Abstract
OBJECTIVE
The American Heart Association (AHA) recommends an automated external defibrillator (AED) be considered for a specific location if there is at least a 20% annual probability the device will be used. We sought to evaluate the cost-effectiveness of the AHA recommendation and of AED deployment in selected public locations with known cardiac arrest rates.
DESIGN
Markov Decision Model employing a societal perspective.
SETTING
Selected public locations in the United States.
PATIENTS
A simulated cohort of the American public.
INTERVENTION
Strategy 1: individuals experiencing cardiac arrest were treated by emergency medical services equipped with AEDs (EMS-D). Strategy 2: individuals were treated with AEDs deployed as part of a public access defibrillation program. Strategies differed only in the initial availability of an AED and its impact on cardiac arrest survival.
RESULTS
Under the base-case assumption that a deployed AED will be used on 1 cardiac arrest every 5 years (20% annual probability of AED use), the cost per quality-adjusted life year (QALY) gained is $30,000 for AED deployment compared with EMS-D care. AED deployment costs less than $50,000 per QALY gained provided that the annual probability of AED use is 12% or greater. Monte Carlo simulation conducted while holding the annual probability of AED use at 20% demonstrated that 87% of the trials had a cost-effectiveness ratio of less than $50,000 per QALY.
CONCLUSIONS
AED deployment is likely to be cost-effective across a range of public locations. The current AHA guidelines are overly restrictive. Limited expansion of these programs can be justified on clinical and economic grounds.
Keywords: emergency medical services, heart arrest, electric countershock, public access difibrillation
It is estimated that 250,000 Americans die each year from out-of-hospital cardiac arrests.1,2 Efforts to improve survival have been hampered by logistical difficulties involved in transporting specialized equipment and responders to the arrest victim.3,4 In an effort to reduce time-to-shock intervals and ultimately improve survival, municipalities have increasingly turned to a decentralized first-responder system predicated upon public access to automated external defibrillators (AEDs).5,6 While AEDs have been available for over 20 years as research instruments, only recently have reductions in their size and cost as well as improvements in their usability made public access defibrillation (PAD) a viable option.7 Evidence is accumulating to support the assertion that public access to AEDs can improve survival compared with historical data.8–10
The American Heart Association has responded to these data by recommending that public access defibrillators be installed if “the frequency of cardiac arrest events is such that there is a reasonable probability of 1 AED use in 5 years.”1 More recently PAD received an endorsement from the United States Congress with the passage of the Community Access to Emergency Defibrillation Act of 2001 to increase federal funding for AED deployment.11
While PAD appears to be a convenient solution to the problem of out-of-hospital cardiac arrest, health authorities faced with limited resources must address the subtleties of deciding precisely which locations warrant deployment of AEDs. Several cost-effectiveness analyses examining AED deployment have been published, but provide limited guidance for policymakers attempting to make informed decisions regarding AED deployment.12–14 A study by Jermyn examined the potential cost-effectiveness of equipping fire fighters with AEDs, but did not evaluate the cost-effectiveness of deploying defibrillators in specific public locations.12 Foutz and Sayre demonstrated that AED deployment in nursing homes may be cost-effective, but did not extend their analysis to other public sites where AEDs might be placed.13 Nichol et al. evaluated the cost-effectiveness of treating victims of out-of-hospital cardiac arrest with emergency medical services (EMS) compared to a strategy of EMS supplemented by AEDs deployed in public locations.14 The investigators found the AED-based strategy to be cost-effective, but interpretation of their results is difficult because the analysis was based upon the assumption that AEDs were deployed in a manner “such that one device was available for each cardiac arrest that occurred in public.”
Furthermore, none of these studies addressed the critical relationship between the probability of cardiac arrest at a given location (and by extension probability of AED use) and the overall cost-effectiveness of AED deployment. While precise data regarding cardiac arrest probabilities at public locations are certainly limited, there is a small body of literature providing estimates of annual arrest rates at several public locations.10,15–17 In light of the rapid adoption of PAD across a range of geographic sites with varying cardiac arrest rates, it is critical to better define the relationship between the probability of cardiac arrest and the cost-effectiveness of AED deployment.
We constructed a Markov model to evaluate the cost-effectiveness of the American Heart Association guideline for AED deployment and to clarify the relationship between the probability of cardiac arrest at a given location and the cost-effectiveness of AED deployment. An additional objective was to use available data on cardiac arrest rates at public locations to provide physicians and other public health experts with a practical tool to use when contemplating AED deployment in the community.
METHODS
Literature Review
Using medline, the 1966 to 2002 medical literature was searched using key words cardiac arrest, defibrillation or defibrillator, and emergency medical services. Additional articles were obtained by scanning bibliographies of relevant articles. For model inputs where a single estimate was available in the medical literature, this estimate was used in the model with broad confidence intervals to account for uncertainty. In cases where multiple estimates for a particular input were available from multiple sources, 1 of the study authors (PC) carefully assessed the methodology of each of the available studies. When 1 study demonstrated clear methodological superiority, the estimate provided by that study was used as the base-case estimate. When no study was identified as methodologically superior, the authors reached a consensus about a base-case estimate and confidence intervals based upon the available literature.
Decision Analytic Model
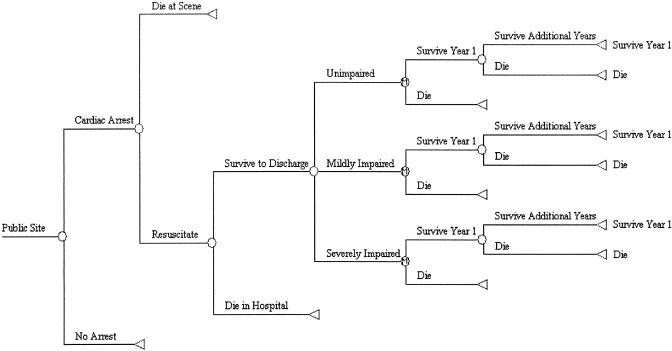
A Markov model was constructed (Fig. 1) using the societal perspective to estimate the clinical and economic consequences of 2 alternative management strategies:
FIGURE 1.
Markov Decision Model: Model for strategies 1 and 2 are identical except for the availability of automated external defibrillator in strategy 1 and the resulting changes in probabilities of cardiac arrest survival.
Strategy 1: Cardiac arrest victims receive treatment by emergency medical services equipped with AEDs (EMS-D).
Strategy 2: Cardiac arrest victims receive initial resuscitation with a nearby AED deployed as part of a PAD program. Upon arrival of EMS, care proceeds according to strategy 1.
All historical costs were adjusted to 2002 dollars using an inflation rate of 3.9% per year to reflect the medical component of the consumer price index between 1998 and 2002.18 Likewise, future costs and benefits were discounted to 2002 dollars at 3% per annum in accordance with the recommendations of the Panel on Cost-effectiveness in Health and Medicine.19 The analysis was performed using DATA 4.0 (TreeAge Software Inc, Williamstown, Mass) and Excel 2000 (Microsoft Inc, Redmond, Wash).
Probability of Clinical Events
The model evaluates the cost-effectiveness of AED deployment (strategy 2) when compared with EMS-based defibrillation (strategy 1). The probabilities of clinical events used in the model are shown in Table 1.
Table 1.
Clinical Probabilities and Cost Inputs Used in Model
| Variable | Base-case | Range | Reference |
|---|---|---|---|
| Probabilities | |||
| Probability of cardiac arrest | 0.2 | 0.01 to 1.00 | 15–17 |
| Probability of automated external defibrillator (AED) use on arrest victim | 1.0 | 0.6 to 1.00 | 8,10,20 |
| Probability of initial resuscitation with emergency medical services (EMS) | 0.25 | 0.15 to 0.35 | 27–29 |
| Probability of initial resuscitation with AED | 0.50 | 0.25 to 0.70 | 8–10 |
| Probability of surviving to hospital discharge with EMS | 0.10 | 0.02 to 0.20 | 27–30 |
| Probability of surviving to hospital discharge with AED | 0.25 | 0.20 to 0.50 | 8–10,31 |
| Probability of dying in first year after cardiac arrest | 0.20 | 0.10 to 0.40 | 32–35 |
| Probability of dying in subsequent years after cardiac arrest | 0.15 | 0.10 to 0.20 | 32–35 |
| Effectiveness | |||
| Mean life expectancy for arrest survivors, y | 5.00 | 3.00 to 7.00 | 32–35 |
| Probability of surviving unimpaired | 0.87 | 0.80 to 0.95 | 30,36 |
| Probability of surviving moderately impaired | 0.09 | 0.05 to 0.15 | 30,36 |
| Probability of surviving severely impaired | 0.04 | 0.00 to 0.10 | 30,36 |
| Quality of life | |||
| Unimpaired | 0.85 | 0.7 to 1.00 | 36,37 |
| Moderately impaired | 0.20 | 0 to 0.40 | 40 |
| Severely impaired | 0.1 | 0 to 0.20 | 40 |
| Costs, $ | |||
| AED purchase | 2,000 | 250 to 3,000 | 21 |
| AED maintenance | 40 | 20 to 80 | 21 |
| AED training | 270 | 100 to 800 | 22–24 |
| AED supplies per use | 150 | 100 to 200 | 21 |
| Hospitalization | |||
| Survive to discharge | 49,000 | 30,000 to 200,000 | 14,22,25,26 |
| Death in hospital | 3,900 | 2,800 to 31,000 | 14,22,25,26 |
| Future medical costs | |||
| First year | 10,600 | 9,000 to 20,000 | 22 |
| Subsequent years | 7,800 | 6,200 to 15,000 | 22 |
To establish a framework for the analysis, we assumed that the baseline probability of cardiac arrest is 0.2 arrests per site per year (1 arrest every 5 years) and that if an arrest occurred at a site equipped with an AED, the device would be used (probability of cardiac arrest equals probability of AED use). The assumption that an available AED always would be used to treat a nearby arrest is based upon the finding of several studies examining the use of AEDs by lay-responders.8,10,20 These studies found that all cardiac arrest victims in casinos, a sports stadium, and an international airport were promptly treated by lay responders using available AEDs. However, it also is possible to envision circumstances in which a cardiac arrest victim might not receive treatment with a nearby AED, despite its availability (probability of cardiac arrest is greater than probability of AED use); this possibility was evaluated using sensitivity analysis. The baseline probability of cardiac arrest (0.2 arrests per site per year) was drawn from the American Heart Association recommendation concerning AED deployment.1 We defined a site as a geographic area that could reasonably be serviced by a single centrally located AED. For example, a private residence is considered a single site while a sports stadium requiring multiple devices would instead contain several sites.
The range of probabilities of cardiac arrests at various sites was derived from the published medical literature (Table 2).10,15–17 Certain large facilities such as airports may have a high annual incidence of cardiac arrests on location, but because of their size, require a correspondingly large number of AEDs to be deployed and consequently, each AED has a low annual probability of being used. Similarly, certain small facilities such as health clubs may have a low annual incidence of cardiac arrests, but can be serviced by a single centrally placed AED.
Table 2.
Annual Incidence of Cardiac Arrest at Various Sites
| Location | Annual Number of Cardiac Arrests Observed at the Location | Number of AEDS Required per Site | Annual Probability of AED Use | Cost per Life-year Gained, $ | Cost per Quality Adjusted Life-year Gained, $ |
|---|---|---|---|---|---|
| International airport | 7 | 15 | .47 | 9,500 | 13,000 |
| Public sports venue | 0.4 | 4 | .1 | 45,000 | 62,000 |
| Golf course | 0.1 | 1 | .1 | 45,000 | 62,000 |
| County jail | 1 | 11 | .09 | 50,000 | 65,000 |
| Health club | 0.08 | 1 | .08 | 56,000 | 74,000 |
| Large shopping mall | 0.6 | 9 | .07 | 64,000 | 84,000 |
| Community center | 0.03 | 1 | .03 | 148,000 | 194,000 |
| Primary care practice | 0.011 | 1 | .01 | 430,000 | 590,000 |
| Hotel | 0.01 | 1 | .01 | 430,000 | 560,000 |
| Restaurant | 0.002 | 2 | .001 | 4,300,000 | 6,000,000 |
| Retail store | 0.0005 | 1 | .0005 | 9,000,000 | 12,000,000 |
Adapted from Becker et al.16 with permission.
AED, automated external defibrillator.
Costs
The cost estimates used in the model are shown in Table 1. AED costs were estimated both by review of the published literature as well as discussion with device manufacturers. AEDs cost approximately $2,000, but this cost is amortized over an expected useful life of 10 years, resulting in an annual cost of $200 per device deployed.21 Training costs were based upon an expectation that 4 employees would each require 2 hours of training per year per AED deployed, and that these employees would earn 150% their normal wage of $14.00 per hour during training.22,23 A cost of $100 per AED per year would be incurred for hiring professional trainers (S. Spenler, Director, Johnson County EMS, written communication, September 24, 2002). This would result in an aggregate training cost of $270 per AED per year. An additional cost of $40 per AED would be incurred annually for device maintenance.21 Furthermore, a cost of $150 is incurred each time an AED is used.21
The estimated costs of hospitalization for cardiac arrest survivors have been reported in several studies and range from $30,000 to $200,000.14,22,24,25 The most comprehensive study of hospitalization costs was conducted by Larsen et al., based upon data collected prospectively during the Antiarrhythmics Versus Implantable Defibrillators trial.25 They calculated costs of initial hospitalization of cardiac arrest survivors (1997 dollars) of either $24,000 or $46,000, depending upon whether the patients received implantable cardiac defibrillators. We estimated a base-case cost of $49,000 by taking the average of the 2 costs reported by Larsen et al. and adjusting for inflation.
Survivors of cardiac arrests can be expected to accrue substantial medical costs over their remaining lifetime as a result of their cardiac disease. A recent study by Groeneveld et al. reported annual medical costs of cardiac arrest survivors (2002 dollars) of $10,600 during the first year and $7,800 in subsequent years.22
Effectiveness of Strategy 1
The benefit of AED deployment stems from any increase in life expectancy afforded by the availability of AEDs on-site (strategy 2) when compared to EMS-D care (strategy 1). The probability of survival of out-of-hospital cardiac arrest to hospital discharge under strategy 1 was estimated to be 10%.26–29
Effectiveness of Strategy 2
While several studies have now demonstrated survival rates of 50% with public use of AEDs, it is likely that AED effectiveness would be significantly lower in less-controlled environments.8–10 Based upon an average time-to-shock interval of 4.5 minutes, a survival rate of 25% appears more consistent with the published literature.30
Life Gained From AED
The life expectancy for cardiac arrest survivors was calculated based upon an expected mortality of 20% during the first year after arrest and 15% thereafter, and takes into account the fact that many cardiac arrest survivors would receive implantable cardiac defibrillators.31–34 On the basis of these estimates, cardiac arrest survivors were expected to have a mean life expectancy of 5 years. Survivors of cardiac arrest were assigned to 1 of 3 cerebral performance categories (CPC) based upon data from the Heartstart Scotland Project as well as the findings of Granja et al.: CPC-1, unimpaired with no residual deficit; CPC-2, moderately impaired with minimal deficits, but able to live independently; CPC-3/4, severely impaired, requiring institutional care.29,35 Utility scores for unimpaired survivors were based upon the findings of Granja et al. and Nichol et al.35,36 Nichol measured health care utility scores of cardiac arrest survivors using the Health Utilities Index Mark 3 System, while Granja et al.obtained similar utility estimates using the EuroQol questionnaire.37,38 Utility scores for the moderately and severely impaired survivors were estimated on the basis of published data from stroke survivors with similar levels of functional impairment.39
Sensitivity Analysis
Because of uncertainty regarding the precise values of model inputs, sensitivity analysis was performed using 3 different techniques. First, 1-way sensitivity analysis was performed for each model input across the entire range of values reported in the literature. Second, 2-way sensitivity analyses were performed for selected inputs that were identified as critical in the 1-way analyses. Finally, a Monte Carlo simulation was performed. This method repeatedly samples from each of the input variables’ distribution ranges, calculating costs and effectiveness for each simulation.40 For the purposes of our analysis, the Monte Carlo simulation was conducted while holding the probability of cardiac arrest and probability of AED use at their base-case values (20% and 100%, respectively), and allowing all other model inputs to vary freely across the range of reported values. For this analysis, cost variables were assigned log-normal distributions.41 All other variables were assigned normal distributions.40
RESULTS
Cost-effectiveness: Base-case
The base-case analysis assumes a 20% annual probability of cardiac arrest at the site of each deployed AED (1 arrest every 5 years). Under this condition, the model demonstrates that AED deployment results in a gain of 0.114 quality-adjusted life years (QALYs) per site (0.15 life years per site) at a cost of $3,400 per site per year. This results in an annual cost of $30,000 per QALY gained ($22,700 per life year gained) for AED deployment (strategy 2) when compared with EMS-D based care (strategy 1).
Cost-effectiveness: Sensitivity Analysis
One-way Sensitivity Analysis
Given the uncertainty in many of the model inputs, multiple 1-way sensitivity analyses were performed across the ranges of data available for the variables (Table 3). Key variables that were observed to substantially impact the results include the annual probability of cardiac arrest at the AED deployment site, the probability that an available AED is used on the cardiac arrest victim, the probability of surviving to hospital discharge with AED, the probability of surviving to hospital discharge with EMS, the cost of hospitalization for the arrest survivors, and the mean life expectancy of cardiac arrest survivors. It is of particular interest that under base-case conditions, as the probability that a cardiac arrest victim is treated with an available AED falls (probability of AED use) from 100% (base-case) to 60%, the cost per QALY gained increases from $30,000 to $49,000.
Table 3.
Results from 1-way Sensitivity Analysis of Selected Variables
| Variable | Range of Variable Estimates | Cost per QALY Gained, $ |
|---|---|---|
| Annual probability of cardiac arrest per site | 0.01 to 1.0 | 590,000 to 6,000 |
| Probability of surviving to hospital discharge with automated external defibrillator (AED) | 0.20 to 0.50 | 44,000 to 11,000 |
| Probability of surviving to hospital discharge with emergency medical services (EMS) | 0.02 to 0.20 | 19,000 to 89,000 |
| Probability of AED use on arrest victim | 0.60 to 1.0 | 49,000 to 30,000 |
| Cost of hospitalization for arrest survivors, $ | 30,000 to 200,000 | 25,000 to 69,000 |
| Future medical costs for arrest survivors, $ | 25,000 to 115,000 | 25,000 to 48,000 |
| AED purchase costs, $ | 250 to 3,000 | 28,000 to 30,000 |
| AED maintenance and training, $ | 100 to 900 | 28,000 to 35,000 |
| Cost of hospitalization for deaths in hospital, $ | 2,800 to 31,000 | 29,000 to 34,000 |
| Life expectancy for arrest survivors, y | 3 to 7 | 61,000 to 18,000 |
| Quality of life for unimpaired survivors | 0.7 to 1 | 35,000 to 25,000 |
| Probability of surviving unimpaired | 0.80 to 0.95 | 32,000 to 28,000 |
QALY, quality-adjusted life year.
Two-way Sensitivity Analysis
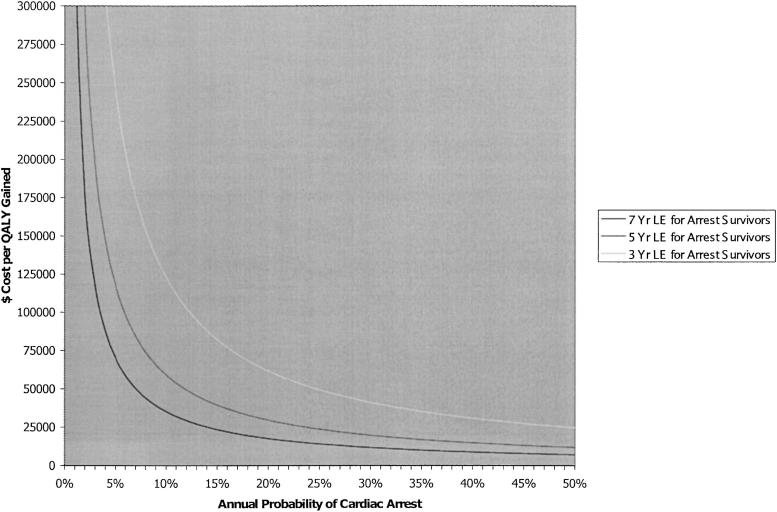
Figure 2 demonstrates the impact of a 2-way sensitivity analysis involving the probability of cardiac arrests at the deployment site and the life expectancy of cardiac arrest survivors on the incremental cost-effectiveness of AED deployment. While the base-case probability of AED use was estimated at 20% per year, the published literature suggests that depending upon the precise location, the annual probability of AED use may be as high as 47% (international airport) or as low as 1% (hotel; Table 2). Under the base-case expectation of a 5-year life expectancy for cardiac arrest survivors, the cost per QALY gained may range from $12,000 (at 50% probability of AED use) to $590,000 (at 1% probability of AED use). The cost per QALY gained is less than $50,000, $100,000, and $150,000 thresholds provided the annual probability of cardiac arrest (and AED use) per site is greater than 12%, 6%, and 4%, respectively.
FIGURE 2.
Sensitivity analysis of the effect of increasing probability of cardiac arrest at a given site on the incremental cost-effectiveness of automated external defibrillator (AED) deployment. By increasing the annual probability of cardiac arrest (and AED use) across a wide range (0.01–0.50), the incremental cost-effectiveness can be seen to decrease from $500,000 to $10,000, given a 5 year life-expectancy (LE) for survivors.
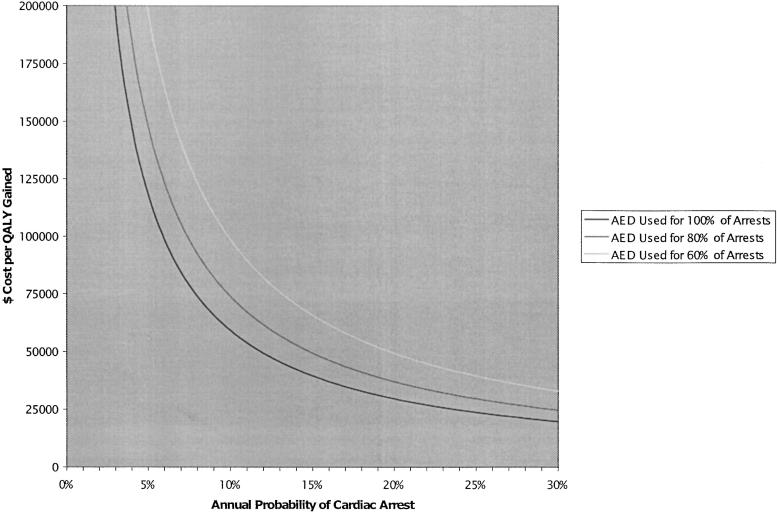
Figure 3 demonstrates the impact of a 2-way sensitivity analysis involving the probability of cardiac arrests at the deployment site and the probability that an available AED is used on the incremental cost-effectiveness of AED deployment, holding all other model inputs at their base-case levels. While available data suggest that all cardiac arrest victims will be treated with an available AED (probability of AED use = 100%), it is likely that this will not always be the case. Under the base-case assumption of a 20% annual probability of cardiac arrest, the cost per QALY gained increases from $30,000 to $37,000 to $50,000 as the probability of AED use falls from 100% to 80% to 60%, respectively.
FIGURE 3.
Sensitivity analysis of the effect of reducing the probability that a deployed automated external defibrillator (AED) is used on the incremental cost effectiveness of AED deployment. As the probability that an available AED is used falls from 100% to 60%, the incremental cost-effectiveness of AED deployment is reduced as well.
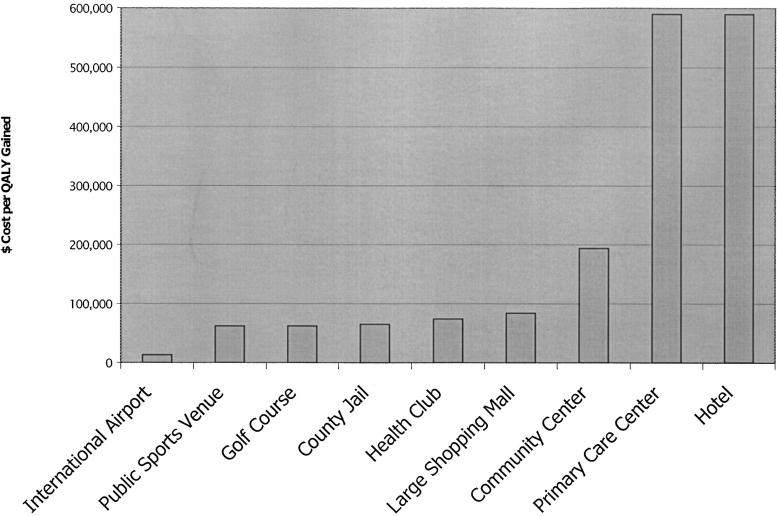
Figure 4 displays cost-effectiveness ratios for several venues with varying cardiac arrest rates where AED deployment might be considered. The cost per QALY gained for AED deployment at various public locations ranges from $13,000 (international airport) to $590,000 (hotel).
FIGURE 4.
The cost-effectiveness of automated external defibrillator (AED) deployment across a range of public sites. The figure provides cost-effectiveness ratios for a range of potential sites of AED implementation.
Monte Carlo Simulation
Monte Carlo simulation performed while holding the probability of cardiac arrest and the probability of AED use constant at 20% and 100%, respectively, resulted in a mean cost per QALY gained of $37,000, a median cost of $33,000 per QALY, and 87% of simulations costing less than $50,000 per QALY gained (95% confidence interval, $15,000 to $73,000). The simulation demonstrated that less than 1% of all trials resulted in a cost-effectiveness ratio greater than $100,000.
DISCUSSION
Automated external defibrillators are easy to use and relatively affordable to purchase. Manufacturers have publicized these attributes in an effort to expedite the transition to PAD.42 While this publicity appears to have succeeded in broadening public awareness of cardiac arrest, it also may have contributed to imprudent AED deployment. Reports abound concerning purchase of defibrillators by relatively low-risk executives and concerned high school students.43,44 Before a strategy of PAD is further expanded, it is imperative to understand the costs and benefits associated with this potentially life-saving technology.
Ideally, the probability of cardiac arrest at each and every site would be known and AEDs could then be deployed accordingly. The results of the ongoing Public Access Defibrillation Trial will certainly help to answer a number of questions related to PAD.45 However, even after completion of this study, there will be many locations where AED deployment is considered, but the precise probability of cardiac arrest is unknown.
In the absence of comprehensive location-specific cardiac arrest rates, our analysis provides important guidance as to where AED deployment should be considered. The results of this study support the results of earlier studies suggesting that AED deployment in selected public locations is a cost-effective use of health resources.13,14,22 Our results also suggest that the current American Heart Association guidelines limiting AED deployment to sites with a 20% annual probability of cardiac arrest and cost per QALY gained of $30,000 may be overly conservative.
Several aspects of the sensitivity analysis warrant additional discussion. First, it is important to note that our analysis suggests that deployment of AEDs in locations with exceedingly low cardiac arrest rates is unlikely to be cost-effective even using the most optimistic assumptions. Second, the cost-effectiveness of AED deployment is sensitive to the probability that the deployed AED is actually used on a cardiac arrest that does occur at the site of deployment. Therefore, it is critical that deployed AEDs be accessible and easily identifiable to potential responders. Finally, it is important to note that the cost-effectiveness of AED deployment depends upon the relative benefit that AED deployment provides relative to EMS-D–based care. The cost-effectiveness of AEDs may be reduced by any improvement in cardiac arrest survival that might be generated by optimization of existing EMS-D systems. Therefore, many sites with low cardiac arrest rates might carefully consider encouraging optimization of existing EMS services rather than spending limited resources on AEDs that are unlikely to be used.
We were deliberately conservative in many of our estimates to avoid biasing our findings in favor of overly aggressive AED deployment. For example, we estimated annual mortality of 15% for cardiac arrest survivors, despite evidence that it may be significantly lower. We also took a conservative approach by estimating that only 25% of cardiac arrest victims survived their arrest despite evidence from Valenzuela et al. and Caffrey et al. that results may be significantly higher.8,10 Furthermore, we did not include potential utility gains that may be realized by the public from the sense of security (a.k.a. passive benefit) afforded by AED availability.46 Finally, we included substantial costs for AED maintenance and employee training despite evidence that training may not be necessary and AED maintenance costs may be minimal.10,47
There are several limitations to our study that are important to understand. First, it is important to acknowledge that the precise probability of cardiac arrests for any specific location is impossible to predict with certainty because each location serves a unique population. Our study relies on generalization of cardiac arrest rates in King County, Washington to other locations across the United States. While such generalization is not ideal, King County is a large metropolitan area with a diverse population that is representative of the overall population of the United States. Therefore, it is reasonable to generalize these cardiac arrest rates to other areas.48,49 Likewise, it is difficult to define with precision both the number of AEDs required for each location and the related probability that the device will be used. Becker et al. estimated the number of AEDs required at various public locations by using common sense (i.e., a shopping mall would require 1 AED per main entrance), and we applied these estimates to our model.16 While this approach may be criticized as arbitrary, the current decisions of precisely how many AEDs should be deployed in a shopping mall or airport are based on similar reasoning and likewise were applied to this analysis.10 Finally, while experience to date suggests that Good Samaritans consistently use publicly available AEDs on cardiac arrest victims, our analysis demonstrates that the cost-effectiveness of this intervention is reduced by any failure to use a publicly available AED on a nearby cardiac arrest victim; further experience will provide additional guidance as to how often this occurs.
Despite these limitations, this analysis provides important data to support a policy of AED deployment at selected public locations. Conversely, this analysis suggests that deployment of AEDs in other public locations including hotels and retail stores may not be justified on clinical and economic grounds alone. It is critical to understand that the cost-effectiveness of defibrillator deployment improves as the probability of that defibrillator being used on a cardiac arrest victim rises. Reaching a critical threshold of aggregate risk may occur within a single individual at high risk for cardiac arrest (justifying an implantable cardiac defibrillator) or among many moderate-risk individuals (thus warranting deployment of an AED). Using this framework correctly will help to ensure that AEDs are placed in the locations where the largest number of people stand to benefit. Further research is needed to more precisely determine which individuals and locations may benefit from AED availability.
Acknowledgments
There was no external source of funding for this study. Dr. Cram was supported by a fellowship grant from the Agency for Healthcare Research and Quality during a portion of this work, and Dr. Vijan is a Veterans Affairs Health Services Research and Development Career Development Awardee. No funding agency had any role in the design, conduct, or reporting of the study.
REFERENCES
- 1.The American Heart Association. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2000;2:1–76. [Google Scholar]
- 2.Zheng Z-J, Croft JB, Giles WH, Mensah GA. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–63. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 3.Becker LB, Ostrander MP, Barrett J, Kondos GT. Outcome of CPR in a large metropolitan area—where are the survivors? Ann Emerg Med. 1991;20:355–61. doi: 10.1016/s0196-0644(05)81654-3. [DOI] [PubMed] [Google Scholar]
- 4.Lombardi G, Gallagher J, Gennis P. Outcome of out-of-hospital cardiac arrest in New York City. JAMA. 1994;271:678–83. [PubMed] [Google Scholar]
- 5.Smith SC, Hamburg RS. Automated external defibrillators: time for federal and state advocacy and broader utilization. Circulation. 1998;97:1321–4. doi: 10.1161/01.cir.97.13.1321. [DOI] [PubMed] [Google Scholar]
- 6.Eisenberg M. Is it time for over-the-counter defibrillators? JAMA. 2000;284:1435–7. doi: 10.1001/jama.284.11.1435. [DOI] [PubMed] [Google Scholar]
- 7.Liberthson RR, Nagel EL, Hirschman JC, Nussenfeld S. Prehospital ventricular defibrillation. N Engl J Med. 1974;291:317–21. doi: 10.1056/NEJM197408152910701. [DOI] [PubMed] [Google Scholar]
- 8.Valenzuela TD, Roe DJ, Nichol G, Clark LL, Spaite DW, Hardman RG. Outcomes of rapid defibrillation by security officers after cardiac arrest in casinos. N Engl J Med. 2000;343:1206–9. doi: 10.1056/NEJM200010263431701. [DOI] [PubMed] [Google Scholar]
- 9.Page RL, Joglar JA, Kowal RC, Zagrodzky JD, Nelson LL, Ramaswamy K. Use of automated external defibrillators by a U.S. airline. N Engl J Med. 2000;343:1210–6. doi: 10.1056/NEJM200010263431702. [DOI] [PubMed] [Google Scholar]
- 10.Caffrey SL, Willoughby PJ, Pepe PE, Becker LB. Public use of automated external defibrillators. N Engl J Med. 2002;347:1242–7. doi: 10.1056/NEJMoa020932. [DOI] [PubMed] [Google Scholar]
- 11.Community Access to Emergency Defibrillation Act of 2001. 107th Congress, 2001. Available at: http://thomas.loc.gov/cgi-bin/query/D?r107:5:./temp/~r107D3P1y7. Accessed March 31, 2003.
- 12.Jermyn BD. Cost-effectiveness analysis of rural/urban first-responder defibrillation program. Prehosp Emerg Care. 2000;4:43–7. doi: 10.1080/10903120090941632. [DOI] [PubMed] [Google Scholar]
- 13.Foutz RA, Sayre MR. Automated external defibrillators in long-term care facilities are cost-effective. Prehosp Emerg Care. 2000;4:314–7. doi: 10.1080/10903120090941010. [DOI] [PubMed] [Google Scholar]
- 14.Nichol G, Hallstrom AP, Ornato JP, et al. Potential cost-effectiveness of public access defibrillation in the United States. Circulation. 1998;97:1315–20. doi: 10.1161/01.cir.97.13.1315. [DOI] [PubMed] [Google Scholar]
- 15.Becker L, Eisenberg M, Fahrenbruch C, Cobb L. Cardiac arrest in medical and dental practices. Arch Intern Med. 2001;161:1509–12. doi: 10.1001/archinte.161.12.1509. [DOI] [PubMed] [Google Scholar]
- 16.Becker L, Eisenberg M, Fahrenbruch C, Cobb L. Public locations of cardiac arrest: implications for public access defibrillation. Circulation. 1998;97:2106–09. doi: 10.1161/01.cir.97.21.2106. [DOI] [PubMed] [Google Scholar]
- 17.Frank RL, Rausch MA, Menegazzi JJ, Rickens M. The locations of nonresidential out-of-hospital cardiac arrests in the city of Pittsburgh over a three-year period. Prehosp Emerg Care. 2001;5:247–51. doi: 10.1080/10903120190939724. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Healthcare inflation index 1998–2002. Available at: http://cms.hhs.gov/statistics/health-indicators/t9.asp. Accessed March 31, 2003. [Google Scholar]
- 19.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. [Google Scholar]
- 20.Wassertheil J, Keane G, Fisher N, Leditschke JF. Cardiac arrest outcomes at the Melbourne cricket ground and shrine of remembrance using a tiered response strategy—a forerunner to public access defibrillation. Resuscitation. 2000;44:97–104. doi: 10.1016/s0300-9572(99)00168-9. [DOI] [PubMed] [Google Scholar]
- 21.Zoll Medical Corporation. Cost of AEDs. Available at: http://www.zoll.com/aed.htm. Accessed March 31, 2003. [Google Scholar]
- 22.Groeneveld PW, Kwong JL, Liu J, et al. Cost-effectiveness of automated external defibrillators on airlines. JAMA. 2001;286:1482–89. doi: 10.1001/jama.286.12.1482. [DOI] [PubMed] [Google Scholar]
- 23.Bureau of Labor Statistics. National compensation survey: occupational wages in the United States, 2001. Available at: http://www.bls.gov/ncs/ocs/sp/ncbl0449.pdf. Accessed March 31, 2003. [Google Scholar]
- 24.Mushlin AI, Hall WJ, Zwanziger J, et al. The cost-effectiveness of automatic implantable cardiac defibrillators: results from MADIT. Circulation. 1998;97:2129–35. doi: 10.1161/01.cir.97.21.2129. [DOI] [PubMed] [Google Scholar]
- 25.Larsen G, Hallstrom A, McAnulty J, Pinski S, Olarte A, Sullivan S. Cost-effectiveness of the implantable cardioverter-defibrillator versus antiarrhythmic drugs in survivors of serious ventricular tachyarrhythmias: results of the AVID economic analysis substudy. Circulation. 2002;105:2049–57. doi: 10.1161/01.cir.0000015504.57641.d0. [DOI] [PubMed] [Google Scholar]
- 26.Sweeney TA, Runge JW, Gibbs MA, et al. EMT defibrillation does not increase survival from sudden cardiac death in a two-tiered urban-suburban EMS system. Ann Emerg Med. 1998;31:234–40. doi: 10.1016/s0196-0644(98)70313-0. [DOI] [PubMed] [Google Scholar]
- 27.Mosesso VN, Jr, Davis EA, Auble TE, Paris PM, Yealy DM. Use of automated external defibrillators by police officers for treatment of out-of-hospital cardiac arrest. Ann Emerg Med. 1998;32:200–6. doi: 10.1016/s0196-0644(98)70137-4. [DOI] [PubMed] [Google Scholar]
- 28.Stults KR, Brown DD, Kerber RE. Efficacy of an automated external defibrillator in the management of out-of-hospital cardiac arrest: validation of the diagnostic algorithm and initial clinical experience in a rural environment. Circulation. 1986;73:701–9. doi: 10.1161/01.cir.73.4.701. [DOI] [PubMed] [Google Scholar]
- 29.Sedgwick ML, Dalziel K, Watson J, Carrington DJ, Cobbe SM. Performance of an established system of first responder out-of-hospital defibrilation. The results of the second year of the Heartstart Scotland Project in the ‘Utstein style’. Resuscitation. 1993;26:75–88. doi: 10.1016/0300-9572(93)90166-n. [DOI] [PubMed] [Google Scholar]
- 30.Valenzuela TD, Roe DJ, Cretin S, Spaite DW, Larsen MP. Estimating effectiveness of cardiac arrest interventions. Circulation. 1997;96:3308–13. doi: 10.1161/01.cir.96.10.3308. [DOI] [PubMed] [Google Scholar]
- 31.The Antiarrhythmics Versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med. 1997;337:1576–83. doi: 10.1056/NEJM199711273372202. [DOI] [PubMed] [Google Scholar]
- 32.Connolly SJ, Hallstrom AP, Cappato R, et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. Eur Heart J. 2000;21:2071–8. doi: 10.1053/euhj.2000.2476. [DOI] [PubMed] [Google Scholar]
- 33.Cobbe SM, Dalziel K, Ford I, Marsden AK. Survival of 1476 patients initially resuscitated from out-of-hospital cardiac arrest. BMJ. 1996;312:1633–6. doi: 10.1136/bmj.312.7047.1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kuilman M, Bleeker Jan K, Hartman AM, Simoons ML. Long-term survival after out-of-hospital cardiac arrest: an 8-year follow-up. Resuscitation. 1999;41:25–31. doi: 10.1016/s0300-9572(99)00016-7. [DOI] [PubMed] [Google Scholar]
- 35.Granja C, Cabral G, Pinto AT, Costa-Pereira A. Quality of life 6-months after cardiac arrest. Resuscitation. 2002;37:37–44. doi: 10.1016/s0300-9572(02)00203-4. [DOI] [PubMed] [Google Scholar]
- 36.Nichol G, Stiell IG, Hebert P, Wells GA, Vandemheen K, Laupacis A. What is the quality of life for survivors of cardiac arrest? A prospective study. Ann Emerg Med. 1999;6:95–102. doi: 10.1111/j.1553-2712.1999.tb01044.x. [DOI] [PubMed] [Google Scholar]
- 37.Torrance GW, Furlong W, Feeny D, Byle M. Multi-attribute preference functions: health utilities index. Pharmacoeconomics. 1995;7:503–20. doi: 10.2165/00019053-199507060-00005. [DOI] [PubMed] [Google Scholar]
- 38.The EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy (New York) 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 39.Gage BF, Cardinalli AB, Owens DK. The effect of stroke and stroke prophylaxis with aspirin or warfarin on quality of life. Arch Intern Med. 1996;156:1829–36. [PubMed] [Google Scholar]
- 40.Doubilet P, Begg CB, Weinstein MC, Braun P, McNeil BJ. Probabilistic sensitivity analysis using Monte Carlo simulation. Med Decis Making. 1985;5:155–77. doi: 10.1177/0272989X8500500205. [DOI] [PubMed] [Google Scholar]
- 41.Pasta DJ, Taylor JL, Henning JM. Probabilistic sensitivity analysis incorporating the bootstrap. Med Decis Making. 1999;19:353–63. doi: 10.1177/0272989X9901900314. [DOI] [PubMed] [Google Scholar]
- 42.National Center for Early Defibrillation. Available at: http://www.early-defib.org/. Accessed March 31, 2003. [Google Scholar]
- 43.Pereira J. For the fearful: portable defibrillators. Wall Street Journal. September 1, 1999: section B: 1. [Google Scholar]
- 44.Schimke A. Huron grads offer gift of life to school. Ann Arbor News. March 14, 2001: section D: 1. [Google Scholar]
- 45.Public Access Defibrillation Trial. Available at: http://depts.washington.edu/padctc/. Accessed March 31, 2003.
- 46.Crum P, Vijan S, Wolbrink A, Fendrick AM. The impact of including passive benefits in cost-effectiveness analysis: the case of automated external defibrillators on commercial aircraft. Value Health. 2003;6:466–73. doi: 10.1046/j.1524-4733.2003.64224.x. [DOI] [PubMed] [Google Scholar]
- 47.Gundry JW, Comess KA, DeRook FA, Jorgenson D, Bardy GH. Comparison of naive sixth-grade children with trained professionals in the use of an automated external defibrillator. Circulation. 1999:1703–7. doi: 10.1161/01.cir.100.16.1703. [DOI] [PubMed] [Google Scholar]
- 48.2000 United States Census Data. National Summary. Available at: http://factfinder.census.gov/servlet/QTTable?ds_name=DEC_2000_SF1_U&geo_id=01000US&qr_name=DEC_2000_SF1_U_DP1. Accessed March 31, 2003.
- 49.2000 United States Census Data. City of Seattle. Available at: http://factfinder.census.gov/bf/_lang=en_vt_name=DEC_2000_PL_U_QTPL_geo_id=16000US5363000.html. Accessed March 31, 2003.