Abstract
OBJECTIVE
To determine changes in the use of do-not-resuscitate (DNR) orders and mortality rates following a DNR order after the Patient Self-determination Act (PSDA) was implemented in December 1991.
DESIGN
Time-series.
SETTING
Twenty-nine hospitals in Northeast Ohio.
PATIENTS/PARTICIPANTS
Medicare patients (N = 91,539) hospitalized with myocardial infarction, heart failure, gastrointestinal hemorrhage, chronic obstructive pulmonary disease, pneumonia, or stroke.
MEASUREMENTS AND MAIN RESULTS
The use of “early” (first 2 hospital days) and “late” DNR orders was determined from chart abstractions. Deaths within 30 days after a DNR order were identified from Medicare Provider Analysis and Review files. Risk-adjusted rates of early DNR orders increased by 34% to 66% between 1991 and 1992 for 4 of the 6 conditions and then remained flat or declined slightly between 1992 and 1997. Use of late DNR orders declined by 29% to 53% for 4 of the 6 conditions between 1991 and 1997. Risk-adjusted mortality during the 30 days after a DNR order was written did not change between 1991 and 1997 for 5 conditions, but risk-adjusted mortality increased by 21% and 25% for stroke patients with early DNR and late DNR orders, respectively.
CONCLUSIONS
Overall use of DNR orders changed relatively little after passage of the PSDA, because the increase in the use of early DNR orders between 1991 and 1992 was counteracted by decreasing use of late DNR orders. Risk-adjusted mortality rates after a DNR order generally remained stable, suggesting that there were no dramatic changes in quality of care or aggressiveness of care for patients with DNR orders. However, the increasing mortality for stroke patients warrants further examination.
Keywords: resuscitation order, mortality, quality of health care
Few large, multicenter studies have examined trends in the use of do-not-resuscitate (DNR) orders and changes in the outcomes of patients receiving them.1–4 Wenger et al. found that the use of DNR orders for Medicare patients increased significantly from 10% in 1981–82 to 13% in 1985–1986.1 Patients with DNR orders hospitalized in 1985–86 were more likely to survive until discharge than patients hospitalized in 1981–82, but 30-day mortality rates were similar for the 2 study periods. Jayes et al. found that the use of DNR orders among patients admitted to intensive care units increased from 5.4% in 1979–82 to 9% in 1988–90, and mortality rates for patients who had a DNR order declined.2
One particularly important event that could have affected use of DNR orders over the last decade was passage of the Patient Self-determination Act (PSDA),5 which was passed in 1990 and implemented on December 1, 1991. The PSDA required hospitals, skilled nursing facilities, and other health care settings to: (1) develop written policies concerning advance directives; (2) ask all new patients whether they had prepared an advance directive and include this information in the patient's chart; (3) give patients written materials regarding the facility's policies on advance directives and the patient's right to prepare such documents; and (4) educate the staff and community about advance directives. The goal of this legislation was to increase patients' involvement in decisions regarding life-sustaining treatments by ensuring that physicians were aware of patients' prior advance directives and to make patients who had not completed advance directives aware of their legal right to do so.6
Several studies have examined changes that occurred after passage of the PSDA. Emanuel et al. interviewed 258 patients who were discharged prior to implementation of the PSDA and 321 patients discharged shortly after implementation of the PSDA. There was an increase in the proportion of patients who had some kind of advance care planning and the proportion who had a general discussion of end-of-life issues with their proxies.7 The proportion of patients who had written advance care plans also increased (from 20% to 26%), but this was not statistically significant in their small study population. The proportion of patients in poor health who spoke with their physician about advance care plans increased from 15% to 25%. Changes in the use of written DNR orders were not reported. A report from the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment found that only half of patients who expressed a desire to forgo resuscitation had a DNR order written, and there was no change in the use of DNR orders after implementation of the PSDA.8 Other studies have examined changes in use of advance directives at nursing homes after implementation of PSDA and found marked increases in the use of advance directives and written DNR orders.9–11 This increase in written advance directives and DNR orders in nursing homes could lead to increases in the use of DNR orders among nursing home residents who are hospitalized for acute medical conditions.
Many previous studies have shown that health care providers often do not discuss patients' preferences about resuscitation, and DNR orders are often not written even when patients have a clear preference to forgo resuscitation.12 If the PSDA achieved its goal of increasing discussions between patients and physicians about patients' preferences for life-sustaining treatments, we would expect that use of DNR orders should have increased after it was implemented. Such discussions also could lead to changes in how patients with DNR orders were treated. For example, if patients became more likely at the time of admission to express a desire to not be treated aggressively, this could lead to shorter lengths of hospital stay or increasing mortality shortly after DNR orders were written. This study examined changes in the use of DNR orders at hospitals in Northeast Ohio between 1991 and 1997, which includes data from the year prior to implementation of the PSDA and the 6 years afterwards. In addition, we examined changes over this same time period in risk-adjusted length of stay and risk-adjusted mortality rates for patients who had DNR orders written.
METHODS
Study Population
This study was approved by the MetroHealth Medical Center Institutional Review Board. We used data from a previous study that combined data from the Cleveland Health Quality Choice (CHQC) program13 with Medicare Provider Analysis and Review (MEDPAR) files from the Health Care Financing Administration. Both the CHQC program13 and our methodology for merging the CHQC database with MEDPAR files have been described previously.14 Briefly, CHQC was a regional initiative designed to objectively measure and compare risk-adjusted outcomes for hospitals in Northeast Ohio. All 29 nonfederal hospitals in greater metropolitan Cleveland participated in CHQC. Every 6 months, hospitals provided CHQC with a list of all patients (excluding interhospital transfers) discharged with a principal diagnosis of acute myocardial infarction (AMI), congestive heart failure (CHF), gastrointestinal (GI) hemorrhage, chronic obstructive pulmonary disease (COPD), pneumonia, and stroke (see previous publication for full list of the International Classification of Diseases, 9th Revision codes for these diagnoses).14 Chart abstraction for CHQC was performed by medical records technicians at each hospital to obtain patients' demographics; admission source (e.g., home, nursing home); comorbid conditions; admission vital signs, and neurological findings; and results of laboratory, radiological, and electrocardiographic testing. Our combined database includes extremely detailed clinical data from the time of admission for all eligible Medicare admissions to nonfederal hospitals in Northeast Ohio between 1991 and 1997 for patients age 18 and over.
Separate databases were created for the 6 conditions. As was done for our previous analyses of mortality trends,14 we selected only an individual's first admission within the CHQC disease-specific database. To exclude patients who were admitted for the same diagnosis before 1991 or who were admitted to a non-CHQC hospital for the same diagnosis prior to their index admission in CHQC (e.g., admitted to a hospital in Florida for CHF in 1994 and to a CHQC hospital in 1995), we searched MEDPAR files from 1989 to 1997 and excluded patients who had a non-CHQC admission with the same diagnosis in the 2 years prior to their index admission in CHQC. Patients with a qualifying first admission in more than 1 disease category (e.g., pneumonia and stroke) were included in all databases.
DNR Orders
The CHQC chart abstractors determined whether a DNR order was written and the hospital day on which it occurred. We created 2 categories of DNR orders: (1) early DNR orders, defined as occurring on the first or second hospital day, and (2) late DNR orders, defined as occurring on day 3 or later. An early DNR order may be a statement of general preferences in the event of an arrest or an indicator that the patient was admitted in moribund condition. In contrast, many late DNR orders are written because a patient's condition is deteriorating, and further treatment is thought to be futile. We postulated that the PSDA would have a greater effect on the use of early DNR orders.
Admission Severity of Illness
The methods for developing our 6 disease-specific admission severity-of-illness models, the complete lists of variables included in the models, and the predictive validity and calibration of the models have been fully described previously.14 Briefly, we developed logistic regression models with death at 30 days after admission as the dependent variable using the data from 1991–92. We then used the β coefficients from these baseline models and individuals' unique values for the variables in the models to determine an admission severity of illness score for all patients (1991–97). The admission severity of illness score indicates patients' probability of death within 30 days of admission (scale ranging from 0% to 100%). All models showed consistent performance (e.g., c-statistics and calibration)15 across all study years.
Analysis of Temporal Trends in Use of DNR Orders
Analyses were conducted using Stata (version 7; Stata Corp., College Station, Tex). We used “DNR status” as the dependent variable with 3 categories: (1) no DNR order written (reference category); (2) early DNR order written; and (3) late DNR order written. The proportion of patients in each category for each year was determined and tabulated. The crude rates of DNR order use showed markedly nonlinear trends, with large changes between 1991 and 1992 and different trends between 1992 and 1997. We therefore conducted separate statistical analyses for these 2 periods using multinomial logistic regression with time as the main independent variable. For the 1991–92 trend analysis, admission year was entered as a dichotomous variable. For 1992–97, all trends were approximately linear by visual assessment, and there were no significant differences between models with year entered as a single continuous variable and models with year entered as a set of dummy variables. We therefore modeled trends with year as a single continuous variable, ranging from 0 (1992) to 1 (1997), to achieve greater power and to decrease the effect of random variation in the data for the start and end of the study period. Covariates included age, sex, race (white vs nonwhite), admission from a nursing home, admission severity of illness, and hospital. Older age, female sex, white race, admission from a nursing home, and greater admission severity of illness were all significantly associated with receiving a DNR order in all models. Analyses were repeated without “admission from a nursing home” in the model, and the results were similar.
The multinomial logistic regression models yield 2 separate β coefficients for time, representing (1) the temporal change in the odds of having an early DNR order written versus not having any DNR order, and (2) the temporal change in the odds of having a late DNR order written versus not having any DNR order. These β coefficients were exponentiated to determine odds ratios, and odds ratios were converted to relative risks using published formulas.16 Trends in not having any DNR order written were analyzed using logistic regression with the dichotomous variable “no DNR order” and the same set of covariates. All analyses adjusted standard errors to account for the clustering of patients within hospitals.
Length of Stay
To analyze whether length of stay declined more for patients with early DNR orders than for those without an early DNR order, we used multivariate linear regression models with length of stay as the dependent variable. Independent variables included admission severity of illness, year of admission, early DNR order (yes/no), and an interaction term between year and early DNR order. The β coefficient for the interaction term represents the difference (days) in the trends in length of stay for patients with and without an early DNR order. Analyses were repeated using the natural logarithm of length of stay because of the highly skewed distribution of length of stay. The results were similar, and only the untransformed results are presented to facilitate interpretation. To fully account for changes over time in the likelihood that a DNR order would be written, we used propensity analysis to adjust for changes over time in the use of DNR orders.17–19 To derive propensity scores, we repeated the condition-specific multinomial logistic regression models with “DNR status” as the dependent variable, and age, sex, race, admission from a nursing home, admission severity of illness, and hospital as the only independent variables (i.e., time was not included). We then repeated the multivariate linear regression models of length of stay trends including each individual's probability of having an early DNR order written as a covariate.
Mortality
We determined whether patients with DNR orders were alive 30 days after the order was written using the date of the DNR order from CHQC and the date of death from the MEDPAR file. Changes in mortality between 1991 and 1997 were determined using separate logistic regression models for patients with (a) early DNR orders and (b) late DNR orders. Multivariate analyses were conducted with year, admission severity of illness, hospital day on which the DNR order was written, and hospital as independent variables. In addition, we included (a) the probability of having an early DNR order written, and (b) the probability of having a late DNR order written in the 2 models, respectively. Beta coefficients from these models were converted to relative risks as described earlier.
RESULTS
Demographic characteristics of patients with the 6 target medical conditions are shown in Table 1. The average age was approximately 77 years old, slightly over half of the patients were women, and ∼85% were white, which is consistent with the demographics of Northeast Ohio.
Table 1.
Demographic Characteristics of Medicare Patients Hospitalized in Northeast Ohio Between 1991 and 1997 with a Principal Discharge Diagnosis of Acute Myocardial Infarction (AMI), Congestive Heart Failure (CHF), Gastrointestinal Hemorrhage (GIH), Chronic Obstructive Pulmonary Disease (COPD), Pneumonia (PNEU), and Stroke (STR)
| AMI | CHF | GIH | COPD | PNEU | STR | |
|---|---|---|---|---|---|---|
| N | 10,426 | 23,480 | 11,079 | 8,484 | 23,709 | 14,276 |
| Mean age, y (SD) | 76.8 (8.7) | 77.9 (9.3) | 77.3 (10.0) | 74.1 (9.2) | 77.4 (10.5) | 77.5 (8.4) |
| Female, % | 52.5 | 57.2 | 56.9 | 59.6 | 53.5 | 58.5 |
| White, % | 88.5 | 84.9 | 83.7 | 84.8 | 85.3 | 84.3 |
Changes in the Use of DNR Orders
The use of DNR orders early during hospitalization (i.e., the first or second day) jumped distinctly between 1991 and 1992 for all conditions, with an absolute increase ranging from 2.7 percentage points for AMI to 4.4 percentage points for CHF (Table 2). In multivariate analyses, the adjusted relative risks of having an early DNR order in 1992 compared to 1991 ranged from 1.12 (95% confidence interval [95% CI], 0.90 to 1.38) for stroke to 1.66 (95% CI, 1.08 to 2.46) for GI hemorrhage. The relative increase in early DNR orders was similar for patients who were admitted from nursing homes and those who were not.
Table 2.
Percentage of Patients for Whom a Do-not-resuscitate (DNR) Order Was Written on Hospital Day 1 or 2 (Early DNR) and on Hospital Day 3 or Later (Late DNR)
| Study Year, % | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Condition, DNR Status | '91 | '92 | '93 | '94 | '95 | '96 | '97 | Adjusted RR* '92 versus '91 (95% CI) | P Value | Adjusted RR for trend '92–'97* (95% CI) | P Value |
| Acute myocardial infarction | |||||||||||
| No DNR (N = 8,245) | 82.7 | 79.9 | 80.8 | 78.7 | 77.9 | 78.0 | 78.5 | 0.96 (0.91 to 1.00) | .04 | 0.99 (0.96 to 1.02) | .64 |
| Early DNR (N = 1,552) | 10.4 | 13.1 | 13.2 | 15.4 | 16.3 | 16.6 | 15.4 | 1.34 (1.04 to 1.71) | .02 | 1.01 (0.91 to 1.31) | .31 |
| Late DNR (N = 629) | 6.9 | 7.0 | 6.0 | 5.9 | 5.8 | 5.5 | 6.2 | 1.12 (0.85 to 1.48) | .42 | 0.91 (0.74 to 1.08) | .28 |
| Congestive heart failure | |||||||||||
| No DNR (N = 19,656) | 85.8 | 82.1 | 83.0 | 82.6 | 85.0 | 83.5 | 84.6 | 0.97 (0.92 to 1.01) | .14 | 1.04 (1.01 to 1.07) | .005 |
| Early DNR (N = 2,819) | 8.6 | 13.0 | 12.5 | 12.7 | 11.2 | 12.8 | 11.7 | 1.41 (1.03 to 1.90) | .03 | 0.84 (0.71 to 0.99) | .04 |
| Late DNR (N = 1,005) | 5.5 | 4.9 | 4.5 | 4.8 | 3.8 | 3.7 | 3.7 | 0.90 (0.69 to 1.18) | .45 | 0.71 (0.52 to 0.95) | .03 |
| GI hemorrhage | |||||||||||
| No DNR (N = 9,277) | 87.2 | 86.0 | 84.1 | 82.6 | 84.6 | 82.7 | 82.5 | 0.96 (0.88 to 1.02) | .18 | 1.02 (0.99 to 1.05) | .26 |
| Early DNR (N = 1,469) | 8.9 | 11.8 | 12.3 | 13.7 | 12.8 | 15.0 | 14.8 | 1.66 (1.08 to 2.46) | .02 | 0.96 (0.75 to 1.22) | .77 |
| Late DNR (N = 333) | 3.9 | 2.2 | 3.7 | 3.7 | 2.6 | 2.3 | 2.7 | 0.63 (0.34 to 1.14) | .13 | 0.62 (0.45 to 0.86) | .005 |
| COPD | |||||||||||
| No DNR (N = 7,432) | 88.7 | 83.9 | 87.4 | 86.8 | 86.8 | 90.0 | 88.0 | 0.92 (0.84 to 0.98) | .008 | 1.06 (1.03 to 1.10) | .001 |
| Early DNR (N = 749) | 6.9 | 9.7 | 9.2 | 9.1 | 10.1 | 7.3 | 8.7 | 1.62 (1.01 to 2.54) | .05 | 0.71 (0.54 to 0.95) | .02 |
| Late DNR (N = 303) | 4.3 | 6.4 | 3.4 | 4.1 | 3.2 | 2.7 | 3.0 | 1.76 (1.12 to 2.71) | .01 | 0.47 (0.30 to 0.71) | <.001 |
| Pneumonia | |||||||||||
| No DNR (N = 16,856) | 75.4 | 72.4 | 70.0 | 70.5 | 70.3 | 71.2 | 71.5 | 0.98 (0.92 to 1.03) | .43 | 1.06 (1.03 to 1.10) | .001 |
| Early DNR (N = 5,271) | 18.0 | 22.1 | 22.8 | 22.2 | 23.2 | 22.4 | 22.1 | 1.16 (0.91 to 1.46) | .23 | 0.82 (0.71 to 0.93) | .002 |
| Late DNR (N = 1,582) | 6.6 | 5.5 | 7.2 | 7.3 | 6.6 | 6.4 | 6.4 | 0.86 (0.68 to 1.06) | .18 | 0.84 (0.70 to 0.99) | .04 |
| Stroke | |||||||||||
| No DNR (N = 10,604) | 77.0 | 74.5 | 73.1 | 74.2 | 73.8 | 75.6 | 73.5 | 0.99 (0.92 to 1.05) | .71 | 1.01 (0.97 to 1.04) | .76 |
| Early DNR (N = 2,717) | 14.7 | 17.8 | 20.1 | 18.7 | 19.9 | 18.9 | 20.2 | 1.12 (0.90 to 1.38) | .30 | 1.04 (0.89 to 1.20) | .62 |
| Late DNR (N = 955) | 8.3 | 7.7 | 6.8 | 7.1 | 6.3 | 5.5 | 6.3 | 0.93 (0.63 to 1.36) | .72 | 0.82 (0.64 to 1.06) | .13 |
Relative risks (RR) and P values for the “No DNR” group are obtained from logistic regression models with “no DNR order” as the reference category. Relative risks and P values for the “Early DNR” and the “Late DNR” groups are obtained from multinomial logistic regression models with the “No DNR” group as the reference category. All models adjust for admission severity of illness, age, sex, race, admission from a nursing home, and hospital. Standard errors are adjusted for the clustering of patients within hospitals. For the 1992–1997 analysis, year was entered as a continuous variable ranging from 1992 = 0 to 1997 = 1. The β coefficients for year were used to estimate the change in the risk of having (a) an early DNR order, or (b) a late DNR order written in 1997 versus 1991 by exponentiating the β coefficient to obtain the odds ratios and then converting the odds ratios to relative risks using published formulas.
However, between 1992 and 1997 (Table 2), the risk-adjusted rates of early DNR orders decreased significantly back toward the 1991 levels for CHF (adjusted relative risk [RR], 0.85 for 1997 vs 1992; 95% CI, 0.71 to 0.99), COPD (adjusted RR, 0.71; 95% CI, 0.54 to 0.95), and pneumonia (adjusted RR, 0.82; 95% CI, 0.71 to 0.93). Risk-adjusted rates of early DNR orders were stable between 1992 and 1997 for AMI, GI hemorrhage, and stroke.
Trends in the use of late DNR orders were quite different than those for early DNR orders (Table 2). Between 1991 and 1992, there was no change in the use of late DNR orders, with the exception of a significant increase for patients with COPD (adjusted RR for 1992 vs 1991, 1.76; 95% CI, 1.12 to 2.71). In contrast, between 1992 and 1997, the adjusted relative risk of having a late DNR order declined for all conditions, with adjusted relative risks ranging from 0.47 (95% CI, 0.30 to 0.71) for COPD to 0.91 (95% CI, 0.74 to 1.08) for AMI. Overall, these countervailing trends in the use of early DNR orders and late DNR orders resulted in a fairly constant proportion of patients with any DNR order over the entire study period (1991–97; Table 2).
Changes in Severity of Illness for Patients with Early DNR Orders
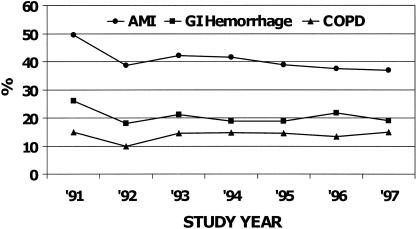
Overall, admission severity of illness remained constant for all conditions between 1991 and 1992 (data not shown). However, changes were seen for patients who had DNR orders written. Among patients with AMI who had an early DNR order written, mean admission severity of illness (±SD) declined dramatically between 1991 and 1992 (49.5 ± 27.5% in 1991 vs 38.6 ± 27.7% in 1992; P < .001). However, it remained fairly stable after 1992 (Fig. 1). The trends were similar for GI hemorrhage and COPD, with an abrupt decline between 1991 and 1992 followed by relative stability between 1992 and 1997 (Fig. 1; P < .001 for 1992 vs 1991 for both conditions). Mean severity of illness did not change significantly for patients with CHF, pneumonia, and stroke (data not shown).
FIGURE 1.
Trends for mean admission severity of illness for patients who had a do-not-resuscitate order written on the first or second hospital day. Abbreviations: AMI, acute myocardial infarction; COPD, chronic obstructive pulmonary disease; GI, gastrointestinal. Mean severity of illness is based on the estimated risk of death within 30 days after admission.
Changes in Length of Stay
Length of stay declined significantly between 1991 and 1997 for patients with CHF, GI hemorrhage, COPD, pneumonia, and stroke, but the magnitude of the declines was similar for patients who had an early DNR order written and for those who did not.
Changes in Mortality after a DNR Order
Mortality rates during the 30 days after a DNR order was written were extremely high, with somewhat higher mortality rates for patients with late DNR orders (Table 3). Overall, there was little change over time in mortality after a DNR order was written (Table 3). Among patients with AMI who had a late DNR order written, mortality decreased significantly between 1991 and 1997 (adjusted RR, 0.81; 95% CI, 0.60 to 0.98; Table 3). For patients with stroke, the adjusted relative risk of death in the 30 days after a DNR order was written increased by 1.21 (95% CI, 1.08 to 1.34) between 1991 and 1997 for those with an early DNR order and by 1.25 (95% CI, 1.05 to 1.42) for those with a late DNR order.
Table 3.
Trends from 1991–97 for the Risk of Death During the 30 Days after a Do-not-resuscitate (DNR) Order Was Written*
| Study Year, % Dead | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Condition, DNR Status | '91 | '92 | '93 | '94 | '95 | '96 | '97 | Adjusted RR for Trend '91–'97 (95% CI)† | P Value |
| Acute myocardial infarction | |||||||||
| Early DNR (N = 1,552) | 67.6 | 50.0 | 62.7 | 55.3 | 60.0 | 52.8 | 51.2 | 0.96 (0.81 to 1.08) | .52 |
| Late DNR (N = 629) | 72.0 | 74.6 | 66.7 | 71.7 | 64.0 | 51.0 | 64.9 | 0.81 (0.60 to 0.98) | .03 |
| Congestive heart failure | |||||||||
| Early DNR (N = 2,819) | 35.0 | 37.8 | 35.8 | 33.2 | 33.0 | 30.5 | 30.9 | 0.86 (0.69 to 1.05) | .14 |
| Late DNR (N = 1,005) | 55.4 | 50.5 | 51.9 | 46.7 | 53.7 | 45.0 | 49.3 | 0.97 (0.78 to 1.17) | .80 |
| Gastrointestinal hemorrhage | |||||||||
| Early DNR (N = 1,469) | 38.8 | 30.7 | 27.5 | 27.4 | 27.3 | 29.6 | 29.3 | 0.98 (0.73 to 1.26) | .90 |
| Late DNR (N = 333) | 51.7 | 47.4 | 55.1 | 50.0 | 57.1 | 65.1 | 48.0 | 1.17 (0.80 to 1.49) | .36 |
| COPD | |||||||||
| Early DNR (N = 749) | 30.6 | 15.0 | 25.9 | 25.9 | 27.3 | 20.0 | 29.0 | 1.08 (0.70 to 1.55) | .71 |
| Late DNR (N = 303) | 56.5 | 57.5 | 57.1 | 51.6 | 68.1 | 61.5 | 46.5 | 1.07 (0.72 to 1.37) | .70 |
| Pneumonia | |||||||||
| Early DNR (N = 5,271) | 39.6 | 41.3 | 39.4 | 39.7 | 41.0 | 40.7 | 42.3 | 1.04 (0.91 to 1.17) | .57 |
| Late DNR (N = 1,582) | 61.6 | 58.0 | 59.3 | 56.7 | 56.6 | 56.7 | 55.3 | 0.93 (0.78 to 1.07) | .31 |
| Stroke | |||||||||
| Early DNR (N = 2,717) | 51.2 | 41.8 | 44.7 | 41.4 | 45.8 | 49.2 | 50.7 | 1.21 (1.08 to 1.34) | .002 |
| Late DNR (N = 955) | 52.1 | 54.0 | 54.7 | 55.6 | 53.0 | 67.4 | 61.3 | 1.25 (1.05 to 1.42) | .01 |
A DNR order was defined as “early” if it was written on the first or second day of hospitalization and “late” if written any time after that.
Adjusted for admission severity of illness (predicted 30-day mortality), probability of having an early or late DNR order written, and the hospital day on which the DNR order was written. The β coefficients for year were used to estimate the change in the risk of having (a) an early DNR order, or (b) a late DNR order written in 1997 versus 1991 by exponentiating the β coefficient to obtain the odds ratios and then converting the odds ratios to relative risks using published formulas.
DISCUSSION
Between 1991 and 1992, there were significant increases in the use of DNR orders on the first or second day of hospitalization for patients with AMI, CHF, GI hemorrhage, and COPD, as well as smaller increases for patients with pneumonia and stroke. At the same time, admission severity of illness decreased for patients with AMI, GI hemorrhage, and COPD who had early DNR orders. This indicates that the use of DNR orders increased among less severely ill patients, as would be expected if discussions about advance directives were happening more frequently as a routine part of care rather than as a response to patients' clinical status. Although this study cannot prove a causal relationship, the temporal association between these changes and implementation of the PSDA at the end of 1991 supports the hypothesis that the Act led to an increase in the use of early DNR orders. However, use of early DNR orders did not increase further between 1992 and 1997, and use of early DNR orders actually declined significantly for patients with CHF, COPD, and pneumonia. Thus, if the PSDA did cause the increase from 1991 to 1992, the effect was only partially sustained over time. This suggests that there may have been gradually diminishing efforts to implement the provisions of the Act after the flurry of attention about it subsided.6,20,21
In contrast, the use of late DNR orders declined from 1991 to 1997 for most conditions. A small portion of this decline was due to the shift in timing from late DNR orders to early DNR orders between 1991 and 1992, which may have been related to implementation of the PSDA. However, most of the decline in use of late DNR orders occurred between 1992 and 1997 when there was no compensatory increase in the use of early DNR orders. This decline in late DNR orders may be related to the decreasing length of stay observed over this same period. Physicians may feel more inclined to discuss patients' preferences for resuscitation and supportive care when patients stay for longer periods of time in the hospital12 or when there is a perceived risk that the patient will die in the hospital. Failure to address patient and family preferences for resuscitation prior to discharge should be viewed as a quality-of-care problem that could have adverse consequences beyond the index hospitalization.22,23 For example, a patient who wants only comfort care instead may go through a cycle of multiple readmissions until this issue is finally addressed.
We originally hypothesized that increasing economic pressures to discharge patients could disproportionately affect patients who had an early DNR order written. However, absolute declines in mean length of stay from 1991 to 1997 were similar for patients with early DNR orders as compared to those who did not have an early DNR order. Previous studies have shown that patients who receive DNR orders have lower hospital expenditures, suggesting that they receive less intensive care than patients with equal severity of illness who do not have a DNR order.24 We did not analyze hospital expenditures in this study, so it remains possible that the intensity of hospital care decreased disproportionately more for patients with DNR orders.
Mortality rates following a DNR order remained fairly constant over the study period, suggesting that there were no dramatic changes in care for patients who had DNR orders written. Outcomes among patients with acute stroke represent an exception; we observed increases in risk-adjusted mortality of about 20% to 25% over the 7-year period among patients who had a DNR order written. We previously reported increasing 30-day mortality rates for patients with stroke in Northeast Ohio between 1991 and 1997.14 Our current findings suggest that much of the previously reported increase in mortality for patients with stroke resulted from changes in care for patients who had a DNR order. Nevertheless, the meaning of this worsening mortality rate for stroke patients with DNR orders remains unclear. Previous studies have shown that when physicians understand patients' preferences for resuscitation, resource use is less.25 If the PSDA increased physicians' understanding of patients' preferences for end-of-life care, this may have led to an appropriate decrease in the intensity of care, which resulted in shorter life expectancy. However, others have expressed concern that patients with DNR orders may not receive appropriate life-sustaining treatments.26 The CHQC program did not collect information on medications prescribed, so we could not determine whether the increasing mortality for stroke patients who had a DNR order resulted from declining quality of care, more frequent medical errors, or other factors.
There are several important limitations to this study. We had data from only 1 year prior to the implementation of the Patient Self-determination Act. Therefore, it is possible that the observed changes in the use of DNR orders were due to changes in the quality of abstraction between the first and second year of the study. This seems unlikely because of the very high interobserver reliability of chart abstractions from CHQC.13 Nevertheless, it remains possible that the observed changes in use of DNR orders resulted from changes in documentation rather than true changes in practice. We found concomitant changes from 1991 to 1992 in the admission severity of illness of patients who received DNR orders (see Fig. 1), which would not be expected if there was random error in abstracting DNR orders in 1991. It is also possible that care patterns may have begun to change shortly after passage of the Act in 11 November 1990 in anticipation of full implementation of the Act in December 1991. If so, then use of DNR orders in 1991 actually could have been higher than in 1990, and our results would underestimate the true changes that occurred in response to the Act.
Our understanding of the effect of the Patient Self-determination Act is also limited by the fact that chart abstractors only recorded whether a DNR order was written, and we do not know how often a discussion took place without an order being written. It is possible that discussions regarding patients' preferences for cardiopulmonary resuscitation increased to a greater degree than the change in the use of DNR orders. Similarly, we do not know whether discussions took place regarding patients' desire to limit the aggressiveness of care aside from the issue of resuscitation. In addition, some discussions regarding end-of-life care may have taken place prior to hospitalization (i.e., in nursing homes), so the trends seen in this study may reflect changes in both hospital care and outpatient care. Finally, our study was conducted in only 1 region of the United States, and we do not know how generalizable our findings are to the remainder of the country.
In conclusion, the PSDA appears to have had a very limited effect on the use of DNR orders in hospitals in Northeast Ohio. Previous studies have shown that almost one third of severely ill hospitalized patients do not desire resuscitation, but only about half of them have a DNR order written.27 Even very intensive interventions to improve communication about patients' resuscitation preferences have been unsuccessful.28–30 Therefore, it seems unlikely that new legislation or attempts to improve compliance with the provisions of the PSDA will be successful. Alternative models for improving communication regarding end-of-life care are needed. Several authors have emphasized the vulnerability of elderly persons to substandard quality of care, including lack of discussions regarding end-of-life care, lack of documentation of care preferences, lack of awareness of advance directives across the continuum of care settings, and undertreatment of medical conditions during the dying process.22,26,31 The declining rate of late DNR orders seen in this study and the increasing mortality rate among stroke patients with DNR orders should intensify concerns about possible quality-of-care problems for these patients.
Acknowledgments
This study was supported by grant number R01 HS09969 from the Agency for Healthcare Research and Quality.
REFERENCES
- 1.Wenger NS, Pearson ML, Desmond KA, Kahn KL. Changes over time in the use of do not resuscitate orders and the outcomes of patients receiving them. Med Care. 1997;35:311–9. doi: 10.1097/00005650-199704000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Jayes RL, Zimmerman JE, Wagner DP, Draper EA, Knaus WA. Do-not-resuscitate orders in intensive care units. Current practices and recent changes. JAMA. 1993;270:2213–7. [PubMed] [Google Scholar]
- 3.Jonsson PV, Mc Namee M, Campion EW. The ‘do not resuscitate’ order. A profile of its changing use. Arch Intern Med. 1988;148:2373–5. [PubMed] [Google Scholar]
- 4.Stern SG, Orlowski JP. DNR or CPR–the choice is ours. Crit Care Med. 1992;20:1263–72. doi: 10.1097/00003246-199209000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Omnibus Budget Reconciliation Act of 1990. Public law no. 101–508. 2002. [PubMed]
- 6.Greco PJ, Schulman KA, Lavizzo-Mourey R, Hansen-Flaschen J. The Patient Self-Determination Act and the future of advance directives. Ann Intern Med. 1991;115:639–43. doi: 10.7326/0003-4819-115-8-639. [DOI] [PubMed] [Google Scholar]
- 7.Emanuel EJ, Weinberg DS, Gonin R, Hummel LR, Emanuel LL. How well is the Patient Self-Determination Act working? An early assessment. Am J Med. 1993;95:619–28. doi: 10.1016/0002-9343(93)90358-v. [DOI] [PubMed] [Google Scholar]
- 8.Teno J, Lynn J, Wenger N, et al. Advance directives for seriously ill hospitalized patients: effectiveness with the patient self-determination act and the SUPPORT intervention. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment. J Am Geriatr Soc. 1997;45:500–7. doi: 10.1111/j.1532-5415.1997.tb05178.x. [DOI] [PubMed] [Google Scholar]
- 9.Bradley EH, Wetle T, Horwitz SM. The patient self-determination act and advance directive completion in nursing homes. Arch Fam Med. 1998;7:417–23. doi: 10.1001/archfami.7.5.417. [DOI] [PubMed] [Google Scholar]
- 10.Castle NG, Mor V. Advance care planning in nursing homes. pre- and post-Patient Self-Determination Act. Health Serv Res. 1998;33:101–24. [PMC free article] [PubMed] [Google Scholar]
- 11.Teno JM, Branco KJ, Mor V, et al. Changes in advance care planning in nursing homes before and after the patient Self-Determination Act: report of a 10-state survey. J Am Geriatr Soc. 1997;45:939–44. doi: 10.1111/j.1532-5415.1997.tb02963.x. [DOI] [PubMed] [Google Scholar]
- 12.Golin CE, Wenger NS, Liu H, et al. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc. 2000;48(suppl):52–60. doi: 10.1111/j.1532-5415.2000.tb03141.x. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal GE, Harper DL. Cleveland health quality choice: a model for collaborative community-based outcomes assessment. Jt Comm J Qual Improv. 1994;20:425–42. doi: 10.1016/s1070-3241(16)30088-8. [DOI] [PubMed] [Google Scholar]
- 14.Baker DW, Einstadter D, Thomas C, Husak S, Gordon NH, Cebul RD. Mortality trends during a program that publicly reported hospital performance. Med Care. 2002;40:879–90. doi: 10.1097/00005650-200210000-00006. [DOI] [PubMed] [Google Scholar]
- 15.Ash AS, Shwartz M. Evaluating the performance of risk-adjustment methods: dichotomous outcomes. In: Iezzoni LI, editor. Risk Adjustment for Measuring Healthcare Outcomes. Chicago, Ill: Health Administration Press; 1997. pp. 444–9. [Google Scholar]
- 16.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 17.Rubin DB. Estimating causal effects from large data sets using propensity scores. Ann Intern Med. 1997;127:757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- 18.Foody JM, Cole CR, Blackstone EH, Lauer MS. A propensity analysis of cigarette smoking and mortality with consideration of the effects of alcohol. Am J Cardiol. 2001;87:706–11. doi: 10.1016/s0002-9149(00)01487-9. [DOI] [PubMed] [Google Scholar]
- 19.Gum PA, Thamilarasan M, Watanabe J, Blackstone EH, Lauer MS. Aspirin use and all-cause mortality among patients being evaluated for known or suspected coronary artery disease: a propensity analysis. JAMA. 2001;286:1187–94. doi: 10.1001/jama.286.10.1187. [DOI] [PubMed] [Google Scholar]
- 20.Wolf SM, Boyle P, Callahan D, et al. Sources of concern about the Patient Self-Determination Act. N Engl J Med. 1991;325:1666–71. doi: 10.1056/nejm199112053252334. [DOI] [PubMed] [Google Scholar]
- 21.Teno JM, Sabatino C, Parisier L, Rouse F, Lynn J. The impact of the Patient Self-Determination Act's requirement that states describe law concerning patients' rights. Law Med Health Care. 1993;21:102–8. doi: 10.1111/j.1748-720x.1993.tb01235.x. [DOI] [PubMed] [Google Scholar]
- 22.Wenger NS, Shekelle PG. Assessing care of vulnerable elders: ACOVE project overview. Ann Intern Med. 2001;135:642–6. doi: 10.7326/0003-4819-135-8_part_2-200110161-00002. [DOI] [PubMed] [Google Scholar]
- 23.Lynn J, Forlini JH. Serious and complex illness in quality improvement and policy reform for end-of-life care. J Gen Intern Med. 2001;16:315–9. doi: 10.1046/j.1525-1497.2001.90901.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teno JM, Lynn J, Phillips RS, et al. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Clin Ethics. 1994;5:23–30. [PubMed] [Google Scholar]
- 25.Teno JM, Hakim RB, Knaus WA, et al. Preferences for cardiopulmonary resuscitation. physician-patient agreement and hospital resource use. The SUPPORT Investigators. J Gen Intern Med. 1995;10:179–86. doi: 10.1007/BF02600252. [DOI] [PubMed] [Google Scholar]
- 26.Shepardson LB, Youngner SJ, Speroff T, Rosenthal GE. Increased risk of death in patients with do-not-resuscitate orders. Med Care. 1999;37:727–37. doi: 10.1097/00005650-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Phillips RS, Wenger NS, Teno J, et al. Choices of seriously ill patients about cardiopulmonary resuscitation: correlates and outcomes. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. Am J Med. 1996;100:128–37. doi: 10.1016/s0002-9343(97)89450-8. [DOI] [PubMed] [Google Scholar]
- 28.The SUPPORT Principal Investigators. A controlled trial to improve care for seriously ill hospitalized patients. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments (SUPPORT) JAMA. 1995;274:1591–8. [PubMed] [Google Scholar]
- 29.Lynn J, De Vries KO, Arkes HR, et al. Ineffectiveness of the SUPPORT intervention: review of explanations. J Am Geriatr Soc. 2000;48(suppl):206–13. doi: 10.1111/j.1532-5415.2000.tb03134.x. [DOI] [PubMed] [Google Scholar]
- 30.Lynn J, Arkes HR, Stevens M, et al. Rethinking fundamental assumptions: SUPPORT's implications for future reform. Study to Understand Prognoses and Preferences and Risks of Treatment. J Am Geriatr Soc. 2000;48(suppl):214–21. doi: 10.1111/j.1532-5415.2000.tb03135.x. [DOI] [PubMed] [Google Scholar]
- 31.Myers SS, Lynn J. Patients with eventually fatal chronic illness: their importance within a national research agenda on improving patient safety and reducing medical errors. J Palliat Med. 2001;4:325–32. doi: 10.1089/109662101753123931. [DOI] [PubMed] [Google Scholar]