharged from 31 Cleveland hospitals during specific time periods in 1990 to 1995 (July 1990 – November 1990, July 1991 – May 1992, and December 1992 – March 1995). Eligibility criteria included all discharges from acute care beds with the exception of: i) in-hospital and known post-discharge deaths; ii) discharges to intermediate or long-term care facilities; iii) discharges against medical advice; and iv) admissions for psychiatric care, alcohol or drug dependence, or labor and delivery (International Classification of Diseases, 9th revision, Clinical Modification primary codes 290-334, 630-648, and 650-676; diagnosis-related groups [DRGs] 370-384 and 424-438).
Data Collection
From each participating hospital, roughly 40 patients per month were surveyed. Patients were identified from computerized files of eligible patients that were submitted monthly by hospitals. Surveys were mailed to eligible patients 8 to 12 weeks after discharge and were accompanied by a letter from the chief executive officer of the hospital explaining the purpose of the survey. Postcard reminders were sent to patients 1 week after the initial questionnaire was mailed, and follow-up letters and questionnaires were sent to all nonrespondents 4 weeks after the initial mailing. Survey fields were closed 8 weeks after the initial mailing. Surveys were returned to an independent survey research firm, which performed all data entry and then returned data files to Cleveland Health Quality Choice.
The response rate was 52%, with 70,423 of the 135,199 patients surveyed responding. Respondents to the patient satisfaction survey, as compared to nonrespondents, were older (mean ages ± SD, 61 ± 17 vs 58 ± 20 years; P < .001) and more likely to be female (56% vs 53%; P < .001) and married (62% vs 47%; P < .001). Of the survey respondents, we further excluded 5,511 patients who did not complete the single item on overall health status (see below) and 12 patients in whom age was missing, leaving a final study sample of 64,900 patients (overall response rate of 48%).
Survey Description
Satisfaction with various aspects of care during hospitalization was assessed using the Patient Judgment System.21 The Patient Judgment System is a validated instrument that was developed on the basis of a comprehensive review of prior patient satisfaction literature, analysis of verbatim patient responses to questions about hospital quality, and discussions with focus groups and hospital leaders. Reliability and validity were initially determined during a pilot test of 2,113 patients in 10 hospitals and later reestablished in 5,625 patients from 32 hospitals.7 The instrument includes 10 multi-item scales, that elicit information about specific aspects of care, (e.g., physician care and nursing care) and several single-item indicators of care.
For this study, we selected 5 scales and 1 single-item indicator for analysis. The 5 scales included physician care (6 questions), nursing care (5 questions), information provided (3 questions), discharge instructions (3 questions), and coordination of care (4 questions). The single-item assessment asked patients to rate the overall quality of care and services received from the hospital. A description of the items comprising each scale is shown in Table 1. Patients were also surveyed about race, education level, and insurance type, whereas other demographic data, including age, gender, and marital status, were obtained from electronic hospital files.
Table 1.
Content of the 6 Satisfaction Measures
| Scale | Items | Content |
|---|---|---|
| Physician care | 6 | Physician attention, availability, concern and caring, skill, communication, teamwork |
| Nursing care | 5 | Nursing skill, attention, speed of response, concern and caring, communication |
| Information provided | 3 | Ease of obtaining, clarity of instructions, informing family and friends |
| Discharge instructions | 3 | Discharge efficiency, discharge instructions, attention to postdischarge needs |
| Coordination of care | 4 | Consideration of needs, teamwork of all hospital staff, helpfulness of staff, sensivity |
| Overall quality | 1 | Overall quality of care received during the hospitalization |
For all satisfaction questions, patients responded on a 5-point scale (poor, fair, good, very good, and excellent), which has been previously demonstrated to produce good response variability and to predict patient behavior.22 For scoring purposes, responses to the 5 multi-item scales were transformed to linear ratings ranging from 0 (poor care) to 100 (excellent care). To assess health status, patients were asked to “rate your overall health” during the prior 2 weeks.
Analyses
Patients were classified into 5 a priori age groups (18 to 35, 36 to 50, 51 to 65, 66 to 80, and >80 years). For the 5 multi-item scales, bivariate associations between satisfaction and age and between satisfaction and health status were determined using analysis of variance (ANOVA). Further stratified analyses examined relationships between age and satisfaction within individual levels of health status. If the results of the ANOVA were significant at the P < .05 level, Scheffe's pairwise comparison procedure was used to examine differences in satisfaction between individual age groups, controlling for the potential problem of multiple testing.
For the single item rating overall quality, analyses examined differences across age groups in the proportion of patients who rated their quality as “excellent” or “very good.” Other categorizations (e.g., proportion of patients rating quality as “excellent” or proportion rating health as “fair” or “poor”) yielded generally similar findings.
Finally, for the 5 multi-item scales, independent associations between age and satisfaction were examined using multivariable linear regression while adjusting for health status, education, gender, race, marital status, type of health insurance, and diagnosis. These analyses included indicator variables for the 4 oldest age categories and provided estimates of differences in satisfaction for each of these groups, relative to patients 18 to 35 years of age. Adjustments for diagnosis were made at the level of the individual DRG using the technique of absorption, which is numerically equivalent to creating individual indicator variables for each DRG.23–25
Independent associations between age and the proportion of patients rating overall quality as excellent or very good were determined using logistic regression. This analysis discerned the odds of responding “excellent” or “very good” for different age groups, relative to patients aged 18 to 35, adjusting for gender, race, health status, marital status, insurance, and level of education. In addition, because data for the 5 patient satisfaction scales were not distributed normally and because data transformations (e.g., logarithmic) were unsuccessful in generating normal distributions, we conducted additional logistic regression analyses that contrasted patients who rated all questions in a particular scale as “excellent” or “very good” with all other patients. The proportions of such patients ranged from 51% for discharge instructions to 60% for coordination of care. These analyses discerned the adjusted odds of responding “excellent” or “very good” to all questions for different age groups, relative to patients aged 18 to 35, and yielded nearly identical patterns to the trends observed in the linear regression analyses. The findings suggest that the results of the linear regression analyses are robust in spite of the non-normality of the satisfaction data, and are not presented (but are available from the authors upon request). All analyses were performed using SAS for Windows, Version 8 (SAS Institute, Inc., Cary, NC).
RESULTS
The mean age of patients was 61 years, and 47% were older than 65 years (Table 2). Eighty-four percent of patients reported their health as fair (27%), good (35%), or very good (22%). Forty-four percent of patients were male, and 84% were white. Sixty percent of survey respondents were admitted with a medical, as opposed to surgical, diagnosis as identified by their DRG. The 10 most common DRGs in the study population are listed in Table 2.
Table 2.
Characteristics of the 64,900 Study Patients
| Patient Characteristics | Patients, % (n) |
|---|---|
| Age, y | |
| 18–35 | 9 (6,159) |
| 36–50 | 17 (11,182) |
| 51–65 | 26 (16,985) |
| 66–80 | 39 (25,059) |
| >80 | 8 (5,515) |
| Health status | |
| Poor | 7 (4,485) |
| Fair | 27 (17,435) |
| Good | 35 (22,757) |
| Very good | 22 (14,568) |
| Excellent | 9 (5,655) |
| Gender | |
| Male | 44 (28,282) |
| Female | 56 (36,618) |
| Race | |
| White | 84 (54,635) |
| African American | 11 (6,941) |
| Other | 2 (1,277) |
| Unknown | 3 (2,047) |
| Marital status | |
| Single | 36 (23,282) |
| Married | 59 (37,994) |
| Unknown | 6 (3,624) |
| Education | |
| Less than 9th grade | 9 (5,628) |
| Some high school | 17 (10,733) |
| High school graduate | 31 (19,977) |
| Technical/trade/vocational school | 8 (5,419) |
| Some college | 16 (10,204) |
| 2-Year college graduate | 5 (3,011) |
| 4-Year college graduate | 7 (4,409) |
| Postgraduate | 5 (3,460) |
| Diagnosis | |
| Medical DRG | 60 (37,065) |
| Surgical DRG | 40 (24,467) |
| 10 Most common individual DRGs | |
| 1. Heart failure and shock (127) | 3.8 (2,402) |
| 2. Angina pectoris (140) | 2.9 (1,821) |
| 3. Uterine and adnexa procedure for nonmalignancy without complication or CC (359) | 2.7 (1,735) |
| 4. Chronic obstructive pulmonary disease (88) | 2.5 (1,566) |
| 5. Chest pain (143) | 2.4 (1,496) |
| 6. Percutaneous cardiovascular procedures (112) | 2.2 (1,391) |
| 7. Back and neck procedures without CC (215) | 2.1 (1,327) |
| 8. Major joint and limb reattachment procedures of lower extremity (209) | 2.1 (1,309) |
| 9. Simple pneumonia and pleurisy, age >17 y, with CC (89) | 2.0 (1,278) |
| 10. Esophagitis, gastroenteritis, and miscellaneous digestive disorders, age >17 y, with CC (182) | 1.9 (1,223) |
DRG, diagnosis-related group; CC, comorbid condition.
Although the 5 multi-item satisfaction scales had a possible range of 0 to 100, distributions were skewed toward the higher range of the scale. For each of these measures, scores were >50 for 70% or more of patients. Mean scores were 74.9 ± 23.4 for physician care, 73.0 ± 24.4 for coordination of care, 71.9 ± 23.8 for nursing care, 70.0 ± 23.0 for discharge instructions, and 69.6 ± 25.0 for information provided. Overall quality was rated as “excellent” or “very good” by 69.2% of patients and “fair” or “poor” by only 7.0% of patients.
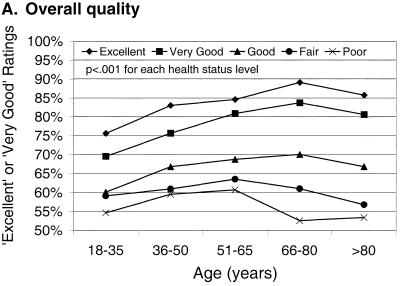
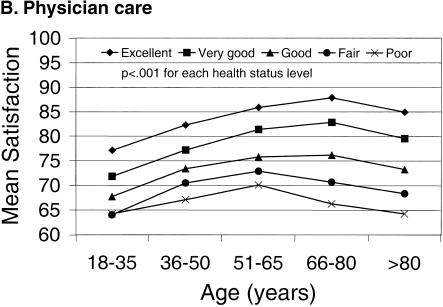
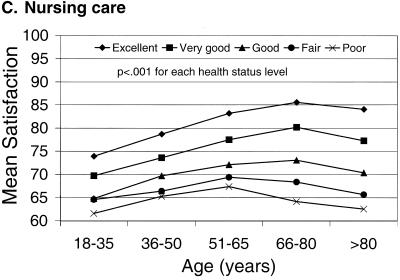
Satisfaction scores for all 5 multi-item scales initially increased (P < .001) until age 65 and then declined (P < .001; Table 3). The percent of patients rating overall quality as “excellent” or “very good” also increased (P < .001) until age 65 and declined (P < .001) in older age groups. For the 5 scales, satisfaction was higher in patients with better self-reported health (Table 4)with the difference in scores between poor and excellent health ranging from 15 to 19 points for the individual scales. The percent of patients reporting overall quality as either “excellent” or “very good” also increased as health status improved.
Table 3.
Differences in Patient Satisfaction Scores According to Age for the 6 Satisfaction Measures
| Age Category (Y)† | |||||
|---|---|---|---|---|---|
| Satisfaction Measure* | 18–35 | 36–50 | 51–65 | 66–80 | >80 |
| Physician care | 70.3 ± 25.9 | 74.9 ± 24.5 | 77.0 ± 22.7 | 75.5 ± 22.6 | 71.3 ± 23.1 |
| Coordination of care | 70.0 ± 26.4 | 72.5 ± 26.1 | 74.3 ± 24.1 | 73.8 ± 23.3 | 69.7 ± 23.6 |
| Nursing care | 68.1 ± 25.5 | 71.3 ± 25.6 | 73.4 ± 23.5 | 72.8 ± 22.7 | 68.8 ± 22.8 |
| Discharge instructions | 66.4 ± 24.7 | 69.2 ± 24.0 | 71.1 ± 22.8 | 70.8 ± 22.3 | 68.1 ± 22.3 |
| Information provided | 66.8 ± 26.7 | 69.6 ± 26.0 | 71.3 ± 24.4 | 70.0 ± 24.3 | 64.9 ± 25.0 |
| Overall quality‡,§ | 65.9 | 70.2 | 71.3 | 69.3 | 63.5 |
Differences between age categories were significant, P < .001, ANOVA. In addition, for each of the scales, mean scores increased (P < .001) between patients 18–35 and 51–65 years, and then decreased (P < .001) between patients 51–65 and >80 years, Scheffe's procedure.
Mean score ±SD.
Percent of patients with rating of “excellent” or “very good.”
Differences between age categories were significant, P < .001. χ2 test. In addition, the proportion of patients with excellent rating increased (P < .001) between patients 18–35 and 51–65 years, and then decreased (P < .001) between patients 51–65 and >80 years. χ2 test for linear trend.
Table 4.
Differences in Patient Satisfaction Scores According to Age for the 6 Satisfaction Measures
| Health Status† | |||||
|---|---|---|---|---|---|
| Satisfaction Measure* | Poor | Fair | Good | Very Good | Excellent |
| Physician care | 66.9 ± 27.8 | 70.6 ± 24.2 | 74.7 ± 22.3 | 79.5 ± 21.4 | 83.3 ± 21.3 |
| Coordination of care | 65.0 ± 28.0 | 68.9 ± 24.8 | 72.7 ± 23.4 | 77.6 ± 22.6 | 81.4 ± 23.4 |
| Nursing care | 64.7 ± 26.9 | 67.8 ± 24.3 | 71.4 ± 22.8 | 76.4 ± 22.0 | 80.4 ± 22.9 |
| Discharge instructions | 63.4 ± 25.9 | 66.1 ± 23.3 | 69.2 ± 22.1 | 74.2 ± 21.5 | 78.9 ± 22.6 |
| Information provided | 60.7 ± 28.7 | 64.9 ± 25.7 | 69.1 ± 23.7 | 74.5 ± 23.2 | 79.5 ± 23.6 |
| Overall quality‡ | 55.7 | 61.1 | 68.2 | 79.1 | 83.2 |
Differences between health status categories were significant, P < .001.
Mean score ±SD.
Percent of patients with rating of “excellent” or “very good.”
Relationships between age and satisfaction were generally similar in analyses stratified by health status. However, for patients rating their health as poor or fair, scores peaked in the 51- to 65-years age group, whereas for patients rating their health as good, very good, or excellent, scores peaked in the 66- to 80-years age group. For all measures, declines in mean satisfaction scores and in the proportion of patients rating over quality as excellent or very good in older patients were less pronounced in patients with better health, compared to patients in poorer health. For example, declines were not statistically significant (P≥ .05) for patients with excellent health for any of the 5 multi-item scales, but were significant (P < .05) for 15 of the 20 possible comparisons across the 5 scales for patients with poor, fair, good, or very good health. Relationships between age and satisfaction, stratified by health status, are shown in Figures 1A – 1C for overall quality, physician care, and nursing care, although relationships were similar for the other measures.
FIGURE 1.
Relationships between age and the proportion of patients rating overall quality as “excellent” or “very good” (A) and between age and mean satisfaction scores for physician care (B) and nursing care (C), stratified according to self-reported health status.
Generally similar relationships between age and satisfaction and between health status and satisfaction were seen in linear regression analyses adjusting for gender, race, marital status, education, diagnosis, and insurance type (Table 5). Satisfaction scores peaked in the 51- to 65-years age group for physician care, information provided, and discharge instructions, and in the 66- to 80-years age group for coordination of care and nursing care. In these analyses, age, health status, gender, race, marital status, education, diagnosis, and insurance type accounted for 6% to 8% of the variance in satisfaction scores. Results for overall quality using logistic regression analysis were similar. The adjusted odds of rating quality as excellent or very good, relative to patients 18 to 35 years of age, peaked in the 51- to 65-years age group and then declined.
Table 5.
Independent Associations Between Satisfaction and Age Adjusting for Gender, Race, Health Status, Marital Status, Insurance, Diagnosis, and Level of Education Using Linear Regression (Five Scales) or Logistic Regression (Single-item Indicator of Overall Quality) Analysis
| Age Category (y)* | ||||
|---|---|---|---|---|
| Satisfaction Measure | 36–50 | 51–65 | 66–80 | >80 |
| Physician care | 5.0 (4.2 to 5.7) | 8.1 (7.4 to 8.9) | 6.6 (5.7 to 7.4) | 4.4 (3.3 to 5.4) |
| Coordination of care | 3.0 (2.2 to 3.8) | 5.3 (4.6 to 6.1) | 5.5 (4.6 to 6.4) | 3.3 (2.2 to 4.3) |
| Nursing care | 3.7 (3.0 to 4.5) | 6.3 (5.5 to 7.0) | 6.4 (5.5 to 7.2) | 4.0 (3.0 to 5.0) |
| Discharge instructions | 3.6 (2.8 to 4.3) | 6.4 (5.6 to 7.1) | 6.3 (5.4 to 7.1) | 4.9 (3.9 to 5.9) |
| Information provided | 3.2 (2.4 to 4.0) | 5.7 (4.9 to 6.5) | 5.1 (4.2 to 6.0) | 2.2 (1.1 to 3.3) |
| Overall quality† | 1.4 (1.3 to 1.5) | 1.6 (1.5 to 1.7) | 1.5 (1.4 to 1.6) | 1.3 (1.2 to 1.4) |
Adjusted difference in satisfaction (95% CI), P < .001 for all values, relative to patients 18 to 35 years.
Adjusted odds of rating of “excellent” or “very good” (95% CI), P < .001 for all values, relative to patients 18 to 35 years.
CI, confidence interval.
DISCUSSION
The current study suggests that patient satisfaction exhibits a complex relationship with age. Examining a large population-based sample of patients discharged from 31 hospitals, we found that patient satisfaction scores increased with age until age 65 to 80 and then declined. We further found that, although better health was associated with greater satisfaction across all age ranges, the relationship between age and satisfaction was modified somewhat by health status. Specifically, declines in satisfaction in older patients were less pronounced in patients with better health. These relationships remained stable even after controlling for potential confounders and were consistent across all 5 distinct domains of satisfaction and for patients' overall ratings of hospital quality.
Most of the existing patient satisfaction literature suggests that patient satisfaction with health care is positively associated with age.2,4,11–17 Interestingly, studies have also suggested that the positive association between age and satisfaction extends to areas outside of health care. In one study of 240 welfare clients in 4 U.S. cities, older clients were more likely to be satisfied with welfare services and with treatment in administrative encounters than were younger clients.26
Most prior studies that have examined the relationship between satisfaction and age have either categorized all patients over age 65 as a single group or have examined age as a continuous variable. One study which did distinguish among older individuals found that, among community-dwelling Medicare beneficiaries 65 years and older, age was inversely related to overall satisfaction with medical care. The authors also found that among this older population, patients in better health rated their care as better.27 This is consistent with the finding in many studies that satisfaction is higher in patients with better health.11–15,18
Whether age-related differences in satisfaction reflect differences in patient expectations of care, differences in perceptions of care, or true differences in care remains unclear. Several theories that have been developed to explain psychosocial determinants of patient satisfaction and that define satisfaction as a balance between expectations for care and delivery of care are likely to be relevant.28
Fulfillment theory defines satisfaction as the perceived simple difference between what an individual desires (or expects) and that which is actually delivered. Discrepancy theory also defines satisfaction as the difference between what is desired and what occurs but postulates that this difference should be viewed in the context of the amount desired. Equity theory defines satisfaction as perceived equity, positing that patients evaluate their balance between expectations and occurrences with their perceptions of the balance of others. Finally, social comparison theory postulates that satisfaction is based upon patients' direct comparisons of the care they received, relative to their perceptions of the care received by others.28,29
A second body of literature has sought to explain differences in satisfaction that may result from differences in perception of treatment.26 The maturational explanation suggests that older individuals are more satisfied with care because they have greater familiarity with the processes of care and greater familiarity with potential shortcomings in the health care delivery system. The generational explanation is based on the nature of the time in which persons are socialized. For example, individuals who were raised during the Great Depression and experienced significant hardships may be more accepting of inadequacies in the health care system than individuals raised in other time periods. Finally, the historical explanation is based on differing reactions between younger and older patients to historical change. For example, older patients may be conditioned to a paternalistic model of care and may find current models, which expect more active patient participation, to be overwhelming and intimidating. Younger patients, however, likely expect to be involved in the decision-making process and would most probably find any alternative unacceptable.
On the basis of these explanations, it is possible that the lower satisfaction of younger patients reflects relatively high expectations that cannot be easily met. As patients become more familiar with health care delivery over time, their expectations may decrease with a resultant increase in their satisfaction. As patients continue to age and develop more health problems that require more health care services and place greater demands on providers, their satisfaction may then decline. Indeed, failure to fulfill patient requests is associated with lower patient satisfaction.30 Alternatively, cohorts within the large diverse elderly population may differ in their historical contexts in ways that affect their assessments of care.
It is also possible that satisfaction may influence health status. However, a prior study using structural equation modeling found that the direction of causation between health status and satisfaction with care was predominantly from the direction of health status to satisfaction31 and that paths going from satisfaction to health over time were not significant. Nonetheless, it is possible that non–health-related factors may influence satisfaction, given that both are based on patient self-reports. For example, individuals who have a negative outlook on life in general may be more likely to both view their health as poor and be dissatisfied with their health care.
When interpreting the results of our study, several limitations must be considered. First, we surveyed only hospitalized patients. Our conclusions may, therefore, not be generalizable to outpatients or to patients not ill enough to require hospitalization. However, our sample did include patients with a wide spectrum of both medical and surgical diagnoses. Second, although we did survey patients from hospitals of varying sizes, our patient population was limited to a single geographic region. Third, the influence of the nonresponse bias remains uncertain. However, prior studies suggest that differences in satisfaction between respondents and nonrespondents may be relatively small.32 Moreover, we are unaware of prior studies suggesting that relationships between satisfaction and age or health status differ in respondents and nonrespondents.
Fourth, differences in satisfaction scores in different age groups were relatively small, on the order of 2 to 8 points (in multivariable analyses), and were less than one half of the standard deviation for most of the scales. This raises the concern that differences between age groups, while statistically significant, may not be relevant in the context of clinical practice or health policy. However, such differences are similar to or larger than differences that are seen in comparisons of individual providers.7,33 Because such data may be used to select providers or determine reimbursement, we would assert that the differences observed in the current study are likely to be of practical importance.
Fifth, because health status was measured using only a single indicator, it is possible that important domains of health status (i.e., physical, emotional, social, and cognitive) were not measured in this study. Sixth, as is the case with many satisfaction instruments, patients responded using qualitative response categories (poor to excellent), which were transformed to linear scales. While this approach is limited in that it imposes specific quantitative relationships on qualitative responses (e.g., excellent is twice as much satisfaction as good), it provides a practical means to integrate multiple items into scales and is commonly used in the measurement of patient satisfaction, health-related-quality-of-life, and numerous other psychosocial parameters.22,34 For example, many of the questions in the widely used Short Form-36 health status survey convert “poor to excellent” responses to “0 to 100” scores.
Finally, the current study evaluated relationships between age, satisfaction, and health status in a cross-sectional manner. The data do not allow for inferences as to whether care received during hospitalization may have affected patients' health status, and, subsequently their satisfaction with care. However, a prior study that examined health status at both admission and discharge found that changes in health status were not associated with satisfaction, when controlling for health at time of discharge,35 suggesting that satisfaction is more likely to reflect patients' underlying health status than changes in health status due to the effectiveness of hospital care.
Although the above limitations should be considered, the current study represents one of the largest population-based evaluations of patient satisfaction in hospitalized patients. The findings confirm that age and self-reported health status are associated with satisfaction. However, unlike most previous studies, we found that that the relationship between age and satisfaction is complex, with declines in satisfaction among the oldest old.
The elderly represent the fasting growing segment of the U.S. population dynamics and account for a disproportionate share of health care utilization. Given the increasing use of patient satisfaction as a means to evaluate health care quality and determine compensation levels for individual physicians,6,8 it is increasingly important to precisely clarify the empirical relationships between satisfaction and age. We believe that the current study provides such needed information.
In conclusion, satisfaction exhibits a complex relationship with age, with scores increasing until age 65 to 80 and then declining. This relationship was consistent across individual satisfaction scales and levels of health status and remained similar after adjusting for potential confounders. These results suggest that age and health status are important modifiers of satisfaction and should be taken into account when interpreting patient satisfaction data.
Acknowledgments
Dr. Jaipaul was supported by a fellowship from the VA National Quality Scholars Program, Office of Academic Affiliations, Department of Veterans Affairs. Dr. Rosenthal is a Senior Quality Scholar, Office of Academic Affiliations, Department of Veterans Affairs.
REFERENCES
- 1.Weisman CS, Nathanson CA. Professional satisfaction and client outcomes: a comparative organizational analysis. Med Care. 1985;23:1179–92. doi: 10.1097/00005650-198510000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Linn MW, Linn BS, Stein SR. Satisfaction with ambulatory care and compliance in older patients. Med Care. 1982;20:606–14. doi: 10.1097/00005650-198206000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Francis V, Korsch BM, Morris MJ. Gaps in doctor-patient communication: patients' response to medical advice. N Engl J Med. 1969;280:535–40. doi: 10.1056/NEJM196903062801004. [DOI] [PubMed] [Google Scholar]
- 4.Zastowny TR, Roghmann KJ, Hengst A. Satisfaction with medical care: replications and theoretic reevaluation. Med Care. 1982;21:294–322. doi: 10.1097/00005650-198303000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Marquis MS, Davies AR, Ware JE. Patient satisfaction and change in medical care provider: a longitudinal study. Med Care. 1983;21:821–9. doi: 10.1097/00005650-198308000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE. Patients' ratings of outpatient visits in different practice settings. JAMA. 1993;270:835–40. [PubMed] [Google Scholar]
- 7.Nelson EC, Hays RD, Larson C, Batalden PB. The patient judgment system: reliability and validity. QRB Qual Rev Bull. 1989;15:185–91. doi: 10.1016/s0097-5990(16)30290-1. [DOI] [PubMed] [Google Scholar]
- 8.Gold M, Wooldridge J. Surveying consumer satisfaction to assess managed-care quality: current practices. Health Care Financ Rev. 1995;16:155–73. [PMC free article] [PubMed] [Google Scholar]
- 9.Dull VT, Lansky D, Davis N. Evaluating a patient satisfaction survey for maximum benefit. Jt Comm J Qual Improv. 1994;20:444–53. doi: 10.1016/s1070-3241(16)30089-x. [DOI] [PubMed] [Google Scholar]
- 10.Fox JG, Storms DM. A different approach to sociodemographic predictors of satisfaction with health care. Soc Sci Med. 1981;15A:557–64. doi: 10.1016/0271-7123(81)90079-1. [DOI] [PubMed] [Google Scholar]
- 11.Cleary PD, Edgman-Levitan S, Roberts M, et al. Patients evaluate their hospital care: a national survey. Health Aff (Millwood) 1991;10:254–67. doi: 10.1377/hlthaff.10.4.254. [DOI] [PubMed] [Google Scholar]
- 12.Young GJ, Meterko M, Desai KR. Patient satisfaction with hospital care. Med Care. 2000;38:325–34. doi: 10.1097/00005650-200003000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Tucker JL, Kelley VA. The influence of patient sociodemographic characteristics on patient satisfaction. Mil Med. 2000;165:72–6. [PubMed] [Google Scholar]
- 14.Zaslavsky AM, Zaborski L, Cleary PD. Does the effect of respondent characteristics on consumer assessment vary across health plans? Med Care Res Rev. 2000;57:379–94. doi: 10.1177/107755870005700307. [DOI] [PubMed] [Google Scholar]
- 15.Cleary PD, Edgman-Levitan S, McMullen W, Delbanco TL. The relationship between reported problems and patient summary evaluations of hospital care. QRB Qual Rev Bull. 1992;18:53–9. doi: 10.1016/s0097-5990(16)30507-3. [DOI] [PubMed] [Google Scholar]
- 16.Carmel S. Satisfaction with hospitalization: a comparative analysis of three types of services. Soc Sci Med. 1985;21:1243–9. doi: 10.1016/0277-9536(85)90273-4. [DOI] [PubMed] [Google Scholar]
- 17.DiMatteo MR, Hays R. The significance of patients' perceptions of physician conduct: a study of patient satisfaction in a family practice center. J Community Health. 1980;6:18–34. doi: 10.1007/BF01324054. [DOI] [PubMed] [Google Scholar]
- 18.Hall JA, Feldstein M, Fretwell MD, Rowe JW, Epstein AM. Older patients' health status and satisfaction with medical care in an HMO population. Med Care. 1990;28:261–70. doi: 10.1097/00005650-199003000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Rosenthal GE, Harper DL. Cleveland health quality choice: a model for collaborative community-based outcomes assessment. Jt Comm J Qual Improv. 1994;20:425–42. doi: 10.1016/s1070-3241(16)30088-8. [DOI] [PubMed] [Google Scholar]
- 20.Rosenthal GE, Hammar PJ, Way LE, et al. Using hospital performance data in quality improvement: the Cleveland health quality choice experience. Jt Comm J Qual Improv. 1998;24:347–60. doi: 10.1016/s1070-3241(16)30386-8. [DOI] [PubMed] [Google Scholar]
- 21.Rubin HR, Ware JE, Nelson EC, Meterko M. The patient judgments of hospital quality (PJHQ) questionnaire. Med Care. 1990;28:17S–18S. doi: 10.1097/00005650-199009001-00005. [DOI] [PubMed] [Google Scholar]
- 22.Ware JE, Hays RD. Methods for measuring patient satisfaction with specific medical encounters. Med Care. 1988;26:393–402. doi: 10.1097/00005650-198804000-00008. [DOI] [PubMed] [Google Scholar]
- 23.SAS Institute Inc. SAS/STAT User's Guide, Version 6. Carey, NC: SAS Insitute, Inc.; 1989. The GLM procedure; pp. 891–996. In: [Google Scholar]
- 24.Jencks SF, Kay T. Do frail, disabled, poor, and very old Medicare beneficiaries have higher hospital charges? JAMA. 1987;257:198–202. [PubMed] [Google Scholar]
- 25.Searle SR. Linear Models. New York, NY: John Wiley and Sons Inc; 1971. [Google Scholar]
- 26.Goodsell CT. The contented older client of bureaucracy. Int J Aging Hum Dev. 198182;14:1–9. doi: 10.2190/m5ty-46xe-u09y-k21k. [DOI] [PubMed] [Google Scholar]
- 27.Lee Y, Kasper JD. Assessment of medical care by elderly people: general satisfaction and physician quality. Health Serv Res. 1998;32:741–57. [PMC free article] [PubMed] [Google Scholar]
- 28.Linder-Pelz S. Toward a theory of patient satisfaction. Soc Sci Med. 1982;16:577–82. doi: 10.1016/0277-9536(82)90311-2. [DOI] [PubMed] [Google Scholar]
- 29.Linder-Pelz S. Social psychological determinants of patient satisfaction: a test of five hypotheses. Soc Sci Med. 1982;16:583–9. doi: 10.1016/0277-9536(82)90312-4. [DOI] [PubMed] [Google Scholar]
- 30.Like R, Zyzanski SJ. Patient satisfaction with the clinical encounter: social psychological determinants. Soc Sci Med. 1987;24:351–7. doi: 10.1016/0277-9536(87)90153-5. [DOI] [PubMed] [Google Scholar]
- 31.Hall JA, Milburn MA, Epstein AM. A causal model of health status and satisfaction with medical care. Med Care. 1993;31:84–94. doi: 10.1097/00005650-199301000-00007. [DOI] [PubMed] [Google Scholar]
- 32.Lasek RJ, Barkley W, Harper DL, Rosenthal GE. An evaluation of the impact of nonresponse bias on patient satisfaction surveys. Med Care. 1997;35:646–52. doi: 10.1097/00005650-199706000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Finkelstein BS, Harper DL, Rosenthal GE. Patient assessments of hospital maternity care: a useful tool for consumers. Health Serv Res. 1999;34:623–40. [PMC free article] [PubMed] [Google Scholar]
- 34.McDowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. 2nd ed. New York: Oxford University Press; 1996. [Google Scholar]
- 35.Covinsky KE, Rosenthal GE, Chren M, et al. The relation between health status changes and patient satisfaction in older hospitalized medical patients. J Gen Intern Med. 1998;13:223–9. doi: 10.1046/j.1525-1497.1998.00071.x. [DOI] [PMC free article] [PubMed] [Google Scholar]