Abstract
OBJECTIVE
To determine the impact of interpretation method on outpatient visit length.
DESIGN
Time–motion study.
SETTING
Hospital-based outpatient teaching clinic.
PARTICIPANTS
Patients presenting for scheduled outpatient visits.
MEASUREMENTS AND MAIN RESULTS
Over a 6-week study period, a research assistant recorded the following information for consecutive patient visits: patient age, gender and insurance type; type of interpreter used (none, hospital interpreter, telephone interpreter or patient-supplied interpreter); scheduled visit length; provider type (nurse practitioner; attending physician; resident in postgraduate year 1, 2 or 3, or medical student); provider gender; amount of time the patient spent in the examination room with the provider (provider time); and total time the patient spent in the clinic from check-in to checkout (clinic time). When compared to patients not requiring an interpreter, patients using some form of interpreter had longer mean provider times (32.4 minutes [min] vs 28.0 min, P < .001) and clinic times (93.6 min vs 82.4 min, P = .002). Compared to patients not requiring an interpreter, patients using a telephone interpreter had significantly longer mean provider times (36.3 min vs 28.0 min, P < .001) and clinic times (99.9 min vs 82.4 min, P = .02). Similarly, patients using a patient-supplied interpreter had longer mean provider times (34.4 min vs 28.0 min, P < .001) and mean clinic times (92.8 min vs 82.4 min, P = .027). In contrast, patients using a hospital interpreter did not have significantly different mean provider times (26.8 min vs 28.0 min, P = .51) or mean clinic times (91.0 min vs 82.4 min, P = .16) than patients not requiring an interpreter.
CONCLUSION
In our setting, telephone and patient-supplied interpreters were associated with longer visit times, but full-time hospital interpreters were not.
Keywords: medical interpreters, limited English proficiency, visit time
With an estimated 19.5 million Americans speaking English less than “very well,”1 health care providers and health care systems in the United States must grapple with the issue of how best to communicate with limited English proficiency patients. High quality interpretation for these interactions is an essential ingredient of optimal patient care; it also is required by Title VI of the Civil Rights Act of 1964, which prohibits discrimination against persons with limited English proficiency (Civil Rights Act of 1964, Title 42 of the United States Code). Recent policy guidance from the Office for Civil Rights has clarified the obligation of health care organizations participating in federal programs such as Medicare or Medicaid to provide language assistance to limited English proficiency patients.2
Despite the association of inadequate interpretation with decreased patient satisfaction,3–6 decreased patient understanding of diagnosis and treatment,7 and widespread calls for improved interpretation in health care settings,8–11 little information exists about how interpretation affects the process of health care, even for uncomplicated outcomes such as visit length. While physicians commonly perceive that interpreted visits take longer,12 1 previous study of outpatient visits using health system interpreters found that interpreted visits did not last significantly longer than visits for English speakers.12 In contrast, another study found that Russian- and Spanish-speaking patients using health system interpreters had visits that were longer than visits for English-speaking patients by an average of 7.1 and 12.2 minutes, respectively.13 This study found that patients using personal (i.e., patient-supplied) interpreters did not have significantly longer visits than English-speaking patients. No previous study has compared the visit lengths of patients using hospital, patient-supplied and telephone interpreters. We conducted a time–motion study to compare the visit lengths of patients using one of these 3 methods of interpretation.
METHODS
Setting
We conducted our study in the Medical Primary Care Unit at Rhode Island Hospital. This urban primary care clinic is staffed predominantly by internal medicine residents and nurse practitioners. Medical students and attending physicians also practice in this clinic. The clinic is divided into 2 modules, and annual visit volume is 18,000. Approximately 30% of the clinic's patients have limited English proficiency. Among these limited English proficiency patients, Spanish is the most common language spoken at home (approximately 90%), with smaller numbers speaking Russian, Cambodian, or Portuguese. Very few (less than 5%) of the providers are fluent in Spanish. Three methods of interpretation are used in the clinic. The hospital employs full-time interpreters who complete a rigorous training and certification process. The hospital interpreters are available by pager and are called when the need for their services is identified. One full-time interpreter is assigned to the Medical Primary Care Unit. This interpreter is frequently called to interpret in other parts of the hospital. Thus, delays for full-time interpreters are common. The hospital also participates in a commercial telephone interpreter service, through which patients and providers access an off-site translator via a speakerphone. Telephone interpretation is used for Spanish as well as the less common non-English languages spoken by the patients. Finally, although the use of patient-supplied interpreters (usually a family member or friend) is not encouraged, it is not prohibited and is a common method of interpretation. During the study period, no attempt was made to encourage providers to use a particular type of interpreter. The choice of interpreter type was determined by the preferences of the provider and the patient, taking into consideration the availability of the full-time interpreter. The study protocol was reviewed and approved by the hospital Institutional Review Board.
Subjects
During a 6-week period in July–August 2001, consecutive patient visits to 1 module of the clinic were included in the study. All visits were included, regardless of the type of provider, scheduled visit length or language of the patient.
Measures
Patient Visit Characteristics
Patient demographic information, including age, gender and insurance status was obtained from the clinic registration system. Provider type (medical student; first, second or third postgraduate year resident; nurse practitioner or attending physician) and scheduled visit length (20, 30 or 40 minutes [min]) were obtained from the clinic schedule. Interpreter type was determined by the research assistant who observed patients, providers and interpreters as they entered and exited examination rooms.
Time–Motion Measures
Using a digital watch and a standardized recording form, the research assistant recorded the time each patient checked in to the clinic area, the amount of time that the patient and provider were in the examination room together, and the time the patient checked out from the clinic. We defined provider time as the amount of time that the patient and the provider were in the examination room together. Time that providers spent out of the examination room talking to clinic preceptors was not included in provider time. We defined clinic time as the total time elapsed from check-in to checkout.
Statistical Analysis
For the 4 interpreter groups (no interpreter, hospital interpreter, patient-supplied interpreter, or telephone interpreter), mean provider times and clinic times were compared using t tests. Variables that were significantly associated with provider time (scheduled appointment length, provider type, and interpreter type) were included in a regression model of provider time. Analyses were performed using Stata, Release 6.0 (Stata Corp., College Station, Tex).
RESULTS
Patient Visit Characteristics
During the study period, there were a total of 613 visits (Table 1). Seventy-two percent (n = 441) of the visits required no interpreter, and 28% (n = 172) used some form of interpreter. Fifteen percent (n = 90) of all visits used a patient-supplied interpreter; this was the most common method of interpretation. Eight percent (n = 51) of all visits used a hospital interpreter, and 5% (n = 31) of all visits used a telephone interpreter. Compared to patients not requiring an interpreter, patients using some form of interpreter were older but were not significantly different with regard to gender, provider type, insurance type or mean scheduled visit length (Table 1). In comparison to patients not requiring an interpreter, patients using a hospital interpreter or patient-supplied interpreter were older. Patients using hospital, telephone or patient-supplied interpreters were not significantly different from patients not requiring an interpreter with regard to gender, provider type, insurance type, or mean scheduled visit time.
Table 1.
Visit Characteristics for the Study Population
| No Interpreter Versus | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| No Interpreter (N = 441) | Any Interpreter (N = 172) | P Value | Hospital Interpreter (N = 51) | P Value | Phone Interpreter (N = 31) | P Value | Patient-supplied Interpreter (N = 90) | P Value | |
| Mean age, y (SD) | 46.3 (15.1) | 53.4 (15.8) | <.001 | 53.0 (15.0) | .003 | 48.6 (14.9) | .42 | 55.3 (16.4) | <.001 |
| Female patient, % | 54.8 | 55.8 | .81 | 43.1 | .16 | 58.1 | .72 | 62.2 | .20 |
| Provider type, % | .5 | .56 | .76 | .17 | |||||
| Nurse practitioner | 15.9 | 9.9 | 7.8 | 22.6 | 6.7 | ||||
| PGY 1 | 27.2 | 31.4 | 25.5 | 25.8 | 36.7 | ||||
| PGY 2 | 19.5 | 20.9 | 19.6 | 22.6 | 21.1 | ||||
| PGY 3 | 22.9 | 22.7 | 27.5 | 16.3 | 22.2 | ||||
| Medical student | 11.6 | 12.8 | 13.73 | 12.9 | 12.2 | ||||
| Attending | 3.0 | 2.3 | 5.9 | 0 | 1.1 | ||||
| Female provider, % | 61.5 | 60.5 | .8 | 52.9 | .24 | 71.0 | .29 | 61.1 | .95 |
| Insurance type, % | .16 | .40 | .18 | .07 | |||||
| Medicare | 26.8 | 29.1 | 17.7 | 19.4 | 38.9 | ||||
| Medicaid | 37.9 | 41.9 | 45.1 | 54.8 | 35.6 | ||||
| No insurance | 28.8 | 26.7 | 33.3 | 25.8 | 23.3 | ||||
| Commercial | 6.6 | 2.3 | 3.9 | 0 | 2.2 | ||||
| Mean scheduled visit time, min (SD) | 24.2 (6.1) | 23.6 (6.0) | .3 | 23.3 | .36 | 24.5 | .72 | 23.4 | .31 |
Time-Motion Measures
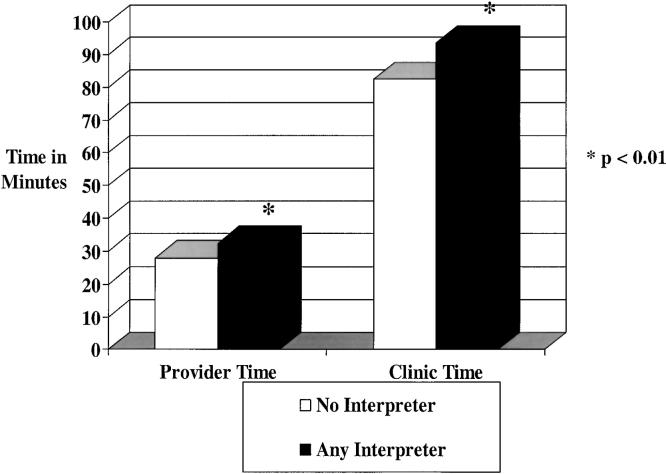
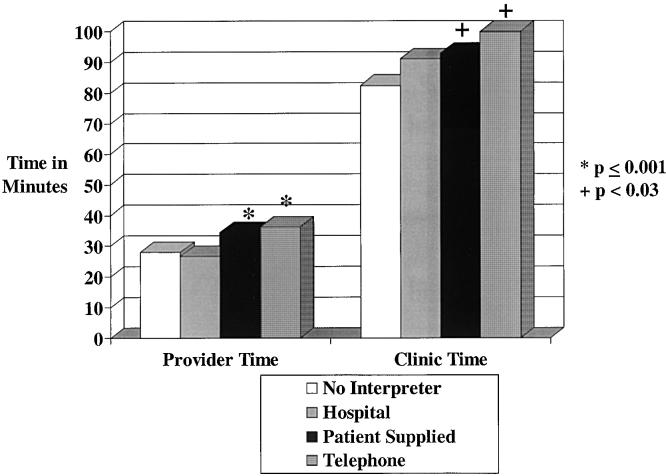
When compared to patients not requiring an interpreter, patients using some form of interpreter had longer mean provider times (32.4 min vs 28.0 min, P < .001) and clinic times (93.6 min vs 82.4 min, P = .002; Fig. 1). Compared to patients not requiring an interpreter, patients using a telephone interpreter had longer mean provider times (36.3 min vs 28.0 min, P < .001) and clinic times (99.9 min vs 82.4 min, P =.02; Fig. 2 Similarly, patients using a patient-supplied interpreter had significantly longer mean provider times (34.4 min vs 28.0 min, P < .001) and mean clinic times (92.8 min vs 82.4 min, P = .027) when compared to patients not requiring an interpreter. In contrast, patients using a hospital interpreter did not have significantly different mean provider times (26.8 min vs 28.0 min, P = .51) or mean clinic times (91.0 min vs 82.4 min, P = .16) than patients not requiring an interpreter.
FIGURE 1.
Mean times by any interpreter use.
FIGURE 2.
Mean times by interpreter type.
Multivariate Analysis
Of the variables age, patient gender, provider gender, insurance status, provider type, interpreter type, and scheduled visit length, only provider type, scheduled visit length, and interpreter type were significantly associated with provider time. These variables were included in a regression model (Table 2). The reference values for the model were nurse practitioner provider, follow-up visit, and no interpreter use. In the model, use of a telephone interpreter was associated with longer mean provider time (8.3 min, 95% confidence interval [95% CI], 3.94 to 12.7) as was use of a patient-supplied interpreter (4.58 min; 95% CI, 1.84 to 7.33). In contrast, hospital interpreter use was not associated with significantly longer mean provider time.
Table 2.
Regression Model of Provider Time (in Minutes)
| Variable | Coefficient | 95% CI |
|---|---|---|
| PGY-1 | 15.6 | 12.5 to 18.7 |
| PGY-2 | 12.2 | 8.9 to 15.5 |
| PGY-3 | 7.2 | 4.0 to 10.5 |
| Medical student | 15.4 | 11.6 to 19.1 |
| Attending | 0.1 | −6.2 to 6.4 |
| Hospital interpreter | −1.7 | −5.2 to 1.8 |
| Phone interpreter | 8.3 | 4.0 to 12.7 |
| Patient-supplied interpreter | 4.6 | 1.8 to 7.3 |
Reference = non-new appointment, nurse practitioner as provider, no interpreter needed.
DISCUSSION
In our setting, patients requiring an interpreter had longer provider times and total clinic times than patients not requiring an interpreter. When different interpretation methods were evaluated, telephone and patient-supplied interpreters were associated with significantly longer visit times, but hospital interpreters were not. Our results for hospital interpreters are consistent with a previous report by Tocher and Larson.12 In their setting, where hospital interpreters were used exclusively, there was no difference in the mean visit times for English- and non–English-speaking patients. However, our results for hospital interpreters differ from the findings of Kravitz et al.13 In their setting, visits for Russian-speaking and Spanish-speaking patients using health system interpreters were longer than visits for English speakers. The reasons for this difference are unclear, but the study populations were somewhat different. We included all patients presenting to our setting, whereas the study by Kravitz et al. included only patients with Medicaid insurance. In the present study, Spanish was the predominant second language, whereas in the Kravitz study, Russian was the most common second language. It also is possible that differences in hospital interpreters between study sites could account for the differences in visit time. In our setting, there is great demand for hospital interpreters, with different departments of the hospital competing for their time. This may create a perceived need on the part of the interpreters to be maximally efficient with their time. Differences in the training of interpreters also could account for the different findings. In our setting, interpreters are trained to assist with achieving closure for patient encounters, and it is possible that the interpreters helped our providers become more efficient by assisting with this aspect of the visit, thereby reducing visit time.
Our finding that interpreted visits took longer than visits not requiring an interpreter is consistent with physicians' perception that interpreted visits take longer.12 The observation that hospital interpreters were the most time efficient may partly explain our previous finding that, in our setting, providers reported higher satisfaction with hospital interpreters than telephone or patient-supplied interpreters.14 It is possible that the higher satisfaction with hospital interpreters was due in part to perceived increased efficiency associated with their use.
The longer visit times associated with telephone interpreter use in this study might be due to the time needed to call the interpreter service and get connected with an interpreter, the need to repeat statements not understood by the patient or telephone interpreter, and the lack of nonverbal communication. The increased visit times associated with patient-supplied interpreters could be due to a number of factors. The patient-supplied interpreter might add observations or concerns that could lengthen the visit and might function also as a patient advocate and increase the visit length by requesting additional explanation, testing, or referral.
Whether the increased efficiency associated with hospital interpreter use in our setting resulted in better patient care is unclear. We previously reported that patients expressed a high degree of satisfaction with our hospital interpreters.14 However, we do not know whether the increased time efficiency observed with hospital interpreters also was associated with less information exchanged during the encounter. Previous research in English-speaking patients has shown an association of increased visit length with a number of desirable outcomes, including increased patient and physician satisfaction, and a decreased risk of malpractice claims.15 In visits with English-speaking patients, extra time may indicate that more information is being exchanged, while in visits with Spanish-speaking patients, extra time may be due to the interpretation process itself.
Our study has a number of limitations. It describes interpreter use in 1 setting and may not be generalizable to other settings with different interpretation needs and methods. In the present study, use of patient-supplied interpreters (52% of all interpreter use) was higher than the rates of 23% to 26% reported in other studies.6,13 The choice of method of interpreter was determined, at least in part, by the paucity of full-time interpreters. This may limit the applicability of our results to settings where full-time interpreters are more available. The large majority of our limited English proficiency patients were Spanish-speaking, and the results might be different in a setting where other non-English languages predominate. We did not assess visits where patients thought an interpreter should have been used, but one was not, and we did not assess visits where providers spoke Spanish with Spanish-speaking patients. However, previous surveys of our residents found that less than 5% were fluent in Spanish, so that the expected number of Spanish concordant visits in our study would be very small (<10).
An additional limitation is the lack of information about the content of the visits, such as the number and severity of problems addressed. We chose a protocol that did not require informed consent, so that we would be able to maximize our response rate and therefore the validity of our findings. The lack of informed consent prevented us from obtaining diagnosis information from the patients' charts. Although we did not have information on diagnosis to include in the regression model, it is not clear that the inclusion of this information would change our results. Previous studies have not found significant differences between visits for English-speaking patients compared to non–English-speaking patients with regard to the Charlson Comorbidity Index12 or mean number of active conditions in the progress note.13 In one of these studies,13 the number of active conditions was significant in the regression model of visit time, but accounted for only 2.24 minutes of visit time. Even if we assume that comorbidity varied among the patients in the interpreter groups, the magnitude of this effect might affect our observed difference in visit time for patient-supplied interpreters, but would not be expected to change our observed difference for visit time associated with telephone interpreters. Finally, we have no information about the quality of, or the satisfaction with, the interpretation for the visits. Therefore, we are unable to determine if the increased time efficiency associated with hospital interpreters came at the expense of losing important information during the encounter.
Our results allow us to estimate the potential savings that could result from eliminating our use of telephone interpreters for Spanish-speaking patients. From our results, 28% of all visits required some form of interpreter. With our annual visit volume of 18,000/year, we could expect 5,040 interpreted visits/year. We found that 18% of all interpreted visits used a telephone interpreter, corresponding to 907 expected telephone interpreter visits/year. The mean visit time for telephone interpreted visits was 36.3 minutes, so that we would expect 907 × 36.3 minutes = 32,924 minutes of telephone interpreter use/year. Since approximately 90% of our telephone interpreter use is for Spanish-speaking patients, we would expect 0.90 × 32,924 minutes = 29,632 minutes of telephone interpretation for Spanish-speaking patients/year. With a cost of $2.30/minute, the yearly cost of telephone interpretation for Spanish-speaking patients would be $2.30 × 29,632 = $68,154/year. With the approximate annual cost of a full-time interpreter in our system at $30,000, 2 additional full-time interpreters could be hired with the cost savings from eliminating telephone interpreter use for Spanish-speaking patients. The addition of 2 new Spanish interpreters would allow us to provide professional interpretation for all Spanish-speaking patients and greatly reduce our reliance on patient-supplied interpreters.
We also can estimate the potential amount of physician time that could be saved by providing hospital interpreters for all Spanish-speaking patients. Since telephone interpreted visits lasted an extra 8.3 minutes on average, we could expect 907 × 8.3 minutes = 7,528 minutes of saved physician time. With an estimated 2,621 visits/year interpreted by patient-supplied interpreters and each of these visits taking an average of 4.6 extra minutes, we could expect 2,621 × 4.6 minutes = 12,057 saved minutes. The total for both groups would be 19,585 minutes. With 90% of these visits being for Spanish speakers, we could expect a savings of 17,627 min/year (294 hours/year) resulting from the provision of hospital interpreters for all Spanish-speaking patients. At 30 minutes/visit, this would represent 588 additional visits/year.
In summary, in our setting, hospital interpreters appeared to be more time-efficient than telephone or patient-supplied interpreters. The time efficiency that we observed in hospital interpreters adds to other potential benefits of hospital interpreters, such as confidentiality, familiarity with medical terminology, cultural sensitivity, and knowledge of the health care system. These results support calls for increased use of professional interpreters in health care settings. Further study is needed to determine how interpretation affects other outcomes, such as the amount and quality of information obtained and transmitted.
REFERENCES
- 1.Profile of Selected Social Characteristics. 2000. U.S. Census Bureau Web site. Available at: http://www.census.gov. Accessed April 8, 2002.
- 2.Office for Civil Rights. Policy guidance: Title VI prohibition against national origin discrimination with limited English proficiency. Available at: http://www.hhs.gov/ocr/lep/guide.html. Accessed October 17, 2002. [Google Scholar]
- 3.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Carrasquillo O, Orav J, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–7. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 5.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14:409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee LL, Batal HA, Maselli JH, Kutner JS. Effect of Spanish interpretation method on patient satisfaction in an urban walk-in clinic. J Gen Intern Med. 2002;17:641–6. doi: 10.1046/j.1525-1497.2002.10742.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baker DW, Parker RM, Williams MV, Coates WC, Pitkin K. Use and effectiveness of interpreters in an emergency department. JAMA. 1996;275:783–8. [PubMed] [Google Scholar]
- 8.Woloshin S, Bickel NA, Schwartz LM, Gany F, Welch HG. Language barriers in medicine in the United States. JAMA. 1995;273:724–8. [PubMed] [Google Scholar]
- 9.Perkins J. Overcoming language barriers to health care. Pop Gov. 1999;65:38–44. [Google Scholar]
- 10.Riddick S. Improving access for limited English-speaking consumers: a review of strategies in health care settings. J Health Care Poor Underserved. 1998;9:S40–S61. [Google Scholar]
- 11.Chang PH, Fortier JP. Language barriers to health care: an overview. J Health Care Poor Underserved. 1998;9:S5–S20. [Google Scholar]
- 12.Tocher TM, Larson EB. Do physicians spend more time with non-English-speaking patients? J Gen Intern Med. 1999;14:303–9. doi: 10.1046/j.1525-1497.1999.00338.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kravitz RL, Helms J, Azari R, Antonius D, Melnikow J. Comparing the use of physician time and health care resources among patients speaking English, Spanish, and Russian. Med Care. 2000;38:728–38. doi: 10.1097/00005650-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Kuo D, Fagan MJ. Satisfaction with methods of Spanish interpretation in an ambulatory care clinic. J Gen Intern Med. 1999;14:547–50. doi: 10.1046/j.1525-1497.1999.07258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dugdale DC, Epstein R, Pantilat SZ. Time and the patient-physician relationship. J Gen Intern Med. 1999;14:s34–40. doi: 10.1046/j.1525-1497.1999.00263.x. [DOI] [PMC free article] [PubMed] [Google Scholar]