Abstract
To assess physicians' use of and attitudes toward electronic mail (e-mail) for patient communication, we conducted a mail-in survey of physicians who see patients in outpatient clinics affiliated with a large academic medical center (N = 283). Seventy-two percent of physicians reported using e-mail to communicate with patients, averaging 7.7 e-mails from patients per month. The lowest level of use was by community-based primary care physicians (odds ratio, 0.22; 95% confidence interval, 0.08 to 0.59). Those physicians who reported using e-mail with patients reported high satisfaction with its use. Although physicians were concerned about the confidentiality of e-mail, few discussed this issue with patients.
Keywords: e-mail, patient, communication, survey, confidentially
Approximately 175 million people in the United States were estimated to have access to the Internet in 2001, up from 18 million in 1995.1 The potential of clinical electronic mail (e-mail) to influence the practice of medicine is widely acknowledged.2–5 In fact, the potential of clinical e-mail to impact physicians has been compared to the introduction of the telephone in the late 1800s.5 These factors have led some organizations to publish guidelines on electronic patient-doctor communication,6–8 but it is unknown how often these recommendations are followed. Thus, we set out to examine the frequency of physicians' use of e-mail to communicate with patients, and to assess physicians' clinical practices and attitudes related to its use.
METHODS
Study Population
We used a database maintained by the University of Washington Physicians to identify all physicians who care for patients in outpatient clinics at the University of Washington and its affiliated community-based primary care clinics. These physicians practice in a wide range of clinical settings including: a university hospital, which offers primary and subspecialty care; a public county hospital, which is the principal provider of primary and specialty care to underserved populations in the Seattle area; and a group of neighborhood primary care clinics staffed by full-time clinicians who have relatively little teaching or research activity compared to physicians at the hospital-based sites. All physicians surveyed had individual office computers, private e-mail accounts, and access to electronic medical records. The study's design was reviewed and approved by the University of Washington Human Subjects Committee.
Questionnaire and Data Collection
National guidelines and other published literature were reviewed to generate a list of issues related to the use of patient e-mail in clinical practice.4–7 This list was used to design a self-administered questionnaire focused on 3 domains: frequency of physicians' use of e-mail to communicate with patients, their clinical practices related to its use, and their attitudes toward its use. Specific questions were designed to address adherence to published guidelines, all of which direct physicians to document e-mail communication in the medical record and to discuss the confidentiality of e-mail with their patients.6–8 Respondents also were invited to add free text comments at the end of the survey.
From November 2000 through March 2001, this anonymous questionnaire was mailed to physicians. Physicians were excluded if their questionnaire was returned undeliverable (n = 12), leaving a pool of 283 eligible respondents.
Data Analysis
Primary data groupings for the main analysis were physician practice location. Additional subgroup analyses were performed by practice type, age, and gender. Statistical significance was assessed for continuous variables using t tests and for categorical variables using the Pearson χ2 test. All significance levels were 2-tailed. Stepwise logistic regression was used to calculate odds ratios for the use of patient e-mail by practice site, adjusting for age, gender, and practice type. Analyses were performed using SPSS Version 10.0 (SPSS Inc., Chicago Ill).
RESULTS
Overall, 249 of 283 (88%) physicians returned completed questionnaires. Six physicians who returned blank questionnaires were considered nonresponders. The characteristics of the study group are presented in Table 1. Sixty-one percent of the respondents were male and about one third worked in primary care.
Table 1.
Physicians' Use of E-mail with Patients (N = 249)
| Characteristic | n (%)* | Physicians Who Use E-mail with Patients, n (%) | E-mails per Month, Mean† |
|---|---|---|---|
| Gender | |||
| Female | 93 (37) | 63 (68) | 8.4 |
| Male | 153 (61) | 112 (73) | 7.4 |
| Age, y | |||
| 30–40 | 80 (32) | 58 (73) | 6.8 |
| 41–50 | 103 (41) | 73 (71) | 7.3 |
| 51–60 | 42 (17) | 31 (74) | 9.2 |
| >60 | 18 (7) | 10 (56) | 7.4 |
| Practice location | |||
| University hospital–based clinics | 131 (53) | 107 (82) | 9.8 |
| County hospital–based clinics | 71 (29) | 47 (66)‡ | 5.4§ |
| Community-based primary care clinics | 47 (19) | 24 (51)| | 2.8¶ |
Percentages may not add up to 100 due to rounding and missing responses.
Mean e-mails received from patients per month among physicians who reported using e-mail with patients.
P = .014 compared to university hospital–based clinics.
P = .023 compared to university hospital–based clinics.
P = .001 compared to hospital-based clinics combined.
P < .001 compared to hospital-based clinics combined.
Frequency of Patient-doctor E-mail
Overall, 178 (72%) of respondents reported using e-mail with patients. As shown in Table 1, there were no significant differences in patient e-mail use by physician age or gender. Significant differences were observed by practice site (P < .001), with lower use at the county hospital than at the university hospital (66% vs 82%; P = .014) and lower use at the community primary care clinics than at the 2 hospital-based sites combined (51% vs 76%; P = .001).
A similar pattern emerged for e-mail volume, with physicians at the county hospital estimating that they received fewer patient e-mails per month than those at the university hospital (5.4 vs 9.8; P = .023), and physicians at the community primary care clinics reporting that they received fewer patient e-mails per month than physicians at the 2 hospital-based sites combined (2.8 vs 8.5; P < .001). These differences in use remained when only primary care physicians were included in the analysis (data not shown). Among physicians at the 2 hospital-based sites, use of patient e-mail by primary care physicians was nearly identical to that of specialty care physicians (77% vs 76%).
Adjusting for age, gender, and practice type (primary care vs specialty care) did not significantly alter the observed differences in use of patient e-mail by practice site. The adjusted odds ratios (ORs) and 95% confidence intervals (95% CIs) for patient e-mail use by practice site were as follows: university hospital based clinics = 1.00 (reference); county hospital-based clinics, OR, 0.43; 95% CI, 0.21 to 0.83; community-based primary care clinics, OR, 0.22; 95%CI, 0.08 to 0.59.
Physician Habits and Attitudes
As illustrated in Figure 1, among physicians who reported using e-mail with patients, more than half stated that they never or rarely document this communication in the medical record. Few physicians discussed confidentiality of e-mail with patients, and more than half reported that they never obtain consent from patients for e-mail communication. Most physicians were satisfied with their e-mail communication with patients all or most of the time.
FIGURE 1.
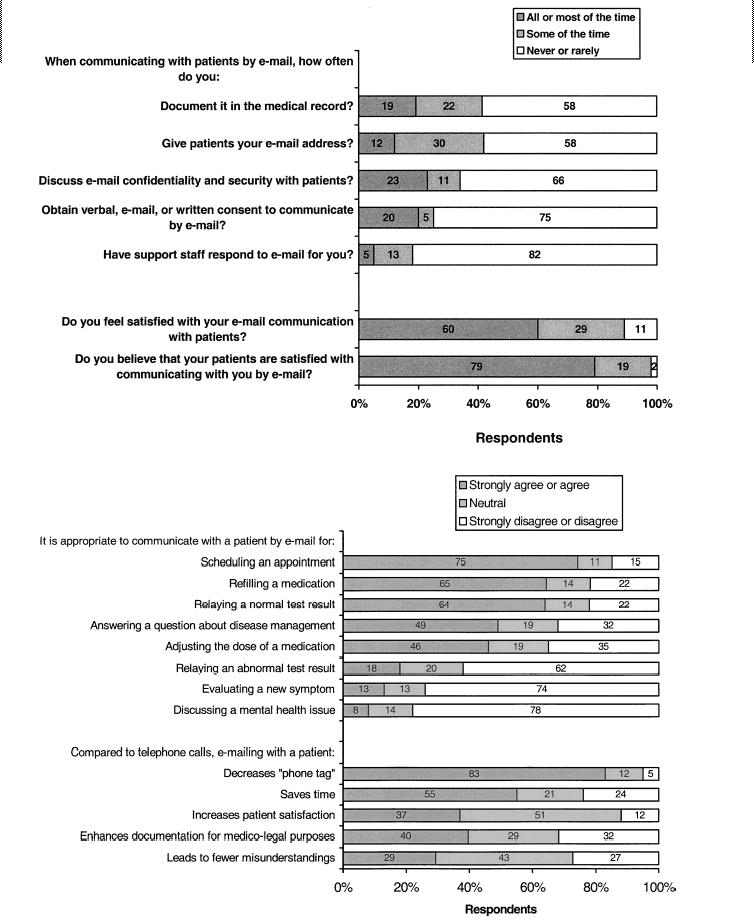
Physician practices and attitudes toward patient electronic mail (e-mail). Values may not add up to 100 due to rounding.
As illustrated in Figure 1, scheduling appointments was the situation most often identified as being appropriate for communicating with patients by e-mail. Responses were mixed regarding using e-mail to answer questions about disease management. The majority of physicians felt that e-mail was inappropriate for evaluating a new symptom.
The 2 problems physicians identified most often as being problems with communicating with patients via e-mail were concerns about confidentiality (“I think e-mail is risky from a medico-legal perspective”) and concerns that e-mail does not “count” for patient billing or personal productivity (“There's no way to get reimbursed for e-mail”).
DISCUSSION
In this study, a large number of physicians at an academic medical center and its affiliated community clinics reported using e-mail to communicate with their patients, although the average number of e-mails received per month was not large. Physicians at the county hospital clinics, who provide care for a higher proportion of poor and underserved patients, as well as those at community-based primary care clinics, reported significantly less patient e-mail use than physicians at the university hospital clinics. The use of patient e-mail as a function of other physician characteristics was remarkably similar.
The dramatically lower use of patient e-mail at the community primary care clinics was unexpected. Although all these community physicians practice primary care, it is unlikely that this accounts for their lower use of patient e-mail, since use of patient e-mail at the other 2 sites did not differ between primary care and specialty care physicians. Another possible reason for their lower use of patient e-mail may be the greater emphasis on productivity that physicians at these clinics face, which may decrease their desire to spend time on a nonreimbursable activity such as patient e-mail. This explanation is supported by the higher number of physicians at these clinics who identified lack of productivity credit as a disadvantage to patient e-mail (data not shown). The nature of academic work may offer another possible explanation. Since physician researchers probably spend more time using e-mail in the course of their day, this may make it easier for them to incorporate patient e-mail into their workflow.
Physician attitudes toward patient e-mail were generally positive. They felt patient e-mail was acceptable for simple, straightforward issues but not for complex situations. Although physicians expressed significant concerns regarding how patient e-mail might affect their future practice, they expressed a high degree of satisfaction with their current e-mail use.
Our results are similar to those obtained by a survey of physicians at another academic medical center in which most physicians felt positively toward patient e-mail, although many also were afraid of being overwhelmed by it.9
The major strengths of this study are its high response rate, making response bias less likely, and its mail-in methodology, which captured all physicians in the study population, not just those who use computers.10 Other strengths of the study include the diverse nature of the patient populations cared for by the respondents, the broad range of physician practices surveyed (primary care and specialists), and the representation of physicians of all ages and of both genders.
Several limitations of this study deserve mention. First, the reliance on physicians' self-reporting of their e-mail use raises the possibility of recall bias, although self-reports of e-mail use by health providers have been shown to correlate well with actual use.11 Second, this study focused on physicians only and did not examine the perspectives of their patients. Finally, we surveyed a relatively small group of physicians affiliated with a single institution, and so this study's generalizability may be limited. Nevertheless, this investigation offers insight into a new and rarely studied form of communication that has the potential to dramatically alter the way that physicians interact with their patients.2
Individual physicians, health care institutions, and professional agencies increasingly will need to make difficult decisions regarding patient e-mail, especially in areas such as patient confidentiality.3,12–15 We found that most physicians did not discuss e-mail security with their patients and did not document patient e-mail communication in the medical record, despite published guidelines recommending that such practices be routine.6–8
Our findings suggest that institutional support will be needed for patient e-mail to become better incorporated into physicians' clinical practice. Secure accounts dedicated to patient communication and the availability of staff to help screen and reply to patient e-mails may be needed.16,17 Careful thought and research are needed to address which uses of patient e-mail are most appropriate, and regulatory agencies will need to examine whether or how physicians can bill for the care they provide via e-mail.
Acknowledgments
The authors wish to thank Deborah Lum, Megan Reynolds, and Lisa Reisch for their technical assistance, and Jack Goldberg for his advice regarding data analysis.
REFERENCES
- 1.Nielsen Net Ratings. Web usage. Available at: http://209.249.142.27/nnpm/owa/NRpublicreports.usageweekly. Accessed September 5, 2002.
- 2.Coile RC., Jr The digital transformation of health care. Physician Exec. 2000;26:8–15. [PubMed] [Google Scholar]
- 3.Sands DZ. Electronic patient-centered communication: managing risks, managing opportunities, managing care. Am J Manag Care. 1999;5:1569–71. [PubMed] [Google Scholar]
- 4.Mandl KD, Kohane IS, Brandt AM. Electronic patient-physician communication: problems and promise. Ann Intern Med. 1998;129:495–500. doi: 10.7326/0003-4819-129-6-199809150-00012. [DOI] [PubMed] [Google Scholar]
- 5.Spielberg AR. On call and online: sociohistorical, legal, and ethical implications of e-mail for the patient-physician relationship. JAMA. 1998;280:1353–9. doi: 10.1001/jama.280.15.1353. [DOI] [PubMed] [Google Scholar]
- 6.Kane B, Sands DZ. Guidelines for the clinical use of electronic mail with patients. The AMIA Internet Working Group, Task Force on Guidelines for the Use of Clinic-Patient Electronic Mail. J Am Med Inform Assoc. 1998;5:104–11. doi: 10.1136/jamia.1998.0050104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Medical Association. Guidelines for patient-physician electronic mail. Available at: http://www.ama-assn.org/ama/pub/category/6460.html. Accessed September 5, 2002. [Google Scholar]
- 8.American Health Information Management Association. E-mail security. J AHIMA. 2000;71:72A–D. [PubMed] [Google Scholar]
- 9.Moyer CA, Stern DT, Dobias KS, Cox DT, Katz SJ. Bridging the electronic divide: patient and provider perspectives on e-mail communication in primary care. Am J Manag Care. 2002;8:427–33. [PubMed] [Google Scholar]
- 10.Mavis BE, Brocato JJ. Postal surveys versus electronic mail surveys. The tortoise and the hare revisited. Eval Health Prof. 1998;21:395–408. doi: 10.1177/016327879802100306. [DOI] [PubMed] [Google Scholar]
- 11.Sands DZ, Safran C, Slack WV, Bleich HL. Use of electronic mail in a teaching hospital. Proc Annu Symp Comput Appl Med Care. 1993:306–10. [PMC free article] [PubMed] [Google Scholar]
- 12.Van Doren JA. If you monitor e-mail, have a policy. Health Care Superv. 1996;15:12–5. [PubMed] [Google Scholar]
- 13.Burns TC, Rashid S. Web-based e-mail communications: issues in responsive service. Top Health Inf Manage. 2001;21:63–9. [PubMed] [Google Scholar]
- 14.Baur C. Limiting factors on the transformative powers of e-mail in patient-physician relationships: a critical analysis. Health Commun. 2000;12:239–59. doi: 10.1207/S15327027HC1203_02. [DOI] [PubMed] [Google Scholar]
- 15.Prady SL, Norris D, Lester JE, Hoch DB. Expanding the guidelines for electronic communication with patients: application to a specific tool. J Am Med Inform Assoc. 2001;8:344–8. doi: 10.1136/jamia.2001.0080344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Meyer F, Lundgren PA, de Moor G, Fiers T. Determination of user requirements for the secure communication of electronic medical record information. Int J Med Inf. 1998;49:125–30. doi: 10.1016/s1386-5056(98)00021-5. [DOI] [PubMed] [Google Scholar]
- 17.James JS. Major email security flaws discovered: how to protect your data. AIDS Treat News. 1998;301:8. [PubMed] [Google Scholar]


