Abstract
OBJECTIVE
This study was initiated by breast cancer survivors living in a rural community in California. They formed a partnership with academic researchers to develop and evaluate a low-cost, community-based Workbook-Journal (WBJ) for improving psychosocial functioning in geographically and economically isolated women with primary breast cancer.
DESIGN
A randomized controlled trial was used to compare the WBJ intervention plus educational materials to educational materials alone (usual care).
SETTING
One rural cancer center and several private medical, surgical, and radiation oncology practices in 7 rural counties in the Sierra Nevada Foothills of California.
PARTICIPANTS
One hundred women with primary breast cancer who were either within 3 months of diagnosis or within 3 months of completing treatment.
INTERVENTION
A community-initiated, theoretically-based Workbook-Journal, designed by rural breast cancer survivors and providers as a support group alternative. It included compelling personal stories, local rural resources, coping strategies, and messages of hope.
RESULTS
Community recruiters enrolled 83% of the women referred to the study. Retention at 3-month follow-up was 98%. There were no main effects for the WBJ. However, 3 significant interactions suggested that women who were treated in rural practices reported decreased fighting spirit and increased emotional venting and posttraumatic stress disorder symptoms if they did not receive the WBJ. Among women who receive the WBJ, 74% felt emotionally supported.
CONCLUSIONS
This community-based Workbook-Journal may be an effective psychosocial intervention for rural, isolated, and low-income women with breast cancer. Community involvement was essential to the success of this project.
Keywords: breast cancer, rural, psychosocial, traumatic stress, recruitment, underserved, coping
Women diagnosed with breast cancer require immediate and continuing educational and emotional support.1 Support groups designed to address these needs have improved knowledge about the disease,2,3 improved coping,4–8 decreased pain,9 reduced psychological distress,2,4,10,11 addressed fears of recurrence,12–15 improved quality of life,6,7,11 and even prolonged life.16 In rural settings, however, distance, education, and cost prohibit many women from participating in support groups. Although many organizations publish educational materials on cancer and treatment, patients must either collect different pamphlets for each question17–25 or wade through textbooks26,27 of information difficult to understand. More importantly, these educational publications do not include one of the most beneficial aspects of support groups: shared personal experiences.28 Rural women with breast cancer need a low-cost psychosocial intervention, appropriate for women with little advanced education, which can be delivered easily over long distances.
Developing interventions for underserved populations, however, is fraught with difficulty. Assessing the needs of underserved patients using traditional assessment instruments and procedures often misses key elements of the problem. Developing an intervention that is accepted, culturally appropriate, and locally endorsed is an enormous challenge. Recruitment and retention of study participants are often so low as to make for questionable generalization of findings. In many cases, the only way to accurately assess and meaningfully address the needs of underserved groups is to include community representatives in the development, assessment, delivery, and evaluation of specifically designed and targeted interventions. We report here on a community–research partnership that successfully developed and scientifically evaluated a psychosocial intervention designed for underserved rural women with breast cancer.
METHODS
Community Participation
The Sierra-Stanford Partnership is a group of rural breast cancer patients, and medical and social work professionals in Nevada City, California, and psychosocial oncology researchers from the Stanford University School of Medicine. This partnership is funded by a Breast Cancer Research Program of the California Community-Initiated Research Collaboration pilot award, a mechanism for supporting the scientific research of community-based ideas in the area of breast cancer.
The community partners included a breast cancer survivor who was the community primary investigator for the project (MAK), an oncology social worker (RM) at the Sierra Nevada Memorial Cancer Center (SNCC) in Grass Valley, California, a home health nurse (PD) who was the leader of the rural breast cancer support group, La Loba, and a graphic artist who lost a parent to cancer (KG). The intervention originated in La Loba during discussions of the limits of psychosocial services for women in rural areas. The community primary investigator envisioned the idea of a Workbook-Journal (WBJ); she wrote the text, with consultation on the content provided by one of the research partners (KLA), and input from the members of La Loba, working closely with the graphic artist.
Community partners took the lead in developing the recruitment procedure, recruiting research participants, conducting assessments, and designing strategies to reduce rural women's fears about participating in a clinical trial. Research partners (KLA, JMT-C, CK) secured funding, oversaw the budget, contributed a theory-based structure to the intervention, identified psychosocial outcomes likely to be affected by the intervention, selected valid and reliable measures, chose the research design, conducted all analyses, and took the lead on papers and presentations.29,30
The Sierra-Stanford Partnership is a foray into a collaboration between community ideas and scientific research. This article highlights our creativity and success at putting science in the hands of the community, along with the barriers and challenges of taking research out of the laboratory.
Participants
Participants were 100 women with biopsy-proven primary breast cancer (stage 0–III, including ductal carcinoma in situ) who were English speaking, over 18 years of age, able to give informed consent, had no other life-threatening illnesses, and were either within 3 months of diagnosis or within 3 months of ending treatment. These 2 periods were chosen because they correspond to times of increased psychosocial distress and need for support.31 Women were recruited from SNCC, rural community-based support groups, and other medical, surgical, and radiation oncology practices in Nevada, Sierra, Amador, Placer, El Dorado, Sutter, and Yuba counties in the Sierra Foothills of California.
Measures
Baseline Demographic and Illness Variables
Demographic variables collected included age, marital status, religious affiliation, family size, ethnic background, education, employment, household income, degree of rural geographic isolation, and access to medical services. Illness variables collected included stage of disease, date of diagnosis, surgical intervention, and chemo-, radiation, and hormonal therapy.
Interview Assessments
Community partners stressed the importance of personal contact in recruitment and assessment, so we developed a semistructured interview that included a needs assessment at baseline32 and a qualitative evaluation of the intervention at follow-up. The baseline interview (∼30–45 min) gave women the opportunity to tell their cancer story and provided the basis for a professional and caring relationship between each woman and her research interviewer. This helped reduce suspicion, improve trust, and streamline participant education regarding clinical trials and randomization. The follow-up interview was designed to improve retention in the trial by soliciting personalized feedback about the intervention from each woman.
Primary Outcome Measures: Posttraumatic Stress Disorder and Mood Disturbance
The primary dependent measures for evaluating the effectiveness of the intervention were the Posttraumatic Stress Checklist-Specific Version (PCL-S) for Diagnostic and Statistical Manual of Mental Disorders, Version IV33,34 to measure posttraumatic stress disorder (PTSD) symptoms, and the Profile of Mood States (POMS)35,36 to measure mood disturbance. The PCL-S yields a total symptom score, with a score >40 indicating clinical levels of PTSD.33 The total mood disturbance score (TMDS), a composite of 6 individual factors,35 was used from the POMS.
Secondary Outcome Measures: Coping
Cancer-specific coping outcomes were assessed on the Mental Adjustment to Cancer (MAC) Scale, short version37 which yields 5 scales: Fighting Spirit, Cognitive Avoidance, Anxious Preoccupation, Fatalism, and Helplessness/Hopelessness.38,39 Three maladaptive coping strategies: emotional venting, behavioral disengagement, and mental disengagement, were assessed on the Coping Operations Preference Enquiry (COPE),40,41 a theoretically derived instrument designed to measure general coping strategies.
The Community-based Intervention: A Workbook-Journal
We developed a community-based, interactive Workbook-Journal entitled, “One in Eight: Women Speaking to Women.” This innovative publication contains disease and treatment-related education, supportive personal experiences from rural women living with breast cancer, facts on the recurrence of breast cancer and validation for related fears, references for national and local community resources, and journal space. Personal stories were compiled by MAK from her interviews with women with breast cancer living in this region. Stories selected for inclusion incorporated key elements of rural life likely to pose the most difficulty (e.g., isolation, coordinating care between physicians), and represented a broad range of positive and negative emotional reactions and coping strategies. Opportunities for journal writing were included throughout the workbook to encourage interactivity and for the emotional release that can come with writing about intense emotional experiences.42,43 The inclusion and organization of chapters in the Workbook-Journal were based on the principles of supportive-expressive group therapy for cancer patients5,44 and the first author's clinical expertise in interviewing and treating women with breast cancer.45–48 These principles include identifying and expressing both positive and negative emotions, personalizing one's own cancer experience, active coping, and soliciting social support.44 Professional graphics and pockets personalized with greeting cards and lavender seeds convey a message of femininity, beauty, and affirmation for life.
Procedure
Recruitment
Patients were recruited for the study in person by 2 experienced, clinically skilled community partners (RM and PD). All patients treated at SNCC who met the eligibility criteria were approached and informed of the study by RM, who routinely visits breast cancer patients to assess their need for services. She explained the study and asked each patient for permission to be contacted by a research interviewer. If a patient was undecided, she asked her permission to check in with her again at a later time. Patients who gave their consent to be contacted were screened, enrolled, and assessed by PD to avoid the possibility of a conflict of interest should RM need to provide services later.
Recruitment at rural private practices was initiated by the community partners (MAK, RM, PD), who gave a presentation to the physicians and staff, outlining the goals of the study, the criteria for enrollment, and a request for referrals. Physicians and staff at all of the practices that were approached agreed to refer patients to the study and to display recruiting materials. RM assessed all participants referred from these practices for whom PD was a treatment provider.
Participant-focused Recruitment Model
Although many of the women approached about the study were interested and eager to participate, most knew nothing about research and were hesitant and suspicious about the possibility of being treated like a “guinea pig.” The way in which our skilled community partners responded to these women was critical to the success of the project. Traditional research defines recruitment procedures to be consistent if each recruiter delivers the same amount of education and information in the same number of contacts to all participants. However, this assumes that each person requires the same amount of information to be informed and learns at the same rate. For this project, we worked closely with our community partners to develop a participant-focused recruitment model. This approach tailors the quality and quantity of recruitment contacts to match the educational and informational needs of each participant. Recruiters educated prospective patients about clinical trials and other research studies, and listened to and validated women's concerns. They gave women time to think about the information, suggesting that they talk it over with family, friends, or physicians before enrolling. Furthermore, they made a point of talking with women who were undecided when they came for treatment. This was a small town, and there were many opportunities for informal professional contacts, which is part of the rural culture. SNCC engaged in public relations activities highlighting their receipt of a research grant to help women with breast cancer and inviting women to “join the partnership” by participating in the trial. In some cases, community partners had up to 4 recruitment contacts with participants before enrolling them in the study.
The community recruiters also received extensive training in research design, issues of bias in recruitment, and human subjects regulations. They were closely supervised via site visits, feedback from taped assessment interviews, and frequent phone consultation. All recruitment and assessment activities were completed before randomizing a participant into her treatment condition. Our approach established recruitment consistency by ensuring that all participants ended up with the amount of education and information they needed, in however many contacts they needed, to make an informed decision about participating and to be able to give true informed consent.
Informed Consent
The project and consent procedures were approved by Stanford University's institutional review board (IRB) ethics committee and SNCC. Community partners reacted strongly to the required legal language about risks, benefits, and liabilities in the informed consent form, fearing that it would heighten rural women's fears about being a “subject” and would be a barrier to participation. To identify ways in which the informed consent process could be adapted to the culture of the community without deviating from the required IRB standards, we asked La Loba for their input. We discovered that changes in format (e.g., font style and size, printing on colored paper), labels, and language (e.g., “participants” rather than “subjects”) reduced this barrier. The community interviewers mailed the informed consent to potential participants before the baseline assessment, encouraging them to read and discuss it with friends and family, and to bring their questions and concerns to the baseline interview. To secure informed consent, the interviewer read through the entire document with each participant, gauging comprehension and offering clarification. All participants were given a copy of the consent form.
Assessments and Randomization
Participants completed all questionnaires at baseline. Women had the option of completing assessments in a private room at their cancer treatment facility, or having the interviewer come to their home. This assessment flexibility was done to accommodate women's treatment schedules, to maximize comfort and a sense of control, and to improve disclosure. The session began with the interviewer asking each woman to tell the story of her breast cancer. Interviewers collected the questionnaires immediately after they were completed, which increased compliance and reduced missing data. We have found this to be an excellent method for establishing rapport with a woman with breast cancer,47,48 forming a relationship with her, and understanding the context in which she joins the study.
Once patients completed all baseline assessments, they were randomly assigned to either the treatment (WkBk; n = 56) or usual care (UC; n = 44) group. The UC group received a packet of 5 breast cancer educational resources,23,49–52 selected by the women of La Loba. The women in the WkBk group received this packet plus the Workbook-Journal. Women were handed their packets after randomization and were told whether they were in the “treatment group” (WkBk) or the “study group” (UC). All women were told that their packets contained materials we believed would be helpful to them in dealing with their breast cancer. Women in the WkBk group were told that their packets contained a new resource, and the WBJ was identified. Women receiving the WBJ were asked not to share it with other patients during the course of the study.
Follow-up Assessments
All women were contacted for one 3-month follow-up, either in person or by phone, by the same interviewer who had conducted her baseline assessment. The interviewers were kept blind to each participant's treatment condition until the final resource evaluation to control for any bias in the outcome assessment. Women completed the same dependent measures they had at baseline, and were then interviewed about their evaluation of the study materials. Women in the WkBk group were asked to evaluate the WBJ separately from the other materials. After completing the follow-up assessment, all women received an end of treatment resource,53 women in the UC group were given the Workbook-Journal, and each participant was paid $25.
To avoid any potential conflicts of interest between study personnel who also were responsible for providing patient care and to reduce potential recruitment bias, no patient was recruited or assessed by someone who could later be a service provider. There are no conflicts of interest between the funding agency and any of the authors.
Data Analysis Procedure
There were no differences between WkBk and UC groups at baseline on demographic, illness, predictor, and outcome variables using t tests for continuous variables or χ2 for categorical variables. We tested 2 a priori hypotheses of the effects of the Workbook-Journal to reduce psychosocial distress (PTSD and mood disturbance), and 8 a priori hypotheses of the effects of this intervention on coping (5 MAC scales, 3 COPE scales) using multiple regression analyses. The multiple regression model for each dependent variable included 4 independent variables: the baseline value on the measure, the treatment condition (WkBk or UC), number of months since diagnosis, and recruitment site (SNCC or other rural practices). Months since diagnosis was included because psychosocial adjustment and coping change as treatment progresses, and recruitment site was included due to the variability in staff and services at different sites. All predictors were centered. We then added 2 interaction terms: treatment condition by months since diagnosis, and treatment condition by recruitment site. All independent variables and interaction terms were entered using the simultaneous entry procedure.
RESULTS
Recruitment and Retention
Between September 1, 1997 and March 31, 1998, 75 women were being treated for breast cancer at SNCC and met study inclusion criteria. Of those, 68 women agreed to participate and were enrolled in the study, a recruitment rate of 90% (Table 1). An additional 45 women were referred from other rural practices and support groups. Of these, 32 women met the criteria and agreed to join the study, a recruitment rate of 71%. Furthermore, we lost only 2 women to follow-up, yielding a retention rate of 98%. One woman dropped out because she moved from the area and the other woman because her breast cancer recurred.
Table 1.
Rates of Recruitment and Retention for Rural Women with Breast Cancer Participating in a Psychosocial Intervention Trial
| Recruitment Site | ||||||||
|---|---|---|---|---|---|---|---|---|
| SNCC* | Rural Practices† | Support Groups | Totals | |||||
| n | % | n | % | n | % | N | % | |
| Eligible patients referred | 75 | 36 | 9 | 120 | ||||
| Patients enrolled | 68 | 90.67 | 23 | 63.89 | 9 | 100 | 100 | 83.33 |
| Patients completing baseline assessments | 68 | 90.67 | 23 | 63.89 | 9 | 100 | 100 | 83.33 |
| Patients completing follow-up assessments | 67 | 89.33 | 22 | 61.11 | 9 | 100 | 98 | 81.67 |
SNCC, Sierra Nevada Memorial Cancer Center.
Rural practices, other rural oncology medical practices.
Demographic and Baseline Comparisons
Detailed demographic and medical characteristics of this sample are reported elsewhere.29 Women in this sample were on average 58.6 years old, predominantly married (66%), and mostly (90%) white. Although 17% of women had no education beyond high school, 31% had a college degree. Nineteen percent earned less than $20,000 per year, but 22% earned more than $60,000. Over 80% reported a religious affiliation. Fifty-two percent had Stage I disease, 46% were treated with mastectomy, 66% received radiation, and 48% underwent chemotherapy. Although 42% lived within 5 miles of a town, the majority (47%) lived farther than 10 miles from their breast cancer treatment provider, with 31% living more than 20 miles from their treatment provider.
Baseline and follow-up means for all outcome variables by treatment group are reported in Table 2. There were no significant baseline differences between women in the WkBk and UC groups on any demographic, medical, rural, or psychosocial variable.
Table 2.
Descriptive Statistics on Outcome Measures for Women Completing Both Baseline and Three-month Follow-up Assessments (N = 98)
| Usual Care Group (N = 43) | Workbook-Journal Group (N = 55) | |||
|---|---|---|---|---|
| Measure | Baseline, n (±SD) | Follow-up, n (±SD) | Baseline, n (±SD) | Follow-up, n (±SD) |
| Primary outcomes | ||||
| Posttraumatic stress checklist (17–85)* | 25.4 (8.7) | 26.6 (10.6) | 28.5 (9.5) | 27.9 (10.1) |
| Profile of mood states (TMDS) (−32–200) | 18.4 (32.8) | 19.4 (37.6) | 24.5 (32.3) | 22.6 (33.2) |
| Secondary outcomes | ||||
| COPE: behavioral disengagement (4–16) | 4.8 (1.2) | 4.8 (1.6) | 5.4 (2.0) | 4.9 (1.4) |
| COPE: mental disengagement (4–16) | 7.4 (2.4) | 7.4 (2.7) | 8.2 (2.5) | 7.6 (2.6) |
| COPE: emotional venting (4–16) | 7.3 (1.8) | 7.6 (2.8) | 8.0 (2.5) | 7.6 (2.3) |
| Mini MAC†: fighting spirit (4–16) | 13.0 (1.7) | 12.3 (1.9) | 12.4 (2.3) | 12.0 (2.3) |
| Mini MAC: anxious preoccupation (8–32) | 17.3 (4.6) | 17.1 (4.3) | 17.9 (5.3) | 16.9 (4.7) |
| Mini MAC: helplessness/hopelessness (8–32) | 10.3 (2.6) | 11.1 (3.8) | 10.3 (2.9) | 10.8 (3.5) |
| Mini MAC: Fatalism (5–20) | 15.1 (2.8) | 15.3 (3.1) | 15.4 (2.7) | 15.3 (2.6) |
| Mini MAC: denial/avoidance (4–16) | 8.8 (2.4) | 8.5 (2.3) | 9.0 (2.5) | 9.3 (2.5) |
Range of possible scores on each measure.
Mini MAC, The Mental Adjustment to Cancer Scale, short version.
Note: no statistically significant difference was found on any of these measures at baseline between the mean scores of participants in the Usual Care group and those in the Workbook-Journal group, using t tests for independent groups.
COPE, Coping Operations Preference Enquiry; TMDS, total mood disturbance score.
Primary Outcomes: Effect of Workbook-Journal on PTSD and TMDS
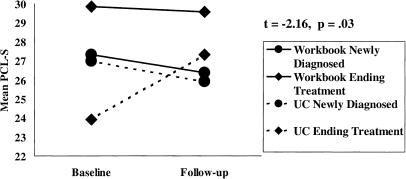
As expected, the baseline PCL-S scores significantly predicted 3-month follow-up PCL-S, resulting in a significant model: F6,90 = 21.19, P = .001. There was no overall main effect for the intervention on PTSD symptoms, but the subgroup of women who were farther out from diagnosis reported higher PTSD symptoms than women who were newly diagnosed (t = 2.86, P = .005). Notably, there was also a significant interaction found between months since diagnosis and intervention: Women who were nearing the end of treatment reported increased PTSD if they were in UC (t = −2.16, P = .03; Fig. 1). There were no between-group differences on the POMS.
FIGURE 1.
Interaction of intervention and months since diagnosis on posttraumatic stress disorder (PTSD). PCL-S, PTSD Checklist-Specific symptoms, where higher scores equal higher PTSD; Workbook, Workbook-Journal group; UC, usual care group.
Secondary Outcomes: Effect of Workbook-Journal on Coping
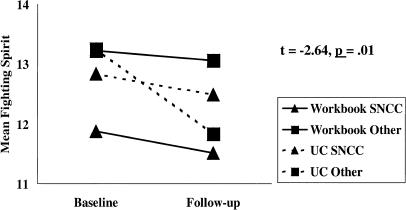
On the MAC, women who were newly diagnosed reported increasing fighting spirit (t = −3.55, P = .001) and decreasing helplessness/hopelessness (t = 2.04, P = .05) compared to women ending treatment (F6.84 = 11.22, P = .001). Women treated at other rural practices showed significantly decreased fighting spirit if they did not received the WBJ, a significant interaction (t = –2.64, P = .01; Fig. 2). There were no significant differences between WkBk and UC groups on any other MAC scales.
FIGURE 2.
Interaction of intervention and treatment site on fighting spirit from the Mental Adjustment to Cancer Scale (MAC). Workbook, Workbook-Journal group; UC, usual care group; SNCC, Sierra Nevada Memorial Cancer Center; Other, other rural practice.
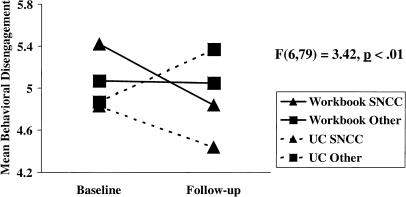
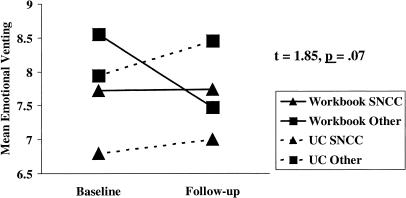
There were no main effects for the intervention on any of the 3 COPE scales. Among women who were newly diagnosed (t = 2.34, P = .02) and who were treated at the SNCC (t = –1.81, P = .07), significantly less behavioral disengagement was reported at follow-up (F6,79 = 3.42, P < .01; Fig. 3), and there was a trend for those recruited in the rural practices to show reductions in emotional venting (t = 1.85, P = .07) if they received the Workbook-Journal (F6,79 = 3.03, P = .01; Fig. 4).
FIGURE 3.
Effect of site on behavioral disengagement from the Coping Operations Preference Enquiry (COPE). A higher value equals higher behavioral disengagement. Workbook, Workbook-Journal group; UC, usual care group; SNCC, Sierra Nevada Memorial Cancer Center; Other, other rural practice.
FIGURE 4.
Interaction of intervention and treatment site on emotional venting from the COPE. A higher value equals higher emotional venting. Workbook, Workbook-Journal group; UC, usual care group; SNCC, Sierra Nevada Memorial Cancer Center; Other, other rural practice.
Women's Evaluations of the Workbook-Journal
Women in the treatment group were asked, “Did the Workbook-Journal change your way of coping with breast cancer?” Forty-four percent (20/45) said that they were better able to cope with breast cancer. However, 53% reported no difference in their coping as a result of the Workbook-Journal. When asked, “How emotionally supported did you feel by the Workbook-Journal?” 74% (32/43) reported feeling more supported by the Workbook-Journal, with only 26% reporting no change in feeling of emotional support.
DISCUSSION
The Sierra-Stanford Partnership is one model of community-based participatory research. Together, we developed and piloted an innovative Workbook-Journal designed to reduce distress and improve coping in rural women with breast cancer. Our participant-focused recruitment model yielded an 83% recruitment rate and 98% retention. There were no main effects for the WBJ on PTSD symptoms, mood disturbance, or coping. However, a significant interaction suggested that women who were ending treatment showed greater benefit in experiencing fewer PTSD symptoms if they received the WBJ. Also, the intervention significantly interacted with treatment site on fighting spirit and emotional venting, indicating that women receiving treatment at more rural practices coped better if they received the WBJ. Over 70% of women in the WkBk group reported feeling more emotionally supported.
Our rate of recruitment and retention in this pilot is unparalleled in medical research, and is even remarkable for psychosocial interventions. We attribute the success of our participant-focused recruitment model to 4 factors: 1) integrating insights and experience from community partners into the model; 2) allowing and budgeting for several interpersonal contacts between recruiters and potential participants; 3) the high skill level of our community recruiters; and 4) the endorsement of the study by the community. This flexible recruitment strategy, involving different numbers of contacts with different participants, offered a way to personalize recruitment to match the education of all participants while maintaining scientific integrity. Safeguards against bias included randomization after assessment and extensive recruiter training.
This study indicated that the Workbook-Journal significantly benefited specific subgroups of rural women. In the case of PTSD symptoms, we saw little change in newly diagnosed women, but women who were farther out from diagnosis benefited from the WBJ. This seems particularly important given that the natural course of PTSD in women with breast cancer worsens over time.54 The WBJ may be an important resource for women who are nearing the end of their treatment for breast cancer, a time for which there are few resources and during which other support diminishes.
In terms of coping, women recruited at SNCC reported little change in fighting spirit or emotional venting. However, women treated at more rural practices who received the WBJ reported less of a decrease in fighting spirit and less of an increase in emotional venting. This suggests that the WBJ may have protected women treated at more rural practices from increases in dysfunctional coping. Our community assessors were compassionate and highly skilled, which may have had the unintended effect of the assessments doing as much psychosocial good as the intervention, particularly for women at SNCC. Although our randomized design would have controlled for any bias in this regard, it highlights the need to carefully train community service providers in the distinction between research assessment and clinical service. This also suggests a strength in cancer centers, even small centers in rural areas, for helping patients cope with and adjust to their illness.
Three important qualifiers should be noted when considering our findings. First, this was a small pilot study with multiple outcomes. These findings, particularly the interactions, need to be confirmed by future studies. Second, although we recruited for this study in a rural area, we cannot assume that all of the women in this region are necessarily isolated or lacking in resources with respect to their breast cancer. Indeed, many of these women reported accessing websites for information and support, and a small number did attend and benefit from rural support groups. Future research could improve upon this study by more carefully detailing the nature of isolation (e.g., geographic, economic, ethnic), and testing the effectiveness of our intervention for different features of isolation.
Third, the 3-month follow-up, which was determined by study time and funding constraints rather than clinical expectation, may have enhanced our recruitment and retention rates and may not have been of sufficient duration to observe the full potential of the intervention. Many women initially report more distress upon beginning a psychosocial intervention as they begin to address their fears and anxieties. A longer follow-up might have shown more distinct differences between WkBk and UC. Our partnership is currently researching these longer-term effects in another sample.
Lessons For Community–Research Partnerships
This pilot was both challenging and rewarding, and we offer several lessons for future collaborations. Experimental control has to be carefully balanced against barriers to participation. This tension can be minimized by including community input in the design of recruitment, consent, and measurement procedures. Multiple recruitment contacts, which may be necessary in samples with low education or familiarity with research, could lead to bias and pressure to enroll. However, community recruiter enthusiasm, combined with education and supervision, can lead to phenomenal recruitment and retention.
Equally important is the need for researchers to be open to novel methods for approaching and assessing participants whose culture and level of trust may be different from those usually studied. It is vital to include underserved and understudied participants in health research; but it requires patience, creativity, and a trusting relationship. Researchers need to consistently demonstrate their respect toward participants and to teach them how to tell us about their experience. Community–research partnerships are a way to build a bridge between community experience and academic knowledge, improving our ability to develop interventions that are more effective for more people.
Acknowledgments
We wish to express our appreciation to the Sierra Nevada Memorial Cancer Center, William A. Newsom, Jr., MD, David Campbell, MD, Steven Wahlen, MD, Ayse Turkseven, Janine Giese-Davis, PhD, David Spiegel, MD, Xin-Hua Chen, the La Loba breast cancer support group, and to all of the women who participated in the study.
This project was supported by a Community-Initiated Research Collaboration (CIRC) award from the Breast Cancer Research Program (BCRP) CIRC Pilot Award #3AB-1301 to Dr. Koopman and Ms. Kreshka.
REFERENCES
- 1.Spiegel D, Lazar SG. The need for psychotherapy in the medically ill. In: Lichtenberg J, Lazar SJ, editors. Psychoanalytic Inquiry. Hillsdale, NJ: The Analytic Press; 1996. [Google Scholar]
- 2.Johnson J. The effects of a patient education course in persons with a chronic illness. Cancer Nurs. 1982;5:117–23. [PubMed] [Google Scholar]
- 3.Felic M, Goldman A, Kennedy BJ. Group counseling in adult patients with advanced cancer. Cancer. 1979;43:760–6. doi: 10.1002/1097-0142(197902)43:2<760::aid-cncr2820430253>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 4.Cain EN, Kohorn EI, Quinlan DM, Latimer K, Schwartz PE. Psychosocial benefits of a cancer support group. Cancer. 1986;57:183–9. doi: 10.1002/1097-0142(19860101)57:1<183::aid-cncr2820570135>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 5.Spiegel D, Bloom JR, Yalom ID. Group support for patients with metastatic cancer: a randomized prospective outcome study. Arch Gen Psychiatry. 1981;38:527–33. doi: 10.1001/archpsyc.1980.01780300039004. [DOI] [PubMed] [Google Scholar]
- 6.Berglund G, Bolund C, Gustafsson U, Sjoden P. Starting again—a comparison study of a group rehabilitation program for cancer patients. Acta Oncol. 1994;32:15–21. doi: 10.3109/02841869309083879. [DOI] [PubMed] [Google Scholar]
- 7.Fawzy FI, Cousins N, Fawzy NW, Kemeny ME, Elashoff R, Morton D. A structured psychiatric intervention for cancer patients. I. changes over time in methods of coping and affective disturbance. Arch Gen Psychiatry. 1990;47:720–5. doi: 10.1001/archpsyc.1990.01810200028004. [DOI] [PubMed] [Google Scholar]
- 8.Heinrich RL, Schag CC. Stress and activity management: group treatment for cancer patients and spouses. J Consult Clin Psychol. 1985;53:439–46. doi: 10.1037//0022-006x.53.4.439. [DOI] [PubMed] [Google Scholar]
- 9.Spiegel D, Bloom JR. Group therapy and hypnosis reduce metastatic breast carcinoma pain. Psychosom Med. 1983;45:333–9. doi: 10.1097/00006842-198308000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Fawzy FI, Fawzy NW, Arndt LA, Pasnau RO. Critical review of psychosocial interventions in cancer care. Arch Gen Psychiatry. 1995;52:100–13. doi: 10.1001/archpsyc.1995.03950140018003. [DOI] [PubMed] [Google Scholar]
- 11.Telch CF, Telch MJ. Group coping skills instruction and supportive group therapy for cancer patients: a comparison of strategies. J Consult Clin Psychol. 1986;54:802–8. doi: 10.1037//0022-006x.54.6.802. [DOI] [PubMed] [Google Scholar]
- 12.Koocher G, O'Malley J. The Damocles Syndrome: Psychosocial Consequences of Surviving Childhood Cancer. New York, NY: McGraw Hill; 1981. [Google Scholar]
- 13.Rieker PP, Edbril SD, Garnik MB. Curative testis cancer therapy: psychosocial sequelae. J Clin Oncol. 1985;3:1117–26. doi: 10.1200/JCO.1985.3.8.1117. [DOI] [PubMed] [Google Scholar]
- 14.Quigley KM. The adult cancer survivor: psychosocial consequences of cure. Semin Oncol Nurs. 1989;5:63–9. doi: 10.1016/0749-2081(89)90024-7. [DOI] [PubMed] [Google Scholar]
- 15.Mahon SM, Cella DF, Donovan MI. Psychosocial adjustment to recurrent cancer. Oncol Nurs Forum. 1990;17(3 suppl):47–54. [PubMed] [Google Scholar]
- 16.Spiegel D, Bloom JR, Kraemer HC, Gottheil E. Effect of psychosocial treatment on survival of patients with metastatic breast cancer. Lancet. 1989;2:888–91. doi: 10.1016/s0140-6736(89)91551-1. [DOI] [PubMed] [Google Scholar]
- 17.American Cancer Society. Helping Children Understand: A Guide for a Parent with Cancer. Atlanta, Ga: American Cancer Society; 1986. [Google Scholar]
- 18.National Cancer Institute. What are Clinical Trials All About? A Booklet for Patients with Cancer. Bethesda, Md: National Institutes of Health; 1996. [Google Scholar]
- 19.National Cancer Institute. Chemotherapy and You: A Guide to Self-help During Treatment. Bethesda, Md: National Institutes of Health; 1995. [Google Scholar]
- 20.National Cancer Institute. Bone Marrow Transplantation and Peripheral Blood Stem Cell Transplantation. Bethesda, Md: National Institutes of Health; 1994. [Google Scholar]
- 21.National Cancer Institute. Radiation Therapy and You: A Guide to Self-help During Treatment. Bethesda, Md: National Institutes of Health; 1993. [Google Scholar]
- 22.National Cancer Institute. Taking Time: Support for People with Cancer and the People Who Care About Them. Bethesda, Md: National Institutes of Health; 1993. [Google Scholar]
- 23.National Cancer Institute. Understanding Breast Changes: A Health Guide for All Women. Bethesda, Md: National Institutes of Health; 1993. [Google Scholar]
- 24.National Cancer Institute. What are Chemoprevention Clinical Trials? A Booklet for People Wanting to Know More About Chemoprevention Clinical Trials. Bethesda, Md: National Institutes of Health; 1992. [Google Scholar]
- 25.National Cancer Institute. When Someone in Your Family has Cancer. Bethesda, Md: National Institutes of Health; 1992. [Google Scholar]
- 26.Love SM. Dr. Susan Love's Breast Book. Menlo Park, Calif: Addison-Wesley Publishing Company; 1995. [Google Scholar]
- 27.Dollinger M, Rosenbaum EH, Cable G. Everyone's Guide to Cancer Therapy: How Cancer is Diagnosed, Treated, and Managed Day to Day. New York, NY: Somerville House Books; 1991. [Google Scholar]
- 28.Spiegel D. Proceedings of the National Conference on Human Values and Cancer: Psychological, Social and Ethical Issues. New York, NY: American Cancer Society; 1981. Group counseling in cancer. [Google Scholar]
- 29.Koopman C, Angell K, Turner-Cobb J, et al. Distress, coping, and social support among rural women recently diagnosed with primary breast cancer. Breast J. 2001;7:1–9. doi: 10.1046/j.1524-4741.2001.007001025.x. [DOI] [PubMed] [Google Scholar]
- 30.Angell KL, Kreshka MA, Turner-Cobb J, Donnelly P, McCoy R, Koopman C. A Workbook-Journal: An innovative psychosocial approach for reaching rural women with breast cancer. Presented at the 106th Annual Convention of the American Psychological Association, San Francisco, Calif, August 14–18, 1998. [Google Scholar]
- 31.Cordova MJ, Andrykowski MA, Kenady DE, McGrath PC, Sloan DA, Redd WH. Frequency and correlates of posttraumatic-stress-disorder-like symptoms after treatment for breast cancer. J Consult Clin Psychol. 1995;63:981–6. doi: 10.1037//0022-006x.63.6.981. [DOI] [PubMed] [Google Scholar]
- 32.Giese-Davis J, Spiegel D. Group Demographics Interview. Stanford, Calif: Department of Psychiatry, Stanford University School of Medicine; 1994. [Google Scholar]
- 33.Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behav Res Ther. 1996;34:669–73. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- 34.Blake D, Weathers F, Nagy L, et al. Clinician-Administered PTSD Scale (CAPS) for the diagnosis of post-traumatic stress disorder in motor vehicle accident victims. Behav Res Ther. 1990;33:471–5. doi: 10.1016/0005-7967(94)00064-q. [DOI] [PubMed] [Google Scholar]
- 35.McNair DM, Lorr M, Droppleman LF. Edits Manual for the Profile of Mood States. San Diego, Calif: Educational and Industrial Testing Service; 1971. [Google Scholar]
- 36.Bloom JR, Ross RD, Burnell G. The effect of social support on patient adjustment after breast cancer. Patient Couns Health Educ. 1978;1:50–9. doi: 10.1016/s0738-3991(78)80002-0. [DOI] [PubMed] [Google Scholar]
- 37.Watson M, Law M, dosSantos M, Grerr S, Baruch J, Bliss J. The Mini-MAC: Further development of the Mental Adjustment to Cancer scale. Psychooncology. in press. [Google Scholar]
- 38.Watson M, Greer S, Bliss J. Mental Adjustment to Cancer (MAC) Scale: Users' Manual. Sutton, Surrey, UK: CRC Psychological Medicine Research Group; 1989. [Google Scholar]
- 39.Schwartz CE, Daltroy LH, Brandt U, Friedman R, Stolbach L. A psychometric analysis of the Mental Adjustment to Cancer Scale. Psychol Med. 1992;22:203–10. doi: 10.1017/s0033291700032864. [DOI] [PubMed] [Google Scholar]
- 40.Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56:267–83. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 41.Carver CS, Pozo C, Harris SD, et al. How coping mediates the effect of optimism on distress: a study of women with early stage breast cancer. J Pers Soc Psychol. 1993;65:375–90. doi: 10.1037//0022-3514.65.2.375. [DOI] [PubMed] [Google Scholar]
- 42.Smyth JM. Written emotional expression: effect sizes, outcome types, and moderating variables. J Consult Clin Psychol. 1998;66:174–84. doi: 10.1037//0022-006x.66.1.174. [DOI] [PubMed] [Google Scholar]
- 43.Smyth JM, Stone AA, Hurewitz A, Kaell A. Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. JAMA. 1999;281:1304–9. doi: 10.1001/jama.281.14.1304. [DOI] [PubMed] [Google Scholar]
- 44.Classen C, Diamond S, Solomon A, Fobair P, Spira J, Spiegel D. Brief Supportive-Expressive Group Therapy for Women with Primary Breast Cancer: A Treatment Manual. Psychosocial Treatment Laboratory, Breast Cancer Intervention Project. Stanford, Calif: Stanford University School of Medicine, Department of Psychiatry and Behavioral Sciences; 1993. [Google Scholar]
- 45.Classen C, Abramson S, Angell K, et al. Effectiveness of a training program for enhancing therapists' understanding of the supportive-expressive treatment model for breast cancer groups. J Psychother Pract Res. 1997;6:211–8. [PMC free article] [PubMed] [Google Scholar]
- 46.Koopman C, Hermanson K, Diamond S, Angell KL, Spiegel DS. Social support, life stress, pain and emotional adjustment to advanced breast cancer. Psychooncology. 1998;7:101–11. doi: 10.1002/(SICI)1099-1611(199803/04)7:2<101::AID-PON299>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 47.Angell KL. Chronic life stressors and negative social support predict delay in treatment for breast cancer. Poster presented at the 21st annual meeting of the Society of Behavioral Medicine, Nashville, Tenn, April 6, 2000. [Google Scholar]
- 48.Angell KL. Women's social environments predict delay in seeking treatment for breast cancer. Invited paper presented as part of a symposium at the 5th World Congress of Psycho-Oncology, Melbourne, Victoria, Australia, September 4, 2000. [Google Scholar]
- 49.American Cancer Society. Breast Self-exam. Atlanta, Ga: American Cancer Society; 1995. [Google Scholar]
- 50.American Cancer Society. Eating Smart: Tips for Patients with Cancer. Atlanta, Ga: American Cancer Society; 1995. [Google Scholar]
- 51.American Cancer Society. Cooking Smart: Tips for Patients with Cancer. Atlanta, Ga: American Cancer Society; 1995. [Google Scholar]
- 52.National Cancer Institute. The Immune System and How It Works. Bethesda, Md: National Institutes of Health; 1996. [Google Scholar]
- 53.National Cancer Institute. Facing Forward: A Guide for Cancer Survivors. Bethesda, Md: National Institutes of Health; 1994. [Google Scholar]
- 54.Classen C, Butler LD, Koopman C, et al. Supportive-expressive group therapy and distress in patients with metastatic breast cancer. Arch Gen Psychiatry. 2001;58:494–501. doi: 10.1001/archpsyc.58.5.494. [DOI] [PubMed] [Google Scholar]