Abstract
OBJECTIVE
Hepatitis C virus is the most prevalent chronic blood-borne infection in the United States, typically acquired through contaminated blood products or needle sharing. We hypothesized that patients with chronic hepatitis C infection experience stigmatization independent of mode of acquisition and that it negatively affects quality of life.
DESIGN
Cross-sectional observation study.
SETTING
Specialty clinic in a tertiary referral hospital.
PATIENTS
Two hundred and ninety outpatients diagnosed with chronic hepatitis C infection and seen in a hepatology clinic. Thirty participants were excluded because of missing data.
MEASUREMENTS AND MAIN RESULTS
Patients were asked to complete a demographic profile, a semistructured interview, the Sickness Impact Profile, and the Hospital Anxiety Depression Scale. A team of two blinded coders analyzed the interviews. A total of 147 of the 257 study patients experienced stigmatization that they attributed to the disease. Women were more likely to report perceived stigmatization than men (P < .05). Age, education, professional status, and mode of infection did not influence the likelihood of stigmatization. Stigmatization was associated with higher anxiety (P < .01) and depression (P < .01), worsened quality of life (P < .01), loss of control (P < .01), and difficulty coping (P < .01). Individuals who experienced stigmatization also mentioned problems in their health care (P < .01) and work environment (P < .01) as well as with family members (P < .01).
CONCLUSION
Stigmatization is a very common emotionally burdensome experience for patients with hepatitis C, which can erode social support. As it penetrates even into the health care environment, physicians and other care providers should be aware of the existence and impact of such negative stereotyping.
Keywords: stigmatization, anxiety, depression, hepatitis C, quality of life
Hepatitis C virus (HCV) is the most prevalent chronic blood-borne infection in the United States and the leading cause of chronic liver disease.1 An estimated 3.9 million Americans are infected with hepatitis C, with 170 million persons affected worldwide.2,3 It results in cirrhosis of the liver in an estimated 20% of patients.4 Ten percent will ultimately die as a result of complications of cirrhosis, including liver failure and liver cancer, making hepatitis C an important public health concern.5 While clinicians are continually confronted with treating and referring such patients, relatively little information is available about the impact of this disease on the quality of life of infected individuals.6,7
The HCV is transmitted by needle stick injury, transfusion, or other forms of exposure to contaminated blood. As a blood-borne disease, hepatitis C is reminiscent of infection with HIV. This association is strengthened by the fact that intravenous drug abuse is a significant risk factor for contracting both diseases, something that can potentially lead to stigmatizing experiences.8
Stigmatization is defined as attitudes expressed by a dominant group which views a collection of others as socially unacceptable.9–11 It can affect the self-esteem and quality of life of the affected individuals.12,13 Certain categories of patients have been ostracized throughout history, as exemplified by individuals infected with leprosy or HIV.14,15 In the medical environment, stigmatization may cause differences in delivery or even frank denial of treatment, both of which can result in severe adverse effects for the patient.16 This can reduce a patient's ability or willingness to implement and continue demanding lifestyle changes or to follow a complicated medical treatment regimen.17,18
While the association between this illness and intravenous drug use may lead to stigmatization, no study has explored the prevalence and consequences of such stereotyping on the quality of life in patients with HCV. We hypothesized that (1) patients with chronic hepatitis C infection commonly experience stigmatization, and (2) that it is associated with a lower quality of life, with an increase in feelings of anxiety and depression, and with a deterioration of social support. We explored this hypothesis by integrating qualitative themes with demographic information, survey results, and clinical variables.
METHODS
Patients
We enrolled patients with chronic hepatitis C infection attending the liver clinic at the University of Iowa between October 1998 and May 2001. A trained assistant asked them at the time of their clinic visit to participate in an extensive interview and to complete health-oriented questionnaires. After obtaining informed consent, we noted age, gender, race, education, employment level, and likely mode of acquisition of HCV. We excluded patients if they were younger than 18 years of age, considered legally incompetent, prisoners, unable to communicate verbally, or pregnant. Only patients who completed all aspects of the study were included in the final analysis. The University of Iowa's Institutional Review Board had approved the study.
Structured Interview
A trained assistant conducted the semistructured interview in an environment that assured privacy. The interviews, comprised of 24 questions and structured follow-up responses, ranged in length between 20 minutes and 2 hours, with a mean time of 50 minutes (Appendix 1). The interview addressed questions related to the patient's quality of life, perception of self, experiences with stigmatization, social interactions at work, home, and in the health care environment, and stressors and changes in the patient's life attributed to the disease. The interviewer recorded responses with a hand-held tape recorder and transcribed verbatim. We removed all identifiers and demographic information from the transcribed interviews.
Coding
The frequency and types of stigmatizing themes were determined through qualitative methods.19 Drawing on Crabtree and Miller's “quasi-statistical” typology, the analysis began by generating a code book.20 Twenty trained interviewers, each with more than 1 year of experience in interviewing, read 50 randomly selected texts from 150 transcribed interviews and ranked the top 10 themes. Two trained coders and the primary investigator synthesized the list of topics and constructed a master code book related to quality of life, social interaction, and stigmatization. It contained ordinal scales for each topic in order to note the intensity as well as the frequency of its use.
Employing Atlas.ti (Scolaris, Berlin, Germany), a qualitative analysis software package, a team of two trained coders independently assessed each interview. The coders attended a 3-week training course before the analysis began and worked for the entire duration of the project. Differences between coders were processed until 100% agreement was attained between them, and a master databank was developed. We used the coders’ initial coding spreadsheets to determine a final kappa score demonstrating the agreement between the evaluators before the final agreement step began.
Stigmatization Codes
We operationally defined stigmatization as (1) being negatively judged by others and (2) as a result of the patient's HCV infection. Patients who had negative self-thoughts about contracting the disease but who had not experienced pejorative judgments from others were not categorized as stigmatized. Further criteria for distinguishing mild, moderate, and severe stigmatization were developed for coding (Appendix 2).
Questionnaires
After the interview, we asked patients to fill out the Sickness Impact Profile (SIP), a well-validated health status survey, containing 12 major categories, with a subtotal for both psychosocial and physiological status.21 Patients also completed the Hospital Anxiety Depression Scale (HAD), a validated screening tool for the assessment of depressive and anxious emotional disturbances.22
Cause and Stage of Hepatitis C
All patients also underwent a detailed history and physical examination as part of their routine clinic visit. Suspected risk factors for the acquisition of the hepatitis C infection were identified by interview and chart review. All patients carried the diagnosis of hepatitis C based on antibody testing and demonstration of viral RNA in serum or whole blood. At the time of their clinic visit, alanine aminotransferase (ALT), albumin, and the prothrombin time (PT) were obtained through a routine blood test.
Statistical Evaluation
All statistical analyses were performed using GB-STAT 6.0 software (Dynamic Microsystems, Inc. Silver Spring, MD). Unless otherwise indicated, data are given as mean and 95% confidence intervals. To determine whether the frequency of stigmatization differed between stigmatized and nonstigmatized subgroups, comparisons with the C2 statistic were performed. To assess the associations between the experience of stigmatization and differences in quality of life, the HAD scores and the psychosocial subscores of the SIP were compiled and compared between those who did and those who did not report such experiences. These assessments and additional analyses on the previously defined subgroups were performed using the t test for unpaired variables and analysis of variance, as appropriate. P < .05 was considered statistically significant.
Conflict of Interest
No conflict of interest exists that would in any way affect the accuracy of the data published here.
RESULTS
Patients’ Characteristics
Between October 1998 and May 2001, 359 patients were approached to enroll in the study. Sixty-nine patients (19.2%) declined owing to time limitations or involvement in other research protocols, leaving 290 subjects. Thirty-three of these patients (9.2%) were excluded because of incomplete data. There were no significant differences in the characteristics between the subjects who refused, those who were excluded, and the patients included in the study (Table 1). In addition, we compared our study group with the data for the entire outpatient population evaluated and treated for HCV infection at the University of Iowa during the duration of the study (Table 1). Age and sex did not differ between our sample and the population, arguing against a significant selection bias owing to our sampling method. A total of 141 persons (55%) had contracted the disease as a result of using illicit drugs or shared needles. The remaining patients had contracted the virus through needle stick injuries (3%), exposure to blood products (14%), potential sexual contact (3%), or some route unrelated to substance abuse, but that remained unknown (25%). Only one patient had also been infected by HIV through contaminated blood products.
Table 1.
Baseline Characteristics of Patients with Known Hepatitis C Infection
| Study Group | Excluded Group | Refused Group | Clinic Pop. | P Value | |
|---|---|---|---|---|---|
| Patients, N | 257 | 33 | 69 | 1,292 | |
| Women % | 37 | 38 | 39 | 40 | .37 |
| Age, years, % | 45.0 | 46.1 | 46.2 | 44.8 | .67 |
| 95% CI | 43.9 to 46.1 | 42.5 to 49.7 | 44.1 to 48.3 | 44.2 to 45.6 | |
| No prior therapy, % | 28 | 38 | .14 | ||
| ALT (U/L) | 75.5 | 59.6 | .35 | ||
| 95% CI | 64.6 to 84.4 | 35.3 to 83.9 | |||
| Albumin (g/dL) | 4.2 | 4.0 | .25 | ||
| 95% CI | 4.13 to 4.27 | 3.77 to 4.23 |
CI, confidence interval; ALT, alanine aminotransferase; Pop, population.
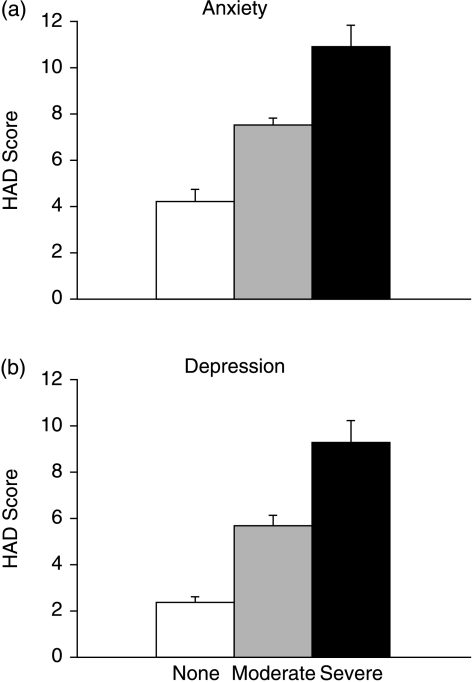
Reliability and Crossvalidation of Qualitative Data
To assess the reliability of data obtained from the qualitative analysis of patient interviews, we determined the initial agreement between coders. The total mean κ-value of 0.82 and the κ-value of 0.84 on the ordinal code of “stigmatization” demonstrates what Landis and Koch23 define as “near perfect” agreement between coders (Table 2). To validate the qualitative coding extracted from the interviews, we compared the numerical score of HAD for anxiety and depression with the severity of emotional disturbance, as judged qualitatively within the interview (Fig. 1).
Table 2.
Qualitative Codes and Intercoder Reliability
| Coding Category | Intercoder κ |
|---|---|
| Experiences of stigmatization | 0.84 |
| Feelings of depression or sadness | 0.84 |
| Feelings of anxiety and worrying | 0.73 |
| Relationships with family | 0.72 |
| Relationships with doctors | 0.74 |
| Comparison of diagnosis to HIV/AIDS | 0.93 |
| Blamed for sexual promiscuity and HCV diagnosis | 0.90 |
| Blamed for substance abuse and HCV diagnosis | 0.89 |
| Relationship in work environment | 0.83 |
| Ability/inability to cope | 0.81 |
| Feeling in/out of control | 0.85 |
| Negative/positive outlook | 0.70 |
| Total | 0.82 |
HCV, hepatitis C virus.
FIGURE 1.
Correlation between qualitative and quantitative data for anxiety and depression. Patients’ expressions of anxiety (a) and depression (b) coded qualitatively as none (□), moderate (▒), or severe (▪). Numeric score for anxiety or depression was obtained using the Hospital Anxiety Depression Scale (HAD). The coding of interview data reflects the severity of anxiety and depression as assessed by the HAD (P < .01).
Stigmatization and Hepatitis C
A total of 147 participants (57%) experienced stigmatization attributable to the disease. While age, biochemical markers of liver injury and function, educational background, and mode of acquisition did not differ significantly between the stigmatized and the nonstigmatized, women were more likely to report stigmatizing experiences than men (Table 3). The only patient with concomitant HCV and HIV infection, a hemophiliac who had acquired the diseases through contaminated blood products, did not report stigmatization.
Table 3.
Social and Demographic Variables and Stigmatization in Patients with Hepatitis C Infection
| No Stigmatization | Stigmatization | P Value | |
|---|---|---|---|
| Patients, N | 110 | 147 | |
| Women, % | 31 | 43* | <0.05 |
| Age years, % | 45.8 | 44.0 | 0.12 |
| 95% CI | 43.7–47.9 | 42.7–45.3 | |
| Mode of acquisition, % | |||
| Blood products | 10 | 15 | 0.24 |
| IV drug use | 54 | 55 | 0.82 |
| Education, % | |||
| High school degree | 47 | 35 | 0.06 |
| Some college | 32 | 38 | 0.3 |
| College degree | 12 | 12 | 0.92 |
| Masters or doctoral degree | 9 | 16 | 0.09 |
| Professional background, % | |||
| Unemployed | 5 | 3 | 0.1 |
| Disabled | 6 | 3 | 0.09 |
| Part-time employment | 9 | 5 | 0.17 |
| Full-time employment | 70 | 79 | 0.1 |
| Homemaker | 4 | 5 | 0.94 |
| Retired | 6 | 5 | 0.58 |
Significant results. CI, confidence interval; IV, intravenous.
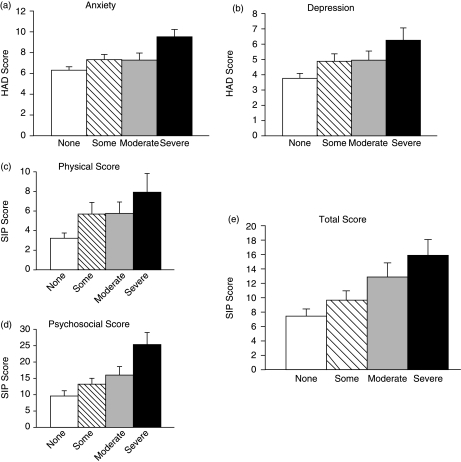
Stigmatization was associated with an increase in emotional problems. Using the ordinal scale for the perceived severity of stigmatization, there was a significant relationship between stigmatization and the anxiety and depression scores as determined by the HAD (Fig. 2). This is consistent with the psychosocial subscale of the SIP, which also showed a progressive worsening of the patient's emotional/interpersonal state as stigmatization increased (Fig. 2).
FIGURE 2.
Correlation between severity of stigmatization and the Hospital Anxiety Depression Scale (HAD) and Sickness Impact Profile (SIP). The mean HAD scores for anxiety (a) and depression (b) compared for patients who experienced none (□), mild (hatched bars), moderate (▒), or severe (▪) stigmatization. The HAD scores increased significantly with worsening experience of stigmatization for anxiety (P < .05) and depression (P < .01). The mean SIP scores for physical (c), psychosocial (d), and the total SIP score (e) compared for patients who experienced none (□), mild (□), moderate (▒), or severe (▪) stigmatization. While the psychosocial score differed significantly between the groups (P < .01), the physical and total scores were not statistically different dependent on the severity of experienced stigmatization (P > .1).
Qualitatively, an experience of stigmatization was found to be associated with a weakened resolve to optimistically face the future (negative outlook: 15% vs 40%, control vs stigmatized, respectively; P < .01), a sense of having lost control (19% vs 60%, control vs stigmatized, respectively; P < .01), problems coping with the disease and its consequences (14% vs 48%, control vs stigmatized, respectively; P < .01), expressions of anxiety (56% vs 82%, control vs stigmatized, respectively; P < .01), and depression (28% vs 65%, control vs stigmatized, respectively; P < .01).
Perceived Causes of Stigmatization
Patients most commonly articulated three themes in explaining why they felt stigmatized: society's association of hepatitis C with HIV/AIDS, promiscuity, and substance abuse. Thirty of the patients (12%) felt stigmatized because most lay people did not differentiate between having HCV and HIV/AIDS. “It's hard sometimes because when people find out it's like ‘Oh, she's got AIDS.’ I literally wanted to kill myself because a lot of my friends just backed off.” In addition, given the public's perception about HIV/AIDS, an association has been drawn in the general population between HCV and sexual promiscuity. Twenty-one patients (8%) had experienced stigmatization because of this negative association: “It's not my fault. I wasn’t out having sex with a bunch of people. I’m not promiscuous.” Furthermore, 22 patients (9%) felt stigmatized because of the connection forged between HCV and intravenous drug use: “The image to everyone was ‘you must shoot up drugs’—because society does have that stigma attached to it. And that wasn’t the case.”
Stigmatization within the Health Care Setting
Patients explained that they also felt stigmatized by health care workers. Sixty percent of the stigmatized patients experienced problems in the health environment, as opposed to 40% of patients who did not feel stigmatized (P < .01). Patients felt directly stigmatized by their physicians who they believed viewed their HCV infection with prejudice and suspicion. Patients who were health care workers specifically mentioned the medical environment as the area where they experienced the most stigmatization: “They actually took me out of the nursing program I was in and would not let me do an OB rotation. I had to threaten to sue them to let me complete the program.”
Stigmatization and the Work Environment
Twenty-six percent of the study participants had experienced problems in their interactions with colleagues and coworkers in their professional lives. A significant difference in perception of the workplace emerged between those who experienced stigmatization versus those who did not (1% vs 44%, control vs stigmatized, respectively; P < .01). This was also reflected in reported changes in employment or professional status. Prior to the diagnosis of the disease, 12% of all hepatitis C participants were listed as unemployed or disabled (13% vs 9%, control vs stigmatized, respectively; P = .32, not significant). This number increased to 29% after hepatitis C had been diagnosed (21% vs 33% for control group vs stigmatized group, respectively; P < .01 for increased compared to baseline, P < .05 for comparison between the groups). Patients shared specific examples of being stigmatized in the work environment because of their disease: “They tell me that I need to go home until they figure out what this hepatitis C is, if it's contagious. And then they went so far as to put covers in the bathroom. They didn’t want me drinking out of the water fountain.”
Stigmatization and Familial Relationships
Hepatitis C patients experienced hardships within their own families as well. For those who experienced stigmatization, 48% felt left alone or pushed aside by their families compared with 10% of the other patients (P < .01). Stigmatizing circumstances generally revolved around issues of contamination and abandonment: “My family is afraid of me. I was invited to go camping.[participant cries in interview.]They asked me to get my own tent. Now they won’t have me in their house because they’re afraid they might get it.”
DISCUSSION
Using an analysis of patient interviews, this study demonstrates a high prevalence of stigmatization in individuals infected with the HCV. The patients’ words provide powerful testimony to the tremendous impact of negative stereotyping on quality of life. However, we attempted to go beyond anecdotal accounts of traumatic experiences. We instead employed a novel approach toward integrating and crossvalidating qualitative and quantitative data that relied on well-defined inclusion–exclusion criteria, quality controls at various levels to assure the validity of interpretations, and crossvalidation with quantitative survey data.24 With this combination of methods, we were able to qualitatively examine the concept of stigmatization, its association with clinical and demographic variables, and its potential causes as articulated by the patients themselves.25
While this is the first study, to our knowledge, to define levels of stigmatization in this patient population, others have previously investigated stereotyping in various disease groups. Patients with HCV infection face negative stereotyping nearly as often as persons infected with HIV.26 Both HIV and HCV infection share risk factors and are associated with marginalized or even criminal behavior, which may account for some of the similarities. In both cases, fears of contracting a potentially lethal disease may also contribute to the common prejudicial attitudes. Based on these considerations, it is not surprising that patients infected with HIV or HCV face higher degrees of stigmatization than individuals with other chronic diseases.27 Such experiences, and the assumption that diagnoses such as HIV infection will trigger negative reactions, can lead to secrecy, fueled by the fear of discrimination and concerns related to disruption of familial and professional relationships.28,29
Previously published work showed a similar impact of stigmatization in mentally ill individuals. One study consistently found stigmatization leading to isolation, anxiety, and poor coping with the disease.30 During follow-up, patients frequently expressed feelings of rejection, self-depreciation, and a weakened “sense of mastery,” feelings that persisted even when the underlying psychiatric problem itself had improved.31–33 In our study, problems with coping were apparent in the high percentage of patients with hepatitis C who expressed a sense of helplessness, loss of control, and the prospect of a bleak future. The parallels between patients with very different illnesses points to stigmatization as an important contributor to such difficulties in adjusting to life with and treatment of a disease.
We also found a correlation between stigmatization and problems in the professional lives of patients, further increasing the burden of the disease. While little is known about the likelihood of discrimination in patients with chronic liver disease, prior studies have demonstrated a relationship between popular conceptions of a disease and problems patients encounter in the professional sphere.34,35
In addition, many individuals spoke of significant problems within the private sphere. Estrangement from family was associated with a decrease in social support, thereby potentially further interfering with their ability to cope with the disease. Similar results were found in studies of patients with HIV/AIDS and tuberculosis, where patients expressed the feeling of being shunned by those to whom they felt closest.36,37 Such experiences result in adverse effects on well-being, as expressed by many of the patients interviewed here or as reported in the literature.38
While hepatitis C plays an important role in triggering fears and concerns, psychosocial problems may, in some individuals, result from preexisting personality traits that can lead to risk-taking behavior and which may have resulted in the acquisition of hepatitis C.39 However, the likelihood of experiencing stigmatization did not correlate with differences in the mode of acquisition, indicating that emotional problems cannot be simply explained by drug abuse and the associated personality and psychosocial problems. Rather, such feelings were more clearly associated with negative stereotyping, as we noted significant differences in all of these topics between those who did experience stigmatization compared to those who did not.
Interestingly, women were more likely to report stigmatization than men. Very little is known about the influence of gender on the likelihood of negative stereotyping. Studies with disfiguring diseases, such as leprosy, suggest that the distorted body image increases the perceived or actual frequency of stigmatizing experiences.14,40 The acquisition of a potentially contagious disease violates the image of women and mothers as protectors of innocent and helpless infants, thereby marginalizing female patients with HIV or other infections.15,41 More studies are required to determine whether and how patients’ sex affects social interactions between patients and their environment.
Stigmatization not only affects the individual, it also directly impacts the treatment of the disease. Health care workers are not immune to prejudicial views related to disease. Therefore, stereotyping can function as a significant barrier to treatment.42 As a result of such experiences, individuals may resort to secrecy in an attempt to avoid the label of a disease.43 Such secrecy, in turn, may result in further withdrawal and social isolation or may prevent individuals from seeking medical help.44
The study relied on information abstracted from lengthy patient interviews. While this process is a potential source of bias, we controlled for the quality of these data by using intercoder reliability measures and correlating the qualitative and quantitative results. The sample size and these internal and external validity checks allow conclusions that go beyond those obtained by many other studies relying on such extensive interviews. The patients included are representative of the patient population with hepatitis C seen at a tertiary referral center in the more rural Midwest. However, additional investigations are needed to determine whether patients in metropolitan areas or ethnically more diverse regions similarly experience stigmatization. It is conceivable that a referral center attracts a disproportionate fraction of patients with psychosocial problems who are willing to travel longer distances for their medical care. Yet interestingly, neither the size of the town of origin nor the distance to the University of Iowa correlated with the experience of stigmatization. These results and the importance of the University of Iowa Health Care as the main provider of specialized antiviral therapy in this patient population within the region argue against significant distortion resulting from referral bias.
More than half of the patients experienced stigmatization. This key finding clearly highlights the need to discuss such problems with patients and their families. Our results also demonstrate the need for broad-based educational efforts to increase the popular understanding of diseases associated with pejorative stereotypes. These efforts should include health care providers, who may also be affected in their judgment by widespread misconceptions about illnesses such as hepatitis C. Additional studies using qualitative methods or surveys will be needed to determine whether a similar prevalence of stigmatizing experiences can be found in patients attending other specialty or primary care clinics. Moreover, it will be important to assess whether supportive and educational interventions can lessen the emotional burden associated with the disease and improve the quality of life of patients.
The authors thank Nicole Taylor for administrative assistance and Vicki Hudachek for secretarial help.
Grant support: Central Investment Fund for Research Enhancement, 2001, University of Iowa.
APPENDIX 1
Interviewing Questions
| (1) | Can you tell me what your condition is exactly? What physical limitations do you have and when were you initially diagnosed? |
| (2) | Could you tell us a little bit about yourself: the things you’ve done, your roles in life, who you are? What in your life are you most proud of? |
| (3) | Can you share with us anything specific that might have caused or helped cause your illness? |
| (4) | Have any of your family members had similar health problems? Does this family history worry you? |
| (5) | What impact has your physical condition had on the quality of your life? Would you say that your quality of life as compared with 1 year ago is better, about the same, or worse? |
| (6) | As you go through this experience, have you begun to think about yourself differently? |
| (7) | What has been the hardest thing for you to cope with related to this experience? How do you go about coping with your condition? |
| (8) | How does this illness make you feel emotionally? If there was one emotion that you would use to express how you feel, what would that be? |
| (9) | Since you were diagnosed, what would you say has been your biggest regret? Would you say you feel emotionally worse since you were diagnosed, about the same as before, or emotionally better off than before? |
| (10) | Can you share what health-related worries you have? Do you worry more about your health than you do other aspects of your life? Did you share these worries with your doctor or nurse? |
| (11) | How would you describe your outlook or thoughts as you look to the future? |
| (12) | What are the various things that make your life meaningful for you? What do you turn to when you are in need of strength? |
| (13) | We are interested in the impact this illness has had on your relationships: |
| • | If you were in a crisis, who would you turn to? |
| • | Do you have a spouse or significant other? How has that person reacted to your situation of being ill? When you think about when you were healthy, would you describe the two of you as closer, somehow further part, or just as close as you always were? |
| • | Can you describe the level of support you can find in your family? Can you explain why are you able or not able to rely on your family to help you through difficult times? |
| • | Would you say that you are close to others outside of your family? Why would you say that? What about coworkers, are they understanding and supportive? |
| (14) | Have you encountered any negative judgments from others because of your disease? If yes, can you say who has made you feel this way and under what circumstances? |
| (15) | How has your disease affected your sense of control in your life? What are the situations where you feel you’re not in control? |
| (16) | What has been your experience with your doctors here or elsewhere? Would you describe it as positive or negative and what has made it positive or negative? What in your eyes makes a good doctor? |
| (17) | Do you feel that you can ask your doctor or nurse any question? Do you worry that you may be taking their time with your concerns? |
| (18) | Where do you get most of your medical information? Is there a source you tend to rely or believe in the most? In general, are there other things about your health condition that you would like to learn from your doctor? |
| (19) | What is the most difficult part of following the treatment the doctor recommended for you? Can you describe situations where you are unable to follow the doctor's treatment, such as taking your medicines, watching your diet, or exercising? |
| (20) | Did you feel comfortable with your treatment decisions? Do you feel you had choices in your treatment and that they were respected? Who did you discuss your treatment decisions with; what really helped you to make up your mind? |
| (21) | Do you use other or supplemental, herbal, or alternative medicines, and if yes, what are those? |
| (22) | If you were to describe yourself as something—it can be anything in this world—an object, an animal, anything—before when you were healthy and now, what two things would you choose? |
| (23) | Is there anything else that you would like to add that would help us to understand your experience? |
| (24) | Finally, is there anything you would like us to share with a social worker, a pastor, or your health care team about the way you are feeling? |
APPENDIX 2
Rating Criteria for Coding Stigmatization
| (1) | If the interview did not allow for an assessment of stigmatization, the code cannot judge was used and the data were not included in the final analysis (n = 20). |
| (2) | No stigmatization: If patient answered negatively to the stigmatization question, mentioned no additional stigmatizing experience during course of interview. |
| (3) | Mild stigmatization: Patient recounts at least one minor stigmatizing incident during course of interview. Example: “This agency had a woman refuse to come help me because I have hepatitis C.” |
| (4) | Moderate stigmatization: Patient recounts recurring or emotionally intense experience of stigmatization during course of interview: Example: “Prejudice? Yes, from work. Bosses, they would not allow me to work because they did not have a clear understanding. I had one girl even tell a group of girls at work that Hep C was the beginning of AIDS.” |
| (5) | Severe stigmatization: Patient recounts extensive experience with stigmatization or has very strong emotional reaction: “If I do lose my boyfriend then I’m going to be alone. No one's going to want to be involved with a person with hepatitis. When my daughter found out she was very paranoid and didn’t want me to touch the kids or give ’em a kiss. That was real hard, being pushed aside as an outcast.” |
REFERENCES
- 1.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556–62. doi: 10.1056/NEJM199908193410802. [DOI] [PubMed] [Google Scholar]
- 2.Gebp KA, Jenckes MW, Chander G, et al. Management of Chronic Hepatitis C. Evidence Report/Technology Assessment no. 60. Rockville, MD: Agency for Healthcare Research and Quality; 2002. AHRQ Publication no. 02-E030. [Google Scholar]
- 3.Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med. 2001;345:41–52. doi: 10.1056/NEJM200107053450107. [DOI] [PubMed] [Google Scholar]
- 4.Seeff LB. The natural history of chronic hepatitis C virus infection. Clin Liver Dis. 1997;1:587–602. doi: 10.1016/s1089-3261(05)70323-8. [DOI] [PubMed] [Google Scholar]
- 5.Wong JB, McQuillan GM, McHutchison JG, Poynard T. Estimating future hepatitis C morbidity, mortality, and costs in the United States. Am J Public Health. 2000;90:1562–9. doi: 10.2105/ajph.90.10.1562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh N, Gayowski T, Wagener MM, Marino IR. Vulnerability to psychologic distress and depression in patients with end-stage liver disease due to hepatitis C virus. Clin Transplant. 1997;11:406–11. [PubMed] [Google Scholar]
- 7.Mulder RT, Ang M, Chapman B, Ross A, Stevens IF, Edgar C. Interferon treatment is not associated with a worsening of psychiatric symptoms in patients with hepatitis C. J Gastroenterol Hepatol. 2000;15:300–3. doi: 10.1046/j.1440-1746.2000.02090.x. [DOI] [PubMed] [Google Scholar]
- 8.Schafer M, Boetsch T, Laakmann G. Psychosis in a methadone-substituted patient during interferon-alpha treatment of hepatitis C. Addiction. 2000;95:1101–4. [PubMed] [Google Scholar]
- 9.Scrambler G. Stigma and disease: changing paradigms. Lancet. 1998;352:1054. doi: 10.1016/S0140-6736(98)08068-4. [DOI] [PubMed] [Google Scholar]
- 10.Goffman E. Stigma: Notes on the Management of Spoiled Identity. New Jersey: Prentice Hall; 1963. [Google Scholar]
- 11.Crandall CS. Ideology and lay theories of stigma: the justification of stigmatization. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The Social Psychology of Stigma. New York, NY: Guilford Press; 2000. pp. 126–50. [Google Scholar]
- 12.Crocker J, Quinn DM. Social stigma and the self. meaning, situations, and self-esteem. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The Social Psychology of Stigma. New York, NY: Guilford Press; 2000. pp. 153–83. [Google Scholar]
- 13.Miller CT, Major B. Coping with stigma and prejudice. In: Heatherton TF, Kleck RE, Hebl MR, Hull JG, editors. The Social Psychology of Stigma. New York, NY: Guilford Press; 2000. pp. 243–72. [Google Scholar]
- 14.Morrison A. A woman with leprosy is in double jeopardy. Lepr Rev. 2000;71:128–43. doi: 10.5935/0305-7518.20000016. [DOI] [PubMed] [Google Scholar]
- 15.Ingram D, Hutchinson SA. HIV-positive mothers and stigma. Health Care Women Int. 1999;20:93–103. doi: 10.1080/073993399245999. [DOI] [PubMed] [Google Scholar]
- 16.Gardner JR, Sandhu G. The stigma and enigma of chronic non-malignant back pain (CNMBP) treated with long-term opioids. Contemp Nurse. 1997;6:61–6. doi: 10.5172/conu.1997.6.2.61. [DOI] [PubMed] [Google Scholar]
- 17.Hajela R. The stigma facing drug abusers impedes treatment. Can Med Assoc J. 1998;158:1265–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Chesney MA, Smith AW. Critical delays in HIV testing and care: the potential role of stigma. Am Behav Sci. 1999;42:1162–74. [Google Scholar]
- 19.Dey I. Qualitative Data Analysis: A User-Friendly Guide for Social Scientists. London: Routledge; 1993. [Google Scholar]
- 20.Miller W, Crabtree BF. Primary care research: a multi typology and qualitative road map. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. London: Sage Press; 1992. pp. 23–8. [Google Scholar]
- 21.Pollard WE, Bobbit RA, Bergner M, Martin DP, Gilson BS. The sickness impact profile: reliability of a health status measure. Med Care. 1976;14:146–55. doi: 10.1097/00005650-197602000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Dagnan D, Chadwick P, Trower P. Psychometric properties of the Hospital Anxiety Depression Scale with a population of members of a depression self-help group. Br J Med Psychol. 2000;73:129–37. doi: 10.1348/000711200160255. [DOI] [PubMed] [Google Scholar]
- 23.Landis J, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 24.Barbour RS. Mixing qualitative methods: quality assurance or qualitative quagmire? Qual Health Res. 1998;8:352–61. doi: 10.1177/104973239800800306. [DOI] [PubMed] [Google Scholar]
- 25.Morse JM. Determining sample size. Qual Health Res. 2000;10:3–5. [Google Scholar]
- 26.Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. 2000;41:50–67. [PubMed] [Google Scholar]
- 27.Busza JR. Promoting the positive: responses to stigma and discrimination in Southeast Asia. AIDS Care. 2001;13:441–56. doi: 10.1080/09540120120057978. [DOI] [PubMed] [Google Scholar]
- 28.Jorgensen MJ, Marwit SJ. Emotional support needs of gay males with AIDS. AIDS Care. 2001;13:171–5. doi: 10.1080/09540120020027332. [DOI] [PubMed] [Google Scholar]
- 29.Serovich JM, Brucker PS, Kimberly JA. Barriers to social support for persons living with HIV/AIDS. AIDS Care. 2000;12:651–62. doi: 10.1080/095401200750003824. [DOI] [PubMed] [Google Scholar]
- 30.Link BG, Elmer L, Struening MR, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38:177–90. [PubMed] [Google Scholar]
- 31.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatization of people with mental illnesses. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 32.Wright ER, Gronfein WP, Owens TJ. Deinstitutionalization, social rejection, and the self-esteem of former mental patients. J Health Soc Behav. 2000;41:68–89. [PubMed] [Google Scholar]
- 33.Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, causes, dangerousness, and social distance. Am J Public Health. 1999;89:1328–33. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39:335–48. [PubMed] [Google Scholar]
- 35.Glozier N. Workplace effects of the stigmatization of depression. J Occup Environ Med. 1998;40:793–800. doi: 10.1097/00043764-199809000-00008. [DOI] [PubMed] [Google Scholar]
- 36.Kadushin G. Gay men with AIDS and their families of origin: an analysis of social support. Health Soc Work. 1996;21:141–9. doi: 10.1093/hsw/21.2.141. [DOI] [PubMed] [Google Scholar]
- 37.Kelly P. Isolation and stigma: the experience of patients with active tuberculosis. J Community Health Nurs. 1999;16:233–41. doi: 10.1207/S15327655JCHN1604_3. [DOI] [PubMed] [Google Scholar]
- 38.Pierret J. Everyday life with AIDS/HIV: surveys in the social sciences. Soc Sci Med. 2000;50:1589–98. doi: 10.1016/s0277-9536(99)00467-0. [DOI] [PubMed] [Google Scholar]
- 39.Paterson DL, Gayowski T, Wannstedt CF, et al. Quality of life in long-term survivors after liver transplantation: impact of recurrent viral hepatitis C virus hepatitis. Clin Transplant. 2000;14:48–54. doi: 10.1034/j.1399-0012.2000.140109.x. [DOI] [PubMed] [Google Scholar]
- 40.Aziz H, Akhtar H. Epilepsy in Pakistan: stigma and psychosocial problems: a population-based epidemiologic study. Epilepsia. 1997;38:1069–73. doi: 10.1111/j.1528-1157.1997.tb01195.x. [DOI] [PubMed] [Google Scholar]
- 41.Feiring C, Taska L. A process model for understanding adaptation to sexual abuse: the role of shame in defining stigmatization. Child Abuse Negl. 1996;20:767–82. doi: 10.1016/0145-2134(96)00064-6. [DOI] [PubMed] [Google Scholar]
- 42.Corley MC, Goren S. The dark side of nursing: impact of stigmatizing responses on patients. Sch Inq Nurs Pract. 1998;12:99–118. [PubMed] [Google Scholar]
- 43.Troxell J. Epilepsy and employment: the Americans with Disabilities Act and its protections against employment discrimination. Med Law. 1997;16:375–84. [PubMed] [Google Scholar]
- 44.Oliva G, Rienks J, McDermid M. What high-risk women are telling us about access to primary and reproductive health care and HIV prevention services. AIDS Educ Prev. 1999;11:513–24. [PubMed] [Google Scholar]