Abstract
OBJECTIVE
To determine whether educational sessions with medical residents, with or without letters to their patients, improve patient satisfaction with transfer of their care from a departing to a new resident in an internal medicine clinic.
DESIGN
Observational study in Year 1 to establish a historical control, with a randomized intervention in Year 2.
SETTING
An internal medicine clinic in a teaching hospital.
PATIENTS/PARTICIPANTS
Patients of departing residents completed questionnaires in the waiting room at their first visit with a new resident, with mail-administered questionnaires for patients not presenting to the clinic within 3 months after transfer of their care. In Year 1, 376 patients completed questionnaires without intervention. The following spring, we conducted interactive seminars with 12 senior residents to improve their transfer of care skills (first intervention). Half of their patients were then randomized to receive a letter from the new doctor informing them of the change (second intervention). We assessed the efficacy of the interventions by administering questionnaires to 437 patients in the months following the interventions.
MEASUREMENTS AND MAIN RESULTS
Multivariate analysis of Year 1 results identified doctors personally informing patients prior to leaving as the single strongest predictor of patient satisfaction (partial R2=.41). In Year 2, our first intervention increased the percentage of patients informed by their doctors from 71% in 1991 to 79% in 1992 (P < .001). Mean satisfaction dramatically improved, with the fraction of fully satisfied patients increasing from 47% at baseline, to 61% with the first intervention alone, and 72% with both interventions (P < .0001).
CONCLUSIONS
Simple methods such as resident education and direct mailings to patients significantly ease the difficult process of transferring patients from one physician to another. This has implications not only for residency programs, but for managed care networks competing to attract and retain patients.
Keywords: patient satisfaction, doctor-patient relationship, primary care, medical education, continuity of care
The significance of maintaining continuity of care has received considerable attention in recent years because of the challenges posed by managed care contracts as well as the hospitalist movement. Patient satisfaction has also received greater attention, as a more positive impact of competition between health care systems. Continuity of care is associated with greater patient satisfaction, compliance and cooperation with medical instruction, and globally improved doctor-patient relationships.1–3 Provider continuity has been correlated with fewer emergent hospital admissions, shorter hospitalizations, and greater satisfaction.4
Although continuity is desirable, it is not always possible. One setting in which continuity is routinely disrupted is medical education, where residents typically provide longitudinal ambulatory care for a cohort of patients during their residency. However, their graduation almost always requires termination of physician-patient relationships, and transfer of care to incoming residents. We previously reported the results of the first scientific study of the transfer process, identifying 5 independent predictors of patient satisfaction with the process of transferring care to new physicians in an academic medical center.5 Predictors were identified on the basis of questionnaires completed by 376 patients prior to seeing a new resident physician, utilizing univariate analysis followed by stepwise multiple regression. Less than half (47%) of the patients were fully satisfied with the handling of their transfer, another 10% were somewhat satisfied, and 25% were neutral, while the remainder were either somewhat (11%) or very (7%) dissatisfied. Personal notification of the patient by the departing provider was by far the most important determinant, responsible for 41% of the variability in patient satisfaction. Additional independent, but less powerful, predictors included: whether the patient felt the departing physician had done everything possible to facilitate the transfer; whether the physician provided an opportunity to discuss the transfer; whether this discussion was considered sufficient; and patients' impressions of the medical center.
We now report the results of a randomized intervention designed to enhance patient satisfaction with the transfer process, performed in the same clinic a year later, with a different set of senior residents and patients. The first intervention featured interactive seminars on the optimal transfer of care with all senior residents caring for these patients, performed prior to the transfer. Then, at the time of transfer, we randomized half the patients to receive an informational letter from their new doctor. Thus, patients received, in a randomized fashion, either care from a resident who had been exposed to an educational intervention aimed at enhancing transfer techniques (single intervention group) or care from such residents coupled with a transfer letter (dual intervention group). The 2 intervention groups were compared with one another in terms of outcomes as well as to patients from the previous year (historical controls) in which no intervention had occurred.
METHODS
Patients and Setting
The study site was the Internal Medicine Clinic at Walter Reed Army Medical Center, which provides primary care for both active-duty and retired military personnel as well as their dependents. Internal medicine residents follow most of their patients for 2 to 3 years, and upon completion of training, transfer patients to new junior residents who have just completed internship. Patients were eligible for this study if they had just had their care transferred and had at least 2 clinic encounters with the departing resident, including at least 1 visit in the preceding twelve months. After review of clinic files identified 615 patients who appeared to meet entry criteria for the study, 115 were excluded by virtue of: (a) death; (b) dementia; (c) relocation to another area without a forwarding address, or an inaccurate address and phone number on file; (d) selection of another primary physician prior to being informed of the departure of their clinic physician; or (e) despite having seen a resident physician at least twice in this clinic, they reported that their primary care was provided at another site. This left 500 patients eligible for the interventional phase of the study.
Since residents followed patients for 2 to 3 years before transferring their care, and the study was conducted in 2 consecutive years, there was no duplication of patients from Year 1 to Year 2. The study design was approved by the Institutional Review Board of the Department of Clinical Investigation at Walter Reed Army Medical Center.
Questionnaire
A self-administered questionnaire was completed by all participants (available from Dr. Roy on request). The questionnaire was developed after reviewing the medical literature on the transfer of care and patient satisfaction, and modified based upon a pilot study. It enabled comparison of more than 20 potential independent variables with our primary dependent variable, patient satisfaction. The questionnaire asked patients how they learned their doctor would be leaving: by their physician personally, by letter, by a secretary or appointments clerk, or no advance notice. A series of yes/no questions determined whether: (1) patients were told the name of their new doctor; (2) patients expressed their feelings to their doctor; (3) their doctor provided discussed their feelings, and if so, whether the discussion helped them feel better. Additional dichotomous questions explored whether patients would have liked another visit to discuss the doctor's leaving or to follow up on test results, and whether they felt their doctor did everything possible to ease the change. We also assessed their opinion of our hospital in comparison to others on a 5-point Likert scale: excellent, above average, average, below average, or poor. Of greatest importance, we asked how satisfied patients were with the manner in which they learned their doctor would be leaving, measured on a 5-point Likert scale: very dissatisfied, somewhat dissatisfied, neutral, somewhat satisfied, or very satisfied. Several questions that were not found to be useful (e.g., regarding patient reports of specific emotions such as anger or sadness, at what point within an appointment the physician told the patient) in the first year of the study were deleted, and replaced with questions that asked about satisfaction and key predictors in a different manner, all using a 5-point Likert scale, to corroborate the validity of patients' responses. Demographic information was collected both via the questionnaire (years followed in the clinic and number of doctors seen regularly) as well as a computerized hospital database (age, gender).
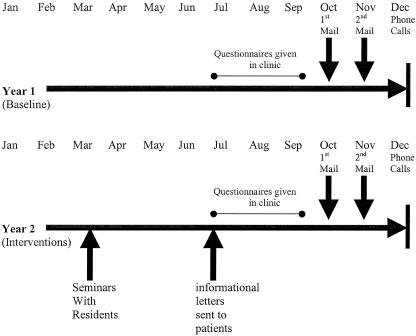
Questionnaires were administered to consecutive patients returning to the clinic for an appointment from July through September for 2 consecutive calendar years (1991 and 1992). Questionnaires were completed in the clinic waiting room prior to each patient seeing their new physician, so that responses would not be confounded by contact with the new physician. No patients returning to the clinic refused to complete the questionnaire. To determine whether patients not returning to the clinic within a few months of the transfer were different from those who had returned, questionnaires were mailed in October of each year to patients who had not yet returned for a clinic visit; this was a randomly selected 50% sample in Year 1, and included all remaining eligible patients in Year 2. A second mailing was sent to nonresponders each November, and follow-up phone contacts were attempted each December to interview nonresponders (Fig. 1).
FIGURE 1.
Study design.
Interventions
Educational Seminars
Interactive 30-minute sessions were held with all 12 senior residents in March of the second year of the study (3 to 4 months prior to their completion of residency and transfer of their patients to a new resident). The seminars were done in small groups (2 or 3 residents in each group) to maximize the opportunity for discussion. The results of the first year of the study were described to residents, with emphasis on the significance of personally informing patients about the transfer of their care, providing the name of the new physician and how to contact him/her or make an appointment, allowing time for discussion of the transfer and for patients to express any feelings they might have about the transfer. If feasible, it was suggested that they offer an additional appointment for further discussion prior to the transfer. This was followed by role-playing in which residents acted out scenarios in which they informed patients of the transfer of their care. Residents were then provided with feedback on their approach, and discussion ensued. All patients in Year 2 of the study were subject to the effects of this intervention.
Personal Letter
A randomly selected 50% of the patients of each departing resident in Year 2 of the study were sent a letter signed by their new physician. The personally addressed letters were mailed on July 1, and among other things, stated “Dr. (name) has left the Walter Reed Internal Medicine Clinic. I am pleased to inform you that I am your new doctor. You can continue to schedule appointments to see me by calling (telephone number).”
Analysis
Statistical analyses were performed using SAS, version 6.03 (SAS Institute, Inc., Cary, NC) and Microsoft Excel 2000 (Microsoft Corporation, Redmond, Wash). The methods of analysis for identification of independent predictors of patient satisfaction have been described previously.7 Briefly, univariate analysis comparing independent variables with patient satisfaction was performed by correlation (for continuous variables such as age), χ2 test (for dichotomous variables such as gender) or Student t-test and analysis of variance (for categorical variables such as impressions of the institution). Factors associated with satisfaction at the P≤ .10 level were then entered into a multiple regression model to identify independent predictors. For comparisons between the no-intervention group (baseline, or Year 1 patients) and the 2-intervention group (Year 2), we used the Mantel-Haenszel χ2 test for linear trends as well as repeated measures analysis of variance for a comparison between mean satisfaction levels for the 3 groups. Multiple logistic regression was performed utilizing the forward selection procedure. Additional questions added in Year 2, with responses graded on 5-point Likert scales ranging from “strongly agree” to “strongly disagree,” were compared to the primary questions utilizing Spearman correlation coefficients, because the variables were categorical.
RESULTS
We enrolled a total of 813 patients who had recently had their care transferred from one resident to another: 376 patients in Year 1, and 437 in Year 2. For the entire study population, the mean age was 65; 407 patients were male and 406 were female. As shown in Table 1, the distribution of patients between the 2 years was similar with respect to age, gender, and median years followed in the clinic. This also was true for each of the randomized groups of the second year. Across the 2 years, 365 patients completed the questionnaire in the clinic, 404 by mail, and 44 by phone. Of those not returning to the clinic within the first 3 months after the transfer of their care, the questionnaire was completed by 85.5% of those eligible for inclusion in the study. Subjects who responded by mail or phone were not significantly different from those who completed questionnaires within the clinic, either demographically or in level of satisfaction. Enrollment rates for Year 1 have been previously reported; in Year 2, review of clinic files identified 615 potentially eligible patients, but 115 were found ineligible, and 437 (86%) of the 500 eligible patients completed questionnaires.
Table 1.
Characteristics of Study Population
| Characteristic | Year 1 | Year 2 Seminar | Year 2 Seminar/Letter | Significance |
|---|---|---|---|---|
| N | 376 | 227 | 210 | |
| Mean age, y | 65 | 65 | 65 | NS |
| Female, % | 48 | 52.2 | 50.7 | NS |
| Median y followed in clinic | 4 | 4 | 4 | NS |
| Told by MD of change, % | 70.5 | 77.8 | 78.4 | .01 |
| Told name of new doctor, % | 76 | 75.8 | 99.5 | * |
| Want another visit to discuss MD's departure, % | 24.2 | 18.0 | 15.1 | .01 |
| Want another visit to follow up on tests, % | 42.5 | 25.1 | 23.1 | <.0001 |
| Feel MD could have done more to ease change, % | 18.2 | 15.5 | 9.4 | .005 |
| Expressed feelings to MD, % | 69.3 | 60.8 | 59.2 | <.05 |
| MD discussed feelings, % | 53.0 | 58.8 | 57.2 | NS |
| Felt better after discussion, % | 91.0 | 91.3 | 96.0 | NS |
| Opinion of institution, mean† | 4.4 | 4.5 | 4.5 | NS |
| Satisfaction with transfer, mean | 3.8 | 4.1 | 4.5 | .0006 |
| Very satisfied, %† | 46.8 | 60.3 | 72.3 | <.0001 |
| Somewhat satisfied, % | 10.4 | 12.5 | 11.8 | |
| Neutral, % | 25.0 | 12.5 | 11.3 | |
| Somewhat dissatisfied, % | 11.4 | 8.5 | 3.3 | |
| Very dissatisfied, % | 6.4 | 6.2 | 1.4 |
The difference between patients being told the name of the doctor before and after the seminar alone is not significant. The letter was from the new physician, thus clearly providing patients with the name of their new doctor, although one patient apparently failed to notice this.
Measured on 5-point Likert scale.
NS, not significant.
The 3 most important independent predictors of patient satisfaction with the transfer process identified in Year 1 were validated in Year 2 of the study. Again, by far the greatest predictor of satisfaction was for the physician to personally inform the patient of their departure (partial R2 = .42), followed by whether the physician could have done more to facilitate the transfer (R2 = .12), and the patient's impressions of the institution (R2 = .02). Likewise, 2 predictors of lesser importance remained significant: whether the doctor provided a discussion of the transfer (R2 = .003), and whether this discussion was deemed significant by the patient (R2 = .016). However, a factor that was not independently associated in Year 1 was slightly more important (R2 = .018) than either of these in Year 2: whether a discussion of the transfer process with their physician helped them to feel better. The R2 for the regression model was higher than for the first year (.59 vs .52), indicating that the predictors identified were responsible for 59% of the variation seen in patient satisfaction.
We added several items to the questionnaire in Year 2 of the study to reiterate important questions in the original questionnaire, seeking to validate responses from patients. In every case, the correlations between the corresponding questions were highly significant (P < .0001). Responses to “I am pleased with the way I was told I would be getting a new doctor” correlated with “How satisfied were you with the way you found out that your doctor would be leaving the clinic” (Spearman correlation coefficient, 0.74). Answers to “My doctor made the transfer of my care as smooth as possible” was inversely correlated with “Could your doctor have done something to make the change easier” (0.53). Two new questions about the site of care (“I can count on doctors at Walter Reed to provide high quality care,” and “I am happy with the care I receive in the internal medicine clinic”) each agreed with responses to “How do you think care at Walter Reed compares to other hospitals” (0.59 and 0.52, respectively).
We compared 3 groups of patients in order to judge the effect of our interventions. No intervention was performed in Year 1; therefore, the 376 patients enrolled in this baseline period served as a historical control group. In Year 2, questionnaires were completed by 227 patients whose doctors had participated in our seminars, and by 210 patients whose doctors participated in the seminars and who also received a letter from their new doctor.
The seminars with residents were associated with a significant increase in the percentage of patients reporting that they were informed by their resident physician of the transfer of their care, from 70.5% at baseline to 78% after the intervention (P = .01). The letter to patients informing them of the transfer had a significant effect on several parameters. For example, when patients were asked, “Would another visit with your doctor have been helpful to discuss his or her leaving?”, nearly one fourth of our baseline group said yes. After our seminars with the residents, only 18% of the patients still desired additional discussion, and an accompanying letter decreased the proportion to 15%. Similarly, the proportion of patients who felt that the doctor could have done something more to ease the transition declined from 18% prior to interventions, to 15.5% after the seminars, and 9.4% after the seminars and letters. Neither intervention had a significant influence on whether patients reported that their physicians discussed their feelings about the transfer with them, or whether this discussion helped them to feel better. Patients in the second year were less likely to report that they expressed their feelings about the transfer to their doctor (59.8% vs 69.3% in Year 1).
Our 2 interventions, the seminars and the letters, had a synergistic effect on patient satisfaction, our primary outcome. As shown in Table 1, the percentage of patients reporting that they were very satisfied with the way their transfer was handled increased from 47% with no intervention, to 60% after the seminars alone, and to 72% after both interventions (P < .0001). In other words, the 2 interventions increased by more than 50% the fraction of patients fully satisfied with the process of transferring their care. Looked at another way, mean satisfaction as measured on a 5-point Likert scale increased from 3.8 at baseline to 4.1 after the seminars alone, and to 4.5 after both seminars and letters (P = .0006).
DISCUSSION
Patient satisfaction is not only a noble goal that physicians should strive for in itself, but is also important for clinical outcomes. It has previously been shown to be a key determinant of patient compliance with medications,6,7 with consequent implications for the efficacy of treatment. Patient satisfaction also has been demonstrated to predict compliance with follow-up, which may be critical to the success of managed care systems competing for patients.8,9 Efforts to increase patient satisfaction are central to the concept of continuous quality improvement. Finally, in some health care systems, physician compensation may be partially dependent upon levels of patient satisfaction.
Our 2-year study represents the first scientific evaluation of the transfer of care process. Several independent predictors of patient satisfaction with the transfer process were identified in the first year and validated in the second year, with a level of predictive power that compares favorably with previous studies of patient satisfaction. Our clinical trial demonstrates that by educating resident physicians on handling the transfer process, it is possible to significantly influence these predictors, and in turn enhance patient satisfaction. In addition, sending letters to patients further potentiates this improvement in satisfaction. The first year of the study demonstrated an association between the predictors and patient satisfaction, but its cross-sectional design lacked the power to show causality. The results from the second year, showing a clear relationship between prospective interventions and improvements in patient satisfaction, strengthen the case that physician or health care system actions influence patient satisfaction.
It is not clear why patients were less likely to report discussing their feelings about the transition with their physicians after the seminar intervention (the letter appeared to have no influence). Perhaps the residents were more adept at addressing their potential concerns, so they no longer felt it necessary to express their feelings. This would be in keeping with patients feeling less need for additional follow-up to discuss test results or to discuss their physician's departure. However, there also appear to be limits to the effects of the seminars with resident physicians: they were no more likely to provide their patients with the name of the new doctor than they had been before.
Our study has several limitations. First, we did not ascertain general satisfaction with the level of care provided by the departing resident, which may have a significant influence on patients' satisfaction with any actions of their resident physician, including the handling of the transfer process. Second, our no-intervention group was an historical rather than a parallel control group. However, the fact that control patients were drawn from the immediately preceding year and were demographically similar to the intervention patients makes the likelihood of secular trends or substantial patient differences less likely. Third, although identification of key independent predictors in a second set of patients helps to validate our first-year study results, replication of the results in another setting or with different types of patients (e.g., psychiatry or pediatrics) would provide greater validation. Moreover, our study was performed in a resident clinic, and there may be something different about patients who see residents; perhaps they are more easily satisfied, more open-minded, or more accepting of transitions, than patients who see private physicians. However, a recent study in university and Veterans Administration hospitals found that patients of resident physicians reported less satisfaction than those of attending physicians.10 Performance of our study at a military institution raises a similar limitation. The demographics and case mix of patients cared for in a military medical center have been shown to be similar to those seen in civilian institutions. Although patient demographics and the case mix at a military medical center resemble those at civilian institutions,11–13 there may be attitudinal differences. For example, military personnel and retirees, and their family members, may be more accustomed to change after periodic disruptions in care when either they or their physicians were subject to transfers or mobilizations. Some patients also may be disinclined to be critical of a military officer—all resident physicians included in the study are also military officers. Such factors would be most likely to diminish the influence that the identified predictors have on satisfaction, and it may be that studies in other settings will have greater power. Each of these limitations relates to the generalizability of our results, which remains a question, because our study involves a relatively small number of residents in a single clinic representing a single medical specialty. It is therefore important for the findings to be replicated in other settings. One additional limitation to acknowledge is that 10 years have passed since the collection of our data, and it may be that attitudinal changes have occurred during this time, perhaps influenced by greater emphasis on managing care, which could have an impact on patient satisfaction with the transfer of care.
One potential limitation present in the first year of the study was that the independent variables as well as the dependent variable were based upon patient responses to single questions. If sizeable numbers of patients misunderstood a question, it could cloud the validity of the results. The companion questions added to the second year questionnaire all showed strong correlations with the initial questions, assuaging this concern.
Our study has a number of strengths. We achieved a high response rate to our questionnaire. The magnitude and additive effect of the interventions upon satisfaction is compelling. Nationwide, thousands of residents graduate and transfer patient care every summer, and we believe the results of this study have significant implications for them. Teaching residents about care transfer can improve this difficult process for them and for their patients. Our results may also be valuable to physicians in practice, whether they are transferring care because of relocation, retirement, or payer contracts, although the utility of the described predictors and interventions in other settings needs to be validated. The interventions we used are simple, harmless, and feasible for a residency program, managed care system, or even an individual or group practice. Benefits include not only greater patient satisfaction but also potentially enhanced adherence to medical recommendations and follow-up. It is possible that the interventions may even be cost effective, because patients exposed to the interventions were less likely to want another visit to discuss their doctor's leaving or to follow up on test results. This could be assessed in future studies. More importantly, in today's competitive health care marketplace, a simple letter or limited discussion may help to provide an edge in retaining patients and maintaining high levels of satisfaction.
Acknowledgments
The authors wish to acknowledge Patricia Koslowe and David Chang of Epistat, Silver Spring, Md, for valuable support in statistical analyses.
The opinions or assertions contained herein are the private views of the authors and are not to be considered as official or as reflecting the views of the Department of the Army, the Department of Defense, or the Department of Veterans Affairs.
REFERENCES
- 1.Rogers J, Curtis P. The concept and measurement of continuity in primary care. Am J Public Health. 1980;70:122–7. doi: 10.2105/ajph.70.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304:1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baker R. Characteristics of practices, general practitioners and patients related to levels of patients' satisfaction with consultations. Br J Gen Pract. 1996;46:601–5. [PMC free article] [PubMed] [Google Scholar]
- 4.Wasson JH, Sauvigne AE, Mogielnicki RP, et al. Continuity of outpatient medical care in elderly men. A randomized trial. JAMA. 1984;252:2413–7. [PubMed] [Google Scholar]
- 5.Roy MJ, Kroenke K, Herbers JE. When the physician leaves the patient: predictors of satisfaction with the transfer of care in a primary care clinic. J Gen Intern Med. 1995;10:206–10. doi: 10.1007/BF02600256. [DOI] [PubMed] [Google Scholar]
- 6.Hulka BS, Cassel JC, Kupper LL, Burdette JA. Communication, compliance, and concordance between physicians and patients with prescribed medications. Am J Public Health. 1976;66:847–53. doi: 10.2105/ajph.66.9.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linn MW, Linn BS, Stein SR. Satisfaction with ambulatory care and compliance in older patients. Med Care. 1982;20:606–14. doi: 10.1097/00005650-198206000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Wartman SA, Morlock LL, Malitz FE, Palm EA. Patient understanding and satisfaction as predictors of compliance. Med Care. 1983;21:886–91. doi: 10.1097/00005650-198309000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Weisman CS, Nathanson CA. Professional satisfaction and client outcomes: a comparative organizational analysis. Med Care. 1985;23:1179–92. doi: 10.1097/00005650-198510000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Yancy WS, Macpherson DS, Hanusa BH, et al. Patient satisfaction in resident and ambulatory care clinics. J Gen Intern Med. 2001;16:755–62. doi: 10.1111/j.1525-1497.2001.91005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson JE, Pinholt EM, Jenkins TR, Carpenter JL. Content of ambulatory internal medicine practice in an academic Army medical center and an Army community hospital. Mil Med. 1988;153:21–5. [PubMed] [Google Scholar]
- 12.Jackson JL, Strong J, Cheng EY, Meyer G. Patients, diagnoses, and procedures in a military internal medicine clinic: comparison with civilian practices. Mil Med. 1999;164:194–7. [PubMed] [Google Scholar]
- 13.Jackson JL, O'Malley PG, Kroenke K. A psychometric comparison of military practices. Mil Med. 1999;164:112–5. [PubMed] [Google Scholar]