Abstract
OBJECTIVE
Residents of East Harlem, an impoverished, non-white community in New York city (NYC), have up to 5 times the mortality and complication rates of diabetes compared with NYC residents overall. To determine potentially remediable problems underlying this condition, a community-based collaboration of health providers, community advocates, and researchers, surveyed East Harlem residents with diabetes to assess their knowledge, behaviors, barriers to care, and actions taken in response to barriers.
DESIGN
Telephone interviews.
SETTING
The 3 hospitals and 2 community clinics serving East Harlem.
PARTICIPANTS
Nine hundred thirty-nine of the 1,423 persons (66%) with diabetes identified from these 5 healthcare sites with 2 or more ambulatory visits for diabetes during 1998 who lived in East Harlem.
RESULTS
While most respondents (90%) said they know how to take their medicines, between 19% and 39% do not understand other aspects of their diabetes management. Many limit their diabetes care due to concerns about money (16% to 40%), and other barriers, such as language and transportation (19% to 22%). In multivariate analyses, Latinos (relative risk [RR] = 0.77; 95% confidence interval [95% CI] 0.63 to 0.91) and those who do not keep a diabetic diet due to concerns about money (RR = 0.85; 95% CI 0.70 to 0.99) had poorer health status.
CONCLUSIONS
A community-based coalition was able to come together, identify areas of concern in diabetes care and assess the needs of adults with diabetes residing and obtaining care in East Harlem. The coalition found that even among those with access to care there remain significant financial barriers to good diabetes care, and a need to address and optimize how individuals with diabetes manage their disease.
Keywords: community, diabetes, African American, Latino, barriers
An estimated 16 million adults in the United States have diabetes, one third of whom are undiagnosed. When compared to non-Latino white adults, the rates of diabetes are 1.6 times greater in non-Latino blacks, and 1.9 times greater in Mexican Americans. Among adults aged 40 to 74, 26% of Puerto Ricans, 24% of Mexican Americans and 19% of African Americans have diabetes, compared to 12% to 13% of whites.1–3 Mexican Americans and African Americans with diabetes have worse glycemic control after adjusting for treatment status.4 Complications of diabetes such as renal disease and blindness are 2 to 4 times higher in African Americans and Latinos. African Americans with diabetes have 2 times the amputation rate, and associated mortality from amputations is twice as high as for white persons. Diabetes-specific mortality rates for African American and Latinos are higher than for whites.5
The toll diabetes takes on residents of communities of color, such as East Harlem in New York city (NYC) is staggering. East Harlem, also known as Spanish Harlem or El Barrio, is situated on the northeast corner of Manhattan. Its 125,000 residents are 50% Latino (predominantly Puerto Rican), 40% black, 6% white and 4% other races.6 East Harlem typifies many predominantly minority communities across the United States, in that its residents struggle with limited resources while bearing a disproportionate burden of chronic diseases, such as diabetes. With one third of its residents living below the poverty level, East Harlem has one of the highest proportions of households in poverty in NYC. Though East Harlem houses 5 major sites for health care (1 municipal hospital, 1 community hospital, 1 tertiary-care academic medical center, and 2 community health centers), residents have the highest rate of preventable admissions for ambulatory care sensitive conditions and the highest all-cause death rates in all of NYC.7 Mortality and hospitalization rates for persons with diabetes in East Harlem are nearly double those for residents of NYC.7 Hospitalizations among persons 65 years and older for diabetes-related amputations in this neighborhood are nearly 5 times those for NYC overall.8
The East Harlem Diabetes Center of Excellence emerged from a partnership between the East Harlem Community Health Committee (a local provider and consumer group), and Island Peer Review Organization (one of the largest quality improvement organizations in the United States), who were conducting a study of diabetes care at local provider sites. In 1997, they brought together a diverse group of health providers (physicians, nurses, nutritionists, health educators, and outreach workers) from the 5 major sites of care located in the neighborhood, as well as community members and leaders, and health policy and health services researchers. The coalition's efforts initially focused on assessing the quality of ambulatory diabetes care. The first project was a chart abstraction of nearly 700 records. That project's findings showed variability in quality performance with a need to improve delivery of basic services such as foot and eye exams.
The group next tried to develop strategies to improve clinical performance across all sites. However, group members found it difficult to develop shared quality improvement initiatives, in part because group members came from different settings and had different priorities. At this juncture, the coalition's leader proposed a patient survey that focused on patient satisfaction with clinical encounters. This suggestion appeared to raise the level of mistrust in the coalition, because some members did not see the relevance of the proposed questions and were uncertain about how the data would be used. In fact, some stated they would refuse to participate in the survey.
In response to members' growing disinterest in, and dissatisfaction with current coalition activities, and lack of group cohesion, coalition leaders asked members to articulate their vision for the Center of Excellence. Most members expressed their interest in shifting the focus of the coalition away from provider sites and toward the East Harlem community. The members wished to work with East Harlem residents with diabetes to improve their self-management practices and their health. To operationalize this change in focus, members formed community outreach and research subcommittees who reported their activities back to the coalition at general monthly meetings.
The coalition first worked to increase community awareness of diabetes. A local artist designed a logo of a woman with diabetes, which highlighted important diabetes-healthy behaviors (Fig. 1). He conducted a “sidewalk art campaign,” chalking the logo on sidewalks throughout East Harlem to trigger discussions about diabetes among neighborhood residents. He also drew advertisements for coalition-sponsored events, such as salsa dances and church events that included diabetes screenings, lectures, local entertainment, serving of healthy local foods and raffles. Over time, these well-attended activities strengthened links between clinicians at different sites and between sites of clinical care and community-based organizations. Clinicians in the coalition became less concerned that their patients would be redirected to the local tertiary care hospital (where coalition leaders were employed), and more interested in ways to reach out to, and learn from their patients.
FIGURE 1.
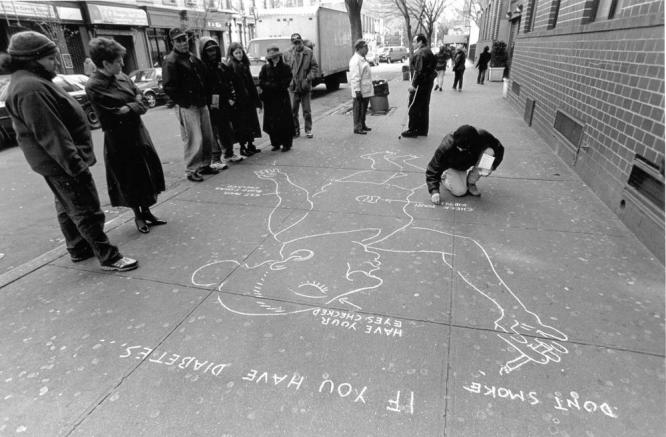
Sidewalk art campaign in East Harlem.
With a renewed group identity and purpose, the coalition moved to address our next goal of identifying East Harlem residents' barriers to good diabetes care. As part of this effort, the group decided that a patient survey would be important. This time, however, we chose to focus the survey on what East Harlem residents understood about diabetes, did to control their diabetes, and the barriers residents faced to obtain high quality diabetes care. The coalition planned to use results of the survey to target areas for further research and community-based interventions.
METHODS
The coalition's research subcommittee led the effort to outline survey domains the coalition was interested in, and review existing scales to assess these domains. In particular, the group was interested in East Harlem residents' understanding and practice of diabetes recommended diet, exercise and other self-management strategies, as well as barriers to controlling diabetes. The group chose to measure knowledge, behaviors and health outcomes related to diabetes using scales from the Diabetes Quality Improvement Program patient survey, which included items about diet, exercise, blood sugar monitoring, and medication adjustments.9,10 We added newly constructed items to measure the perceived effects of poverty on adhering to recommended diabetes therapies. Respondents were asked, “Over the past year, how often have you done any of the following because of concerns about money?” They responded to 6 items: taking less medicine, skipping doses of medicine, skipping blood sugar checks, skipping meals, not keeping a diabetic diet, and not seeing a doctor or nurse for diabetes.
The researchers partnered with key personnel at all sites to obtain Institutional Review Board approval for a telephone survey, and to use each site's administrative database to identify patients. We identified 2,595 adult patients who had 2 or more ambulatory care visits at one of the 5 sites with an associated ICD-9 (International Classification of Diseases-9) code for diabetes (ICD-9 250.xx) during calendar year 1998. Of these, 1,521 patients had a valid telephone number listed and lived in East Harlem. Leaders from clinical sites sent personalized letters to patients, found alternate phone numbers for patients who initially could not be contacted, and encouraged providers to champion the survey to their patients. Community representatives also informed their constituents that they supported this survey. With these efforts, 1,037 patients consented to be surveyed. An additional 311 patients refused to participate, and 173 did not respond after 8 attempts, did not speak English or Spanish, or had disconnected telephones. Omitting the 98 respondents who stated they did not have diabetes, we were left with a final sample of 939 patients of 1,423 eligible patients (66% response rate). The survey was approximately 20 minutes in length. Patients were not paid for their participation, but did receive an educational booklet. We used χ2 tests to compare categorical data and logistic regression for multivariate assessments. Using a formula reported by Zhang and Yu, we corrected adjusted odds ratios from the models to estimate relative risks.11
RESULTS
Overall, this population reflects the East Harlem community. The patients are mostly Latino and African American (93%), and their median age is 61 years (range 18 to 75). Most are poor; 77% have an income of under $20,000 per year, 62% did not graduate high school, and 35% chose to respond to the survey in Spanish. Seven percent are uninsured. Most are ill; the majority report signs of peripheral neuropathy (54%), fair or poor health status (56%) and many say their diabetes is not well-controlled (45%). They have had diabetes for a median of 9 years (range 1 to 60; Table 1).
Table 1.
Baseline Demographics and Clinical Characteristics
| Characteristic | n/N | % |
|---|---|---|
| Women | 689/897 | 77 |
| Household income <$20,000 | 402/897 | 77 |
| Education <high school | 578/897 | 62 |
| Ethnicity | ||
| Latino | 514/897 | 57 |
| African American | 320/897 | 36 |
| Insurance | ||
| Any Medicaid | 618/882 | 71 |
| Uninsured | 62/882 | 7 |
| Cigarette smoker | 202/913 | 22 |
| Takes pills and/or insulin | 860/922 | 93 |
| Self-reported clinical status | ||
| Fair/poor health status | 504/898 | 56 |
| Diabetes not well controlled | 392/879 | 45 |
| Diabetes markedly limits usual activities | 160/876 | 18 |
| Has peripheral neuropathy | 503/923 | 54 |
Denominators vary due to missing responses; not all patients completed all the survey questions.
Numerous respondents report that financial barriers affect their ability to receive diabetes care (Table 2). Less than 30% of patients have insurance that pays all prescription costs, and between 16% and 23% do not see their provider, take less medication than prescribed, skip taking medicines, and skip checking their sugars due to money concerns. Furthermore, due to money constraints, 28% skip meals, and 40% do not keep a diabetic diet (Table 2). Between 19 and 22% state that language barriers, transportation problems and medication costs prevent them from getting the best diabetes care. Compared with Latinos, African Americans are more likely to report skipping meals (33% vs 25%; P < .05), skipping checking their blood sugar (27% vs 21%; P < .05), and skipping taking medications (25% vs 16%; P < .01) due to concerns about money. Multivariate models controlling for patient demographics, health status and insurance revealed that African Americans were more likely than Latinos to skip taking medicines due to monetary concerns (relative risk [RR] = 0.6; 95% confidence interval [95% CI], 0.4 to 0.9). African Americans and Latinos did not differ in other strategies to adapt to financial constraints. Latinos were more likely to have difficulty finding a provider who speaks their language (RR = 4.0; 95% CI, 2.0 to 7.0).
Table 2.
Barriers and Strategies to Adapt
| Barriers | n/N | % |
|---|---|---|
| No insurance that pays all prescription costs | 633/897 | 71 |
| Did not see health care provider due to money concerns | 144/898 | 16 |
| Took less medicine than prescribed due to money concerns | 145/900 | 16 |
| Skipped taking medicine due to money concerns | 183/899 | 20 |
| Skipped checking blood sugar due to money concerns | 210/899 | 23 |
| Skipped meals due to money concerns | 251/899 | 28 |
| Did not keep diabetic diet due to money concerns | 357/899 | 40 |
| Language prevented getting the best diabetes care | 174/902 | 19 |
| Transportation prevented getting the best diabetes care | 196/905 | 22 |
| Medication costs prevented getting the best diabetes care | 188/905 | 21 |
Approximately one fourth of patients did not understand well the basics of diabetes care including what a target blood sugar level should be, how much they should eat and drink, and how to exercise. Even fewer knew how to shop for and prepare a diabetic diet (Table 3). Although 90% report knowing how to take their medications and 71% check their blood sugar more frequently than once a week, there was little associated change in self-management strategies. Only 41% change their diet or exercise regimen, and only 21% of insulin users change their medication dose in response to this information. There were no significant differences in knowledge between African Americans and Latinos. Multivariate analyses revealed that patients with more education, better health status, those with insurance, and patients who had seen a nutritionist were more knowledgeable about diabetes-healthy behaviors (data not shown).
Table 3.
Patients' Diabetes Knowledge and Behaviors
| Knowledge | n/N | % |
|---|---|---|
| Did not understand well | ||
| Diabetes complications | 215/923 | 24 |
| How to take medications | 99/923 | 10 |
| How to control blood sugar levels | 172/925 | 19 |
| How much to eat and drink | 225/929 | 25 |
| How to shop and cook for diabetic diet | 349/902 | 39 |
| What target blood sugar should be | 241/923 | 26 |
| How to control weight | 247/926 | 19 |
| Importance of exercise | 211/932 | 23 |
| Diabetes-related utilization | ||
| ER/urgent care visit in past year for diabetes | 216/910 | 24 |
| Nutritionist visit in past year | 429/911 | 47 |
| Eye exam in past year | 700/915 | 77 |
| Foot exam in past year | 736/910 | 81 |
| Diabetes-related self-management behaviors | ||
| Checks blood sugar <1×/week | 270/922 | 29 |
| Rarely/never changes diet or exercise based on blood sugar | 426/726 | 59 |
| Walked <30 min in past week | 171/922 | 19 |
| Examines feet less than daily | 415/922 | 29 |
| Rarely/never changes diabetes medicine dose based on blood sugar | 610/727 | 84 |
| Rarely/never changes insulin dose based on blood sugar | 250/318 | 79 |
The large percentage of patients experiencing dietary barriers was consistent with community leaders' expectations and experiences. Therefore, the coalition chose to look more closely at whether potentially remediable dietary factors and behaviors were related to patients' poor health by assessing the association between health status and dietary barriers and exercise in a multivariate model. We found that individuals who did not keep a diabetic diet as well as women and Latinos were more likely to have poorer health status (Table 4). Those who knew how to control or lose weight and who had exercised in the past week had better health status.
Table 4.
Factors Related to Fair or Poor Health Status Among East Harlem Residents with Diabetes
| Characteristics | RR | 95% CI for RR |
|---|---|---|
| Did not keep diabetic diet due to money concerns | 0.85 | 0.70 to 0.99 |
| Knows the importance of exercise | 1.07 | 0.94 to 1.18 |
| Knows how to lose or control weight | 1.13 | 1.0 to 1.23 |
| Exercised at least 30 min in the past week | 1.14 | 1.02 to 1.23 |
| Age ≥65 y | 1.09 | 0.96 to 1.2 |
| Female | 0.79 | 0.64 to 0.96 |
| Uninsured | 1.08 | 0.83 to 1.29 |
| Latino | 0.77 | 0.63 to 0.91 |
RR indicates estimated relative risk; CI indicates confidence intervals; Health status coded with fair–poor health status as 0 and good–excellent health status as 1. Logistic model c = 0.64; P < .0001.
The community participants in this study had documented access to care; most were insured, and to be included, they required 2 ambulatory visits for diabetes in a single year. Despite having access to primary care, nearly one fourth of these patients reported diabetes-related visits to emergency or urgent care sites, with African Americans more likely than Latinos in this regard (28% vs 18%, P = .02). Self-reported utilization rates did not differ by age, gender, or insurance status.
DISCUSSION
Recognizing the undue burden of suffering experienced by East Harlem residents with diabetes, a community-centered diabetes coalition consisting of neighborhood providers, community representatives and health services researchers came together to address the underlying problems that contribute to patients' poor outcomes. Through letting the group set its own agenda, a mixture of outreach workers, community leaders, and competing clinicians transformed into an enthusiastic partnership utilizing strengths of coalition members and community resources to focus attention on diabetes and assess patient-centered barriers to care.
We found that persons with diabetes who live in and receive care in East Harlem understand some of what is required to take care of their diabetes, yet they experience important difficulties in their ability to optimize their care. While most patients check their blood sugar at least once a week, few change their diets, medication doses or exercise patterns in response. Perhaps this inaction is related to the large percentage of patients who do not know what a target blood sugar should be, or to a lack of adequate patient education in this area. Many face financial and language barriers. Latinos were more likely to have poor health status, and not surprisingly, had more difficulty finding providers who spoke their language. Limited English proficiency and higher out of pocket costs can reduce patients' ability to obtain appropriate diabetes care, and to self-monitor and manage their diabetes.10,12 Such barriers are common in poor and minority communities and pose great challenges to those trying to improve their diabetes care.13,14
Health-related quality of life in African Americans with diabetes has been associated with barriers to care, including problems with money, housing, crime, family, and caretaker responsibilities.15 In our sample of urban African Americans and Latinos with diabetes, we found poor health-related quality of life was associated with economic barriers relating to keeping a diabetic diet. The Third National Health and Nutrition Examination Survey found 6% of respondents overall and 17% living below the poverty level, report food insufficiency.16 They found no association between food insufficiency and poorer health status. In our sample, 28% of respondents skipped meals due to money concerns, and this practice was associated with poorer health status.
During meetings devoted to reviewing the survey findings, coalition members were struck by the seeming disconnect between patients' knowledge of a healthy diet and their practice, as well as by the prevalence of dietary barriers and their relationship to poor health status. At academic-community forums to discuss diabetes, participants indicated that the East Harlem community does not have adequate information about nutritionally appropriate, affordable, ethnically familiar foods for people with diabetes. They further asserted that recommended foods for persons with diabetes are not readily available at local markets. Yet, coalition members were not certain whether the survey findings about diet reflected problems with the supply of diabetes recommended foods or the patient demand for these foods. Therefore, coalition members wrote for and obtained a second grant to assess factors that influence both the supply of appropriate foods and patients' abilities to adhere to a healthy diet. To explore the supply side, we proposed to assess the availability of food items in East Harlem compared to an adjacent, predominantly white, affluent neighborhood. We also organized a local nutrition consortium where food vendors and distributors, residents, clinicians, advocates and food providers (such as senior center and food pantry staff) could discuss the nutritional environment in the community. To explore patients' points of view about nutrition and a diabetic diet, or the demand side, we conducted focus groups to get a detailed understanding of diabetic residents' views on food and nutrition. Utilizing focus group findings, we are developing and planning to implement a diabetes peer nutrition education program.
Community-based research is a collaborative process in which community and organizational representatives as well as researchers actively partner to contribute their expertise to enhance understanding of a phenomenon. Such research integrates the knowledge gained with action to benefit the community.17 Our coalition began as a partnership around a specific topic: assessing the quality of ambulatory diabetes care. Over time, we shifted away from a clinical focus, and went beyond the statistics that portray East Harlem as the poorest neighborhood, with some of the worst health outcomes in NYC. Instead, we formed relationships with members of grass-roots organizations in East Harlem that helped build the foundation for our approaches to assess diabetes care and improve diabetes-related outcomes.
Our efforts to use a community-based research approach generated several important lessons. First, allowing coalition partners to set the agenda to focus on the community transformed leaders of health centers that compete for patients into collaborators who joined forces to evaluate and improve diabetes care in East Harlem. Moreover, partnering with community members and leaders proved to be essential in bringing a “real life” perspective to data analysis and planning sensible projects. Bringing these disparate groups together allowed all members to broaden their ability to serve the community. Physicians joined the coalition with an interest in addressing processes of care. Many had never before participated in community events, or had the opportunity to work in partnership with community experts. As a result of relationships they formed in the coalition, clinicians volunteered to give lectures and provide some services at a local organization, and began to plan diabetes outreach activities at their own institutions. Through these new endeavors, many physicians began to see patients as people living in a vibrant community struggling to maintain their health with limited individual and community resources.
Second, this experience began to build an infrastructure devoted to improving diabetes care in East Harlem. Community activists obtained an understanding and some ownership for a survey that produced revealing data and helped bring grant money to their neighborhood. Outreach workers learned basics about diabetes. Health center staff learned how to collect and utilize data to improve services offered to their patients. Many members disseminated the lessons we learned to local politicians, religious, business and hospital leaders. With a more complex and sophisticated understanding of the challenges and opportunities for improving chronic disease care, and utilizing each others' strengths, we aim to work with these leaders to effect meaningful changes in the health of the community that last beyond episodic infusions of grant funding.
Direct input from members of disadvantaged communities often has not been included in academic and public health efforts to improve their health.18 Interventions created solely by outsiders may perpetuate the inequalities well-meaning project staff aim to address, create an atmosphere that discourages community experts from sharing invaluable perspectives and ideas, and thwart entry of researchers and projects into communities.19 Our diabetes coalition has an ethnically and professionally diverse representation of the community that co-developed all research tools and intervention ideas, organized local events and championed the mission and activities of the coalition throughout the community. Developing and promoting educational brochures, community events and this survey strengthened the sense of group identity and ownership, and provided a compelling mechanism for community outreach. As a result, coalition partners gained a greater appreciation for using rigorously collected local data as the foundation for defining and addressing problems, and obtaining funding for new initiatives. Community activists and local health workers helped recruit patients for their own survey, and used the resulting data to develop educational materials to improve their patients' or stakeholders' self-management.
Finally, these efforts may have helped begin to address mistrust East Harlem community members have of research and researchers. Members of minority populations may have a “healthy paranoia” of researchers and outside organizations, given a history of racism, marginalization of minority communities by health care systems, and past experiences having researchers enter their community, collect data, provide no direct benefits, and leave without giving feedback or taking noticeable actions.20,21 The local sense of ownership we aimed to achieve and maintain may help our coalition avoid this fate.
Researchers unfamiliar with community-based research should be aware that this process has several challenges. Coalition members need to build trusting relationships over time. Partners are likely to have different perspectives on the relative importance of processes versus outcomes, research versus service and the need for rigorous evaluation. They also may have different styles of communication and decision making, and different opinions about how a community is defined and who may legitimately represent that community.22 We established common goals and ground rules that promote understanding, communication, and respect, to help the coalition thrive despite these tensions.23 Maintaining momentum of a diverse coalition is critical, but challenging.24 Ensuring the success of the diabetes-related community events required major commitments of time and labor from the coalition's steering committee members and dozens of volunteers. From a researcher's standpoint, these may not be viewed as important components of interventions that can be rigorously evaluated. However, the consensus among coalition members is that the events generated significant interest and enthusiasm among people with or at risk for diabetes in East Harlem, strengthened working relationships within the coalition, gave the coalition credibility and staying power, and attracted new ideas and new coalition members.
We surveyed the majority of East Harlem residents with known diabetes who receive care in the community; there are only a few small private physician offices that care for adult patients in East Harlem whose patients we did not attempt to contact. We did not survey East Harlem residents with diabetes who receive their care outside East Harlem, or those who did not visit one of the partner sites for diabetes at least twice in 1998. Given these limitations and a modest response rate, our findings may not reflect the entire East Harlem adult population with diabetes. While these data capture patients' knowledge, behaviors, and self-reported barriers, without links to utilization or clinical data, we cannot assess how these self-reports correlate with the rates of diabetes control or objective measures of diabetes complications. We found associations between health status, dietary barriers, and healthy behaviors, but we cannot attribute causation in these cross-sectional data.
Galvanized by the poor health outcomes of diabetic patients living in East Harlem, our coalition came together to identify and address problem areas experienced by persons with diabetes who reside in East Harlem. The survey reported here is one of numerous coalition-led projects addressing diabetes in our neighborhood. Finding that few East Harlem residents with diabetes know how to shop, cook, and manage their diabetes care has led to the coalition's next projects to assess and address barriers to eating a healthy diet. The coalition has built effective relationships grounded in trust and mutual respect. These were fostered as coalition members, volunteers, students, and civic and religious leaders joined forces to plan culturally appropriate and engaging events, and to develop materials and research tools relevant to the community. These multidisciplinary partnerships may help as we move from documenting the presence of sociocultural disparities and barriers in health care toward developing sustainable strategies to eliminate disparities and improve care.
Acknowledgments
We would like to thank all coalition partners for their enthusiastic partnership, specifically: Margaret Davis and Ann Gel Palermo (Institute for Medicare Practice); Ray Cornbill (East Harlem Community Health Committee and Mount Sinai Medical Center); Kathryn Colson, Stacey Silberzweig, Jane Shin and Andrea Zaldivar (Mount Sinai Medical Center); Susan Hollander and Alan Silver (IPRO); Eric Canales (Center for Urban Epidemiologic Studies); Simon Nzuzi (NY College of Podiatric Medicine); Ronald Cobbs (Metropolitan Hospital); Matthew Weeks (Settlement Health); Erica Estades (East Harlem Council for Human Services); John Figueroa (Institute for Puerto Rican and Hispanic Elderly); Margaret Davis (American Diabetes Association); Father Frances Skelly (St. Cecelia's Church); James DeLa Vega (DeLaVega Studio); and Louise Square (NY State Department of Health) for sharing their ideas and for reviewing portions, or all of this manuscript. We also would like to thank Ann Ruecker for assisting with the data analysis.
This study was funded by the New York State Department of Health, Grant C014647.
REFERENCES
- 1.Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in US adults. Diabetes Care. 1998;24:518–24. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Ezzati TM, Harris MI, et al. Prevalence of diabetes in Mexican Americans, Cubans and Puerto Ricans for the Hispanic Health and Nutrition Examination Survey, 1982–1984. Diabetes Care. 1991;14:628–38. doi: 10.2337/diacare.14.7.628. [DOI] [PubMed] [Google Scholar]
- 3.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195–200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 4.Weatherspoon LJ, Kumanyika SK, Ludlow R, Schatz D. Glycemic control in a sample of black and white clinic patients with NIDDM. Diabetes Care. 1994;17:1148–53. doi: 10.2337/diacare.17.10.1148. [DOI] [PubMed] [Google Scholar]
- 5.Carter JS, Pugh JA, Monterrosa A. Non-insulin-dependent diabetes mellitus in minorities in the United States. Ann Intern Med. 1996;125:221–32. doi: 10.7326/0003-4819-125-3-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 6.U.S. Census Bureau. Census 2000 Summary File 1 Census of Population and Housing. Washington, DC. September 2000.
- 7.Krasner MI, Heisler TE, Brooks P. New York City Community Health Atlas, 1994. New York, NY: United Hospital Fund; 1994. [Google Scholar]
- 8.The Turning Point Community Health Forum. Community Health Profile: Manhattan. New York, NY: New York City Department of Health; 2000. [Google Scholar]
- 9.Fleming BB, Greenfield S, Engelau MM, Pogach LM, Clauser SB, Parrott MA for the DQUIP Group. The diabetes quality improvement project: moving science into health policy to gain an edge on the diabetes epidemic. Diabetes Care. 2001;24:1815–20. doi: 10.2337/diacare.24.10.1815. [DOI] [PubMed] [Google Scholar]
- 10.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Venkat Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136:565–74. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 11.Zhang Jun Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 12.Karter AJ, Ferrara A, Darbinian JA, Acerson LM, Selfy JV. Self-monitoring of blood glucose. Language and financial barriers in a managed care population with diabetes. Diabetes Care. 2000;23:477–83. doi: 10.2337/diacare.23.4.477. [DOI] [PubMed] [Google Scholar]
- 13.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans. Diabetes Care. 2002;25:259–68. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hiss RG, Anderson RM, Hess GE, Stepien CJ, Davis WK. Community diabetes care: a 10-year perspective. Diabetes Care. 1994;17:1124–34. doi: 10.2337/diacare.17.10.1124. [DOI] [PubMed] [Google Scholar]
- 15.Hill-Briggs F, Gary TL, Hill MN, Bone LR, Brancati FL. Health-related quality of life in urban African Americans with type 2 diabetes. J Gen Intern Med. 2002;17:412–9. doi: 10.1046/j.1525-1497.2002.11002.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson K, Cunningham W, Andersen R, Harrison G, Gelberg L. Is food insufficiency associated with health status and health care utilization among adults with diabetes? J Gen Intern Med. 2001;16:404–11. doi: 10.1046/j.1525-1497.2001.016006404.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 18.Oakley P. Community Involvement in Health Development: An Examination of the Critical Issues. Geneva: World Health Organization; 1989. [Google Scholar]
- 19.Lefevre CR, Flora JA. Social marketing and public health interventions. Health Educ Q. 1988;15:219–315. doi: 10.1177/109019818801500305. [DOI] [PubMed] [Google Scholar]
- 20.Grace CA. Practical considerations for program professionals and evaluators working with African-American communities. In: Orlandi MA, editor. OSAP Cultural Competence Series 1. Washington DC: U.S. Department of Health and Human Services; 1992. pp. 55–74. [Google Scholar]
- 21.Casas JM, Thompson C. A racial/ethnic minority research perspective. Couns Values. 1991;35:186–95. [Google Scholar]
- 22.Mac Queen KM, Mc Lellan E, Metzger DS, et al. What is community? An evidence-based definition for participatory public health. Am J Public Health. 2001;91:1929–38. doi: 10.2105/ajph.91.12.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Butterfoss FD, Goodman RM, Wandersman A. Community coalitions for prevention and health promotion. Health Educ Res. 1993;8:315–30. doi: 10.1093/her/8.3.315. [DOI] [PubMed] [Google Scholar]
- 24.Horowitz CR, Davis MH, Palermo AS, Vladeck BC. Approaches to eliminating sociocultural disparities in health. Health Care Financ Rev. 2000;21:57–74. [PMC free article] [PubMed] [Google Scholar]


