Abstract
OBJECTIVE
Prior studies have shown that 60% to 75% of adults with upper respiratory tract infections want antibiotics. More recent research indicates declines in antibiotic prescribing for upper respiratory tract infections. To investigate whether there has been a comparable decrease in patients’ desire for antibiotics, we measured the proportion of adults with upper respiratory tract infections who wanted antibiotics in the winter of 2001–2002. We also sought to identify factors independently associated with wanting antibiotics and antibiotic prescribing.
DESIGN
Prospective survey of adults with upper respiratory tract infections prior to visiting an acute care clinic from November 2001 to February 2002.
MEASUREMENTS AND MAIN RESULTS
Thirty-nine percent of 310 patients wanted antibiotics. Many patients wanted relief from symptoms (43%) or pain (24%) and many patients expected to receive a diagnosis (49%) or reassurance during the visit (13%). In multivariable modeling, independent predictors of wanting antibiotics were prior antibiotic use (odds ratio [OR], 2.4; 95% confidence interval [CI], 1.3 to 4.7) and current smoking (OR, 3.1; 95% CI, 1.3 to 7.3). Physicians prescribed antibiotics to 46% of patients who wanted antibiotics and 29% of patients who did not want antibiotics (P= .01). In multivariable modeling, wanting antibiotics was an independent predictor of antibiotic prescribing (OR, 2.1; 95% CI, 1.1 to 4.4).
CONCLUSIONS
Only 39% of adults seeking care for upper respiratory tract infections wanted antibiotics, less than in previous studies. In continuing efforts to break the cycle of inappropriate antibiotic use, physicians should not assume that most patients with upper respiratory tract infections want antibiotics.
Keywords: antibiotics, respiratory tract diseases, physician's practice patterns
Upper respiratory tract infections are the most common reason for seeking ambulatory care in the United States.1 Although antibiotics are ineffective for most upper respiratory tract infections, antibiotic use for upper respiratory tract infections is common.2–6 Such inappropriate antibiotic use exposes patients unnecessarily to potential adverse effects,7 and increases the prevalence of antibiotic-resistant bacteria.8 Physicians are generally aware of the individual and societal adverse consequences of inappropriate antibiotic use.9 However, physicians frequently prescribe antibiotics to meet perceived patient expectations.9–11
Studies have indeed shown that many patients want antibiotics when seeking care for upper respiratory infections. Studies published or performed between 1996 and 1998 in the United States showed that 60% to 75% of adults with upper respiratory tract infections wanted antibiotics for their illness.12–14 However, these studies were performed prior to more recent research that shows antibiotic prescribing rates for upper respiratory tract infections are decreasing.15–17 It is unknown whether, in the setting of decreased antibiotic prescribing, the proportion of patients wanting antibiotics has also decreased. Additionally, it is unknown whether there has been a change in previously noted associations between prior antibiotic use and wanting antibiotics,18,19 and between wanting antibiotics and actual antibiotic prescribing.10,11
We performed a prospective survey in an acute care clinic during the winter of 2001–02 to measure the proportion of patients with upper respiratory infections who want antibiotics. We also sought to identify factors independently associated with wanting antibiotics and antibiotic prescribing.
METHODS
Patients and Setting
The study was conducted from November 27, 2001 to February 28, 2002 in the Massachusetts General Hospital Medical Walk-In Unit (Boston, Mass.). The Medical Walk-In Unit is an adult acute care clinic, open 7 days a week, where most patients are seen on a first-come, first-served basis.
At check-in, the unit secretary directed patients to a flyer that stated: “Do you have runny nose, cough, congestion or stuffiness, sore throat, ear pain, sinus pain or other symptoms that makes you think you may have pneumonia, bronchitis, sinusitis, a cold, the flu or another respiratory infection?” If the patient had respiratory symptoms, the secretary offered the patient a “Respiratory Illness Survey” to complete in the waiting room. Patients could also receive a survey by responding to flyers posted in the waiting room or by being asked by the triage nurses. The secretaries and nurses were not required to verify the presence of respiratory symptoms. Patients were not informed of the content or purpose of the study prior to being given the survey.
Surveys were filled out and returned to a lockbox in the waiting room before the patient's visit with the physician. Although efforts were made to include as many patients as possible, participation in the study was voluntary. Patients gave their consent to participate by returning a survey. No data are available concerning the demographics or diagnoses of the patients who declined participation.
Information on the survey was not available to the treating physician. Information about recorded history, physical exam findings, diagnosis, and medications prescribed was later abstracted from the chart. The Institutional Review Board of Massachusetts General Hospital approved the study protocol.
Respiratory Illness Survey
Patients answered questions about characteristics of the present illness, reason for the visit, expectations for the visit, desire for antibiotics, demographics, and comorbid illnesses. Questions were derived from prior studies.12–14,19,20 Prior to study use, clinicians and patients reviewed the questionnaire to ensure understandability.
Information about the present illness included asking about the duration of illness, whether the patient missed work due to illness, and 24 specific symptoms using yes/no questions. Patients were asked how bothered they were by the present illness on a 5-point scale, from “extremely bothered” to “not bothered.” Patients indicated their primary reason for coming to the clinic by answering the question “For your visit today, of the reasons for coming to the clinic, which one is most important to you?” With this question, we sought to understand the main goal served by getting better. Possible reasons for the visit included getting better because the symptoms are annoying, getting better because of pain, getting better to care for family, getting better to return to work, getting better for leisure time or travel, or getting better for another reason.
Patients indicated their primary expectation for the visit by answering the question “For your visit today, of the expectations below, which one is most important to you?” With this question, we sought to know what the patient wanted to happen at the visit. Possible expectations included having tests or x-rays, getting a diagnosis, getting reassurance, getting a referral, getting a nonantibiotic treatment, getting an antibiotic prescription, or getting an estimate of how long the symptoms would last.
Desire for antibiotics was assessed using a 5-point Likert scale (strongly agree to strongly disagree) in response to the statement “I want antibiotics for my illness today.” Similar response frames were used to assess whether patients felt that antibiotics work for them when they have a cold, repeated use of antibiotics could be harmful to them personally, or if they planned on asking the doctor for antibiotics.
Patients answered questions about their age, sex, primary language, race/ethnicity, education, insurance status, household income, employment status, and whether or not they had a primary care doctor they have seen before. Patients were asked the number of medicines they took, if they smoked, and if they had heart disease, lung disease, diabetes, or cancer (excluding skin cancer), or were pregnant.
Data Analysis
For the present analysis, we included patients who had a physician-assigned upper respiratory tract infection and who answered the question regarding desire for antibiotics. Because we wanted patients to respond to questions about treatment expectations prior to their visit with the doctor, we anticipated a need to exclude patients who were not given a primary diagnosis of a common upper respiratory tract infection. Included diagnoses were upper respiratory infection, viral syndrome, influenza, otitis media, sinusitis, nonstreptococcal pharyngitis, streptococcal pharyngitis, tonsillitis, infectious mononucleosis, acute bronchitis, and acute cough. Patients with influenza (3 patients) and infectious mononucleosis (1 patient) were considered to have viral syndrome; patients with cough (10 patients) were considered to have acute bronchitis. We excluded patients who reported symptoms for more than 30 days.
We dichotomized patients into those who strongly agreed with the statement “I want antibiotics for my illness today,” and those who had no opinion, disagreed, or strongly disagreed. To assess prior antibiotic use, we dichotomized patients into those who reported using, on average, zero antibiotic courses per year and those who reported using 1 or more antibiotic courses per year.
We did not evaluate diagnosis as a predictor of antibiotic prescribing. The signs and symptoms of common upper respiratory tract infections overlap and a diagnosis might be used to legitimize an antibiotic prescription. For example, if a patient has headache, myalgias, and sinus pain, and insists on an antibiotic, the physician may diagnose the patient with sinusitis—an antibiotic-appropriate diagnosis—instead of upper respiratory tract infection, for which antibiotics would be inappropriate.
Statistical Analysis
To detect a 20% absolute increase—from 40% to 60%—in antibiotic prescribing for patients who wanted antibiotics, assuming 50% of patients would want antibiotics, with Type I error of .05 and 80% power, 180 total patients would be required. Our goal was to enroll 300 total patients to account for exclusions, missing data, and loss of power using a clustered analysis.
We used standard descriptive statistics. We used Fisher's exact test, the χ2 test, the χ2 test for trend, Student's t test, and the Wilcoxon rank-sum test where appropriate.
We developed two multivariable logistic regression models. In the first model, we sought to identify independent predictors of wanting antibiotics. We evaluated any variable associated with wanting antibiotics (P≤ .1 on univariate testing) and adjusted for confounding while minimizing collinearity between variables. We considered confounding or collinearity to be present when the addition of a new variable into the model changed the beta coefficient or standard error, respectively, of another variable by more than 10%.
In the second model, we sought to determine whether wanting antibiotics was independently associated with receiving antibiotics, adjusted for clustering by provider.21 To begin the model building process, we used a forward selection algorithm to identify the strongest predictors of antibiotic prescribing. We also evaluated any other covariate associated with either wanting antibiotics or receiving antibiotics on univariate testing (P≤ .1).
All analyses were performed using SAS 8.1 (SAS Institute, Cary, NC). P values were two-tailed where possible and P values ≤ .05 were considered significant.
RESULTS
Characteristics of the Patients and Visits
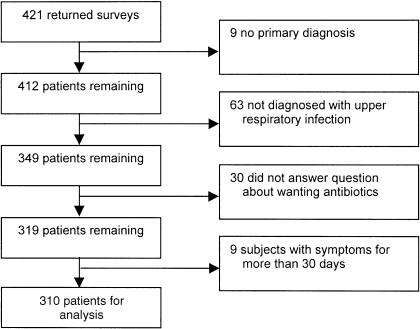
During the study period, 421 surveys were returned, representing approximately 7% of all patients presenting to the clinic for any reason. Of 421 patients who returned surveys, 310 met our inclusion and exclusion criteria (74%; Fig. 1). The most commonly excluded primary diagnoses were pneumonia (8 visits), asthma, (3) urinary tract infection, (3) conjunctivitis, (2) hypertension, (2) otitis externa, (2) and tympanic membrane perforation (2). The other 41 subjects excluded by diagnosis all had separate, unrepeated primary diagnoses.
FIGURE 1.
Exclusion and inclusion of patients.
The patients who met inclusion and exclusion criteria had a mean age of 34 years, were 64% women, and 81% white (Table 1). The subjects were generally of high socioeconomic status with 92% having attended some college and 51% having a household income greater than $50,000.
Table 1.
Characteristics of 310 Adults with Upper Respiratory Tract Infection
| Characteristic | n* | Value (%) |
|---|---|---|
| Mean age, (SD) | 310 | 34 (12) |
| Female | 310 | 197 (64) |
| Race/ethnicity | 307 | |
| White | 248 (81) | |
| Black | 21 (7) | |
| Latino | 14 (5) | |
| Asian | 18 (6) | |
| Other | 6 (2) | |
| Some college | 310 | 285 (92) |
| Insurance | 310 | |
| Private | 209 (67) | |
| Medicare | 18 (6) | |
| Medicaid | 14 (5) | |
| Hospital free care | 31 (10) | |
| Other insurance | 38 (12) | |
| Annual household income | 294 | |
| Less than $50,000 | 143 (49) | |
| More than $50,000 | 151 (51) | |
| Employed | 306 | 256 (85) |
| Primary care doctor | 305 | 220 (72) |
| Comorbidities | ||
| Diseases of heart | 306 | 20 (7) |
| Diseases of lung | 306 | 32 (10) |
| Diabetes | 303 | 3 (1) |
| Cancer† | 305 | 12 (4) |
| Number of daily medicines, median (interquartile range) | 298 | 0 (0, 1) |
| Smoking status | 299 | |
| Current | 33 (11) | |
| Former | 71 (24) | |
| Never | 195 (65) |
Number may be less than 310 because of nonresponse.
Excludes skin cancer.
The primary diagnoses were upper respiratory infection (42% of patients), acute bronchitis (16%), sinusitis (13%), viral syndrome (9%), nonstreptococcal pharyngitis (8%), otitis media (6%), and streptococcal pharyngitis (6%) (Table 2). The most common chief complaints were cough (26%), sore throat (18%), sinus pain or pressure (8%), ear pain or stuffiness (6%), and runny nose (5%). Patients had symptoms for a median of 6 days (interquartile range, 4 to 10 days) prior to coming to clinic. One hundred and sixty-four patients (53%) missed work because of the present illness. Among patients who missed work, the median number of days missed was 2 (interquartile range, 1 to 2 days).
Table 2.
Primary Diagnoses and Antibiotic Prescribing by Diagnosis (N = 310)
| Diagnosis | n (%) | Proportion Receiving Antibiotics (%) |
|---|---|---|
| Upper respiratory tract infection | 131 (42) | 9 |
| Acute bronchitis | 49 (16) | 59 |
| Sinusitis | 39 (13) | 72 |
| Viral syndrome | 28 (9) | 4 |
| Nonstreptococcal pharyngitis | 25 (8) | 20 |
| Otitis media | 20 (6) | 85 |
| Streptococcal pharyngitis | 18 (6) | 100 |
The primary reason subjects sought care was for relief from symptoms (43%), relief from pain (24%), getting better to be able to return to work (13%), to be able to care for family (8%), for leisure time or travel (6%), or for another reason (4%). The primary expectation for the visit was to get a diagnosis (49%), an antibiotic prescription (25%), reassurance there is nothing serious going on (13%), a nonantibiotic treatment recommendation or prescription (5%), have testing carried out (3%), or to obtain an estimate of how long the symptoms would last (2%).
Wanting Antibiotics
When responding to the statement “I want antibiotics for my illness today,” 51 patients strongly agreed (16%), 69 patients agreed (22%), 145 patients had no opinion (47%), 29 patients disagreed (9%), and 16 patients strongly disagreed (5%). Only 19% of patients agreed or strongly agreed with the statement “Antibiotics work for me when I have a cold.” More than a quarter of patients (29%) agreed or strongly agreed with the statement “I plan on asking the doctor for antibiotics today.” Almost three quarters of patients (73%) agreed or strongly agreed with the statement “Repeated use of antibiotics can be bad for me in the long run.” Wanting antibiotics—agreeing or strongly agreeing with the statement “I want antibiotics for my illness today” (39% of patients)—was associated with not having attended college (60% vs 37% who did attend college; P = .03) and smoking status (64% of smokers vs 36% of nonsmokers; P = .002). Wanting antibiotics was also associated with using, on average, 1 or more antibiotic courses per year (44% vs 22% of those who did not report antibiotic use; P < .001). Wanting antibiotics was associated with sinus pain (46% vs 28% of those without sinus pain; P = .002), headache (41% vs 20% of those without headache; P = .007), purulent nasal discharge or sputum (45% vs 29% of those without purulence; P = .004), and productive cough (43% vs 26%; P = .02).
Wanting antibiotics was not associated with age, sex, race, income, insurance, employment, English as a primary language, missing work, duration of illness, overall bother of symptoms, having a primary care physician, heart disease, lung disease, diabetes, cancer, or having had a bad reaction to antibiotics.
In multivariable modeling, independent predictors of wanting antibiotics were prior antibiotic use (odds ratio [OR], 2.4; 95% confidence interval [CI], 1.3 to 4.7) and current smoking (OR, 3.1; 95% CI, 1.3 to 7.3; Table 3).
Table 3.
Multivariable Model of Wanting Antibiotics Among Adults with Upper Respiratory Infections (N = 273)*
| Variable | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Smoker | 3.1 | 1.3 to 7.3 |
| Prior antibiotic use | 2.4 | 1.3 to 4.7 |
| Antibiotics have worked for similar illnesses in the past | 1.6 | 0.8 to 3.4 |
| College | 0.6 | 0.2 to 1.7 |
| Heart disease | 0.3 | 0.1 to 1.2 |
| Sinus pain | 1.4 | 0.8 to 2.5 |
| Productive cough | 1.3 | 0.7 to 2.4 |
| Purulence | 1.7 | 0.9 to 3.2 |
| Headache | 1.7 | 0.7 to 4.1 |
N = 273 owing to nonresponse for some variables.
Antibiotic Prescribing
Among patients who met the inclusion and exclusion criteria, 110 (35%) were prescribed an antibiotic. In univariate testing, patients’ desire for antibiotics prior to the medical visit was associated with physicians’ prescribing antibiotics (OR 2.1, P = .01 adjusted for clustering by provider; Table 4). Patients with lung disease were significantly more likely to be prescribed antibiotics (53% vs 34% of patients without lung disease; P < .05), as were patients with sinus pain (41% vs 28% of patients without sinus pain; P = .02), and patients who missed work (40% vs 29% of patients who did not miss work; P = .04). Antibiotic prescribing was linearly associated with increasing overall bother (P = .03). Physician-charted symptoms that were associated with antibiotic prescribing included fever (46% vs 29% antibiotic prescribing for those without charted fever; P < .005), fatigue (20% vs 38% for patients without charted fatigue; P = .02), sinus pain (59% vs 32% for patients without charted sinus pain; P < .005), and ear pain (51% vs 33% for patients without charted ear pain; P = .03).
Table 4.
Patient Desire and Antibiotic Prescribing (P = .01)*
| Prescribed Antibiotics | No Prescribed Antibiotics | Row Totals | |
|---|---|---|---|
| Wanted antibiotics, n (%) | 55 (46) | 65 (54) | 120 (39) |
| Did not want antibiotics, n (%) | 55 (29) | 135 (71) | 190 (61) |
| Column totals, n (%) | 110 (35) | 200 (65) | 310 (100) |
P value is adjusted for clustering by provider. Patient desire for antibiotics was categorized according to response to the question “I want antibiotics for my illness today” administered prior to the office visit. Prescribing was based on actual prescriptions written by the physician during the visit.
Patients who were prescribed antibiotics had higher mean temperatures than patients who were not prescribed antibiotics (37.0°C vs 36.8°C; P = 0.01). Other physical exam findings that were associated with antibiotic prescribing were tympanic membrane abnormality (66% vs 32%; P < .001), sinus tenderness (69% vs 32%; P < .001), pharyngeal exudate (81% vs 33%; P < .001), lymphadenopathy (63% vs 30%; P < .001), and lung abnormalities (69% vs 32%; P < .001). All 13 of the patients who had a positive rapid test for group A streptococcus were treated with antibiotics (100% vs 33% without a positive rapid test for group A streptococcus; P < .001).
In multivariable modeling, wanting antibiotics remained a significant independent predictor of receiving antibiotics (OR, 2.1; 95% CI, 1.1 to 4.4; Table 5). Several physical exam findings strongly predicted antibiotic prescribing: temperature (OR, 2.0 per °C; 95% CI, 1.3 to 3.0), abnormal lung exam (OR, 11.9; 95% CI, 4.0 to 35.6), pharyngeal exudate (OR, 14.5; 95% CI, 3.3 to 63.7), tympanic membrane abnormality (OR, 8.4; 95% CI, 2.6 to 27.3), sinus tenderness (OR, 7.4; 95% CI, 2.9 to 19.2), and lymphadenopathy (OR, 5.4; 95% CI, 2.1 to 13.8). The only other significant predictor of antibiotic prescribing was physician-charted sinus pain (OR, 3.4; 95% CI, 1.2 to 9.4).
Table 5.
Multivariable Model of Receiving Antibiotics Among Adults with Upper Respiratory Infections (N = 295)*
| Variable | Odds Ratio | 95% Confidence Interval |
|---|---|---|
| Wants antibiotics | 2.1 | 1.1 to 4.4 |
| Abnormal lung exam | 11.9 | 4.0 to 35.6 |
| Pharyngeal exudate | 14.5 | 3.3 to 63.7 |
| Tympanic membrane abnormality | 8.4 | 2.6 to 27.3 |
| Sinus tenderness | 7.4 | 2.9 to 19.2 |
| Lymphadenopathy | 5.4 | 2.1 to 13.8 |
| Temperature (per °C > 37.0) | 2.0 | 1.3 to 3.0 |
| Sinus pain charted by provider | 3.4 | 1.2 to 9.4 |
| Patient-reported lung disease | 1.7 | 0.5 to 5.5 |
| Patient missed work | 1.3 | 0.8 to 2.1 |
N = 295 owing to nonresponse or missing variables. Model is adjusted for clustering by provider.
DISCUSSION
In a prospective study of adults who sought care for upper respiratory tract infections in the winter of 2001–02, we found that 39% of patients wanted antibiotics, less than the 60% to 75% of patients who wanted antibiotics in three directly comparable earlier studies12–14 (Table 6).
Table 6.
Summary of Studies Evaluating Patient Desire for Antibiotics
| Study | Study Period | N | Population | Setting | Consecutive Patients | Wanted Antibiotics, % | Received Antibiotics, % |
|---|---|---|---|---|---|---|---|
| Hamm et al.12 | Not stated(published 1996) | 113 | Patients with respiratory infections | Family practice clinics: 2 community practices,1 academic practice (Oklahoma City, Okla) | No | 65 | 63 |
| Dosh et al.13 | January and February 1998 | 482 | Patients with symptoms of acute respiratory infections | 15 primary care practices in the Upper Peninsula Research Network (Mich) | Yes | 60 | 66 |
| Ray and Rohren14 | Spring 1998 | 210 | Adults with cough, sore throat, or sputum production | Urgent care clinic (Rochester, Minn) | No | 75 | 64 |
| Present study | Winter 2001–02 | 310 | Adults with upperrespiratory symptoms | Acute care clinic (Boston, Mass) | No | 39 | 35 |
There are several explanations for the lower proportion of patients who wanted antibiotics in our study. First, patients’ expectations may have changed in the setting of decreased antibiotic prescribing rates for upper respiratory infections.16,17 Expectations may have changed because of decreased antibiotic prescribing by physicians, increased patient awareness of the inefficacy of antibiotics for upper respiratory infections, patient concern about antibiotic-resistant bacteria, or other factors. Second, our response frame differed from prior studies. In previous studies, patients were asked yes/no questions about their desire for antibiotics.12–14 We allowed patients to express varying degrees of desire for antibiotics with a Likert-type response frame. Almost half of patients (47%) expressed no opinion about wanting antibiotics. Lack of opinion may reflect patients’ uncertainty of either their diagnosis or the utility of antibiotics for upper respiratory tract infections. However, this uncertainty probably does not represent a general ambivalence about antibiotic treatment on the part of patients. A majority of patients (73%) felt that repeated use of antibiotics could be harmful to them and only 19% of patients thought antibiotics were effective when they had a cold. Third, the location and patient population in the present study was different from prior studies. This study was conducted at an academic, urban clinic whereas prior studies were in more rural settings.
Despite these differences with prior studies and the apparent decrease in the proportion of patients who wanted antibiotics, we continue to note an association between previous antibiotic use and wanting antibiotics (OR, 2.4; 95% CI, 1.3 to 4.7). We also note an association between wanting antibiotics and antibiotic prescribing (OR, 2.1; 95% CI, 1.1 to 4.4), even after adjusting for physical exam findings that are very strongly associated with antibiotic prescribing. Apparently, the more antibiotics patients used in the past, the more likely they were to desire antibiotics when presenting for care, and the more likely they were to actually receive antibiotics again. Prior experience may have “proven” to patients that antibiotics work. Alternatively, this finding may reflect the persistent nature of patients who want and receive antibiotics.
Our results should be considered in light of the limitations of this study. First, the study was conducted at a single acute care clinic in an urban, academic medical center and included a patient population that was predominantly educated and employed. However, many doctors perceive that just such a high-functioning patient population can be most demanding for antibiotics. Second, although physicians were not formally told of the study, we cannot exclude the possibility that physicians’ knowledge of the study may have influenced their prescribing behavior. Third, patients who chose to participate in the study may have been systematically different from patients who chose not to participate. To address this potential limitation, we attempted to enroll as many patients as possible. Additionally, patients were not aware of the content of the survey prior to participation. Two prior studies also did not enroll consecutive patients,12,14 yet we still note a large decrease in the proportion of patients who wanted antibiotics from the prior studies to the present study (Table 6).
To improve antibiotic prescribing for upper respiratory tract infections, physicians should know when antibiotics are indicated,22 and be aware of the techniques patients may use to “pressure” physicians for antibiotics.23 Our results indicate that most patients are aware that antibiotics are not effective for the average cold and that exposure to antibiotics carries some risk.
Physicians should remember that antibiotic prescribing has generally not been shown to be a determinant of patient satisfaction.12,14 Patients are satisfied as long as they perceive the physician has shown personal interest, provided reassurance, explained the illness, and the rationale for treatment.12,20 Finally, in continuing efforts to break the cycle of inappropriate antibiotic use, physicians should not assume that most patients with upper respiratory tract infections want antibiotics.
Acknowledgments
The authors wish to thank Nancy Bryant, RN, Barbara Woo, MD, as well as Cynthia Israel, Cynthia Jalbert, Nancy Doyle, and the other unit secretaries at the Medical Walk-In Unit of Massachusetts General Hospital.
Funding sources: Dr. Linder was supported in part by National Research Service Award 5T32PE11001-12.
REFERENCES
- 1.Cherry DK, Burt CW, Woodwell DA. National Ambulatory Medical Care Survey: 1999 Summary Advance Data from Vital and Health Statistics No 322. Hyattsville, Md: National Center for Health Statistics; 2001. [Google Scholar]
- 2.Hughes JM, McCaig LF. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 1995;273:214–9. doi: 10.1001/jama.287.23.3096. [DOI] [PubMed] [Google Scholar]
- 3.Mainous AG, III, Hueston WJ, Clark JR. Antibiotics and upper respiratory infection: do some folks think there is a cure for the common cold. J Fam Prac. 1996;42:357–61. [PubMed] [Google Scholar]
- 4.Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997;278:901–4. [PubMed] [Google Scholar]
- 5.Nyquist AC, Gonzales R, Steiner JF, Sande MA. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998;279:875–7. doi: 10.1001/jama.279.11.875. [DOI] [PubMed] [Google Scholar]
- 6.Metlay JP, Stafford RS, Singer DE. National trends in the use of antibiotics by primary care physicians for adult patients with cough. Arch Intern Med. 1998;158:1813–8. doi: 10.1001/archinte.158.16.1813. [DOI] [PubMed] [Google Scholar]
- 7.Hirschmann JV. Antibiotics for common respiratory tract infections in adults. Arch Intern Med. 2002;162:256–64. doi: 10.1001/archinte.162.3.256. [DOI] [PubMed] [Google Scholar]
- 8.Seppala H, Klaukka T, Vuopio-Varkila J, et al. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997;337:441–6. doi: 10.1056/NEJM199708143370701. [DOI] [PubMed] [Google Scholar]
- 9.Butler CC, Rollnick S, Pill R, Maggs-Rapport F, Stott N. Understanding the culture of prescribing: qualitative study of general practitioners’ and patients’ perceptions of antibiotics for sore throats. BMJ. 1998;317:637–42. doi: 10.1136/bmj.317.7159.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vinson DC, Lutz LJ. The effect of parental expectations on treatment of children with a cough: a report from ASPN. J Fam Prac. 1993;37:23–7. [PubMed] [Google Scholar]
- 11.Macfarlane J, Holmes W, Macfarlane R, Britten N. Influence of patients’ expectations on antibiotic management of acute lower respiratory tract illness in general practice: questionnaire study. BMJ. 1997;315:1211–4. doi: 10.1136/bmj.315.7117.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hamm RM, Hicks RJ, Bemben DA. Antibiotics and respiratory infections: are patients more satisfied when expectations are met? J Fam Prac. 1996;43:56–62. [PubMed] [Google Scholar]
- 13.Dosh SA, Hickner JM, Mainous AG, III, Ebell MH. Predictors of antibiotic prescribing for nonspecific upper respiratory infections, acute bronchitis, and acute sinusitis. An UPRNet study. Upper Peninsula Research Network. J Fam Prac. 2000;49:407–14. [PubMed] [Google Scholar]
- 14.Ray DA, Rohren CH. Characteristics of patients with upper respiratory tract infection presenting to a walk-in clinic. Mayo Clinic Proc. 2001;76:169–73. doi: 10.1016/S0025-6196(11)63124-8. [DOI] [PubMed] [Google Scholar]
- 15.Finkelstein JA, Davis RL, Dowell SF, et al. Reducing antibiotic use in children: a randomized trial in 12 practices. Pediatrics. 2001;108:1–7. doi: 10.1542/peds.108.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Linder JA, Stafford RS. Antibiotic treatment of adults with sore throat by community primary care physicians: a national survey 1989–99. JAMA. 2001;286:1181–6. doi: 10.1001/jama.286.10.1181. [DOI] [PubMed] [Google Scholar]
- 17.McCaig LF, Besser RE, Hughes JM. Trends in antimicrobial prescribing rates for children and adolescents. JAMA. 2002;287:3096–102. doi: 10.1001/jama.287.23.3096. [DOI] [PubMed] [Google Scholar]
- 18.Little P, Williamson I, Warner G, Gould C, Gantley M, Kinmonth AL. Open randomised trial of prescribing strategies in managing sore throat. BMJ. 1997;314:722–7. doi: 10.1136/bmj.314.7082.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hong JS, Philbrick JT, Schorling JB. Treatment of upper respiratory infections: do patients really want antibiotics? Am J Med. 1999;107:511–5. doi: 10.1016/s0002-9343(99)00270-3. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez-Menegay C, Hudes ES, Cummings SR. Patient expectations and satisfaction with medical care for upper respiratory infections. J Gen Intern Med. 1992;7:432–4. doi: 10.1007/BF02599162. [DOI] [PubMed] [Google Scholar]
- 21.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 22.Gonzales R, Bartlett JG, Besser RE, et al. Principles of appropriate antibiotic use for treatment of acute respiratory tract infections in adults: background, specific aims, and methods. Ann Intern Med. 2001;134:479–86. doi: 10.7326/0003-4819-134-6-200103200-00013. [DOI] [PubMed] [Google Scholar]
- 23.Scott JG. Antibiotic use in acute respiratory infections and the ways patients pressure physicians for a prescription. J Fam Prac. 2001;50:853–8. [PubMed] [Google Scholar]