Abstract
OBJECTIVES
To determine the effectiveness of an educational intervention designed to improve physicians' knowledge of drug costs and foster willingness to consider costs when prescribing.
DESIGN
Pre- and post-intervention evaluation, using physicians as their own controls.
SETTING
Four teaching hospitals, affiliated with 2 residency programs, in New York City and northern New Jersey.
PARTICIPANTS
One hundred forty-six internal medicine house officers and attendings evaluated the intervention (71% response rate). Of these, 109 had also participated in a pre-intervention survey.
INTERVENTION
An interactive teaching conference and distribution of a pocket guide, which listed the average wholesale prices of over 100 medications commonly used in primary care
MEASUREMENTS AND MAIN RESULTS
We administered a written survey, before and 6 months after the intervention. Changes in attitudes and knowledge were assessed, using physicians as their own controls, with Wilcoxon matched-pairs signed-rank tests. Eighty-five percent of respondents reported receiving the pocket guide and 46% reported attending 1 of the teaching conferences. Of those who received the pocket guide, nearly two thirds (62%) reported using it once a month or more, and more than half (54%) rated it as moderately or very useful. Compared to their baseline responses, physicians after the intervention were more likely to ask patients about their out-of-pocket drug costs (22% before vs 27% after; P < .01) and less likely to feel unaware of drug costs (78% before vs 72% after; P = .02). After the intervention, physicians also reported more concern about the cost of drugs when prescribing for patients with Medicare (58% before vs 72% after; P < .01) or no insurance (90% before vs 98% after; P < .01). Knowledge of the costs of 33 drugs was more accurate after the intervention than before (P < .05).
CONCLUSION
Our brief educational intervention led to modest improvements in physicians' knowledge of medication costs and their willingness to consider costs when prescribing. Future research could incorporate more high-intensity strategies, such as outreach visits, and target specific prescribing behaviors.
Keywords: drug costs, knowledge, attitudes, physicians, questionnaires
Expenditures for prescription drugs reached $100 billion in 19991 and comprise the fastest growing component of personal health expenditures.2 Among those most affected by rising costs are the 13 million Medicare beneficiaries who have no insurance coverage for medications outside the hospital.3,4 For these elderly Americans, the average cost per prescription has increased from $28.50 in 1992 to $42.30 in 2000.5 When the cost exceeds what patients can afford, prescriptions may go unfilled or drugs may be used less frequently than directed.6 This poor adherence can result in compromised patient health.6 The lack of drug coverage for Medicare beneficiaries has received substantial national attention recently, but there is no political consensus yet as to how to solve the problem.3,6,7
Expenditures for prescription drugs have been rising, in part due to increases in the prices of drugs, but also due to increases in the number of prescriptions written and greater utilization of expensive medications.5,8 If physicians are unaware of the costs of medications, they may unknowingly prescribe regimens that their patients cannot afford and thus cannot follow. In a previous study, we found that physicians were interested in prescribing cost-effectively, but most felt unaware of the actual drug costs and few had received formal education on drug costs.9 Many physicians also seemed unaware that Medicare does not provide outpatient drug coverage. In addition, physicians tended to underestimate the actual costs of 33 medications commonly used in primary care. This study confirmed that a deficit in physicians' knowledge has persisted since it was first recognized in the 1980s and early 1990s.10–19
To address this problem, we developed a brief, multifaceted educational intervention for house officers and attending physicians affiliated with 2 internal medicine residency programs. The purpose of the intervention was to encourage and enable physicians to consider both the cost of drugs and patients' insurance coverage when prescribing, a process we call “cost-conscious prescribing.” The goal of this study was to describe physicians' responses to the intervention, as well as its effect on their knowledge of drug costs and willingness to consider costs when prescribing. Our specific aims were: 1) to assess acceptance of the intervention among all who were exposed, 2) to measure changes in attitudes and knowledge among those physicians for whom both pre- and post-intervention responses were available, and 3) to determine any differences in these outcomes between house officers and attendings.
METHODS
Pre-intervention Survey
Although the methods of the pre-intervention survey have been reported previously,9 we will briefly summarize them for clarity. The intended sample for the pre-intervention survey included: all attending physicians in a Division of General Internal Medicine at an academic medical center in New York City (N = 47), internal medicine house officers at the same urban center (N = 194), and internal medicine house officers at a community teaching hospital in suburban New Jersey (N = 40). We distributed written surveys to all 281 of these physicians in 1998. Each nonrespondent received up to 2 reminder surveys within 2 months of the original. The physicians we sampled write nearly all the prescriptions for their hospital-based primary care clinics. Of note, these clinics do not have their own pharmacies. Therefore, they are not subject to hospital formularies, and they serve patients who fill their prescriptions at outside pharmacies.
The survey included questions regarding demographic variables, attitudes (willingness to consider cost when prescribing), and knowledge of actual drug costs. The following demographic variables were collected: gender, level of training, and year of graduation from medical school. Physicians were asked to agree or disagree with statements about the relevance of cost for prescribing, using a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. Physicians were then asked to agree or disagree with statements about medication costs for patients with a particular insurance type (Medicare, Medicaid, self-pay or health maintenance organization). Finally, physicians estimated the average wholesale price (AWP) for each of 33 commonly used outpatient medications, based on a 30-day supply of each drug or a 10-day supply in the case of antimicrobials. Respondents were given a choice of 5 price categories for each drug ($1 to $10, $11 to $30, $31 to $50, $51 to $80, >$80). The 33 medications were selected from longer lists of the most frequently prescribed drugs in the United States,20,21 adapted to reflect medications commonly used in our local primary care practices. The survey included a variety of generic and brand-name drugs of varying costs. The drugs spanned several therapeutic classes, including analgesics, antimicrobials, antihypertensives, diabetes mellitus medications, antisecretory agents, antidepressants, and asthma medications, among others (see Appendix A).
Description of the Intervention
We created an 8-page pocket guide that contained the average wholesale prices of over 100 drugs commonly used in primary care. The drugs were selected from the same lists used previously of the most frequently prescribed drugs in the United States,20,21 adapted to reflect our local prescribing practices. The drugs were organized by pharmaceutical class and listed alphabetically within each class. Each drug was listed by its chemical name (with trade name added where applicable), with its usual dose, the AWP and relative cost. The guide also noted that the retail price is usually 30% higher than the AWP. The AWP listed was for a 30-day supply of each drug (or a 10-day supply in the case of antimicrobials) in 1998. The relative cost categories corresponded with the categories in the baseline survey ($ = $1 to $10; $$ = $11 to $30; $$$ = $31 to $50; $$$$ = $51 to $80; $$$$$ > $80). Cost information was obtained from The Medical Letter22 and the pharmacy Red Book.23
We also conducted a 45-minute noon conference for house officers. This conference was repeated at the 4 hospitals through which the house officers rotate, with each house officer being potentially exposed to the conference only once. We conducted a similar conference for attendings during a regularly scheduled staff meeting. At these conferences, we discussed insurance coverage and how it impacts the cost of drugs to patients. We emphasized the lack of drug coverage for Medicare patients. We distributed the pocket guide during the conference and then discussed hypothetical cases, using the guide to calculate the costs of several drug regimens. We explained that our goal was not to encourage physicians to choose the cheapest drugs necessarily, but rather to enable them to consider cost when prescribing. Conferences were conducted in November and December 1998. Attendance was taken at all conferences. The pocket guide was distributed by mail to those who did not attend. It was also posted in the precepting rooms of the primary care clinic and posted on the hospital's intranet website (for use from any hospital computer). There was no other part of the residencies' curricula that directly addressed medication costs during the study time period.
Post-intervention Survey
Of the 281 physicians who were eligible for the pre-intervention survey, 61 left the institutions before the intervention was done. Nineteen physicians in the original group were part-time attendings who, by design, were not exposed to the intervention. Six new physicians joined after the pre-intervention survey but before the intervention. We therefore distributed surveys to the remaining 207 physicians eligible for the post-intervention survey, including 30 attendings and 177 house officers.
The post-intervention survey was distributed at a median of 6 months after the intervention and 12 months after the pre-intervention survey. The post-intervention survey was the same as the pre-intervention survey, with the addition of questions to assess attendance at the conferences and receipt of the pocket guide. We also asked respondents to indicate how often they referred to the pocket guide (never, once a year, once a month, once a week, once a day); how useful they found the pocket guide (not useful, a little useful, somewhat useful, moderately useful, very useful); and whether or not they would want the pocket guide to be updated and distributed the following year (definitely not, probably not, no opinion, probably yes, definitely yes). Each nonrespondent received up to 2 reminder surveys within 4 months of the original distribution.
Statistical Analyses
We present descriptive statistics of respondents' characteristics and ratings of the intervention. We used χ2 tests to compare the characteristics of pre- and post-intervention respondents. Physicians were then divided into 2 categories: those with matching data (who completed both pre- and post-intervention surveys) and those without matching data (who completed the post-intervention survey only). The general responses to the intervention (attendance, receipt of the pocket guide, and ratings of the intervention) were compared for these 2 groups using χ2 tests. Subsequent analyses were restricted to those with matching data, in order to assess changes in attitudes and knowledge, using physicians as their own controls. Because respondents could have experienced different facets of the intervention (the conference, the pocket drug cost guide, a posted drug cost guide and/or teaching from a participating attending), we planned to conduct an intention-to-treat analysis. That is, after the intervention, all physicians were considered to have been “exposed.” Because the data were nonparametric, our primary statistical method was the Wilcoxon matched-pairs signed-rank test.24 However, for presentation purposes, we report mean attitude scores as well as the proportion of respondents agreeing with each statement (combining “somewhat agree” and “strongly agree”).
Each drug cost estimate by a respondent was categorized as an underestimate, correct, or an overestimate. The proportion of underestimates, correct answers, and overestimates were calculated for each respondent, in each survey time frame (pre- or post-intervention). The changes in the proportions of underestimates (pre- versus post-intervention) were compared to the null hypothesis of no change, using the Wilcoxon matched-pairs signed-rank test. The same procedure was performed to investigate changes in proportions of correct answers and proportions of overestimates. This analysis was then repeated, stratifying changes in knowledge by drug type (generic versus brand).
Differences in attitudes between house officers and attendings were assessed using χ2 tests. Differences in knowledge between house officers and attendings were assessed using the Wilcoxon rank-sum test.24 All statistical tests were 2-tailed and based on a significance level of α≤ 0.05. Analyses were performed using Stata statistical software (Release 6.0, Stata Corporation, College Station, Tex).
RESULTS
We received completed pre-intervention surveys from 203 of 281 physicians (72% response rate). We received completed post-intervention surveys from 147 of 207 physicians (71% response rate). We will focus on the results of the post-intervention survey and changes across surveys.
Characteristics of Respondents
In the post-intervention survey, 56% of respondents were male (Table 1). Similarly, 50% of nonrespondents were male (P = .45). Eighty percent of respondents were house officers and 20% were attendings. Nonrespondents were more likely to be house officers than attendings (80% of respondents were house officers, 98% of nonrespondents were house officers; P = .001). Although the gender distribution did not change significantly over time, there was a trend toward fewer interns in the post-intervention cohort (P = .06). The median time that attendings had been in practice was 9 years. The 109 physicians who completed both pre- and post-intervention surveys were similar to those who completed only the post-intervention survey.
Table 1.
Characteristics of Respondents
| Pre-intervention (N = 203), n (%) | Post-intervention (N = 147), n (%) | P Value* | Matching Pre- and Post-intervention (N = 109), n % | P Value† | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 117 (58) | 82 (56) | 64 (59) | ||
| Female | 86 (42) | 65 (44) | .73 | 45 (41) | .23 |
| Level of training‡ | |||||
| Attendings | 41 (20) | 29 (20) | 23 (21) | ||
| House staff | 162 (80) | 118 (80) | 86 (79) | ||
| PGY 1 | 81 (40) | 41 (28) | .06 | 31 (28) | |
| PGY 2 | 38 (19) | 42 (29) | 30 (28) | .86 | |
| PGY 3 | 43 (21) | 35 (24) | 25 (23) |
These P values were based on χ2 tests comparing the pre- and post-intervention groups.
These P values were based on χ2 tests comparing those with and without matching data, within the post-intervention group.
Level of training reflects level at the time of survey completion. Respondents with matching pre- and post- data were categorized by level at the time of the post-intervention survey.
PGY, post-graduate year.
General Response to the Intervention
Of the 147 physicians who completed the post-intervention survey, 85% received the pocket guide and 46% attended 1 of the teaching conferences. Of those who received the guide, nearly two thirds (62%) reported using the guide once a month or more. More than half (54%) of physicians who received the guide rated it moderately or very useful. Nearly all those who received the guide (91%) wanted to see it updated and redistributed yearly. Similar responses were observed among the subset of physicians who had completed both pre- and post-intervention surveys.
Changes in Attitudes
Among the 109 physicians who completed both pre- and post-intervention surveys, respondents after the intervention were more likely to report asking their patients about out-of-pocket drug costs (22% before vs 27% after; P < .01) and less likely to feel unaware of drug costs (78% before vs 72% after; P = .02; Table 2).
Table 2.
Effect of the Intervention on Physicians' Willingness to Consider Drug Costs When Prescribing (n = 109)
| Agree, %* | Mean Response† | ||||
|---|---|---|---|---|---|
| Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | P Value‡ | |
| I ask my patients about the cost of drugs to them. | 22 | 27 | 2.8 | 3.1 | <.01 |
| I am often unaware of actual drug costs. | 78 | 72 | 3.9 | 3.7 | .02 |
| I believe cost is an important consideration when prescribing. | 84 | 95 | 4.1 | 4.3 | .20 |
| I have easy access to drug cost information. | 36 | 36 | 2.7 | 2.7 | .94 |
| I am willing to sacrifice some efficacy for affordability. | 72 | 82 | 3.7 | 3.8 | .33 |
| I prefer brand-name drugs to generic regardless of cost. | 10 | 6 | 1.8 | 1.7 | .29 |
Those responding with “Somewhat agree” or “Strongly agree.”
Mean response reflects answers on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree).
These P values are based on our primary statistical method of assessing intervention effectiveness, the Wilcoxon matched-pairs signed-rank test. We compared the matched changes (pre- versus post-intervention) to the null hypothesis of no change.
Among these physicians, there were also changes in their awareness of the implications of different insurance policies for drug coverage (Table 3). Compared to their baseline reports, physicians after the intervention were more concerned about cost for Medicare patients (58% before vs 72% after; P < .01) and those who were self-pay (90% before vs 98% after; P < .01). Physicians after the intervention were less concerned about cost for Medicaid patients (38% before vs 28% after; P < .01).
Table 3.
Effect of the Intervention on Physicians' Concern for Cost, by Patients' Insurance Status (n = 109)
| Agree, %* | Mean response† | ||||
|---|---|---|---|---|---|
| “The cost of medications is more of a concern to me when my patient's insurance is ____.” | Pre-intervention | Post-intervention | Pre-intervention | Post-intervention | P Value‡ |
| Medicare | 58 | 72 | 3.6 | 4.0 | <.01 |
| Self-pay | 90 | 98 | 4.6 | 4.8 | <.01 |
| Medicaid | 38 | 28 | 2.9 | 2.5 | <.01 |
| HMO | 28 | 32 | 2.8 | 2.7 | .47 |
Refers to those responding with “Somewhat agree” or “Strongly agree.”
Mean response reflects answers on a 5-point Likert scale (1 = strongly disagree, 5 = strongly agree).
These P values are based on our primary statistical method of assessing intervention effectiveness, the Wilcoxon matched-pairs signed-rank test. We compared the matched changes (pre- versus post-intervention) to the null hypothesis of no change.
Changes in Knowledge
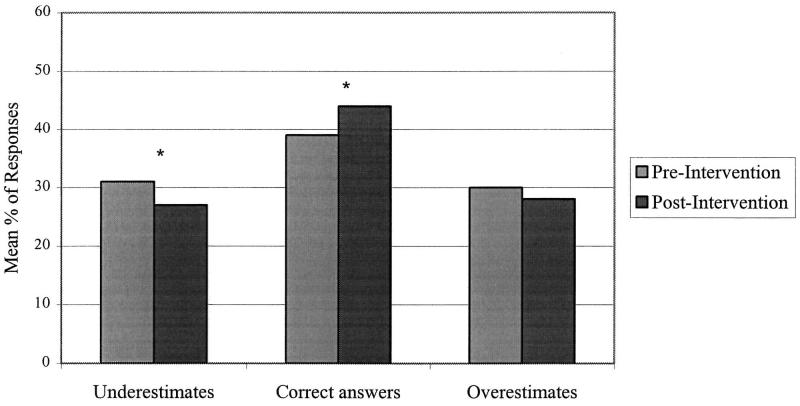
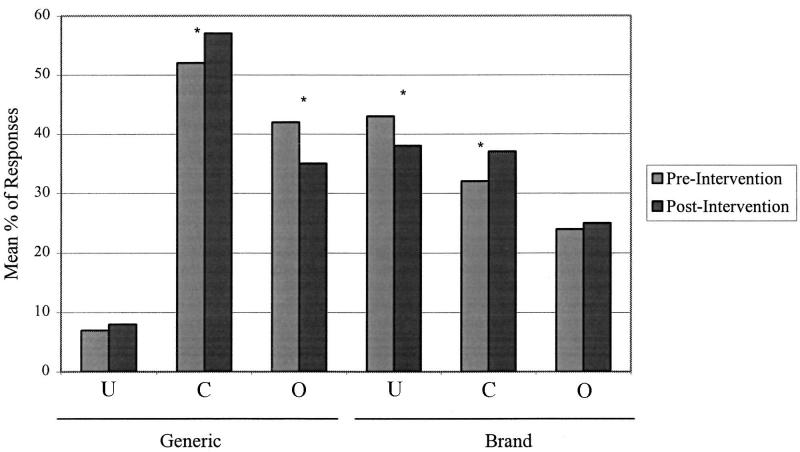
Overall estimates of drug costs were more accurate after the intervention (Fig. 1). The proportion of correctly estimated medication costs increased (39% before vs 44% after; P = .01) and the proportion of underestimates decreased (31% before vs 27% after; P = .04). Drug costs were estimated more accurately after the intervention both for generic drugs and for brand-name drugs (Fig. 2
FIGURE 1.
Overall changes in knowledge of drug costs. *P < .05, comparing pre- and post-intervention responses by Wilcoxon matched-pairs signed-rank test.
FIGURE 2.
Changes in knowledge of drug costs by drug type. *P ≤ .05, comparing pre- and post-intervention responses by Wilcoxon matched-pairs signed-rank test. U, underestimates; C, correct answers; O, overestimates.
Differences Between House Officers and Attendings
There were no differences between house officers and attendings in the rates at which they attended the conferences or received the pocket guides, how often they said they referred to the pocket guide or how useful they rated it. The attitudes of house officers and attendings toward cost-conscious prescribing were similar, except that house officers were still more likely than attendings to feel unaware of drug costs after the intervention (78% of house officers vs 57% of attendings; P = .04). However, there were no significant differences between house officers and attendings in their knowledge of actual drug costs.
DISCUSSION
Our low-intensity educational intervention, consisting of a 1-time teaching conference and a pocket guide listing the costs of over 100 commonly used medications, led to modest improvements in physicians' willingness to consider costs when prescribing. Although the effect size was small, we were able to sensitize physicians to the importance of costs for patients with Medicare, many of whom lack outpatient drug coverage. Using physicians as their own controls, we were also able to demonstrate a small improvement in knowledge of actual drug costs. These improvements applied to both generic and brand-name drugs, across therapeutic classes. Despite these encouraging findings, we were somewhat humbled by the limited effect of the intervention. For example, although physicians reported asking patients about drug costs more often, this was still an uncommon practice. One in four physicians still seemed unaware that Medicare does not pay for outpatient drugs. Knowledge of actual drug costs improved, but underestimates were still fairly common. The intervention did not change willingness to sacrifice efficacy for affordability, nor did it change preferences for generic drugs over brand-name drugs.
There are a number of reasons why our findings might have been modest in magnitude. First, the intervention was relatively brief. Each physician was only exposed to one 45-minute conference, and despite our best efforts, only half of the target audience was in attendance. Attendance is consistently a challenge when designing educational programs for busy clinicians. Second, the pocket guides were designed to be carried by the physicians, ready for use in real time, but we do not know how often the guides were actually carried. Third, physicians may not have tried to memorize drug costs, because they could refer to the pocket guide or because they knew that drug prices would change frequently. Finally, respondents may have been subject to countervailing forces, such as discussions with pharmaceutical representatives or exposure to pharmaceutical advertising, which emphasize attributes of drugs other than cost.
Many studies have documented that physicians are poorly equipped to consider cost when prescribing.9–19 This is not surprising, given the paucity of formal education on this subject in most medical schools and residency training programs. Unfortunately, very few published interventions have addressed these deficiencies. One study was able to show that adding information about drug costs is associated with physicians' choosing more cost-effective drug regimens in hypothetical scenarios.25 However, ours is the first study to our knowledge to demonstrate sustained improvement in attitudes toward cost-conscious prescribing and knowledge of actual drug costs.
Our study had several strengths. First, physicians were used as their own controls, which enabled us to track individuals' changes in attitudes and knowledge over time. Second, because of concerns about recall bias in some educational intervention studies, we intentionally allowed 6 months to elapse before re-surveying the physicians. Our significant findings at the 6-month mark suggest that the improvements we observed were real and sustainable. They also suggest that we may be underestimating the short-term impact of the intervention. Third, the low cost and limited intensity of the intervention maximize the likelihood that it may be replicated elsewhere.
Several limitations merit discussion. There was no concurrent control group in our study. Because of the wide curricular interest in drug costs and insurance policies, the intervention was intentionally not restricted to an experimental group. Therefore, we cannot exclude a secular trend toward greater sensitivity to medication costs. However, drug costs were not a part of the standard curricula, and we found no differences between the knowledge of interns and third-year residents in the baseline survey. This suggests that additional post-graduate training was not sufficient to improve knowledge in the specific area of drug costs. A second limitation is the possibility of selection bias. It is possible that the physicians most interested in drug costs responded, which could lead us to overestimate our effects. Third, because the intervention had multiple components, we cannot distinguish which aspect had the greatest effect. Finally, like all survey research, this study measured attitudes, knowledge, and a few self-reported behaviors but did not record actual behavior.
Some aspects of our intervention may not be generalizable to other settings. For our purposes, the average wholesale price was the best estimate of drug costs in our communities, acknowledging an approximate 30% premium for retail sale. In other settings that are more restricted by formularies, providing actual charges may be more appropriate for a similar intervention. In addition, New York State, like many states, has a law requiring mandatory generic substitution at all pharmacies, unless physicians write the brand name and “DAW,” for “dispense as written.” Our drug cost guide listed the generic prices whenever they were available, but it also highlighted discrepancies between generic and brand-name prices when the difference was particularly striking.
Our findings have different implications for medical education and health care policy. Presented as an educational program, this project was well received by physicians in both academic and community settings. In fact, we received requests for distribution of the pocket guide to other physician groups and requests for more education on health care economics for the practicing physician. From a policy perspective, it is notable that as physicians became more cost-conscious in our study, they took on the perspective of individual patients rather than the perspective of society. If replicated on a larger scale, the greater attention to prescribing for Medicare patients would be good news for both patients and society, while less attention to prescribing for Medicaid or HMO patients would result in little change for patients but higher costs for society. This differential effect of our intervention likely reflects physicians' improved understanding of the insurance programs, including the generous drug benefit in New York's Medicaid program.
In conclusion, we have shown that a brief educational intervention can improve physicians' knowledge of actual drug costs and willingness to consider cost when prescribing. Although the magnitude of our effect was modest, we believe this is still noteworthy, given the larger literature on the challenges of changing physician behavior. Our intervention utilized some strategies previously shown to be effective, such as responding to a needs assessment, teaching with an interactive format, and using a multifaceted approach.26–29 Our conference and drug cost pocket guide could easily be incorporated into other residency programs and/or medical school curricula. Future research could evaluate interventions using hand-held computers, for which drug cost databases are increasingly available.30,31 Future interventions could also target specific prescribing behaviors and use more high-intensity strategies that have been proven to change practice, such as outreach visits and opinion leaders.26–29 We need to encourage physicians to talk with their patients about their ability to pay for medications, especially when adherence to prescribed regimens is a concern.
Acknowledgments
The authors would like to thank Marie Diener-West, PhD, of the Johns Hopkins University Bloomberg School of Public Health for her statistical review. The authors would also like to thank Lawrence Smith, MD, and Albert Siu, MD, MSPH, of the Mount Sinai School of Medicine for their support of the project. We are indebted to all the physicians who participated in the survey.
Dr. Korn was a fellow in the Robert Wood Johnson Foundation Clinical Scholars Program at the time this project was completed. Dr. Halm is supported in part by the Robert Wood Johnson Foundation Generalist Physician Faculty Scholars Program. Funding for the educational intervention was provided by the Department of Medicine, Mount Sinai School of Medicine, New York, NY. The authors have no conflicts of interest to disclose.
APPENDIX A
Drugs Listed on Survey, Categorized by Average Wholesale Price*
| $1 to $10 | $11 to $30 | $31 to $50 | $51 to $80 | >$80 |
|---|---|---|---|---|
| Diphenhydramine (G†) | Albuterol (G) | Beclomethasone dipropionate | Zafirlukast | Troglitazone |
| Acetaminophen (G) | Novolin (G) | Fluticasone propionate | Loratadine | Ranitidine |
| Ibuprofen (G) | Tylenol #3 (G) | Metformin | Fluoxetine | Omeprazole |
| Propranolol (G) | Cimetidine (G) | Naproxen | Nabumetone | Itraconazole |
| HCTZ (G) | Atenolol (G) | Amlodipine | Lovastatin | |
| TMP-SMX (G) | Verapamil SR | Nifedipine XL | Clarithromycin | |
| Erythromycin (G) | Enalapril | Ciprofloxacin | Cefpodoxime | |
| Glipizide |
Average wholesale prices are for a 30-day supply of each drug (or a 10-day supply in the case of antimicrobials) in 1988. The order of these drugs was scrambled for the purposes of the survey and actual costs omitted.
Drugs with generic equivalents are marked with a “G.” All other drugs are considered brand-name drugs. All drugs were listed on the survey by both chemical and trade names where applicable.
HCTZ, hydrochlorothiazide; TMP-SMX, trimethoprim-sulfamethoxazole; SR, sustained-release; XL, extended release.
REFERENCES
- 1.Iglehart JK. Medicare and prescription drugs. N Engl J Med. 2001;344:1010–5. doi: 10.1056/NEJM200103293441311. [DOI] [PubMed] [Google Scholar]
- 2.Iglehart JK. The American health care system—Expenditures. N Engl J Med. 1999;340:70–6. doi: 10.1056/NEJM199901073400122. [DOI] [PubMed] [Google Scholar]
- 3.Pear R. Budget office's estimates for drug spending grow: adding to challenge of Medicare coverage. New York Times. February 24 2001:A7. [Google Scholar]
- 4.Davis M, Poisal J, Chulis G, Zarabozo C, Cooper B. Prescription drug coverage, utilization, and spending among Medicare beneficiaries. Health Aff (Millwood) 1999;18:231–43. doi: 10.1377/hlthaff.18.1.231. [DOI] [PubMed] [Google Scholar]
- 5.Mehl B, Santell J. Projecting future drug expenditures—2001. Am J Health Syst Pharm. 2001;58:125–33. doi: 10.1093/ajhp/58.2.125. [DOI] [PubMed] [Google Scholar]
- 6.Soumerai SB, Ross-Degnan D. Inadequate prescription-drug coverage for Medicare enrollees—A call to action. N Engl J Med. 1999;340:722–8. doi: 10.1056/NEJM199903043400909. [DOI] [PubMed] [Google Scholar]
- 7.Etheredge L. Purchasing Medicare prescription drug benefits: a new proposal. Health Aff (Millwood) 1999;18:7–19. doi: 10.1377/hlthaff.18.4.7. [DOI] [PubMed] [Google Scholar]
- 8.Pear R. Spending on prescription drugs increases by almost 19 percent: doctors are using more of costliest medicines. New York Times. May 8 2001 A1, A16. [Google Scholar]
- 9.Reichert S, Simon T, Halm EA. Physicians' attitudes about prescribing and knowledge of the costs of common medications. Arch Intern Med. 2000;160:2799–803. doi: 10.1001/archinte.160.18.2799. [DOI] [PubMed] [Google Scholar]
- 10.Beringer GB, Biel M, Ziegler DK. Neurologists' knowledge of medication costs. Neurology. 1984;34:121–2. doi: 10.1212/wnl.34.1.121. [DOI] [PubMed] [Google Scholar]
- 11.Fowkes FG. Doctors' knowledge of the costs of medical care. Med Educ. 1985;19:113–7. doi: 10.1111/j.1365-2923.1985.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 12.Glickman L, Bruce EA, Caro FG, Avorn J. Physicians' knowledge of drug costs for the elderly. J Am Geriatr Soc. 1994;42:992–6. doi: 10.1111/j.1532-5415.1994.tb06594.x. [DOI] [PubMed] [Google Scholar]
- 13.Hoffman J, Barefield FA, Ramamurthy S. A survey of physician knowledge of drug costs. J Pain Symptom Manage. 1995;10:432–5. doi: 10.1016/0885-3924(95)00018-t. [DOI] [PubMed] [Google Scholar]
- 14.Miller LG, Blum A. Physician awareness of prescription drug costs: a missing element of drug advertising and promotion. J Fam Pract. 1993;36:33–6. [PubMed] [Google Scholar]
- 15.Oppenheim GL, Erickson SH, Ashworth C. The family physician's knowledge of the cost of prescribed drugs. J Fam Pract. 1981;12:1027–30. [PubMed] [Google Scholar]
- 16.Rowe J, MacVicar S. Doctors' knowledge of the cost of common medications. J Clin Hosp Pharm. 1986;11:365–8. doi: 10.1111/j.1365-2710.1986.tb00865.x. [DOI] [PubMed] [Google Scholar]
- 17.Ryan M, Yule B, Bond C, Taylor RJ. Scottish general practitioners' attitudes and knowledge in respect of prescribing costs. BMJ. 1990;300:1316–8. doi: 10.1136/bmj.300.6735.1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Walzak D, Swindells S, Bhardwaj A. Primary care physicians and the cost of drugs: a study of prescribing practices based on recognition and information sources. J Clin Pharmacol. 1994;34:1159–63. doi: 10.1002/j.1552-4604.1994.tb04726.x. [DOI] [PubMed] [Google Scholar]
- 19.Weber ML, Auger C, Cleroux R. Knowledge of medical students, pediatric residents, and pediatricians about the cost of some medications. Pediatr Pharmacol (New York) 1986;5:281–5. [PubMed] [Google Scholar]
- 20.Cardinale V, editor. 1998 Drug Topics Red Book. Montvale, NJ: Medical Economics Co.; 1998. Top 200 brand-name Rx drugs; p. 130. [Google Scholar]
- 21.Cardinale V, editor. 1998 Drug Topics Red Book. Montvale, NJ: Medical Economics Co.; 1998. Top 200 generic Rx drugs; p. 131. [Google Scholar]
- 22.Abramowicz M, editor. The Medical Letter: On Drugs and Therapeutics. New Rochelle, NY, Feb. 1995 – Aug. 1998.
- 23.Cardinale V. 1998 Drug Topics Red Book. Montvale, NJ: Medical Economics Co.; 1998. ed. [Google Scholar]
- 24.Rosner B. Fundamentals of Biostatistics. 5th ed. Pacific Grove, Calif: Duxbury; 2000. [Google Scholar]
- 25.Salman H, Bergmann M, Hart J, et al. The effect of drug cost on hypertension treatment decision. Public Health. 1999;113:243–6. doi: 10.1038/sj.ph.1900579. [DOI] [PubMed] [Google Scholar]
- 26.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274:700–5. doi: 10.1001/jama.274.9.700. [DOI] [PubMed] [Google Scholar]
- 27.Grimshaw JM, Shirran L, Thomas R, et al. Changing provider behavior: an overview of systematic reviews of interventions. Med Care. 2001;39:II2–45. [PubMed] [Google Scholar]
- 28.Grol R. Improving the quality of medical care: building bridges among professional pride, payer profit, and patient satisfaction. JAMA. 2001;286:2578–85. doi: 10.1001/jama.286.20.2578. [DOI] [PubMed] [Google Scholar]
- 29.Thomson O'Brien MA, Freemantle N, Oxman AD, Wolf F, Davis DA, et al. The Cochrane Library, Issue 2. Oxford: Update Software; 2002. Continuing education meetings and workshops: effects on professional practice and health care outcomes (Cochrane Review) [DOI] [PubMed] [Google Scholar]
- 30. ePocrates Rx. version 4.0. Available at: http://epocrates.com. Accessed September 23, 2002.
- 31.Pocket Pharmacopeia software. Available at: http://tarasonpublishing.com/store/palm.asp. Accessed September 23, 2002.