Abstract
BACKGROUND
Primary care physicians are spending fewer hours in direct patient care, yet it is not known whether reduced hours are associated with differences in patient outcomes.
OBJECTIVE
To determine whether patient outcomes vary with physicians' clinic hours.
DESIGN
Cross-sectional retrospective design assessing primary care practices in 1998.
SETTING
All 25 outpatient-clinics of a single medical group in western Washington.
PARTICIPANTS
One hundred ninety-four family practitioners and general internists, 80% of whom were part-time, who provided ambulatory primary care services to specified HMO patient panels. Physician appointment hours ranged from 10 to 35 per week (30% to 100% of full time).
MEASUREMENTS
Twenty-three measures of individual primary care physician performance collected in an administrative database were aggregated into 4 outcome measures: cancer screening, diabetic management, patient satisfaction, and ambulatory costs. Multivariate regression on each of the 4 outcomes controlled for characteristics of physicians (administrative role, gender, seniority) and patient panels (size, case mix, age, gender).
MAIN RESULTS
While the effects were small, part-time physicians had significantly higher rates for cancer screening (4% higher, P = .001), diabetic management (3% higher, P = .033), and for patient satisfaction (3% higher, P = .035). After controlling for potential confounders, there was no significant association with patient satisfaction (P = .212) or ambulatory costs (P = .323).
CONCLUSIONS
Primary care physicians working fewer clinical hours were associated with higher quality performance than were physicians working longer hours, but with patient satisfaction and ambulatory costs similar to those of physicians working longer hours. The trend toward part-time clinical practice by primary care physicians may occur without harm to patient outcomes.
Keywords: part-time physicians, quality of care, primary care, physicians characteristics, patient satisfaction
While physicians' total hours of work have not decreased,1 the time that primary care physicians spend in direct patient care decreased by 10% during the 1990s.2,3 In part, this decrease in clinical hours was associated with the new and varied practice environments. As integrated delivery systems, managed care organizations, and other health services organizations have adapted to and innovated practices, the employment of part-time physicians has increased (T. Syltebo, MD, in conversation, January 2000). Whether the reduction in hours is dictated by organizations, is a consequence of organizational changes, or is a personal choice of physicians, the impact of part-time practice on patient outcomes is unknown.
Physicians reduce their clinical time for a wide variety of reasons.4 Some physicians hold related responsibilities within the same environment, such as teaching, conducting research, or managing programs on a part-time basis. Others choose to care for family members, foster social causes, pursue avocations, begin entrepreneurial enterprises, or extend their education (interviews conducted by Parkerton in 1999). Furthermore, the primary care role has been changed by the increased specialization of physicians, including the emergence of hospitalists, and the administrative demands (and opportunities) of managed care.5,6
The trend toward more primary care physicians engaging in clinical practice on a part-time basis gives rise to concerns about patient outcomes, deterring some managed care organizations from employment of part-time providers.7 Because primary care is defined as continuous, coordinated, and comprehensive care,8 it could easily be inferred that continuous physician availability is important and that a traditional, full-time work schedule would be beneficial to patient care. However, validation that physicians' clinic hours are a marker for better patient care is unavailable. In one academic setting, for example, part-time physicians' performance did not differ from that of full-time physicians.9 To shed more light on this line of inquiry, we attempted to understand the consequences of reduced hours in the community ambulatory setting, and investigated the association between clinical hours and patient outcomes. While previous studies have assessed part-time practice,10,11 they have neither enumerated nor evaluated direct patient-care hours as a continuous variable.4,7,9,12,13 This study examines the association between the number of physician primary care clinical hours and 4 patient outcomes: cancer screening, diabetic management, patient satisfaction, and ambulatory costs.
METHODS
Study Design, Setting, and Data
This is a cross-sectional design assessing primary care practice in all medical clinics of a single group-model HMO. Medical group physicians worked in 25 western Washington medical clinics, all of which provided primary care, radiology, laboratory, pharmacy, and business services and, in some of them, specialty services. The study population included all 194 family practitioners or general internists providing ambulatory primary care services for at least 9 months of 1998 to a defined patient panel (from 320,000 adult HMO members). Therefore, physicians providing urgent care exclusively were not included, as they did not have a patient population for which they were responsible.
The medical group generated measures of individual physician performance from which the study outcome measures were derived. These measures have been distributed quarterly to the physicians since 1997, encouraging data validation. In addition to patient outcomes, data included clinical hours, appointment access, panel composition, and case mix. Medical group human resources provided data on employment date, seniority, and administrative role. Board certification and verification for specialty and gender were obtained from medical directories and the American Medical Association's web site.12–16 Following approval by the Institutional Review Board associated with the Center for Health Studies, data were merged using a random identifier to protect physician confidentiality. All physicians had 4 quarters of data. Data collected independently each quarter on ambulatory costs were averaged for the preceding year, producing annualized component measures. All other data were reported as averages of the previous twelve months.
Funding sources placed no constraints upon this research and Group Health Cooperative of Puget Sound, the HMO, allowed access to the organization and its data without determining the topic of inquiry, its analysis, or interpretation.
Part-time Status
Physician part-time practice status was measured as the percent of full-time clinical hours minus full-time equivalent (FTE). The HMO defined full time as 10 sessions, or 35 hours per week of patient appointment hours; fewer were considered part time. Three sessions were the fewest that primary care physicians could work and have their own designated patient panel and, therefore, be included in this study. The actual range of 0.30 to 0.95 FTE was treated as a continuous variable. Of these 194 physicians, 39% were employed full time by the organization. The other 61% were employed on a part-time basis. However, because 18.5% of physicians employed full time also held administrative or other clinical responsibilities that reduced primary care clinical time, full-time clinicians represented only 20.5% of the total.
Outcome Measurement
Four types of outcomes and 4 corresponding aggregate measures were selected based on availability and frequency of reporting: preventive services (cancer screening), treatment services (diabetes management), patient-reported outcomes (patient satisfaction), and economic outcomes (ambulatory costs), as presented in Appendix A. These 4 measures are consistent with published conceptual models of quality of care,17–19 have been validated and used widely,20 are common enough for reliable assessment,21 and represent different aspects of care. Table 1 contains their descriptive statistics. All but the cost measures are included in the Health Plan Employer Data and Information Set required of managed care organizations by the National Committee on Quality Assurance (NCQA).22 Additionally, the cost measures are consistent with NCQA report cards.22 While there are many opinions on what constitutes “quality,” Donabedian, the architect of quality definitions, would support the inclusion of patient satisfaction and costs as essential.23 Other definers of quality also identify patient satisfaction and costs as valid measures.17,19,24
Table 1.
Outcome Variable Descriptive Statistics and Comparisons of Means for Part-time and Full-time Physicians
| Full Time (N = 38) | Part Time (N = 156) | ||||
|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | t Test, Significance |
| Outcome measures | |||||
| Cancer screening, % | 73 | 6.1 | 77 | 4.9 | 0.001* |
| Diabetic management, % | 79 | 9.3 | 82 | 8.4 | 0.033† |
| Patient satisfaction, % excellent | 40 | 11.3 | 43 | 8.5 | 0.035† |
| Ambulatory costs‡, $ | 83 | 12.0 | 86 | 11.2 | 0.239 |
P < .001.
P < .05.
Full time, N = 35; part time, N = 141.
The provision of preventive services is a central element of primary care and the rates of both mammography and Pap testing are considered to reflect attentive care.20,25,26 These screening tests for cancer in women were needed by a large enough population to have sufficient numbers in individual panels for reliable evaluation and were found to have a moderate correlation coefficient of 0.47 (P = .01). This preventive measure was formed from the means of the mammography rates for women aged 52 to 64 years and of Pap testing in women aged 21 to 64 years.
The high presence of diabetes mellitus in the U.S. population (6%) makes it an appropriate condition for the study of chronic care management.27 The rates of microalbuminuria testing, hemoglobin A1c testing, annual retinal examinations, and annual foot examinations—all measures of good clinical management as identified by the Diabetic Quality in Practice Project28—are monitored for the HMO's nearly 20,000 diabetic patients. Their mean formed the diabetic management outcome measure. The number of diabetics per practice panel ranged from 8 to 267, and we included all panels in the analysis.
Consistent with other health plans, this HMO evaluates patient satisfaction with the Consumer Assessment of Health Plans Survey.29 A 4-page survey was mailed to a percentage of each physician's patients, following doctor visits, selecting the patients from a stratified sample based upon their visit utilization rates (to avoid a bias toward those with frequent appointments). Each of the 7 questions, focused upon the provider, were rated on a Likert scale and reported as the percentage of responses rated excellent.
Total ambulatory costs included both primary care and specialty costs, including laboratory, radiology, and prescriptions. Because the data included costs separately for Medicare patients (13% of patients) and non–Medicare patients (87%), a weighted average of Medicare and non-Medicare costs was used in the analysis.
The component measures are consistent with industry standards22 and accepted quality measures.17,19 Reliability testing was performed across the 4 quarters of data on the component measures using SPSS, version 10 (SPSS, Inc., Chicago, Ill), reliability analysis, α technique.30 Individual physician assessments with Cronbach's α under 0.80 should be viewed with caution.31 Three of the 23 component measures had alphas between 0.70 and 0.73, and were included only as part of aggregate measures.
Control Variables: Physician and Patient Panel Characteristics
Variables that might be correlated with both clinical hours and outcome measures would confound results. Therefore, both physician and patient panel characteristics were included in the analysis to control for their influence on outcomes. Because variation in the number and case-mix severity of patients might impact the assessment of practice, the panel sizes and case-mix variables were included in the analysis. The actual panel sizes were divided by the physicians' FTEs so that they became a measure of workload. Because utilization is a factor in ambulatory costs and in stratification prior to the patient satisfaction survey, we have included 3 indicators of patient panel case mix/severity: patient gender (percent female); average patient age; and chronic disease score (CDS) developed at Group Health Cooperative, which uses administrative prescription data to identify illness severity and prevalence.32 The closed-panel nature of this organization with pharmacy and prescription benefits leads to highly reliable pharmacy benefit data, making the CDS useful.
Three physician characteristics, with possible relationships with hours worked, were available as control variables for this study: gender, administrative role, and seniority. Previous studies have shown that female physicians work fewer hours than do their male counterparts,33–35 administrators reduce their clinical hours to meet management responsibilities, and seniority might influence the desire to work full time. A relationship was hypothesized for each characteristic with 1 or 2 of the outcomes: female physicians with higher patient satisfaction and better cancer screening,36 administrative role with lower costs, and seniority with lower costs and higher clinical quality. The 33 administrative physicians included team leaders, medical center chiefs, district chiefs, and those with other HMO responsibilities such as clinical guideline development. Seniority was represented by years since graduation from medical school, which was highly correlated (0.65, P < .01) with years with the HMO. Over 90% of these physicians were board certified, and 92% were family practitioners; therefore, specialty and certification were not assessed. Table 2 presents descriptive statistics on all control variables.
Table 2.
Control Variable Descriptive Statistics and Comparisons of Means for Part-time and Full-time Physicians
| Full Time (N = 38) | Part Time (N = 156) | ||||
|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | t Test, Significance |
| Physician characteristics | |||||
| Physician gender, % male | 87 | — | 58 | — | 0.001* |
| Administrative time (FTE) | — | — | 0.07 | 14.3 | — |
| Medical seniority, y‡ | 24 | 6.7 | 19 | 6.7 | 0.000† |
| Patient panel characteristics | |||||
| Workload (panel size/FTE) | 2,111 | 355 | 2,142 | 365 | 0.636 |
| Patient gender, % male | 52 | 11.3 | 42 | 16.6 | 0.001† |
| Mean age, y | 46 | 4.0 | 43 | 4.7 | 0.006* |
| Panel case mix (CDS) | 1.08 | 0.35 | 0.988 | 0.30 | 0.096 |
FTE, full-time equivalent; CDS, chronic disease score.
P < .01.
P < .001.
Part time, N = 152.
Analysis
Patient-level data for each component measure were averaged across patients, within each physician panel. Then, the mean component measures were averaged to generate aggregate, physician-level outcomes. Higher rates are better outcomes for cancer screening, diabetic management compliance, and patient satisfaction. However, cost is defined as the better outcome when lower. We performed linear regression analysis to determine the relationships between physicians' clinical hours and each of the 4 outcome measures for their panels (total ambulatory costs, and percent of eligible patients screened for cancer, receiving appropriate diabetic management, and rating satisfaction as excellent). Each model controlled for physician gender, physician administrative role, physician seniority, gender distribution of the panel, average age of patients in the panel, physician workload, and case mix. All analyses were performed using SPSS software, version 10. Introducing the control variables as a block in the regressions on each outcome followed by the physician clinical hours variable facilitated partitioning of variance to assess the amount of independent association of physician hours on performance measures.
RESULTS
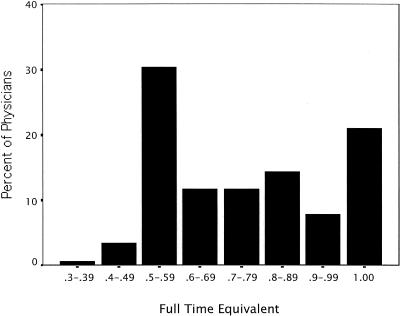
Physicians' primary care clinic hours were distributed as shown in Figure 1, with a bimodal distribution, 30% half time (0.50–0.59 FTE) and 20% full time (1.0 FTE). Thirty-nine percent of the physicians worked for the HMO full time. However, just 4% worked less than half time, the commitment required for fringe benefits. Part-time physicians were more likely to be female (P = .001) and less senior than full-time physicians (P = .001). The 33 administrative physicians were all part-time clinicians and included team leaders, medical center chiefs, district chiefs, and those with other Medical Group responsibilities such as clinical guideline development.
FIGURE 1.
Clinical appointment hours of primary care physicians. One full time equivalent (1.0 FTE ) equals 35 hours. Distribution of 194 physicians.
Bivariate results are displayed in Table 1, which compares the uncontrolled outcomes of part-time and full-time physicians, and Table 2, which compares the means of all independent variables by part- or full-time status. Part-time physicians had significantly higher rates for cancer screening (4% higher, P < .001), for diabetic management (3% higher, P = .033), and for patient satisfaction (3% higher, P = .035). The rates did not differ significantly for ambulatory costs. Five of the 7 control variables, all but those for physician and patient-panel gender, were significant for 1 or 2 of the outcomes. Professional seniority had a quadratic relationship with costs (P = .008, .003), which were highest for physicians with 16 to 25 years since medical school and lowest after 35 to 44 years. Physicians holding an administrative role were associated with increased ambulatory costs (P = .005). An increase in patient panel size was associated with a decrease in cancer screening (P = .019) and ambulatory costs (P < .001). Higher case-mix severity was related to higher ambulatory costs (P = .002).
Multivariate regression revealed statistically significant associations between clinical hours and 2 of the 4 outcomes, as shown in Table 3. Part-time practice was significantly associated with higher cancer-screening rates (P = .010) and better diabetic management (P = .008). After adjusting for potential confounders, as physician appointment hours decreased 10%, the women screened for cancer increased 0.7% and diabetic examinations increased 1.1%. There was no association with patient satisfaction (P = .212) or ambulatory costs (P = .323). While the data did support the analysis of continuous data, with a minimum of 0.3 FTE, no “threshold” of performance was found. As hours (FTE) decreased, cancer screening (P = .010) and diabetic management (P = .008) rates increased. Neither patient satisfaction nor ambulatory costs were significantly influenced by physician appointment hours. The 8 independent variables explained 23% of the variation in cancer screening rates while they explained only 5% of the variation in diabetic management. Measures considered in this study did not predict patient satisfaction (R2 = .003). However, the 8 control measures provided the most explanatory power for ambulatory costs, at 42% of the variation. Despite the selection of variables to limit multicolinearity within equations, the confounding presence of correlated variables required care in interpretation of results. Therefore, regression results, with and without FTE in each equation, were examined and no significant differences were found.
Table 3.
| Outcome Measure | β Coefficient‡ | Confidence Interval | Significance | N |
|---|---|---|---|---|
| Cancer screening (% screened) | −0.073 | (−.116 to −0.030) | 0.010§ | 186 |
| Diabetic management (% examined, tested) | −0.107 | (−.186 to −0.029) | 0.008| | 186 |
| Patient satisfaction (% rating excellent) | −0.052 | (−.133 to 0.030) | 0.212 | 186 |
| Ambulatory costs ($ per member per month) | −4.192 | (−12.54 to 4.16) | 0.323 | 171 |
Physician appointment hours as a continuous independent variable ranging from 3.5 to 35 hours or .30-1.00 full-time equivalent (FTE).
Each regression controlled for: physician gender, administrative hours, and professional years; patient panel adjusted size, case mix, age, and % female; and quadratic and interaction terms (if significant).
Inverse change in outcome per FTE. As hours decreased, outcome measures increased.
P < .05
P < .01
DISCUSSION
Not only was there no reduction in patient outcomes associated with reduced clinical hours, quality of care—as measured by cancer screening and diabetic management—was slightly higher among physicians working fewer hours (down to 0.3 FTE). This finding is consonant with 2 of the 3 recent empirical studies of physician performance directly assessing the impact of work hours.4,12,13 Murray et al. defined part-time as anything under 40 hours, and found no performance differential; however, part-timers were more satisfied with their time with patients and with time for personal and family life.4 Katon et al., examining depression treatment in 4 primary care clinics, showed no difference between part-time and full-time physicians.12 The Ambulatory Medical Audit Demonstration Project defined part time as those physicians working fewer than 5 sessions while covering nights or weekends.13 This intervention to improve performance was more effective with full-time than with part-time physicians despite similar performance preintervention. Furthermore, this was the only study demonstrating any performance disadvantage associated with part-time practice, exclusively involving provision of urgent care off-hours.
This medical group had presumed a negative impact of part-time practice on both patient satisfaction and ambulatory costs (interviews conducted by Parkerton during 1999), primarily because part-time practice might be inconsistent with members' desires and therefore an organizational survival threat. While this organization had reduced some physicians' hours in the past (during enrollment decline), current hours were at the physicians' discretion. Although physicians' determination of reduced hours might influence their performance, there is no evidence from these data that physician availability measured by appointment hours contributes to patient dissatisfaction or costs.
Concerns about patient-panel variation often limit performance assessments, reduce system credibility with physicians, and place organizational emphasis upon balancing patient panels rather than improving care. Case-mix (CDS) was found to be a factor influencing ambulatory cost, explaining nearly 10% of the cost variation, consistent with other case-mix measures in ambulatory care.37 However, CDS was not associated with the other patient outcome measures.
The 3 physician characteristics (gender, administrative role, seniority) had insignificant or minimal impact on the outcomes. We found that female physicians had 5.9% higher rates of cancer screening and 7.2% higher ambulatory costs, though neither was significant after controlling for other physician and patient characteristics. An administrative role of 0.20 FTE or more, equivalent to 1 day per week, was associated with higher ambulatory costs. However, when we re-ran the analysis for the following year, after a reorganization, administrative role was no longer associated with significantly higher costs (analysis not presented here). Professional seniority was associated with ambulatory costs only to the extent that they were the lowest during the middle years of practice (4 to 15 years). This is a finding consistent both with the benefits of clinical experience and with training received after the initiation of managed care and cost controls.
Possible explanations for a positive influence of reduced hours on patient outcomes include the following:
Practice structures selected by part-timers might improve physician performance and enhance patient outcomes. These structure enhancements might include the use of mid-level practitioners, augmented nursing role, or working in teams with other physicians. Team members may be ensuring the conduct of cancer screening, or provision of retinal and foot examinations and education for diabetics. They also may make better use of organizational systems, such as computer-generated flow sheets.
There might be a performance effect, whereby physicians attempt to compensate for working reduced hours. Part-time physicians might be concerned that decreased presence would be interpreted as a lack of interest and knowledge. Therefore, they might acquire clinical knowledge on their own time, follow patients more carefully, or work more cooperatively with other staff. Despite the prevalence of part-time physicians in this setting, American physicians have been expected to work long hours.
If working fewer hours leads to higher physician satisfaction (unmeasured in this study), part-time physicians might be happier at work and experience less depleting stress.38 Thus, communication with both patients and staff might be enhanced, leading to more satisfied patients and more cooperative colleagues.
Because patient panels tend to be proportionate to the number of hours the physician is available, fewer hours result in smaller patient panels. This might make it more possible for physicians to be more conscious of the care provided to each patient.
The balance of part-time primary care physicians' time might be spent in activities that improve their skills, knowledge, or ability to communicate with patients (e.g., in teaching or parenting).
By studying physicians working within a single medical group, with common operating systems, a common primary care role, and for specified patient panels, it is possible to obtain administrative data and limit the number of potentially confounding factors. Because the HMO has incorporated these outcome measures into their goals and subjected them to internal review, the face validity of these measures was accepted. Most importantly to this endeavor, the single medical group facilitated the availability of data on multiple aspects of physician performance measured in a consistent manner. Furthermore, because physicians are the health care system's primary mode of production, assessing them across a broad spectrum of measures, complying with quality of care definitions, would comply with recommended management indicators.39
There are specific limitations to this study setting that may reduce the generalizability of results. Those limitations affecting external validity include the following. 1) The physicians work within a large, prepaid, group practice, which is not the modal form of practice in the United States. 2) The physicians review their performance data quarterly, possibly facilitating change. 3) A measure of provider satisfaction, which might have illuminated these results, was absent.39 4) The composition and roles of clinical team members was specific to the organization and might alter performance results. 5) Patient sociodemographic variables were not considered. Income and racial distributions among panels may vary, and both have been previously associated with health status and patient behavior.40 6) Ambulatory costs were composed of primary care, specialty care, pharmacy, laboratory, and radiology expenses, which included facility overhead. It is possible that cost distortion resulted from different age and size of facilities included in the overhead. Further, hospital costs were not included, but may be directly or inversely related to ambulatory costs. 7) Adaptation of the medical clinic systems over years may have occurred to support reduced hours. A practice that suddenly reduces primary care physician hours may have different short-run outcomes. 8) Finally, our measures may not fully capture the dynamics of the patient care/satisfaction process.
Threats to the internal validity of this study include the following. 1) While we observed no systematic bias in these data that would require restricting analysis to a subset of the physicians with larger numbers of patients, sample sizes were small for some physicians. 2) Only 30.4% of the physicians had at least 100 diabetic patients, the minimum suggested by Hofer et al.21 3) While there are measures of case mix other than CDS that might be superior in accounting for differences among ambulatory patients, the CDS was the only one available in the administrative data of this organization. 4) While the cancer-screening rate is both valid and reliable for middle-aged female patients, generalizing to the total adult population is limited by the lack of male patients and senior patients. 5) Aggregating component measures should increase reliability. However, if they are assessing different dimensions of care they may mask issues of performance. 6) Finally, unmeasured confounders, including physician satisfaction, might influence or explain differences between full- and part-time physicians.
The effect of part-time practice and reduced clinical hours is a line of inquiry for which further research is needed. We have not addressed issues of minimum hours for clinical competency nor system resources required to support physicians practicing at varying levels of clinical hours. Any relationship between clinical performance and reduced clinical hours could be related to unmeasured physician characteristics, changes in the availability and continuity of care, or differences in practice structure. Future research, therefore, might examine the following questions. How do part-time physicians practice effectively despite their limited availability? How is physician practice performance related to what they do with the balance of their time and their reasons for working reduced hours, other than administrative work? How does physician time commitment influence the adequacy of our supply of primary care physicians and how might we leverage the supply by permitting flexible scheduling?
Conclusions
The trend toward part-time clinical practice by primary care physicians may occur without harm to patient outcomes. That a reduction in clinical hours did not equate to a reduction in any of the 4 patient outcomes was not consistent with hypotheses. Rather than demonstrating lower performance, primary care physicians working fewer clinical hours were associated with both slightly higher cancer screening rates and better diabetic management, and with patient satisfaction and ambulatory costs similar to those of full-time physicians. Identifying the mechanisms used by physicians working fewer hours to organize their practices may be a step toward improving patient outcomes for all. Perhaps working the traditional, full-time schedule is not required to achieve positive patient outcomes.
Acknowledgments
We thank the editors and reviewers who were generous with their time and thoughtful comments. The Sandy MacColl Institute for Healthcare Improvement and Group Health Cooperative of Puget Sound leaders providing insight and data access included Matthew Handley, MD, Gary Feldbau, MD, Brian Austin, and Susan Crissman, MPH. Renee Anspach, PhD, and Carol Weisman, PhD, both of the University of Michigan, provided conceptual guidance. Thomas Rice, PhD, and Lynn Soban, MPH, of UCLA's Department of Health Services, provided editorial review.
This study received financial support from The Blue Cross Blue Shield of Michigan Foundation, Rackham Graduate School, and the Department of Health Management and Policy at the University of Michigan.
APPENDIX A
Ranges of Component Measures for Patient Outcomes*
| Measure | Range | Measure | Range |
|---|---|---|---|
| Patient satisfaction† | Excellent score‡ | Cancer screening, women | Rate |
| Friendliness and caring | 14–80% | Mammography, age 52-64 | 53–92% |
| Attention paid to patient | 20–79% | Papanicolaou test, age 21–64 | 53–88% |
| Opportunity to ask questions | 20–71% | ||
| Explanations given about care | 10–68% | Ambulatory Costs | pmpm§ |
| Support on ways to stay healthy | 14–63% | Primary care, Medicare | $36–78 |
| Time spent | 10–54% | Primary care, non-Medicare | $21–46 |
| Thoroughness and competence | 17–76% | Special care, Medicare | $37–145 |
| Special care, non-Medicare | $11–39 | ||
| Diabetic Management | Rate | Radiology, Medicare | $2–20 |
| Annual foot examination | 11–100% | Radiology, non-Medicare | $2–8 |
| Annual retinal examination | 36–90% | Laboratory, Medicare | $3–12 |
| Microalbuminuria testing | 50–100% | Laboratory, non-Medicare | $1–6 |
| Hemoglobin A1c testing | 68–100% | Pharmacy, Medicare | $22–87 |
| Pharmacy, non-Medicare | $11–56 |
Rates or costs for each physician panel.
Measured as patient-reported satisfaction with physician performance on each component; all other measures come from administrative data.
5-Point Likert scale from poor to excellent.
Pmpm = per member per month cost.
REFERENCES
- 1.Zhang P, Thran SL. Physician Socioeconomic Statistics: Profiles for Detailed Specialties, Selected States, and Practice Arrangements. 1999–2000 ed. Chicago, Ill: Center for Health Policy Research; 1999. American Medical Association, editor. [Google Scholar]
- 2.American Academy of Family Practice. Facts about Family Physicians. 1991.
- 3.American Academy of Family Practice. Facts about Family Practice. 1998.
- 4.Murray A, Safran DG, Rogers WH, Inui T, Chang H, Montgomery JE. Part-time physicians. Physician workload and patient-based assessments of primary care performance. Arch Fam Med. 2000;9:327–32. doi: 10.1001/archfami.9.4.327. [DOI] [PubMed] [Google Scholar]
- 5.Lohr KN, Vanselow NA, Detmer DE. The Nation's Physician Workforce: Options for Balancing Supply and Requirements. Washington, DC: Institute of Medicine, National Academies Press; 1996. [PubMed] [Google Scholar]
- 6.McWhinney IR. Primary care: core values. Core values in a changing world. BMJ. 1998;316:1807–9. doi: 10.1136/bmj.316.7147.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warde CM. Time is of the essence. J Gen Intern Med. 2001;16:712–13. doi: 10.1111/j.1525-1497.2001.08020.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Donaldson MS, Yordy KD, Lohr KN, Vanselow NA. Primary Care: America's Health in a New Era. Washington, DC: National Academies Press; 1996. [PubMed] [Google Scholar]
- 9.Fairchild DG, McLoughlin KS, Gharib S, et al. Productivity, quality, and patient satisfaction. J Gen Intern Med. 2001;16:663–7. doi: 10.1111/j.1525-1497.2001.01111.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anonymous. Need part time be second-rate? BMJ. 1977;2:210. [PMC free article] [PubMed] [Google Scholar]
- 11.Gibson H. Are part time doctors better doctors? BMJ. 1997;315(suppl):2–3. [Google Scholar]
- 12.Katon W, Rutter CM, Lin E, et al. Are there detectable differences in quality of care or outcome of depression across primary care providers? Med Care. 2000;38:552–61. doi: 10.1097/00005650-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Hargraves JL, Palmer RH, Orav EJ, Wright EA. Practice characteristics and performance of primary care practitioners. Med Care. 1996;34(suppl 9):67–76. doi: 10.1097/00005650-199609002-00007. [DOI] [PubMed] [Google Scholar]
- 14.AMA. Doctor Finder: American Medical Association web site; 1999. Available at: http://www.ama-assn.org/. Accessed July 18, 1999. [Google Scholar]
- 15.American Board of Medical Specialties. The Official ABMS Directory of Board Certified Medical Specialists. 31st ed. New Providence, NJ: Marquis Who's Who; 1999. [Google Scholar]
- 16.AMA. Directory of Physicians in the United States. 36 ed. Chicago, Ill: American Medical Association; 1999. [Google Scholar]
- 17.Brook RH, McGlynn EA, Cleary PD. Part 2: measuring quality of care. N Engl J Med. 1996;335:966–70. doi: 10.1056/NEJM199609263351311. [DOI] [PubMed] [Google Scholar]
- 18.Donabedian A. The definition of quality: a conceptual exploration. In: Donabedian A, editor. The Definition of Quality and Approaches to Its Assessment. Ann Arbor, Mich: Health Administration Press; 1980. pp. 3–31. [Google Scholar]
- 19.Lohr KN. How do we measure quality? Health Aff. 1997;16:22–5. doi: 10.1377/hlthaff.16.3.22. [DOI] [PubMed] [Google Scholar]
- 20.Mainous AG, III, Talbert J. Assessing quality of care via HEDIS 3.0. Is there a better way? Arch Fam Med. 1998;7:410–3. doi: 10.1001/archfami.7.5.410. [DOI] [PubMed] [Google Scholar]
- 21.Hofer TP, Hayward RA, Greenfield S, Wagner EH, Kaplan SH, Manning WG. The unreliability of individual physician “report cards” for assessing diabetes costs and quality. JAMA. 1999;282:2098–105. doi: 10.1001/jama.281.22.2098. [DOI] [PubMed] [Google Scholar]
- 22.NCQA. HEDIS 2000 List of Measures: National Committee on Quality Assurance. Available at http://www.ncqa.org/programs/hedis/h00meas.htm. Accessed June 26, 2003. [Google Scholar]
- 23.Donabedian A. Quality and cost: choices and responsibilities. J Occup Med. 1990;32:1167–72. doi: 10.1097/00043764-199012000-00008. [DOI] [PubMed] [Google Scholar]
- 24.McGlynn EA. Six challenges in measuring the quality of health care. Health Aff. 1997;16:7–21. doi: 10.1377/hlthaff.16.3.7. [DOI] [PubMed] [Google Scholar]
- 25.Scanlon DP, Chernew M. HEDIS measures and managed care enrollment. Med Care Res Rev. 1999;56(suppl 2):60–84. [PubMed] [Google Scholar]
- 26.Spoeri RK, Ullman R. Measuring and reporting managed care performance: lessons learned and new initiatives. Ann Intern Med. 1997;127:726–32. doi: 10.7326/0003-4819-127-8_part_2-199710151-00058. [DOI] [PubMed] [Google Scholar]
- 27.van den Arend IJ, Stolk RP, Krans HM, Grobbee DE, Schrijvers AJ. Management of type 2 diabetes: a challenge for patient and physician. Patient Educ Couns. 2000;40:187–94. doi: 10.1016/s0738-3991(99)00067-1. [DOI] [PubMed] [Google Scholar]
- 28.McCulloch DK, Glasgow RE, Hampson SE, Wagner E. A systematic approach to diabetes management in the post-DCCT era. Diabetes Care. 1994;17:65–9. doi: 10.2337/diacare.17.7.765. [DOI] [PubMed] [Google Scholar]
- 29.CAHPS Fact Sheet: Agency for Healthcare Policy and Research. 2001. Available at: http://www.ahrq.gov/qual/cahps. Accessed July 15, 2003.
- 30.Norusis MJ. SPSS Professional Statistics 6.1. Chicago, Ill: SPSS Inc.; 1994. [Google Scholar]
- 31.Pedhazur EJ, Schmelkin LP. Measurement, Design, and Analysis: An Integrated Approach. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc.; 1991. [Google Scholar]
- 32.VonKorff M, Wagner EH, Saunders K. A chronic disease score from automated pharmacy data. J Clin Epidemiol. 1992;45:197–203. doi: 10.1016/0895-4356(92)90016-g. [DOI] [PubMed] [Google Scholar]
- 33.Dedobbeleer N, Contandriopoulos A-P, Desjardins S. Convergence or divergence of male and female physicians' hours of work and income. Med Care. 1995;33:796–805. doi: 10.1097/00005650-199508000-00005. [DOI] [PubMed] [Google Scholar]
- 34.De Koninck M, Bergeron P, Bourbonnais R. Women physicians in Quebec. Soc Sci Med. 1997;44:1825–32. doi: 10.1016/s0277-9536(96)00292-4. [DOI] [PubMed] [Google Scholar]
- 35.COGME. Fifth Report: Women and Medicine. Rockville, MD: Council on Graduate Medical Education, U.S. Department of Health and Human Services, Public Health Services, Health Resources and Services Administration; 1995. pp. 45–6. [Google Scholar]
- 36.Schmittdiel J, Grumbach K, Selby JV, Charles P, Quesenberry J. Effect of physician and patient gender concordance on patient satisfaction and preventive care practices. J Gen Intern Med. 2000;15:761–9. doi: 10.1046/j.1525-1497.2000.91156.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Newhouse JP. Patients at risk: health reform and risk adjustment. Health Aff. 1994;13:132–46. doi: 10.1377/hlthaff.13.1.132. [DOI] [PubMed] [Google Scholar]
- 38.Linzer M, Konrad TR, Douglas J, et al. Managed care, time pressure, and physician job satisfaction: results from the physician worklife study. J Gen Intern Med. 2000;15:441–50. doi: 10.1046/j.1525-1497.2000.05239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haas JS, Cook EF, Puopolo AL, Burstin HR, Cleary PD, Brennan TA. Is the professional satisfaction of general internists associated with patient satisfaction? J Gen Intern Med. 2000;15:122–8. doi: 10.1046/j.1525-1497.2000.02219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams DR, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–86. [Google Scholar]