Abstract
BACKGROUND
For patients with chronic illnesses, it is hypothesized that effective patient-provider collaboration contributes to improved patient self-care by promoting greater agreement on patient-specific treatment goals and strategies. However, this hypothesis has not been tested in actual encounters of patients with their own physicians.
OBJECTIVE
To assess the extent to which patients with type 2 diabetes agree with their primary care providers (PCPs) on diabetes treatment goals and strategies, the factors that predict agreement, and whether greater agreement is associated with better patient self-management of diabetes.
DESIGN
One hundred twenty-seven pairs of patients and their PCPs in two health systems were surveyed about their top 3 diabetes treatment goals (desired outcomes) and strategies to meet those goals. Using several measures to evaluate agreement, we explored whether patient characteristics, such as education and attitudes toward treatment, and patient-provider interaction styles, such as shared decision making, were associated with greater agreement on treatment goals and strategies. We then examined whether agreement was associated with higher patient assessments of their diabetes care self-efficacy and self-management.
RESULTS
Overall, agreement on top treatment goals and strategies was low (all κ were less than 0.40). In multivariable analyses, however, patients with more education, greater belief in the efficacy of their diabetes treatment, and who shared in treatment decision making with their providers were more likely to agree with their providers on treatment goals or strategies. Similarly, physician reports of having discussed more content areas of diabetes self-care were associated with greater agreement on treatment strategies. In turn, greater agreement on treatment goals and strategies was associated both with higher patient diabetes care self-efficacy and assessments of their diabetes self-management.
CONCLUSION
Although patients and their PCPs in general had poor agreement on goals and strategies for managing diabetes, agreement was associated with higher patient self-efficacy and assessments of their diabetes self-management. This supports the hypothesis that enhancing patient-provider agreement on both overall treatment goals and specific strategies to meet these goals may lead to improved patient outcomes.
Keywords: chronic disease management, diabetes, patient-doctor communication, self-management
Successful management of chronic illnesses such as diabetes requires close teamwork between patients and their health care providers. Providers need to prescribe optimal medications, order and act on appropriate tests, and counsel patients on treatment plans. Patients in turn must sustain often-complicated medication, diet, and exercise regimens, a set of skilled behaviors called self-management. Patients' self-management practices and confidence in their ability to complete these activities (self-efficacy1) have been clearly associated with improved clinical outcomes.2,3 More effective patient-provider communication, in turn, has been associated with better patient self-care and health.4–8 Yet, it is not clear which aspects of patient-provider interactions are most important in improving patients' self-management and diabetes care self-efficacy.
There is growing evidence that people with defined health goals have more effective self-care behaviors.9–12 Building on this research, some experts advocate moving from a directive to a more collaborative patient-provider style, with joint definition of problems, treatment goals, and management strategies.13–18 Proponents postulate that actively engaging patients in setting treatment goals and strategies encourages greater patient understanding and motivation to follow treatment plans, as well as providing a benchmark against which to measure success.6,13,15,19–23
A central hypothesis behind such arguments is that improved patient-provider collaboration leads to improved outcomes by promoting greater agreement on treatment goals and strategies.13,19,21,24,25 Certainly, it makes intuitive sense that patients and providers with a shared view of treatment goals and strategies might work together better to manage that patient's diabetes. Greater agreement may also be a marker for more effective communication. These hypotheses, however, have not been rigorously tested.
Qualitative research suggests there is often disagreement between patients and providers on the nature and outcomes of health problems,26–31 and on goals and strategies in diabetes management.32–35 Most prior studies on diabetes, however, compare patients with diabetes and providers in general, rather than patients with their own physicians.
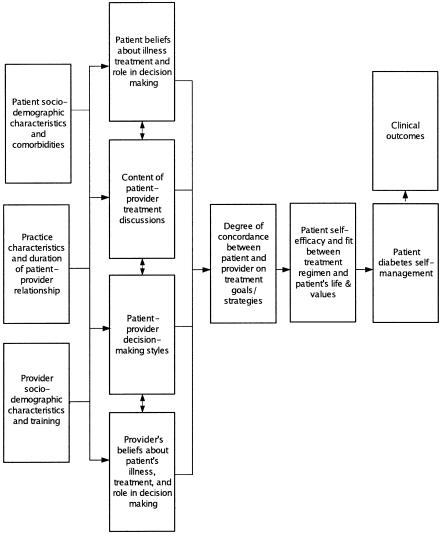
To address these gaps in knowledge, we conducted a study to explore three questions: 1) to what extent do patients with type 2 diabetes and their health care providers agree on treatment goals and strategies for that patient?; 2) what factors predict agreement?; and 3) is greater agreement associated with better patient self-efficacy and diabetes self-management? The conceptual model guiding this study is shown in Figure 1. In particular, we sought to test 2 hypotheses: 1) more collaborative patient–doctor interaction styles will be associated with greater agreement; and 2) greater agreement on treatment goals and strategies will correlate with better patient self-efficacy in managing diabetes, reported self-care behaviors, and assessments of self-management.
Figure 1.
Conceptual model: patient and provider factors influencing degree of concordance and hypothesized effects of concordance between patient and provider.
METHODS
Study Population/Data Collection
The participants in this study were surveyed in a VA and an academic medical center (AMC) in Michigan. The study received IRB approval, and written informed consent was obtained for all participants. The study was carried out between May and December 2001.
Patients were eligible if they were at least 30 years old and had at least 1 prescription for a glucose control medication or monitoring supplies, 1 hospitalization with a diabetes-related ICD-9 code, or 2 outpatient visits with a diabetes-related ICD-9 code. They had to have seen their PCP in the prior 6 months and be scheduled to see the same PCP again in the next 6 months. To further ensure patients and their PCPs had an established relationship, only patients of physicians who were senior residents or attending faculty were included. Finally, patients were excluded if administrative data indicated they had seen an endocrinologist in the prior 2 years.
In the VA, 562 patients were eligible and sent surveys. AMC patients were drawn from the diabetes registry of an AMC-affiliated managed care organization. A total of 720 of the 1,060 eligible AMC patients were randomly sampled and sent surveys. The 91 PCPs of these patients, 34 from the VA and 57 from the AMC, were then sent a general survey. We sent 2 waves of mailings, including a pocket flashlight with the first mailing. Seventy-four patients were excluded because they reported not having type 2 diabetes, suffered severe dementia, or were deceased. A total of 663 of the remaining patients completed the survey (56% response rate). Respondents were older and more likely to be male, married, and nonblack than nonrespondents. The response rate among providers was 74%.
We then e-mailed 10 patient-specific questions to the PCPs the same day they had a clinic visit with a participating patient within 3 months of that patient completing the survey. Based on pilot interviews with providers on how many postvisit surveys they would be willing to complete, PCPs were sent emails on no more than 3 patients. Each e-mail a PCP completed counted as an entry in a raffle of a Palm Pilot. Of the 54 providers who received e-mails, 50 providers (93%) returned at least 1 e-mailed questionnaire. Response rates of providers sent an e-mail about a second and third patient were 69% and 73%, respectively. During the study period, providers returned questionnaires on 127 patients (see Table 1 for respondent characteristics.) For this study's analyses, we included respondents who marked exactly 3 goals or strategies. While all providers listed three goals and strategies, 9 patients listed fewer than 3 goals and 28 listed more than 3 goals; 10 patients listed fewer and 25 listed more than 3 strategies.
Table 1.
Respondent Characteristics
| Patient (N = 127) | Provider (N = 50) | |
|---|---|---|
| Mean age, y (SD) | 64 (11) | 40 (10) |
| Male, % | 81 | 56 |
| Ethnicity, % | ||
| White | 88 | 82 |
| Minority | 12 | 18 |
| Length of time with diabetes, % | ||
| Less than 3 years | 33 | – |
| 4–10 years | 40 | – |
| More than 10 years | 27 | – |
| Years of education, (SD) | 13 (3) | – |
| Annual Income | ||
| $20,000 or less | 51 | – |
| $20,001–$40,000 | 31 | – |
| $40,001–$60,000 | 6 | – |
| $60,001 or more | 12 | – |
| Hypoglycemic regime, % | ||
| Oral medications only | 66 | – |
| On insulin | 31 | – |
| No medications | 3 | – |
| Health status, % | ||
| Excellent or very good | 16 | – |
| Good | 46 | – |
| Fair | 28 | – |
| Poor | 10 | – |
| Have “high blood pressure,”% | 73 | |
| Have “high cholesterol,”% | 62 | |
| Duration with doctor who takes care of diabetes, % | ||
| Less than 6 months | 14 | – |
| 6 months to 1 year | 21 | – |
| 1 year to 5 years | 41 | – |
| More than 5 years | 24 | – |
| Receive most information on diabetes self-management from their doctor, % | 67 | |
| Medical specialty, % | ||
| Internal medicine | – | 82 |
| Family medicine | – | 4 |
| Nurse practitioner/physician assistant | – | 14 |
| Years in clinical practice, (SD) | – | 12 (9) |
| Amount of time for return visits, minutes (SD) | – | 21 (7) |
| Providers who provide all or most self-management education to diabetic patients, % | – | 22 |
Survey Instruments
There were 3 survey instruments. A patient survey included questions on sociodemographic and clinical characteristics, self-efficacy, self-management behaviors, confidence in treatment efficacy,36 and their providers' communication and decision-making styles (see Table 2 for key variables.) Two items requested patients to list their top 3 treatment goals and strategies, as described below. The patient survey was pilot tested with 25 adults with type 2 diabetes. Providers completed a general survey on their diabetes care attitudes and practices and up to 3 concordance questionnaires, in which the provider evaluated the diabetes management and listed their top 3 diabetes treatment goals and strategies for the patient just seen. These 10 questions and the larger general provider survey were piloted with 10 endocrinologists and 11 primary care physicians.
Table 2.
Summary Descriptions of Principal Independent and Dependent Variables
| Variable | Item(s) | Range | Meaning of High Score | Mean (SD) (95% CI) | Cron-bach's α |
|---|---|---|---|---|---|
| A. Predictor Variables | |||||
| Patient belief in treatment efficacy | “Following my prescribed diabetes treatment plan will make a big difference in preventing long-term complications.” | 1 to 5 | More strongly agree with the statement | 3.8 (3.6 to 3.9) | N/A |
| Health Care Climate Scale* | 16 items including whether physician provides patient with choices, encourages questions, answers questions fully, provides patient with “all the support” that he/she needs, etc. | 0 to 100 | Higher assessment of how collaborative provider is | 73.5 (70.4 to 76.6) | 0.96 |
| Shared treatment decision making | 1) Leave decisions about treatment to my doctor (coded 1) | 1 to 3 | More equally shared decision making | 1.08 (0.94 to 1.2) | N/A |
| 2) Doctor makes final decision, but considers opinion (coded 2) | |||||
| 3) Doctor and patient share responsibility for deciding treatment (coded 3) | |||||
| 4) Patient makes final decision after considering doctor's opinion (coded 2) | |||||
| 5) Patient makes final selection with little input from doctor (coded 1) | |||||
| Number of diabetes self-care areas discussed | 1) How and when to take meds | 0 to 8 | More areas of diabetes self-care discussed in office visits in past 6 months | Patients: 2.9 (2.5 to 3.4) Providers: 5.3 (5.1 to 5.6) | N/A |
| 2) How and when to check blood glucose | |||||
| 3) How to time meals | |||||
| 4) What to eat | |||||
| 5) How to increase physical activity | |||||
| 6) How to change meds | |||||
| 7) How to deal with emotional demands of diabetes | |||||
| 8) Where to find community resources for diabetes | |||||
| B. Outcome Variables | |||||
| Self-efficacy scale | 1) I feel confident in my ability to manage my diabetes | 0 to 100 | Higher self-efficacy in managing diabetes | 70.2 (67.0 to 73.4) | 0.88 |
| 2) I feel capable of handling my diabetes now | |||||
| 3) I am able to do my own routine diabetes care now | |||||
| 4) I am able to meet the challenge of controlling my diabetes | |||||
| Self-management activities in past 7 days* | 1) Taking medications | Each domain scaled from 0 to 7 | Completed greater number of activities in past 7 days | 1) 6.5 (6.3 to 6.8) | 0.96 0.76 0.76 N/A 0.64 |
| 2) Exercising regularly | 2) 2.6 (2.2 to 3.1) | ||||
| 3) Following eating plan | 3) 4.4 (4.0 to 4.8)> | ||||
| 4) Checking blood sugar | 4) 4.9 (4.4 to 5.4)> | ||||
| 5) Checking feet for wounds or sores | 5) 4.4 (3.9 to 4.9) | ||||
| Patient overall assessment of their diabetes self-care in past 6 months | “What grade would you give yourself on your diabetes self-care in the past six months?” | A – F (1–5) | Higher patient assessment of their diabetes self-management | 3.4 (3.2 to 3.6) | N/A |
The entire scale considered missing if half or more of its components were missing; CI, confidence interval.
Treatment Goals and Strategies Variables
Based on a medsearch literature review and discussions with chronic disease experts, we developed 2 separate lists of treatment goals (desired outcomes) and specific strategies.13,19,32,37,38 Patients and providers were each asked to rank their top 3 goals from a list of 11 possible treatment outcomes (see list in Table 3). Then, each rated their top 3 strategies from a list of 9 treatment strategies (Table 3). In both cases, patients and providers could also write in other goals or strategies.
Table 3.
Patient and Provider Agreement on Goals and Strategies*
| One of Three for Both Patient and Provider, % | Not Selected by Patient or Provider, % | Patient Only, % | Provider Only, % | |
|---|---|---|---|---|
| A. Individual goals (N = 90 pairs) | ||||
| Keep blood sugar close to normal to avoid long-term complications | 63 | 7 | 18 | 12 |
| Succeed in losing weight | 18 | 47 | 21 | 14 |
| Become more physically fit | 12 | 55 | 19 | 14 |
| Keep blood pressure normal | 8 | 52 | 7 | 34 |
| Avoid ulcers or injury to feet | 7 | 69 | 12 | 12 |
| Avoid symptoms from too low blood sugar | 7 | 62 | 10 | 21 |
| Avoid going on insulin | 3 | 71 | 25 | 1 |
| Lower blood cholesterol | 2 | 71 | 9 | 18 |
| Follow a treatment that does not interfere with life | 2 | 69 | 7 | 22 |
| Lessen physical discomfort/pain | 1 | 83 | 14 | 2 |
| Be able to get off medications | 1 | 74 | 25 | 0 |
| Follow affordable treatment | 1 | 87 | 8 | 4 |
| B. Treatment strategies (N = 92 pairs) | ||||
| Take diabetes medications | 38 | 11 | 42 | 9 |
| Exercise regularly | 30 | 33 | 12 | 25 |
| Eat to keep blood sugar close to normal | 23 | 16 | 46 | 15 |
| Monitor blood sugar | 13 | 41 | 36 | 10 |
| Follow a reduced calorie diet | 6 | 64 | 3 | 27 |
| Follow good foot care | 5 | 69 | 9 | 17 |
| Treat high blood pressure | 5 | 54 | 7 | 34 |
| Follow a low fat diet | 4 | 73 | 8 | 15 |
| Treat high cholesterol | 1 | 68 | 9 | 22 |
Samples include only those patients and providers who listed exactly 3 goals and 3 strategies.
To measure agreement on treatment goals and strategies, we created 2 sets of variables. The first was the number of goals or strategies (from 0 to 3) that both the provider and patient within a pair listed as 1 of their top 3 priorities. Because it is not clear whether agreement on a larger number of goals or strategies or just agreement on a top priority would be more important, we also created variables for whether the PCP's top goal or strategy was among the top 3 the patient listed.
Variables We Hypothesized Would Predict Concordance on Treatment Goals and Strategies
The conceptual model in Figure 1 guided our choice of independent variables to test in our models. In particular, we sought to explore the association of patient-doctor collaboration and communication with concordance. We used two standard measures to assess the degree of collaboration in patient-doctor interaction styles (Table 2). The first was the Health Care Climate Questionnaire, a well-validated 16-item scale, for patients to assess the patient-centeredness of their providers.2,39 For the second, we constructed a continuous variable from a validated question asking patients to describe how they and their providers usually make decisions about diabetes treatments.40–42
Because collaboration requires exchange of information, we used content areas from Glasgow and Ruggiero's scale of reported diabetes self-care recommendations43 (Table 2) to construct an index summing the self-care content areas that the patient reported their provider had discussed with them, and another summing the number of areas the provider reported discussing in the past 6 months (range of 0 to 8). We used the patient and provider reports as separate variables in analyses.
We hypothesized that patients' beliefs about the efficacy of their prescribed diabetes treatment would be associated with concordance with their providers about treatment goals and strategies. Patients rated their level of agreement on a 5-point Likert scale with the statement: “Following my prescribed diabetes treatment plan will make a big difference in preventing long-term complications” (Table 2).
Finally, we tested the patient sociodemographic and clinical characteristics of gender, ethnicity, age, years of education, annual household income, self-reported health status, number of diabetes comorbidities, and diabetes duration.36,44,45 Because of limited sample size, we did not systematically assess practice or provider characteristics.
Outcome Variables We Hypothesized Concordance Would Predict
Our outcome variables were patients' confidence, or self-efficacy, in their diabetes self-management abilities, reported self-management behaviors in the past 7 days, and overall evaluation of their diabetes self-management over the past 6 months (Table 2). To evaluate self-efficacy, we used a validated 4-item scale.2 This measure has been significantly associated with glycemic control and other improved clinical outcomes in prospective studies.2 To assess self-care behaviors, respondents were asked on how many of the past 7 days they carried out recommended self-care activities in 5 areas.46 Because adherence in 1 area of diabetes care does not correlate strongly with adherence in others,46,47 we looked separately at each area. The third outcome was patients' overall assessment of how well they had managed their diabetes in the prior 6 months (Table 2).
Analyses
We generated descriptive statistics to characterize the study populations and distribution of responses. We assessed agreement between patients and clinicians with 3 measures: 1) overall agreement; 2) Cohen's κ statistics;48 and 3) the summary statistics of agreement on goals and strategies described above.
We then examined bivariate and multivariable associations between our variables of interest and concordance on treatment goals and strategies. We included as covariates in the multivariable analyses only patient sociodemographic characteristics that were associated with any of the concordance measures at a level of significance of < .10 in bivariate analyses. We also adjusted for diabetes severity by including diabetes duration and self-reported health status (both of which were highly correlated with insulin use). For the ordinal dependent variables, we used ordinal logistic regression, and for the dichotomous outcomes we used logistic regression. In all multivariable analyses, to account for the clustering effects of within-physician correlation, we adjusted standard errors using the Huber/White sandwich estimator of the cluster corrected variance/covariance matrix.49,50 Regression diagnostic procedures yielded no evidence of multicollinearity or overly influential outliers in any of the models.
RESULTS
Patient and Provider Characteristics
Characteristics of the patients and their providers for whom we have paired data are presented in Table 1. Patients were predominantly male (81%) and white (88%), with a mean age of 64. As patients from the VA constituted 70% of the sample, 51% of respondents had annual household incomes of less than $20,000. A total of 97% were on oral medications and/or insulin, and 67% of the sample had had diabetes 4 or more years. Eighty-six percent of the patients had been with their primary care doctor for more than 6 months. Eighty-two percent of the providers were general internists, with a mean of 12 years of clinical practice. The majority of providers (56%) were men, and 82% were white.
Agreement Between Patients and Their Providers on Goals and Strategies
Table 3 shows the extent of agreement between patients and their providers on the top 3 treatment goals. Although overall agreement was quite low (κ from .00 to .24), patients and providers were most likely both to list normalizing blood glucose levels (63%), losing weight (18%), and becoming more physically fit (12%) as goals (Table 3). Patients were more likely to be the only one in their pair to list avoiding starting insulin (25%), getting off all medications (25%), and lessening physical discomfort (14%) as their goals. Providers were most likely to be alone in listing keeping blood pressure normal (34%), lowering blood cholesterol (18%), and, somewhat surprisingly, having the patient follow a treatment plan that does not interfere too much with the patient's life (22%). Although 73% of respondents reported having hypertension and 62% reported having hypercholesterolemia, only 15% included blood pressure control as one of their top 3 goals, and 11% included lipid control.
Overall agreement on specific treatment strategies was also low (Table 3B). All κ for agreement on individual strategies were less than 0.40. Patients and their providers were most likely to agree on taking diabetes medications (38%) and exercising regularly (30%). Patients were more likely than providers to emphasize strategies geared toward glycemic control such as eating to keep blood sugar close to normal (46%), taking diabetes medications (42%), and monitoring blood sugar (36%). Providers were more likely to prioritize treating high blood pressure (34%), following a reduced calorie diet (27%), and exercising regularly (25%). Twelve percent of patients included treating blood pressure as 1 of their top 3 treatment strategies, and 10% listed treating high cholesterol.
Figure 2 shows the amount of overlap between patients and their providers on goals and strategies. There was considerable variation among pairs in levels of agreement; a third of the pairs agreed on 2 of the 3 top goals, and 21% agreed on 2 of the top 3 strategies. Fifty-five percent of respondents had included their provider's top goal and strategy among their top 3. In the majority of cases, when there was agreement, patients and providers agreed on goals and strategies related to glycemic control.
Figure 2.
Overlap between patients and providers on treatment goals and strategies.
What “Predicts” Concordance?
Table 4A presents the results of 4 separate regression models, 1 for each of the following outcomes: number of goals agreed on; agreement on top goal; number of strategies agreed on; and agreement on top strategy. The independent variables (Table 2) that, after adjustment for demographic and clinical factors, were associated with the various types of agreement (P < .10) are included. The stronger the patient's belief in the efficacy of their prescribed treatments, the more goals they shared with their provider (P = .013) and the more likely they were to have included their provider's top treatment goal among their top 3 goals (P = .03). Patients with more education were more likely to have their provider's top treatment strategy among their top 3 strategies (P = .015).
Table 4.
Significant Correlates of Concordance on Diabetes Treatment Goals and Strategies in Multivariate Analyses
| Independent Variable | Dependent Variable | β-Coefficient | P Value |
|---|---|---|---|
| A. What predicts concordance?* | |||
| 1. Patient's belief in treatment efficacy† | Number of treatment goals agreed upon by patient and provider† | 0.65 | .013 |
| 2. Patient's belief in treatment efficacy‡ | Agreement on top treatment goal‡ | 0.63 | .03 |
| 3. Patient years of education‡ | Agreement on top treatment strategy‡ | 0.18 | .015 |
| 4. Number of areas of diabetic self-management on which provider reports counseling‡ | Agreement on top treatment strategy‡ | 0.46 | .007 |
| Number of areas of diabetic self-management on which provider reports counseling† | Number of treatment strategies agreed upon by patient and provider† | 0.41 | .006 |
| 5. Patient reports that s/he shares responsibility with provider in making treatment decisions† | Number of treatment strategies agreed upon by patient and provider† | 0.50§ | .096§ |
| B. What does concordance predict?¶ | |||
| 1. Number of treatment goals agreed upon by patient and provider† | Patient's assessment of their diabetes self-management† | 0.68 | .004 |
| 2. Agreement on top treatment strategy† | Patient self-efficacy in managing diabetes† | 1.17 | .005 |
Table 4A presents the results of 4 separate regression models, 1 for each of the following outcomes: number of goals agreed on; agreement on top goal; number of strategies agreed on; and agreement on top strategy. The independent variables that, after adjusting for all covariates listed below, are significant at a level of P < .10 are included in the table.
Ordinal logit models adjusting for patient age, years of formal education, diabetes duration, self-reported health status, and clustering by primary care provider.
Logit regression models adjusting for patient age, years of formal education, diabetes duration, self-reported health status, and clustering by primary care provider.
In bivariate analyses: (β-coefficient = 0.57, P = .026.
¶ Table 4B presents the results of 2 separate regression models, each with the same covariates (above) but including the 2 different concordance measures as principal independent variables.
Patients who reported sharing responsibility with their providers in making treatment decisions agreed with their providers on significantly more treatment strategies in bivariate analyses (P = .026), an association that was attenuated in the multivariate analyses (P = .096). A physician report of having discussed more areas of diabetes self-management was also associated with greater overlap on treatment strategies (P = .006) and with greater agreement on the most important treatment strategy (P = .007). The final variable we hypothesized would correlate with concordance, higher patient assessments of provider “patient-centeredness,” although associated in bivariate analyses with agreement on the provider's top recommended treatment strategy (P = .04), was not associated with this (P = .12) or other outcome measures in multivariate analyses.
In addition, we conducted alternative analyses including length of patient-provider relationship and health care site (VA vs AMC) as covariates. Including these variables did not affect our findings.
What Does Concordance “Predict”?
As Table 4B shows, agreement on treatment goals and strategies was associated with 2 of the 3 measures of patients' self-management. After adjusting for potential confounders, patients who shared their providers' top treatment strategy had higher self-efficacy than those who did not (P = .005). Moreover, those who agreed with their providers on more treatment goals rated their diabetes self-management more positively than those who agreed on fewer goals (P = .004). We found no significant associations in multivariable analyses between agreement on treatment goals or strategies and patients' reported self-care activities in the prior 7 days.
DISCUSSION
In these primary care practices, agreement between patients with diabetes and their PCPs on diabetes treatment goals and strategies in general was quite low. Recent randomized clinical trials have found that multifaceted programs that promote patient involvement in defining diabetes treatment goals and strategies improve clinical outcomes.20,51 Nevertheless, collaborative goal setting is not a standard part of chronic disease management in many primary care practices. Thus, one likely explanation for the low rates of agreement is that providers are not explicitly discussing treatment goals or strategies and seeking to reach agreement with their patients on priority areas to target.52,53 In light of the importance of blood pressure and lipid control for clinical outcomes in diabetes,54 the especially low agreement on goals and strategies targeting lipid and blood pressure control is concerning, and raises the possibility that doctors have more effectively conveyed to patients the importance of glycemic control than lipid and blood pressure control.
Although agreement in general was low, there was significant variation in levels of agreement across patient-provider pairs, and more agreement was indeed associated with higher patient self-efficacy and more positive assessment of their diabetes self-management. Those patients who shared responsibility with their physicians for making treatment decisions more often agreed on priority treatment strategies with their providers. Moreover, provider reports of having discussed more content areas of diabetes self-care were associated with greater agreement on treatment strategies. A supportive style by itself, however, was not enough in the absence of discussion on what patients need to know to be able to prioritize treatment goals and strategies. In fact, those patients who evaluated their providers overall as being more patient centered, after adjustment for potential confounders, were not more likely to agree with them on treatment goals or strategies. What appeared to predict agreement was sharing in treatment decision making and having discussed the relevant content areas.
In our sample, patients who might be more likely to share their providers' views—those with more confidence in the efficacy of their medical treatment regimens and those with more formal education—were indeed more likely to agree with their providers on treatment goals and strategies. These results coincide with prior research finding that patient adherence is more likely if patients and their doctors share disease models and agree on which medical problems are important and how to evaluate therapeutic success.38,55–57
Greater patient self-efficacy and more positive assessments of diabetes self-management are beneficial outcomes and have been associated with improved clinical outcomes such as glycemic control.2,3,58 Our findings support the hypothesis that greater concordance between patients and their providers on goals and strategies may be a mechanism by which better patient-provider communication and collaboration contribute to improved patient outcomes, as postulated in Figure 1. Accordingly, we need to understand better factors, such as those highlighted in this study, that contribute to or impede agreement between patients and providers on treatment goals and strategies.
There are a number of ways effective goal setting between patients and providers might enhance processes and outcomes of diabetes and other chronic illness care. Besides encouraging patients and providers to articulate their goals and thus provide opportunities to negotiate potential conflicts in priorities,31,32 recommended plans of care can be linked to desired outcomes, clarifying for patients the purpose of various recommendations.18 While it is possible that differing goals might expand the number of issues addressed, poor agreement on treatment goals and strategies suggests that patients and providers may be failing to work together as a team—or even may be working at cross-purposes to each other.31
These data from a small sample of patient-provider pairs in only two health systems represent exploratory findings on this little investigated dimension of patient-provider relations. Several limitations must be noted. First, we elicited patient and provider goals and strategies only once. Of note, however, all participating patients had seen their provider at least once before, and 86% of the patients had seen this same PCP 6 months or longer. Thus, patients and providers had had several visits in which to discuss and establish mutual goals and strategies. Second, several features of our study design may have led to overestimating concordance. The patients had ranked their top goals and priorities before they saw their provider, which may have primed them to discuss these at their visit before their provider completed the after-visit questionnaire. Moreover, while respondents had the option of writing in other choices, we largely focused on biomedical outcomes and strategies in the list from which participants chose. While our aim was to assess whether there would be agreement within this more limited range of goals most closely associated with patients' clinical outcomes, our method likely did not capture the full universe of patients' valued treatment goals and strategies.
Third, our sample size was too small to enable us to explore significant differences among PCPs. Certain PCPs might have better agreement with their patients. For example, women providers may be more likely to adopt collaborative styles with their patients, ask more questions, and have better communication,59 and race-concordant pairs may have more participatory decision-making styles.45 Similarly, we had insufficient numbers of ethnic minorities to assess possible ethnic differences in degree of concordance with providers. This study needs to be replicated in a larger, diverse sample and with a longitudinal design to track whether and how agreement on treatment goals and strategies varies and to assess the consequences of different levels of agreement for self-management and clinical outcomes over time.
In conclusion, while many patients and providers in standard primary care practices have poor agreement on diabetes treatment goals and strategies, better agreement on both of these is associated with improved self-efficacy and self-management. Increased patient-provider discussion of treatment goals and specific strategies to meet these goals may increase agreement on these and lead to improved patient outcomes. We need to explore how best to operationalize appropriate goal setting in clinical settings and evaluate the effects of encouraging patients and providers to jointly define and pursue shared diabetes treatment goals and strategies.
Acknowledgments
This work was supported by The Department of Veterans Affairs (VA) Health Services Research & Development (HSR & D) Service, The Robert Wood Johnson Clinical Scholars Program, and by NIH grants #1 R18 DK062323-01 and #5P60-DK20572. Dr Vijan is a VA HSR & D Career Development awardee. The views expressed herein do not necessarily represent those of The Robert Wood Johnson Foundation or The Department of Veterans Affairs.
REFERENCES
- 1.Bandura A. Englewood Cliffs, NJ: Prentice Hall; 1986. Social Foundations of Thought and Action. A Social Cognitive Theory. [Google Scholar]
- 2.Williams GC, Freedman ZR, Deci EL. Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care. 1998;21:1644–51. doi: 10.2337/diacare.21.10.1644. [DOI] [PubMed] [Google Scholar]
- 3.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. How well do patients' assessments of their diabetes self-management correlate with actual glycemic control and receipt of recommended diabetes services? Diabetes Care. 2003;26:738–43. doi: 10.2337/diacare.26.3.738. [DOI] [PubMed] [Google Scholar]
- 4.Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med. 2002;17:243–52. doi: 10.1046/j.1525-1497.2002.10905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.DiMatteo MR. Enhancing patient adherence to medical recommendations. JAMA. 1994;271:83. doi: 10.1001/jama.271.1.79. [DOI] [PubMed] [Google Scholar]
- 6.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician–patient interactions on the outcomes of chronic disease. Med Care. 1989;27:110S–127S. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 7.Stewart MA. Effective physician–patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 8.Sherbourne CD, Hays RD, Ordway L, DiMatteo MR, Kravitz RL. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15:447–68. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 9.Brownell KD, Cohen LR. Adherence to dietary regimens. 1. An overview of research. Behav Med. 1995;20:149–54. doi: 10.1080/08964289.1995.9933731. [DOI] [PubMed] [Google Scholar]
- 10.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11:257–61. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 11.Clark MM, Abrams DB, Niaura RS, Eaton CA, Rossi JS. Self-efficacy in weight management. J Consult Clin Psychol. 1991;59:739–44. doi: 10.1037//0022-006x.59.5.739. [DOI] [PubMed] [Google Scholar]
- 12.Levetan CS, Dawn KR, Robbins DC, Ratner RE. Impact of computer-generated personalized goals on HbA (1c) Diabetes Care. 2002;25:2–8. doi: 10.2337/diacare.25.1.2. [DOI] [PubMed] [Google Scholar]
- 13.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127(12):1097–102. doi: 10.7326/0003-4819-127-12-199712150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 15.Anderson RM, Funnell MM, Butler PM, Arnold MS, Fitzgerald JT, Feste CC. Patient empowerment. Results of a randomized controlled trial. Diabetes Care. 1995;18:943–9. doi: 10.2337/diacare.18.7.943. [DOI] [PubMed] [Google Scholar]
- 16.Anderson RM, Funnell MM. Compliance and adherence are dysfunctional concepts in diabetes care. Diabetes Educ. 2000;26:597–604. doi: 10.1177/014572170002600405. [DOI] [PubMed] [Google Scholar]
- 17.Glasgow RE, Anderson RM. In diabetes care, moving from compliance to adherence is not enough. Something entirely different is needed. Diabetes Care. 1999;22:2090–2. doi: 10.2337/diacare.22.12.2090. [DOI] [PubMed] [Google Scholar]
- 18.Bradley EH, Bogardus ST, Jr, Tinetti ME, Inouye SK. Goal-setting in clinical medicine. Soc Sci Med. 1999;49:267–78. doi: 10.1016/s0277-9536(99)00107-0. [DOI] [PubMed] [Google Scholar]
- 19.Wolpert HA, Anderson BJ. Management of diabetes: are doctors framing the benefits from the wrong perspective? BMJ. 2001;323:994–6. doi: 10.1136/bmj.323.7319.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Olivarius NF, Beck-Nielsen H, Andreasen AH, Horder M, Pedersen PA. Randomised controlled trial of structured personal care of type 2 diabetes mellitus. BMJ. 2001;323:970–5. doi: 10.1136/bmj.323.7319.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Golin CE, DiMatteo MR, Gelberg L. The role of patient participation in the doctor visit. Implications for adherence to diabetes care. Diabetes Care. 1996;19:1153–64. doi: 10.2337/diacare.19.10.1153. [DOI] [PubMed] [Google Scholar]
- 22.Glasgow RE, Funnell MM, Bonomi AE, Davis C, Beckham V, Wagner EH. Self-management aspects of the improving chronic illness care breakthrough series: implementation with diabetes and heart failure teams. Ann Behav Med. 2002;24:80–7. doi: 10.1207/S15324796ABM2402_04. [DOI] [PubMed] [Google Scholar]
- 23.Senecal C, Nouwen A, White D. Motivation and dietary self-care in adults with diabetes: are self-efficacy and autonomous self-regulation complementary or competing constructs? Health Psychol. 2000;19:452–7. doi: 10.1037//0278-6133.19.5.452. [DOI] [PubMed] [Google Scholar]
- 24.Martin TL, Selby JV, Zhang D. Physician and patient prevention practices in NIDDM in a large urban managed-care organization. Diabetes Care. 1995;18:1124–32. doi: 10.2337/diacare.18.8.1124. [DOI] [PubMed] [Google Scholar]
- 25.Ashton C, Haldet P, Paterniti D, et al. Racial and ethnic disparities in the use of health services. J Gen Intern Med. 2003;18:1–7. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Starfield B, Steinwachs D, Morris I, Bause G, Siebert S, Westin C. Patient–doctor agreement about problems needing follow-up visit. JAMA. 1979;242:344–6. [PubMed] [Google Scholar]
- 27.Starfield B, Wray C, Hess K, Gross R, Birk PS, D'Lugoff BC. The influence of patient–practitioner agreement on outcome of care. Am J Public Health. 1981;71:127–31. doi: 10.2105/ajph.71.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freidin RB, Goldman L, Cecil RR. Patient–physician concordance in problem identification in the primary care setting. Ann Intern Med. 1980;93:490–3. doi: 10.7326/0003-4819-93-3-490. [DOI] [PubMed] [Google Scholar]
- 29.Helman CG. Communication in primary care: the role of patient and practitioner explanatory models. Soc Sci Med. 1985;20:923–31. doi: 10.1016/0277-9536(85)90348-x. [DOI] [PubMed] [Google Scholar]
- 30.Kwoh CK, O'Connor GT, Regan-Smith MG, et al. Concordance between clinician and patient assessment of physical and mental health status. J Rheumatol. 1992;19:1031–7. [PubMed] [Google Scholar]
- 31.Bogardus ST, Bradley EH, Williams CS, Maciejewski PK, van Doorn C, Inouye SK. Goals for the care of frail older adults: do caregivers and clinicians agree? Am J Med. 2001;110:97–102. doi: 10.1016/s0002-9343(00)00668-9. [DOI] [PubMed] [Google Scholar]
- 32.Hunt LM, Pugh J, Valenzuela M. How patients adapt diabetes self-care recommendations in everyday life. J Family Pract. 1998;46:207–15. [PubMed] [Google Scholar]
- 33.Boyer BA, Lerman C, Shipley TE, Jr, McBrearty J, Quint A, Goren E. Discordance between physician and patient perceptions in the treatment of diabetes mellitus: a pilot study of the relationship to adherence and glycemic control. Diabetes Educ. 1996;22:493–9. doi: 10.1177/014572179602200509. [DOI] [PubMed] [Google Scholar]
- 34.Cohen MZ, Reimer TT, Smith C, Sorofman B, Lively S. Explanatory models of diabetes: patient practitioner variation. Soc Sci Med. 1994;38:59–66. doi: 10.1016/0277-9536(94)90300-x. [DOI] [PubMed] [Google Scholar]
- 35.Gillespie CR, Bradley C. Causal attributions of doctor and patients in a diabetes clinic. Br J Clin Psychol. 1988;27:67–76. doi: 10.1111/j.2044-8260.1988.tb00754.x. [DOI] [PubMed] [Google Scholar]
- 36.Lorig KR, Sobel DS, Stewart AL, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37:5–14. doi: 10.1097/00005650-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Wagner EH. Meeting the needs of chronically ill people. BMJ. 2001;323:945–6. doi: 10.1136/bmj.323.7319.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hunt LM, Arar NH, Larme AC. Contrasting patient and practitioner perspectives in type 2 diabetes management. West J Nurs Res. 1998;20:656–76. doi: 10.1177/019394599802000602. [DOI] [PubMed] [Google Scholar]
- 39.Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight-loss maintenance. J Pers Soc Psychol. 1996;70:115–26. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- 40.Deber RB, Kraetschmer N, Irvine J. What role do patients wish to play in treatment decision making? Arch Intern Med. 1996;156:1414–20. [PubMed] [Google Scholar]
- 41.Beisecker AE, Beisecker TD. Patient information-seeking behaviors when communicating with doctors. Med Care. 1990;28:19–28. doi: 10.1097/00005650-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 42.Strull WM, Lo B, Charles G. Do patients want to participate in medical decision making? JAMA. 1984;252:2990–4. [PubMed] [Google Scholar]
- 43.Ruggiero L, Glasgow R, Dryfoos JM, et al. Diabetes self-management. Self-reported recommendations and patterns in a large population. Diabetes Care. 1997;20:568–76. doi: 10.2337/diacare.20.4.568. [DOI] [PubMed] [Google Scholar]
- 44.Stewart AL, Napoles-Springer A, Perez-Stable EJ. Interpersonal processes of care in diverse populations. Milbank Q. 1999;77:274. doi: 10.1111/1468-0009.00138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient–physician relationship. JAMA. 1999;282:583–9. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 46.Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23:943–50. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- 47.Goodall TA, Halford WK. Self-management of diabetes mellitus: a critical review. Health Psychol. 1991;10:1–8. doi: 10.1037//0278-6133.10.1.1. [DOI] [PubMed] [Google Scholar]
- 48.Fleiss JL. Statistical Methods for Rates and Proportions. New York: Wiley and Sons; 1981. [Google Scholar]
- 49.Huber P. The behavior of maximum likelihood estimates under non-standard conditions. Proc Fifth Berkeley Symp Mathemat Statistics Probability. 1967;1:221–3. [Google Scholar]
- 50.White H. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica. 1980;40:817–30. [Google Scholar]
- 51.Berger M, Muhlhauser I. Diabetes care and patient-oriented outcomes. JAMA. 1999;281:1676–8. doi: 10.1001/jama.281.18.1676. [DOI] [PubMed] [Google Scholar]
- 52.Glasgow RE, Boles SM, Calder D, Dreyer L, Bagdade J. Diabetes care practices in primary care: results from two samples and three measurement sets. Diabetes Educ. 1999;25:755–63. doi: 10.1177/014572179902500508. [DOI] [PubMed] [Google Scholar]
- 53.Glasgow RE, Strycker LA. Preventive care practices for diabetes management in two primary care samples. Am J Prev Med. 2000;19:9–14. doi: 10.1016/s0749-3797(00)00157-4. [DOI] [PubMed] [Google Scholar]
- 54.Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med. 2003;138:593–602. doi: 10.7326/0003-4819-138-7-200304010-00018. [DOI] [PubMed] [Google Scholar]
- 55.Daltroy LH. Doctor–patient communication in rheumatological disorders. Baillieres Clin Rheumatol. 1993;7:221–39. doi: 10.1016/s0950-3579(05)80087-1. [DOI] [PubMed] [Google Scholar]
- 56.Larme AC, Pugh JA. Attitudes of primary care providers toward diabetes: barriers to guideline implementation. Diabetes Care. 1998;21:1391–6. doi: 10.2337/diacare.21.9.1391. 0149–5992. [DOI] [PubMed] [Google Scholar]
- 57.Peyrot M, McMurry JF, Hedges R. Living with diabetes: the role of personal and professional knowledge in symptom and regimen management. Res Sociol Health. 1987;6:107–46. [Google Scholar]
- 58.Harris MA, Wysocki T, Sadler M, et al. Validation of a structured interview for the assessment of diabetes self-management. Diabetes Care. 2000;23:1301–4. doi: 10.2337/diacare.23.9.1301. [DOI] [PubMed] [Google Scholar]
- 59.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002;288:756–64. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]