Abstract
OBJECTIVE
To decrease unnecessary antibiotic use for acute respiratory tract infections in adults in a point-of-service health care setting.
DESIGN
Prospective, nonrandomized controlled trial.
SETTING
An urban urgent care clinic associated with the major indigent care hospital in Denver, Colorado between October 2000 and April 2001.
PATIENTS/PARTICIPANTS
Adults diagnosed with acute respiratory tract infections (bronchitis, sinusitis, pharyngitis, and nonspecific upper respiratory infection). A total of 554 adults were included in the baseline period (October to December 2000) and 964 adults were included in the study period (January to April 2001).
INTERVENTIONS
A provider educational session on recommendations for appropriate antibiotic use recently published by the Centers for Disease Control and Prevention, and placement of examination room posters were performed during the last week of December 2000. Study period patients who completed a brief, interactive computerized education (ICE) module were classified as being exposed to the full intervention, whereas study period patients who did not complete the ICE module were classified as being exposed to the limited intervention.
MEASUREMENTS AND MAIN RESULTS
The proportion of patients diagnosed with acute bronchitis who received antibiotics decreased from 58% during the baseline period to 30% and 24% among patients exposed to the limited and full intervention, respectively (P < .001 for intervention groups vs baseline). Antibiotic prescriptions for nonspecific upper respiratory tract infections decreased from 14% to 3% and 1% in the limited- and full-intervention groups, respectively (P < .001 for intervention groups vs baseline).
CONCLUSION
Antibiotic use for adults diagnosed with acute respiratory tract infections can be reduced in a point-of-service health care setting using a combination of patient and provider educational interventions.
Keywords: antibiotic, acute respiratory tract infections, patient education, quality improvement
Decreasing excess antibiotic consumption in ambulatory practice is an important objective for combating rising rates of antibiotic resistance among community bacterial pathogens such as Streptococcus pneumoniaeStaphylococcus aureus. Acute respiratory tract infections (ARIs) (such as colds, ear infections, and bronchitis) collectively are the single most frequent reason for seeking ambulatory medical care in the United States, and account for about 75% of ambulatory antibiotic prescriptions each year.1,2 Acute respiratory tract infections are important targets for strategies aimed at reducing excess antibiotic use in the United States, because antibiotics are frequently prescribed even for those illnesses that have a predominantly viral etiology (e.g., colds, upper respiratory infections, and bronchitis).3
Recent evidence suggests that primary care physicians are beginning to heed the call to limit antibiotic prescribing for ARIs. An analysis of U.S. ambulatory antibiotic prescribing practices estimates that overall antibiotic prescribing for ARIs decreased from 65% of visits in 1995 to 52% of visits in 1999.4 However, there is still significant room for improvement, since it has been estimated that only 25% of patients with ARIs who seek medical attention have a bacterial etiology of their illness.5 Achieving additional decreases in excess antibiotic use may require coordinated efforts developed and implemented at the local level that are tailored to the specific characteristics of patients, providers, and practice settings.
The importance of patient education is a consistent finding of previous interventions to decrease inappropriate antibiotic use in ambulatory practices.6,7 Physician-centered interventions that have used education, practice guideline dissemination, or practice profiling with feedback have resulted in little or no success.8–10 However, multidimensional interventions using both physician and patient education appear to hold greater promise. A multisite, controlled intervention at a group-model HMO that consisted of physician and patient education (using household and office level materials) showed significant reductions in antibiotic use for adults with acute bronchitis.6 This effect was sustained with minimal reinforcement during the subsequent winter.11 Similarly, a community- and office-based intervention by Finkelstein et al. consisting of physician education by a peer leader (including feedback on previous prescribing rates), patient home mailings, and waiting room materials also showed a decrease in antibiotic use for children in managed care office practice settings.7 Both of these trials employed patient/parent educational materials that required adequate literacy and English language skills. It is challenging to transfer these types of interventions to point-of-service practice settings, particularly those serving socioeconomically and ethnically diverse populations, in which literacy and language barriers are common.
The present study differs from previous work by our group and others by targeting a vastly different patient and provider population: patients and providers in a point-of-service health care setting (i.e., an urgent care clinic); and patients belonging to very low socioeconomic strata. In addition, the intervention developed to address these differences—an interactive computerized education (ICE) tool—has not been previously described or evaluated for this purpose. We hypothesized that education of our provider staff in combination with a patient-directed ICE (to overcome language and literacy barriers to traditional forms of patient education, such as printed materials) would optimize antibiotic prescriptions for ARIs in an urban urgent care setting by reducing prescriptions for predominately viral ARIs (bronchitis, colds) and by limiting antibiotic treatment to adults with sinusitis that fulfill recommended clinical criteria for antibiotic therapy.12 Interactive computerized education modules have advantages over other modes of assessment and education in that they provide a private learning environment, are designed to give user-customized information, save time by providing interactive information before/after a provider visit, and use audio/visual formats suitable for low-literacy populations.13–15
METHODS
Setting
This study was performed in the Walk-in Clinic (WIC) at Denver Health Medical Center (DHMC), a 349-bed, public city hospital associated with a vertically integrated network of 11 community health centers in Denver, Colorado. Seventy-one percent of patient charges at DHMC are for Medicaid, medically indigent, or self-paying patients who lack health insurance. The population served by Denver Health is 50% Hispanic, 25% Caucasian, 15% African American, and 1% Native American. Approximately 21% of all visits to the WIC are by patients who are monolingual Spanish.
The WIC is located within DHMC and provides urgent care services for adults, serving more than 43,000 patients per year. The WIC is open 7 days a week from 7:30 am to 11:00 pm. Patients with trauma within 24 hours or with certain vital sign abnormalities (oral temperature ≥40°C, pulse oximetry <88%, pulse >130 beats per minute) are triaged to the emergency department. Patients are seen without appointment on a first-come basis and are evaluated in the clinic regardless of their ability to pay. The WIC is staffed with internists and nurse practitioners; in addition, medical students and residents provide patient care under the supervision of a designated staff physician. The staff physician is responsible for signing charts of the nurse practitioners but is only consulted in the more complex cases. During winter months, ARIs (defined as visits with principal diagnoses of nonspecific upper respiratory tract infection (URI), pharyngitis, sinusitis, otitis media, bronchitis, or pneumonia) account for 27% of visits. An audit of the management of patients diagnosed with acute bronchitis revealed that 82% were prescribed an antibiotic in December 1999.
Design
We conducted a prospective nonrandomized, controlled trial of a multimodal educational intervention to reduce antibiotic use for ARIs. The baseline period was October through December 2000. The study/intervention period was January through April 2001.
Intervention
Our intervention strategy was composed of 3 components: 1) a provider educational session; 2) examination room posters directed at providers; and 3) a patient-directed ICE module. The provider education session occurred in the last week of December 2000 and was attended by 75% (6/8) of physicians and 70% (7/10) of nurse practitioners who have regular shifts in the clinic. One of the study investigators (RH) conducted the 1-hour educational session. During this session, guidelines for appropriate antibiotic use for treatment of acute respiratory tract infections in adults, based on those recently developed by the Centers for Disease Control and Prevention, were presented.12,16–18 Major points included in the presentation were: 1) the lack of effectiveness of antibiotics in uncomplicated acute bronchitis and nonspecific URIs in adults; 2) that antibiotics should not be prescribed to patients with mild to moderate rhinosinusitis, especially with fewer than 7 days of symptoms; and 3) that recent antibiotic use is a major risk factor for nasopharyngeal carriage and invasive disease with drug-resistant S. pneumonia. Two 11 × 17-inch posters were placed in each of the WIC's 15 examination rooms at the initiation of the study period. One poster included a graphic depicting the lack of effect of antibiotic treatment on duration of illness for acute bronchitis. The other poster listed diagnoses for which antibiotics were not indicated (URI, rhinosinusitis with less than 7 symptom days, and acute bronchitis) and included 2 graphics: 1) the epidemiological curve for the prevalence of invasive antibiotic-resistant S. pneumonia in Colorado; and 2) a graph depicting the association between prior antibiotic use and the risk of carriage of antibiotic-resistant S. pneumonia. These same graphics were previously used in a successful multidimensional intervention in a group-model HMO setting.6
The ICE module for patients was a computer-based audio-visual, bilingual (English and Spanish) program that communicated a likely illness diagnosis, self-care strategies, and the role of antibiotics (or lack thereof) in the management of their illness. The survey was written in English at a 6th-grade reading level. A professional medical interpreter then translated it into Spanish. Two of the authors who are bilingual reviewed the translation for cultural appropriateness to the predominantly Mexican population served by the WIC. Finally, the bilingual actress who audiotaped each question then reviewed each Spanish language passage prior to recording. The first component of the program was a 58-item knowledge, attitude, and behavior survey. The results of this survey are being analyzed and reported separately. The second part of the program included an ARI symptom inventory and a past medical history review. A likely diagnosis was calculated based upon the symptom inventory and vital signs. The computer then provided a short audio and text-based educational session relating to the computer-generated ARI diagnosis, a language-appropriate printout of this same information, and an English language printout of the reported symptoms, without the computer generated ARI diagnosis, for the patient to give to the provider. Patients completed the interaction in a mean time of 18.6 minutes and median of 17.4 minutes (range, 8.6 to 44.9 min). Two personal computers with the ICE module were placed in the waiting room during the intervention period.
The analysis of the correlation between computer-based diagnosis and clinician diagnosis is currently being analyzed and will be reported separately. Challenges in interpreting these data include lack of a reliable referent standard, since clinician-assigned diagnoses may not follow evidence-based recommendations on which the computer-generated diagnoses were based. In addition, clinicians based their diagnoses on physical examination findings, which were not incorporated into the computer-based algorithms. Given these considerations, preliminary analyses showed that computer-generated diagnoses had the following sensitivity/specificity/positive likelihood ratio using clinician diagnosis as the referent standard: pharyngitis (83%/80%/10.8); sinusitis (25%/93%/3.5); bronchitis (33%/84%/2.1). Although the computer never provided a likely diagnosis of pneumonia, the need to exclude pneumonia as a message was generated for specific chief complaints (e.g., chest pain, shortness of breath, bronchitis with vital sign abnormalities). The sensitivity/specificity/positive likelihood ratio compared to clinician assigned diagnosis of pneumonia was 80%/64%/6.8.
Patients were classified as having limited or full exposure to the intervention. Patients who did not perform the ICE module were classified as receiving a limited intervention, because ARI prescribing patterns for these patients (compared to the baseline period) would be primarily associated with the impact of the provider educational session and examination room posters. Patients who performed the ICE module were classified as receiving the full intervention.
Subjects
Patients eligible for the ICE module included all English- or Spanish-speaking adults 18 years of age and older who presented to the WIC with symptoms of an ARI (cough, sore throat, nasal congestion, ear ache) during the intervention period. After triage evaluation, patients with ARI symptoms were approached in the waiting room by our study coordinator. They were asked to participate in the study by completing the ICE module, and were offered a $2 gift certificate for food as an incentive to participate. Patients were briefly introduced to the computer and its purpose and were helped with the entry of vital signs (measured at triage) and medical record number. At the beginning of the module, patients completed a computerized informed consent, which was approved by the Colorado Multiple Institutional Review Board. After completion of the ICE module, patients were evaluated in the clinic. By default, patients who chose not to complete the ICE module were assigned to the limited-intervention group. All patients in the limited-intervention group had usual care, but may have had their care altered by the information provided during the physician education session or by information provided on the examination room posters. Because the physician education session and examination room posters were compatible with routine quality improvement activities of the clinic, there was no informed consent procedure employed for limited-intervention patients during this period. Providers were not blinded as to whether patients with ARI symptoms had completed the computer education, and providers understood that the objective of the exam room posters, provider education session, and ICE module was to decrease antibiotic prescribing for ARIs.
To identify patient visits for the baseline and limited-intervention groups, visits diagnosed as nonspecific URI (or common cold, viral syndrome), bronchitis (or cough illness), pharyngitis (or sore throat), sinusitis, and pneumonia were identified from WIC log sheets. All physicians and nurse practitioners who cared for patients diagnosed with ARIs in the baseline and study periods were included in the analysis. Providers directly involved in the design and implementation of the study, along with corresponding patient visits, were excluded.
Measurements
To analyze the impact of the intervention, medical record review was conducted on patients receiving the full intervention, as well as on a systematic sample of visits occurring October 2000 through March 2001. For the baseline and-limited intervention group analysis, depending on the total number of ARI visits in 1week, every third or fourth ARI case was selected to achieve 50 to 70 ARI visits per week for review. This strategy was employed to ensure that each day of the study period was represented equally. We chose to perform daily systematic sampling to limit potential bias that could be introduced by fluctuations in viral etiologies, or by daily variations in staffing composition, that might not have been adequately accounted for in a random sample of visits. Data on patient age, gender, and ethnicity from hospital administrative files were merged with the data from the medical record review.
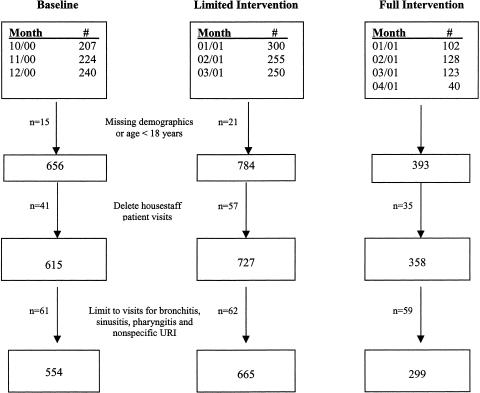
A total of 1,869 patient encounters were initially reviewed. A flow diagram stratified by group assignment is shown in Figure 1. Administrative demographic data were missing for 32 of the patients, and 4 of the patients were less than 18 years of age, excluding these patients from analysis. In addition, 133 visits in which the primary providers were residents or students were excluded, as were 182 visits for a diagnosis of pneumonia (n = 46), asthma (n = 86), otitis media (n = 18), no diagnosis (n = 21) or “other” (n = 11). The “other” diagnosis represented patients who initially reported ARI symptoms and were recruited for the ICE tool, but who, when evaluated by the provider, were given non-ARI diagnoses (e.g., depression, migraine, or chronic bronchitis).
FIGURE 1.
Flow diagram for subject enrollment, by group assignment.
Statistical Analysis
We conducted an intent-to-treat analysis, whereby patients who initiated the ICE module, getting past the initial questions on sociodemographics, were included in the full-intervention group. The primary outcome measures were the proportion of bronchitis, pharyngitis, sinusitis and URI visits prescribed an antibiotic, and the proportion of antibiotic-treated sinusitis visits having an illness duration of ≥7 days. Comparisons in the primary outcome measures between baseline and intervention periods, as well as by patient age, gender, race/ethnicity, tobacco use, diagnosis, and provider type were performed using the χ2 test. Because there was no difference in antibiotic prescription rates among patients in the limited- (31%) and full-(34%) intervention groups (P = .25), the 2 groups were combined for multivariable analysis. The dependent variable was antibiotic treatment for all ARIs, and independent variables included race/ethnicity, tobacco use, provider type, and specific ARI diagnosis. Independent variables considered for the multivariable model predicting antibiotic use included patient age, gender, race/ethnicity, tobacco use, diagnosis, and provider type. Variables that were associated with antibiotic use on bivariate testing with a P < .20 were included in the final multivariable model.19 Specific ARI diagnoses also were included in the multivariable model to control for potential shifts in use of diagnosis categories between baseline and intervention periods. Interaction terms between the intervention period and the other independent variables were tested for significance (P < .05) in order to assess whether different rates of change in antibiotic treatment were associated with these patient, provider, and illness characteristics. Patients were classified as having received the full intervention only if they completed all the initial demographic data and the self-assigned diagnosis question. For full-intervention patients who did not complete the ICE module before being called to the exam room, subsequent responses were treated as missing data. All statistical tests were performed using the SAS statistical application software (version 8.2; SAS, Inc., Cary, NC).
Statistical analyses were performed by investigators who had full access to all data, and analyses were performed without restrictions or outside control by the sponsor. The authors report no potential conflict of interest and accept full responsibility for the integrity and accuracy of the data and data analysis.
RESULTS
Table 1 displays the demographic characteristics of the baseline, limited-intervention and full-intervention groups. For all groups, the patient populations were predominantly Hispanic and less than 45 years of age, with high rates of tobacco use. There were some modest differences in the distribution of specific ARI diagnoses in the full-intervention group. For example, the proportion of ARI visits given a URI diagnosis was less for the full-intervention group (47%) compared to the limited-intervention group (54%), whereas there was a greater proportion of ARI visits given a bronchitis/cough diagnosis in the full-intervention group (18%) compared to the limited-intervention group (12%; P = .04). Approximately equal numbers of visits were cared for by physicians and nurse practitioners, with a small proportion of visits cared for by residents and medical students. Nurse practitioners (N = 17) cared for 56% of the patient visits in our study population, and physicians (N = 25) cared for the remaining 44% of patients. There was no statistically significant difference in the proportion of visits cared for by a nurse practitioner compared to a physician across the 3 arms of the study (P = .27). P values for comparisons between physician and nurse practitioner visit rates within study groups were: baseline, .27; limited, .20; and full, .32. There were very few patients with more than 1 visit in the sampling frame (4 in the baseline group, 8 in the limited group, and 0 in the full-intervention group).
Table 1.
Demographic Characteristics of Patients Presenting with Acute Respiratory Tract Infections by Intervention Group
| Intervention Group* | ||||
|---|---|---|---|---|
| Characteristic | Baseline (N = 554) | Limited (N = 665) | Full (N = 299) | P Value† |
| Age, y, n (%) | .21 | |||
| 18–30 | 227 (41) | 295 (44) | 133 (44) | |
| 31–44 | 218 (39) | 220 (33) | 108 (36) | |
| ≥45 | 109 (20) | 150 (23) | 58 (20) | |
| Female gender, n (%) | 337 (61) | 390 (59) | 180 (60) | .73 |
| Race/ethnicity, n (%) | <.01 | |||
| White | 214 (39) | 247 (37) | 106 (35) | |
| Hispanic | 235 (42) | 317 (48) | 123 (41) | |
| African American | 86 (16) | 78 (12) | 26 (9) | |
| Other | 19 (3) | 23 (3) | 44 (15) | |
| Current tobacco smoker, n (%) | 223 (42) | 270 (42) | 135 (45) | .60 |
| Duration of illness <7 days, n (%) | 338 (61) | 394 (60) | 160 (54) | .11 |
| Diagnosis, n (%) | <.01 | |||
| URI/viral illness | 263 (48) | 359 (54) | 139 (47) | |
| Pharyngitis | 140 (25) | 153 (23) | 62 (21) | |
| Sinusitis | ||||
| <7 Days of illness | 40 (7) | 16 (2) | 11 (4) | |
| ≥7 Days of illness | 40 (7) | 56 (9) | 32 (11) | |
| Bronchitis/cough | 71 (13) | 81 (12) | 54 (18) | |
| Provider type, n (%) | .27 | |||
| Internist | 261 (47) | 286 (43) | 127 (42) | |
| Nurse practitioner | 293 (53) | 379 (57) | 172 (58) | |
| Median visits per provider, n (IQR) | .30 | |||
| Internist | 6.0 (2 to 19) | 12.0 (3 to 23) | 5.5 (2 to 11) | |
| Nurse practitioner | 14.5 (3.5 to 28) | 17.5 (6 to 37.5) | 9.0 (2 to 19) | |
ns vary due to nonresponse by no more than 4%.
Tests of significance based on χ2 test except for median visits per provider (based on Wilcoxon Rank Sum Test).
URI, upper respiratory tract infection; IQR, interquartile range.
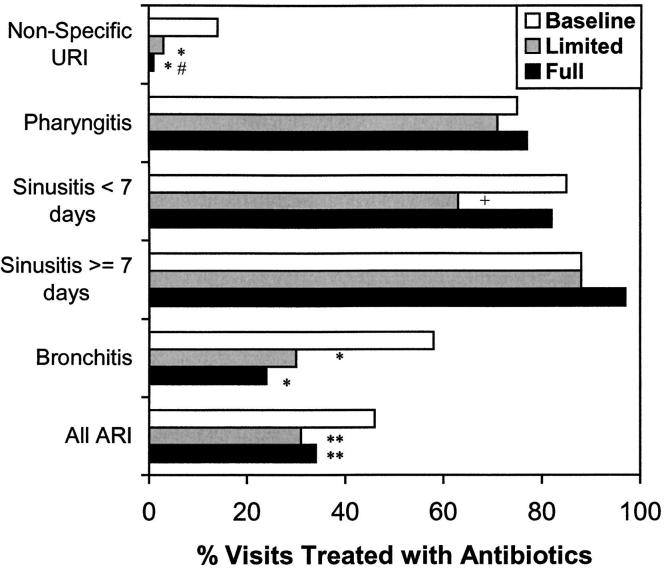
Figure 2 shows stratified antibiotic prescription rates for adults with nonspecific URI, pharyngitis, sinusitis, and bronchitis during the baseline and intervention periods. One of the major messages of the educational intervention was to stop prescribing antibiotics for nonspecific URIs and acute bronchitis. Compared to the baseline period, both the limited- and full-intervention groups had substantially lower antibiotic prescription rates for bronchitis and nonspecific URIs (Fig. 2). The proportion of patients diagnosed with bronchitis that received antibiotics decreased from 58% in the baseline group to 30% and 24% in the limited- and full-intervention groups, respectively (P < .001 for intervention groups vs baseline; no difference between limited- and full-intervention groups). Nonspecific URI antibiotic prescriptions decreased from 14% in the baseline group to 3% and 1% in the limited- and full-intervention groups, respectively (P < .001 for intervention groups vs baseline; no difference between limited- and full-intervention groups). A second major message of the educational intervention was to improve the diagnosis and treatment of acute rhinosinusitis by recommending that antibiotic treatment be reserved for patients with at least 7 days of symptoms (in addition to sinus-localizing features) in accordance with recent CDC recommendations.12 As shown in Figure 2, antibiotic prescription rates for sinusitis did not change after the intervention, regardless of duration of symptoms. However, among patients diagnosed with sinusitis and treated with antibiotics, the proportion that had illness duration ≥7 days increased from 51% in the baseline period to 83% in the limited-intervention group and 78% in the full-intervention group (P < .001 for baseline vs limited- or full-intervention groups). Antibiotic prescribing for pharyngitis did not differ between the groups. Total antibiotic prescription rates for all ARIs for the limited- (31%) and full- (34%) intervention groups were significantly lower compared to the baseline period (46%; χ2 test; P < .001).
FIGURE 2.
Impact of a multimodal education intervention on antibiotic prescription rates for acute respiratory tract infections by diagnosis. *P < .001, limited and full intervention compared to baseline group; #P = .10, full intervention compared to limited group; +P = .06, limited intervention compared to baseline group; **P value < .001 limited and full intervention compared to baseline group.
Multivariable logistic regression analyses were performed to identify independent predictors of antibiotic treatment of ARIs in our clinical setting and to control for shifts in diagnosis assignment as contributing to changes in antibiotic prescription rates between periods. The intervention period was associated with a decreased likelihood of antibiotic use for ARIs compared to the baseline period (adjusted odds ratio [OR], 0.43; 95% confidence interval [95% CI], 0.31 to 0.59), independent of patient race/ethnicity, tobacco use, specific ARI diagnosis, and provider type. Bronchitis and nonspecific URI were associated with a decreased likelihood of antibiotic use compared to pharyngitis, whereas sinusitis was associated with a greater likelihood of antibiotic use (Table 2). Current tobacco use was associated with a greater likelihood of antibiotic treatment (adjusted OR, 1.7; 95% CI, 1.3 to 2.3). Nurse practitioners were less likely than physicians to prescribe antibiotics for ARIs (adjusted OR, 0.42; 95% CI, 0.31 to 0.57). Bronchitis and nonspecific URIs each had a significantly lower association with antibiotic treatment during the intervention period compared to the baseline period (based on the addition of an interaction term between diagnosis and time period to the full multivariable model described above; P = .012 and .001, respectively). Additional models testing interactions between time period, provider type, and smoking status showed no significance (P = .32 and .72, respectively).
Table 2.
Independent Predictors of Antibiotic Treatment for Patients with Acute Respiratory Infections (N = 1,471)
| Adjusted Odds Ratio (95% CI) | |
|---|---|
| Baseline period | Referent |
| Intervention period | 0.4 (0.3 to 0.6) |
| Race/ethnicity | |
| White | Referent |
| Hispanic | 0.8 (0.6 to 1.2) |
| African American | 1.1 (0.7 to 1.7) |
| Other | 1.4 (0.7 to 2.6) |
| Provider type | |
| Internist | Referent |
| Nurse practitioner | 0.4 (0.3 to 0.6) |
| Diagnosis | |
| Pharyngitis | Referent |
| Bronchitis | 0.2 (0.1 to 0.3) |
| Sinusitis | 2.2 (1.3 to 3.5) |
| URI | 0.02 (0.01 to 0.03) |
| Nonsmoker | Referent |
| Current smoker | 1.7 (1.3 to 2.3) |
URI, upper respiratory tract infection.
DISCUSSION
In an urban, urgent care clinic that serves a predominantly minority, low-socioeconomic population, we have demonstrated that antibiotic prescribing for ARIs is high. The levels of antibiotic prescribing for nonspecific URIs and bronchitis are in the range that has been measured in other private practice settings. We have also demonstrated that antibiotic prescribing behavior for ARIs can be improved using a multimodal intervention strategy that consisted of provider education, examination room posters, and a computer-based education module, although an added value of the computer-based education module was not evident. Specifically, this multimodal intervention reduced antibiotic prescription rates for patients with diagnoses of predominantly viral conditions, and shifted the diagnostic criteria for antibiotic treatment of sinusitis toward that recommended by recently published national guidelines. During the intervention period, providers appeared to diagnose sinusitis less frequently in patients with <7 days of symptoms (i.e., 40 of 80 patients [50%] diagnosed with sinusitis in the baseline period had symptoms <7 days, compared to 27 of 115 patients [23%] diagnosed with sinusitis in the study period; P = .001). Interestingly, nurse practitioners were less likely to prescribe antibiotics for ARIs than were physicians. In the WIC, provider assignment is not based upon degree of illness or vital-sign abnormalities, and therefore, patient selection bias would not have affected these results. Guideline use and guideline incorporation into practice habits may align more easily with nurse practitioner training than with physician training. In a subsequent analysis of a prior study in group-model HMO practices, we also found that nurse practitioners improved prescribing behavior to a greater degree than did physicians in the first year of the intervention; but physicians “caught-up” with nurse practitioners in the subsequent year.20 The decrease in antibiotic treatment of ARIs was independent of the distribution of specific ARI diagnoses that might justify antibiotic use. The changes that occurred in antibiotic prescribing during the study period correlated specifically with the emphasized educational points of the provider education session and examination room posters. The specificity of changes in prescription and diagnosis behavior supports the conclusion that these changes were a direct result of the intervention.
A major limitation of our study was that we did not include a concurrent control clinic in which no intervention was performed. On the basis of temporal trends of the influenza season in Denver during our study (January to February), we probably had more influenza visits during the intervention period than during the baseline period. Influenza diagnostic testing is not routinely performed in the WIC, and therefore most suspected influenza is labeled “viral syndrome,” URI, or bronchitis. During the study period there were no competing antibiotic campaigns targeted to our providers or patient population that would have influenced prescribing. The dramatic change in prescribing and the specificity of some of the changes in prescribing argue against the national temporal trend in ARI antibiotic prescription reductions as the cause for the change in prescribing habits, but without a concurrent control the magnitude of temporal trend effect is unknown.
It is also difficult to determine whether diagnostic shift by the provider could account for the reduction in prescriptions for URI and acute bronchitis. It is possible that during the intervention period, providers could have changed a URI diagnosis to sinusitis or a bronchitis diagnosis to atypical pneumonia in order to justify an antibiotic. Another limitation of our study was the lack of demographic data, such as comorbidities, insurance, education level, income, and housing status, which may confound the prescription rates. However we cannot hypothesize a reason why these variables would be distributed unevenly across the intervention groups. Patients diagnosed with chronic obstructive pulmonary disease or chronic sinusitis were not included in the sample. The use of systematic sampling of visits for the comparison groups (baseline and limited-intervention) was used to guarantee equal representation of work shifts and clinic days; however, this also could have resulted in bias if there was maldistribution of providers or illness syndromes as a result. We believe this was unlikely, given that we sampled a high frequency of visits (1 out of every third or fourth visit). A final limitation of our study was the lack of outcome data to suggest either a positive or negative effect of our intervention on our patients' health.
During the intervention period, we found that the total antibiotic prescription rate for all ARIs (bronchitis, sinusitis, pharyngitis, and nonspecific URI) fell to 32% from a baseline of 46%, which equates to 140 fewer antibiotic prescriptions per 1,000 ARI patient visits. In the study clinic, we estimate that the intervention resulted in approximately 500 fewer antibiotic prescriptions for ARIs over 4 months. The sustainability of this reduction in antibiotic prescribing is unknown in our study. A previous study6 in a different population did show a sustained effect over the subsequent ARI season.11
Real or assumed patient expectations have often been cited as one of the reasons for the excessive use of antibiotics in ARIs, and only interventions that have incorporated patient education components have been successful in decreasing total antibiotic use for ARIs. Traditional types of patient education often have relied heavily on patient literacy and English-language skills, two skills that are underrepresented in many public urban practice settings. ICE modules have reported good acceptability in patient populations with low-socioeconomic backgrounds, in part due to the nonthreatening nature of the education.14 ICE modules improve knowledge and involve patients in their own decision making,21 and could be cost-effective and efficient ways to deliver patient education at the point of care. A previous study of an ICE module to educate patients about the common cold reduced the time of health care visits for URIs, and the patients in that study felt the computer-based information was reliable and accurate.13
Our study failed to show any additional benefit from the ICE module, even though we were able to overcome some of the traditional barriers encountered in educating an urban underrepresented patient population by implementing a bilingual ICE module. There could be several reasons why an additive effect on prescribing patterns was not seen. First, provider awareness of the existence of such an educational tool in the waiting room could have caused a generalized effect on prescribing to all patients with ARIs. Second, the ICE module may have been effective in modifying patient expectations and demands for antibiotics, but providers generalized its effect to non-ICE module patients. Third, providers in a public health care setting may be less influenced by patient expectations than providers in a private setting. Overcoming patient expectations of antibiotics may be easier in a public hospital urgent care setting because the clinicians are in general less concerned, compared with private practice, with maintaining a practice population. There is also an inherent anonymity of a denial for antibiotics in an urgent care setting, since the same clinician is unlikely to se the patient for a revisit with worsening illness. Fourth, a change in patient expectations may not correlate with a change in the provider's perception of patient expectation. Fifth, the ICE module may not have provided effective education and therefore did not change expectations. Further studies are needed to determine if ICE modules change patient expectations.
The results of this study show that a multidimensional educational intervention can be effective in improving antibiotic use for ARIs in an urban urgent care clinic. The clinical specificity of our educational points may have been the key to the success of our clinician education. The educational session and the posters were designed with specific recommendations (acute bronchitis should not receive antibiotics; sinusitis less than 7 days should not be given antibiotics). These specific recommendations translated into specific alterations in prescribing habits. Clinician education alone, particularly among nurse practitioners, may be effective in changing clinical behavior in an urban urgent care setting, in which there is more “anonymity” and less financial pressure to maintain a practice population. The most complex and costly component of our education, the patient ICE tool, did not have a measurable additive effect on prescribing compared to clinician education alone. Further studies need to be done to better characterize what ICE module format would be most effective in patients with low literacy. Effective modules should reduce patient expectations for antibiotics and in turn reduce prescription rates for ARIs.
Acknowledgments
The authors would like to acknowledge the administrative and conceptual contributions of Kenneth Gershman, MD, MPH, of the Colorado Department of Public Health and Environment.
This work was supported by the Centers for Disease Control via Epidemiologist and Laboratory Capacity for Infectious Diseases Cooperative Agreement Program 95043/97020.
REFERENCES
- 1.Schappert SM. Ambulatory care visits of physician offices, hospital outpatient departments, and emergency departments, United States, 1995. Vital Health Stat 13. 1997;129:1–38. [PubMed] [Google Scholar]
- 2.McCaig LF, Hughes JM. Trends in antimicrobial drug prescribing among office-based physicians in the United States. JAMA. 1995;273:214–9. [PubMed] [Google Scholar]
- 3.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–4. [PubMed] [Google Scholar]
- 4.Gonzales R, Maselli J, Sande MA. Trends in antimicrobial treatment of acute respiratory tract infections by United States primary care physicians, 1994–1999. J Gen Intern Med. 2001;16(suppl):196–7. [Google Scholar]
- 5.Gonzales R, Malone D, Sande MA. Estimating the amount and cost of ideal and excess antibiotic use for acute respiratory tract infections in the United States. Clin Infect Dis. 2001;33:757–62. doi: 10.1086/322627. [DOI] [PubMed] [Google Scholar]
- 6.Gonzales R, Steiner JF, Lum A, Barrett PH., Jr Decreasing antibiotic use in ambulatory practice: impact of a multidimensional intervention on the treatment of uncomplicated acute bronchitis in adults. JAMA. 1999;281:1512–9. doi: 10.1001/jama.281.16.1512. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7. doi: 10.1542/peds.108.1.1. [DOI] [PubMed] [Google Scholar]
- 8.Poses RM, Cebul RD, Wigton RS. You can lead a horse to water–improving physicians' knowledge of probabilities may not affect their decisions. Med Decis Making. 1995;15:65–75. doi: 10.1177/0272989X9501500110. [DOI] [PubMed] [Google Scholar]
- 9.Mainous AG, III, Hueston WJ, Love MM, Evans ME, Finger R. An evaluation of statewide strategies to reduce antibiotic overuse. Fam Med. 2000;32:22–9. [PubMed] [Google Scholar]
- 10.O'Connor PJ, Amundson G, Christianson J. Performance failure of an evidence-based upper respiratory infection clinical guideline. J Fam Pract. 1999;48:690–7. [PubMed] [Google Scholar]
- 11.Gonzales R, Steiner JF, Maselli JH, Miller R, Lum A, Barrett PH., Jr Sustainability of an intervention strategy for reducing antibiotic use for uncomplicated acute bronchitis. J Gen Intern Med. 2000;15(suppl):118. [Google Scholar]
- 12.Hickner JM, Bartlett JG, Besser RE, Gonzales R, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for acute rhinosinusitis in adults: background. Ann Intern Med. 2001;134:498–505. doi: 10.7326/0003-4819-134-6-200103200-00017. [DOI] [PubMed] [Google Scholar]
- 13.Buchanan BG, Moore JD, Forsythe DE, Carenini G, Ohlsson S, Banks G. An intelligent interactive system for delivering individualized information to patients. Artif Itell Med. 1995;7:117–54. doi: 10.1016/0933-3657(94)00029-r. [DOI] [PubMed] [Google Scholar]
- 14.Reis J, Wrestler F. Consumer attitudes toward computer-assisted self-care of the common cold. Patient Educ Couns. 1994;23:55–62. doi: 10.1016/s0738-3991(05)80022-9. [DOI] [PubMed] [Google Scholar]
- 15.Kinzie MB, Schorling JB, Siegle M. Prenatal alcohol education for low-income women with interactive multimedia. Patient Educ Couns. 1993;21:51–60. doi: 10.1016/0738-3991(93)90059-6. [DOI] [PubMed] [Google Scholar]
- 16.Gonzales R, Bartlett JG, Besser RE, Cooper RJ, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of uncomplicated acute bronchitis: background. Ann Intern Med. 2001;134:521–9. doi: 10.7326/0003-4819-134-6-200103200-00021. [DOI] [PubMed] [Google Scholar]
- 17.Cooper RJ, Hoffman JR, Bartlett JG, et al. Principles of appropriate antibiotic use for acute pharyngitis in adults: background. Ann Intern Med. 2001;134:509–17. doi: 10.7326/0003-4819-134-6-200103200-00019. [DOI] [PubMed] [Google Scholar]
- 18.Gonzales R, Bartlett JG, Besser RE, Hickner JM, Hoffman JR, Sande MA. Principles of appropriate antibiotic use for treatment of nonspecific upper respiratory tract infections in adults: background. Ann Intern Med. 2001;134:490–4. doi: 10.7326/0003-4819-134-6-200103200-00015. [DOI] [PubMed] [Google Scholar]
- 19.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley and Sons; 1989. [Google Scholar]
- 20.White K, Barrett PH, Jr, Price D, Maselli J, Gonzales R. Changing clinician behavior: characteristics associated with decreasing antibiotic prescribing in ambulatory practice. J Gen Intern Med. 2000;15(suppl):154. [Google Scholar]
- 21.Lewis D. Computer-based approaches to patient education: a review of the literature. J Am Med Inform Assoc. 1999;6:272–82. doi: 10.1136/jamia.1999.0060272. [DOI] [PMC free article] [PubMed] [Google Scholar]