Abstract
BACKGROUND
While religious involvement is associated with improvements in health, little is known about the relationship between church participation and health care practices.
OBJECTIVES
To determine 1) the prevalence of church participation; 2) whether church participation influences positive health care practices; and 3) whether gender, age, insurance status, and levels of comorbidity modified these relationships.
DESIGN
A cross-sectional analysis using survey data from 2196 residents of a low-income, African-American neighborhood.
MEASUREMENTS
Our independent variable measured the frequency of church attendance. Dependent variables were: 1) Pap smear; 2) mammogram; and 3) dental visit—all taking place within 2 years; 4) blood pressure measurement within 1 year, 5) having a regular source of care, and 6) no perceived delays in care in the previous year. We controlled for socioeconomic factors and the number of comorbid conditions and also tested for interactions.
RESULTS
Thirty-seven percent of community members went to church at least monthly. Church attendance was associated with increased likelihood of positive health care practices by 20% to 80%. In multivariate analyses, church attendance was related to dental visits (odds ratio [OR], 1.5; 95% confidence interval [CI], 1.3 to 1.9) and blood pressure measurements (OR, 1.6; 95% CI, 1.2 to 2.1). Insurance status and number of comorbid conditions modified the relationship between church attendance and Pap smear, with increased practices noted for the uninsured (OR, 2.3; 95% CI, 1.2 to 4.1) and for women with 2 or more comorbid conditions (OR, 1.9; 95% CI, 1.1 to 3.5).
CONCLUSION
Church attendance is an important correlate of positive health care practices, especially for the most vulnerable subgroups, the uninsured and chronically ill. Community- and faith-based organizations present additional opportunities to improve the health of low-income and minority populations.
Keywords: church attendance, health care services, health care practices, preventive services, religiosity
The African-American church often occupies a central place in the lives of African Americans.1 Public health practitioners, researchers, and policy makers recognize this role and are increasingly using the church to access African Americans for health improvement efforts.1,2 Moreover, there is growing evidence that religious involvement, in addition to providing greater access to health intervention, exerts positive and diverse health benefits for African Americans.1–11
Research on religious involvement or religiosity describes three types of involvement.1,2,12 Organizational religious involvement refers to formal or public participation of individuals in religious congregations. These include church attendance and prayer meetings. Non-organizational involvement refers to a person's private devotional acts and includes Bible reading and prayer. Subjective religious involvement describes a person's self-perception or self-presentation as religious. Spirituality, a related concept, refers to a basic or inherent quality in all humans that involves a “belief in something greater than the self and a faith that positively affirms life.”13 A growing body of literature attempts to operationalize these concepts and clarify the relationship between spirituality and religiosity.13
Religious participation reduces the mortality risks5,8,10,14,15 and improves health status6,7 and quality of life for African Americans.6,7,13–16 A longitudinal study of white and black Americans showed that those who attended church weekly had reduced mortality risk as compared to those who attended church less frequently, even after controlling for demographic characteristics, health conditions, social connections, and health practices.8 Another, large, 9-year, prospective study that used a nationally representative sample showed similar results.5 The magnitude of the protective effect of religious attendance on survival is comparable to that of such commonly recommended personal health habits, such as physical activity and reduced alcohol consumption.10 With respect to health status, Steffen et al.7 showed that religious involvement was importantly related to ambulatory blood pressure levels for black, but not white, Americans. Higher levels of religiousness were associated with lower awake and sleep blood pressure, independent of social support. This study confirmed earlier findings by Livingston et al.6 that showed that religious affiliation was associated with lower blood pressure in African Americans. Religiousness is also related to several improvements in quality-of-life indicators; these include a more optimistic life orientation,16 greater perceived social support,16 improved life satisfaction,17 improved adjustment to chronic diseases,16 and higher resilience to stress and lower levels of anxiety.16
Research into pathways that may underpin the religiousness-health relationship is underway. The pathways include: 1) improved health behaviors and lifestyle3,4,11,18; 2) better religious coping strategies and resources9,15,16; 3) enhanced social resources5; 4) improved psychological resources such as self-esteem, personal efficacy, and self-worth18,19; and 5) positive emotions and beliefs.17 Several studies have demonstrated that religious participation is related to health behaviors, especially for women. For example, Strawbridge's prospective study10 showed that religious involvement was associated with improving and maintaining health behaviors related to tobacco use, alcohol consumption, and physical activity over a 30-year period, with women showing larger gains than men. Another study of both black and white men and women revealed that religious and civic group participation predicted good smoking, alcohol, and physical activity behaviors for African-American women only.4 While the studies of both Strawbridge and Gallant are longitudinal, these studies used small samples of African Americans and primarily assessed lifestyle behaviors and not patients' health system-related behaviors; these health care practices have received little attention.
The poorer health outcomes for African Americans have been partially attributed to low rates of recommended health services. For African Americans, we know little about the relationship between religious involvement and health care practices. A notable exception is a 1993 study by Kang and Bloom20 that demonstrated a positive effect on cancer screening. Confirming such a relationship would increase our understanding of the effect of church participation on health care. If church participation improves cancer screening, does it also improve other health care practices, such as blood pressure measurement or dental services? Furthermore, are the positive effects limited to specific groups of African Americans, such as women, those without health insurance, the chronically ill, and the elderly? It is possible that church participation helps to compensate for other risk factors, such as lack of insurance, poor health status, or older age. The role of religious involvement in improving health care practices is important for African Americans, as health practitioners and policy makers work on reducing health care disparities.
This study explored the relationship between church participation and health care practices in a large, African-American, low-income community. We determined 1) the prevalence of church participation; 2) whether church participation influenced positive health care practices; and 3) how church participation interacted with gender, age, insurance status, and levels of comorbidity.
METHODS
Data Source
Data were collected during a neighborhood survey to identify and recruit adults with high blood pressure to participate in a community-based trial to improve high blood pressure care and control in an inner-city African-American community. All adults 18 years of age and older were eligible for the survey. The survey used a stratified sampling method that divided the neighborhood into 3 districts. Surveyors canvassed the neighborhood during daytime, evening, and weekend hours to enter functioning households. Almost half of the households that were eligible to be interviewed were accessed by interviewers. Non-entry into households was primarily due to these households being vacant and or condemned. Of the households that were accessed, 80% of the adults completed the interviews. See Bone et al.21 for more details of the neighborhood survey.
The survey included sociodemographic information and a general health interview. The sociodemographic information included age, gender, educational attainment, employment status, marital status, and church attendance. The general health interview survey assessed perceived health status, morbidity, health care utilization, and health insurance.
Variables
We constructed the independent variable, frequency of church attendance, from responses to the following two questions: 1) “do you ever attend church or religious services” and 2) “if attend, how often do [you] attend church or religious services?” The response categories were high attendance, that is attending church “every week of the month”; moderate attendance represented “twice a month” or “once a month attendance”; and low attendance. Low attendance included those who attended church “a few times a year,”“never attended church,” or “used to attend church” but were not currently doing so.
Our dependent variables included the following 6 health care practices: 1) a Pap smear within 2 years; 2) a mammogram within 2 years; 3) a dental visit within 2 years; 4) a blood pressure measurement within 1 year; 5) a regular source of care; and 6) no perceived delays in care in the previous year. Respondents who responded “no” to the question “during the past year, were there times you thought you should go to the doctor and didn't” were considered to have no perceived delays in care.
Analysis
For each outcome, we conducted bivariate analysis with the independent variable using a χ2 test of independence. We then conducted multivariate logistic regression, controlling for demographic variables, number of comorbid conditions, insurance status, and regular source of care. We did not control for regular source of care when it was the dependent variable. We also assessed whether church attendance had different effects on health care practices in different risk groups. Therefore, we tested sequentially for interactions between church attendance and age, gender, comorbid conditions, and insurance status. The level of significance used was P < .05.
Conflict of Interest
There is no potential conflict of interest. There are no financial and personal relationships between the authors and others that might bias this work. The authors accept full responsibility for the integrity of the data and the accuracy of the data analysis. The Institutional Review Board approved the study.
RESULTS
Two thousand, one hundred ninety-six adults completed the survey. Those surveyed had a mean age of 44 years; 37% were male, 45% had a high school education or less, 21% were married, 37% had part- or full-time employment, and 25% had two or more chronic conditions. Three quarters or more reported having health insurance or a regular source of care.
About 37% of the respondents reported that they attended church at least once a month. Of the 818 respondents who attended church at least monthly or regularly, 462 attended weekly and 356 attended once or twice a month. The low attendees were those who attended less than once a month (N = 1,378) and included those who attended church a few times or less (42%) a year and those who either never or no longer attended church (58%). Compared to those who did not attend church regularly, those who did were older, more likely to be female, married, employed, and to have health insurance.
In unadjusted analyses (Table 1), church attendance is associated with increased reporting of all of the health care practices. Church attendance increased these practices by 20% to 80%. For example, respondents who attended church regularly were more likely to have a dental visit (OR, 1.7; 95% confidence interval [CI], 1.4 to 2.0), blood pressure measurement (OR, 1.8; 95% CI, 0.9 to 2.4), or a regular source of care (OR, 1.6; 95% CI, 1.2 to 2.1) than those who did not attend church regularly. Also, while there was a tendency for church attendance to increase the likelihood of Pap tests and mammograms, these increases did not meet statistical significance.
Table 1.
The Effect of Church Attendance and Other Covariates on Health Care Practices, Fully Adjusted Models
| Odds Ratio, 95% CI | ||||||
|---|---|---|---|---|---|---|
| Independent Variables | Pap | Mammogram | Dental | Blood Pressure | Regular Source of Care | No Delays in Care |
| Church attendance | 1.2 (0.9 to 1.9) | 1.4 (0.9 to 2.2) | 1.5 (1.3 to 1.8) | 1.6 (1.2 to 2.1) | 1.2 (0.9 to 1.7) | 1.1 (0.9 to 1.4) |
| Age, ≥65 | 0.4 (0.2 to 0.6) | 0.6 (0.4 to 1.1) | 0.6 (0.4 to 0.8) | 1.0 (0.7 to 1.8) | 1.0 (0.6 to 1.9) | 1.9 (1.4 to 2.6) |
| Female | – | – | 1.4 (1.1 to 1.7) | 1.0 (0.7 to 1.8) | 2.5 (1.8 to 3.4) | 0.8 (0.6 to 0.9) |
| Completed high school | 1.5 (1.1 to 2.0) | 1.1 (0.7 to 1.8) | 1.7 (1.4 to 2.0) | 1.2 (1.0 to 1.7) | 1.1 (0.8 to 1.4) | 1.1 (0.9 to 1.4) |
| Married | 1.4 (1.0 to 2.1) | 0.9 (0.5 to 1.6) | 1.0 (0.8 to 1.2) | 0.8 (0.6 to 1.1) | 0.9 (0.6 to 1.2) | 0.9 (0.7 to 1.0) |
| Employed full or part time | 1.1 (0.8 to 1.6) | 0.8 (0.4 to 1.6) | 1.5 (1.2 to 1.8) | 0.9 (0.7 to 1.2) | 0.8 (0.6 to 1.0) | 1.1 (0.9 to 1.4) |
| Two or more comorbidities | 0.9 (0.7 to 1.3) | 1.6 (1.0 to 2.7) | 1.0 (0.8 to 1.2) | 1.0 (0.8 to 1.2) | 1.5 (1.0 to 2.3) | 0.7 (0.6 to 1.0) |
| Has insurance | 2.4 (1.7 to 3.4) | 2.0 (1.3 to 3.8) | 2.0 (1.6 to 2.5) | 2.0 (1.4 to 2.6) | 11.2 (8.0 to 15.5) | 1.4 (1.1 to 1.8) |
| Has a regular source of care | 3.0 (1.8 to 4.9) | 4.9 (1.0 to 13.1) | 1.9 (1.4 to 2.7) | 1.9 (1.4 to 2.7) | – | 1.3 (1.0 to 1.8) |
CI, confidence interval.
For some practices, the effect of church attendance persisted in multivariate analyses. Regular church attendance increased the likelihood of dental visits (OR, 1.5; 95% CI, 1.3 to 1.9) and blood pressure measurement (OR, 1.6; 95% CI, 1.2 to 2.1). However, the effect of church participation on having a mammogram (OR, 1.4; 95% CI, 0.9 to 2.2) and a regular source of care (OR, 1.2; 95% CI, 0.9 to 1.7) were not statistically significant.
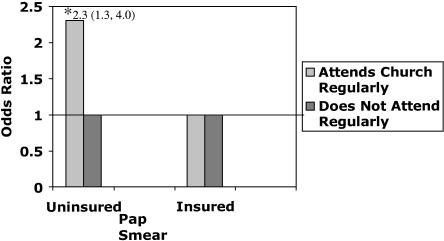
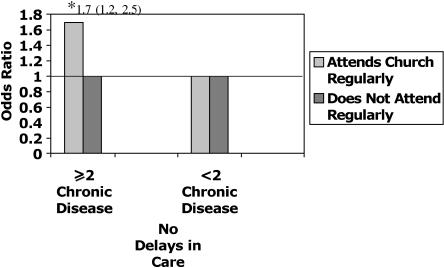
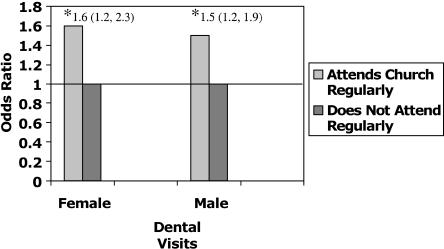
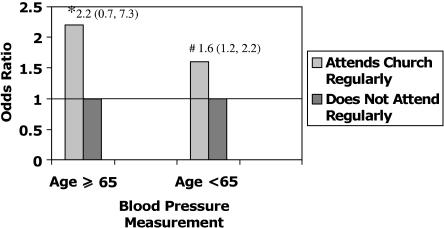
Significant interactions were found for the effect of church participation by subgroup status. There was a significant interaction between church attendance and insurance status for Pap smear. As displayed in Figure 1, church attendance more than doubled the likelihood of having a Pap smear in women who were uninsured (OR, 2.3; 95% CI, 1.2 to 4.1), but had no effect on those women with insurance (OR, 1.0; 95% CI, 0.7 to 1.4). For uninsured women, the relationship between church attendance (OR, 2.3; 95% CI, 1.2 to 4.1) and Pap smear was as important as that between having a regular source of care (OR, 2.5; 95% CI, 1.4 to 4.5) and Pap smear. Similarly, level of comorbidity modified the relationship between church attendance and Pap smear. Church status nearly doubled the likelihood (OR, 1.9; 95% CI, 1.1 to 3.5) of having a Pap smear for women with 2 or more chronic conditions, but had no effect on those with fewer than 2 conditions. For the sicker subgroup of women, while the effect of church status (OR, 1.9; 95% CI, 1.1 to 3.5) and insurance (OR, 2.3; 95% CI, 1.1 to 4.7) on Pap smear receipt were similar, having a regular source of care (OR, 7.3; 95% CI, 2.3 to 22.2) had a much more powerful effect. As displayed in Figure 2, there was also a significant interaction between church attendance and level of comorbidity for no perceived delays in seeking care. Church attendance was associated with increased rates of having no perceived delays in seeking care for the sicker subgroup (OR, 1.7; 95% CI, 1.2 to 2.5); there was no association for the less sick subgroup. There was no interaction between church attendance and age and gender (Figs. 3 and 4).
Figure 1.
Odds ratio and confidence intervals for the effect of church attendance and insurance status on Pap smear. * P = .004, fully adjusted models.
Figure 2.
Odds ratio and confidence intervals for the effect of church attendance and level of comorbidity on no delays in care. * P = .027, fully adjusted models.
Figure 3.
Odds ratio and confidence intervals for the effect of church attendance by gender on dental visits. * P ≤ .005, fully adjusted models.
Figure 4.
Odds ratio and confidence intervals for the effect of church attendance by age on blood pressure measurement. * P = .20, #P = .003, fully adjusted models.
As expected, insurance status and having a regular source of care were the most powerful predictors of positive health care practices. As Table 1 shows, among sociodemographic variables, church attendance was equivalent to or more important than other traditional sociodemographic variables. For example, church attendance (OR, 1.6; 95% CI, 1.2 to 2.4) had a stronger effect than educational achievement (OR, 1.3; 95% CI, 1.0 to 1.6) on blood pressure measurement.
DISCUSSION
In an African-American, low-income community, about one third of the residents attend church regularly. Church attendance was associated with multiple positive health care practices. Those who attended church were 20% to 80% more likely to report practices such as mammogram, blood pressure measurements, and dental visits than their counterparts who did not attend church. Even after sociodemographic characteristics were taken into account, church attendance continued to be associated with modest and large increases in some practices. Moreover, even when there was no important overall benefit, church attendance was very important for some subpopulations. For high-risk groups, such as the uninsured or the chronically ill, church status was importantly associated to whether a respondent received a Pap smear or experienced no delays in care. The effect of church attendance was equivalent to or more important than most traditional sociodemographic and economic variables, except for insurance status or a regular source of care.
Consistent with the findings from earlier studies,4,10,20 this study showed a positive association between religious involvement and health and health care. Kang's cross-sectional study23 demonstrated a positive relationship between social integration (a composite measure that included church affiliation) and 2 of 6 cancer prevention services in approximately 600 African-American women. The use of a composite measure and different study outcomes may explain the differences between the study of Kang20 and our own. Our study suggests that religious involvement confers survival benefits to participants by improving health care practices.
This study is also unique in that it explores the relationship between church participation and a diverse group of health care practices in a mixed-gender African-American population. While the prevalence of church participation was lower than the previously reported national average of 52%,22 church participation increased the likelihood of positive health care practices. In addition, the strength of the relationships varied among the practices and for at-risk subpopulations. We hypothesized that church participation would effect greater benefit for the more vulnerable subpopulations. Our study did not show the gender-specific effect of that prior work 4,10,11 on church attendance supports. This absence may be due to differences in populations and outcomes. For example, Strawbridge's11 study of church attendance used a community sample that was 8% African American and did not include subgroup analyses for African Americans. In addition, the studies of both Gallant4 and Strawbridge11 assessed personal health habits and not health care practices.
For this low-income community, church participation increased the likelihood of a wide array of health care practices. These practices are diverse in several respects—some of the practices (Pap smear, blood pressure, and mammogram) are nationally recommended procedures, some (regular source of care and no delays in care) capture the nature of relationships that patients have with the health system, and others (blood pressure measurement and mammograms) are delivered in traditional fee-based or insurance-based health systems, as well as in community or lay settings such as health fairs or churches at no cost to the patient. If attending religious services does affect health care practices, what are the potential reasons for this association? Church attendance may exert its positive effects through a number of pathways. First, church attendance may provide social support that facilitates and reinforces positive health-seeking behaviors. A large body of literature points to the African-American church providing social support for its members.23,24 Religious adherents may be more likely to adopt healthy practices because of the church's emphasis on respect for the body.25 In addition, the church may provide access to services serving as a site of service delivery (direct access) or providing information on available services (indirect access). Church attendance may increase attendees' self-efficacy about their health promotion.9,26–28
Our study has several limitations. The high household vacancy rate in this community suggests that residents with unstable housing, the homeless, or near homeless were underrepresented in our study. A comparison of nonparticipants and participants, however, revealed that there were no differences in sociodemographic characteristics and self-reported high blood pressure. Second, we cannot draw conclusions about causality from this cross-sectional study. We also cannot comment on the long-term effects of church participation. Third, our study looked at organizational religiosity and did not address nonorganization and subjective religiosity and spirituality. We therefore cannot comment on the relationship between the other types of religiosity and spirituality and these health care practices. There is an ongoing debate as to whether spirituality mediates the effect of organizational religiosity on health.13 People may be highly spiritual yet have no church affiliation. In addition, some consider religious participation a barrier to spirituality. Finally, while we have information on the frequency of attendance, we have no information about the nature of the experiences and are limited in our ability to explain these associations.
This study suggests that attendance at church may improve the health status of urban African Americans by increasing the likelihood of preventive health practices. Importantly, this benefit is particularly observed among those most in need—the uninsured and chronically ill. Our study has several important policy implications. First, public health programs that aim to reach low-income residents may be strengthened through collaboration with churches. The church may extend the reach of these programs to church attendees. These programs could also build on the church's traditional commitment to reach out to nonattendees,3,23 the community outside its congregation, by using lay health workers in these partnerships. This model could help extend the health benefits seen within the church to noncongregants. Faith-based and community initiatives at the federal and state level may facilitate these partnerships. Second, these partnerships are not limited to service delivery but increasingly, community-based organizations, including churches, and local leaders are involved in participatory research efforts to improve community health and health care. In addition, this study demonstrates that the African-American church may contribute informally to the health care safety net in low-income communities. The church's role in supporting the safety net may become more prominent as the number of uninsured Americans increases and term limits for welfare recipients expire. Third, in addition to assessing patients' spirituality, clinicians may use church status to identify low-income persons who are at risk for not maintaining preventive health care practices and are in need of preventive services. For this high-risk group, clinicians could use every clinical encounter to assess status of preventive services and provide such services.29 Finally, while the church represents an important though informal partner in the health care safety net, it should not be the sole strategy. Because churches do not reach a substantial segment of low-income communities, additional community-based strategies, including the use of community health outreach workers, need to be employed in public programs aimed at reaching low-income communities.
While faith- and community-based strategies are getting more attention from policy makers, further research on the effect of faith- and other community-based strategies is needed to understand how to improve health and health care practices among patients who are often locked out of the traditional health care system. Additional research is needed to clarify the role of the church in Latino or rural communities and the relationship among other aspects of religiosity and spirituality and health.
Acknowledgments
Funding: This is a substudy of a randomized clinical trial that was funded by The National Heart, Lung, and Blood Institute, grant number HL511-01. Work supported by the Agency for Healthcare Research and Quality.
REFERENCES
- 1.Chatters LM, Levin JS, Ellison CG. Public health and health education in faith communities. Health Educ Behav. 1998;25:689–99. doi: 10.1177/109019819802500602. [DOI] [PubMed] [Google Scholar]
- 2.Chatters LM. Religion and health: public health research and practice. Annu Rev Public Health. 2000;21:335–67. doi: 10.1146/annurev.publhealth.21.1.335. [DOI] [PubMed] [Google Scholar]
- 3.Campbell MK, Motsinger BM, Ingram A, et al. The North Carolina Black Churches United for Better Health Project: intervention and process evaluation. Health Educ Behav. 2000;27:241–53. doi: 10.1177/109019810002700210. [DOI] [PubMed] [Google Scholar]
- 4.Gallant MP, Dorn GP. Gender and race differences in the predictors of daily health practices among older adults. Health Educ Res. 2001;16:21–31. doi: 10.1093/her/16.1.21. [DOI] [PubMed] [Google Scholar]
- 5.Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and U.S. adult mortality. Demography. 1999;36:273–85. [PubMed] [Google Scholar]
- 6.Livingston IL, Levine DM, Moore RD. Social integration and black intraracial variation in blood pressure. Ethn Dis. 1991;1:135–49. [PubMed] [Google Scholar]
- 7.Steffen PR, Hinderliter AL, Blumenthal JA, Sherwood A. Religious coping, ethnicity, and ambulatory blood pressure. Psychosom Med. 2001;63:523–30. doi: 10.1097/00006842-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Strawbridge WJ, Cohen RD, Shema SJ, Kaplan GA. Frequent attendance at religious services and mortality over 28 years. Am J Public Health. 1997;87:957–61. doi: 10.2105/ajph.87.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Strawbridge WJ, Shema SJ, Cohen RD, Roberts RE, Kaplan GA. Religiosity buffers effects of some stressors on depression but exacerbates others. J Gerontol B Psychol Sci Soc Sci. 1998;53:118S–126S. doi: 10.1093/geronb/53b.3.s118. [DOI] [PubMed] [Google Scholar]
- 10.Strawbridge WJ, Cohen RD, Shema SJ. Comparative strength of association between religious attendance and survival. Int J Psychiatry Med. 2000;30:299–308. doi: 10.2190/ECB2-0Q3M-333C-GK62. [DOI] [PubMed] [Google Scholar]
- 11.Strawbridge WJ, Shema SJ, Cohen RD, Kaplan GA. Religious attendance increases survival by improving and maintaining good health behaviors, mental health, and social relationships. Ann Behav Med. 2001;23:68–74. doi: 10.1207/s15324796abm2301_10. [DOI] [PubMed] [Google Scholar]
- 12.Koenig HG. Religion and medicine I: historical background and reasons for separation. Int J Psychiatry Med. 2000;30:385–98. doi: 10.2190/2RWB-3AE1-M1E5-TVHK. [DOI] [PubMed] [Google Scholar]
- 13.Musgrave CF, Allen CE, Allen GJ. Spirituality and health for women of color. Am J Public Health. 2002;92:557–60. doi: 10.2105/ajph.92.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Helm HM, Hays JC, Flint EP, Koenig HG, Blazer DG. Does private religious activity prolong survival? A six-year follow-up study of 3,851 older adults. J Gerontol A Biol Sci Med Sci. 2000;55:M400–M405. doi: 10.1093/gerona/55.7.m400. [DOI] [PubMed] [Google Scholar]
- 15.Koenig HG. An 83-year-old woman with chronic illness and strong religious beliefs. JAMA. 2002;288:487–93. doi: 10.1001/jama.288.4.487. [DOI] [PubMed] [Google Scholar]
- 16.Pardini DA, Plante TG, Sherman A, Stump JE. Religious faith and spirituality in substance abuse recovery: determining the mental health benefits. J Subst Abuse Treat. 2000;19:347–54. doi: 10.1016/s0740-5472(00)00125-2. [DOI] [PubMed] [Google Scholar]
- 17.Levin JS, Chatters LM, Taylor RJ. Religious effects on health status and life satisfaction among black Americans. J Gerontol B Psychol Sci Soc Sci. 1995;50:154S–163S. doi: 10.1093/geronb/50b.3.s154. [DOI] [PubMed] [Google Scholar]
- 18.Bourjolly JN. Differences in religiousness among black and white women with breast cancer. Soc Work Health Care. 1998;28:21–39. doi: 10.1300/J010v28n01_02. [DOI] [PubMed] [Google Scholar]
- 19.Levin JS, Chatters LM. Religion, health, and psychological well-being in older adults: findings from three national surveys. J Aging Health. 1998;10:504–31. doi: 10.1177/089826439801000406. [DOI] [PubMed] [Google Scholar]
- 20.Kang SH, Bloom JR. Social support and cancer screening among older black Americans. J Natl Cancer Inst. 1993;85:737–42. doi: 10.1093/jnci/85.9.737. [DOI] [PubMed] [Google Scholar]
- 21.Bone LR, Hill MN, Stallings R, et al. Community health survey in an urban African-American neighborhood: distribution and correlates of elevated blood pressure. Ethn Dis. 2000;10:87–95. [PubMed] [Google Scholar]
- 22.Taylor RJ, Ellison CG, Chatters LM, Levin JS, Lincoln KD. Mental health services in faith communities: the role of clergy in black churches. Soc Work. 2000;45:73–87. doi: 10.1093/sw/45.1.73. [DOI] [PubMed] [Google Scholar]
- 23.Davis DT, Bustamante A, Brown CP, et al. The urban church and cancer control: a source of social influence in minority communities. Public Health Rep. 1994;109:500–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Eng E, Hatch JW. Networking between agencies and black churches: The lay health advisor model. Pre Hum Serv. 1991;10:123–46. [Google Scholar]
- 25.Whooley MA, Boyd AL, Gardin JM, Williams DR. Religious involvement and cigarette smoking in young adults: the CARDIA study. Arch Intern Med. 2002;162:1604–10. doi: 10.1001/archinte.162.14.1604. [DOI] [PubMed] [Google Scholar]
- 26.Pargament KI, Ensing DS, Falgout K, et al. God help me: religious coping efforts as predictors of outcomes to significant negative life events. Am J Community Psychol. 1990;18:793–824. [Google Scholar]
- 27.Mendes de Leon CF, Seeman TE, Baker DI, Richardson ED, Tinetti ME. Self-efficacy, physical decline, and change in functioning in community-living elders: a prospective study. J Gerontol B Psychol Sci Soc Sci. 1996;51:183S–190S. doi: 10.1093/geronb/51b.4.s183. [DOI] [PubMed] [Google Scholar]
- 28.Seeman T, McAvay G, Merrill S, Albert M, Rodin J. Self-efficacy beliefs and change in cognitive performance: MacArthur Studies of Successful Aging. Psychol Aging. 1996;11:538–51. doi: 10.1037//0882-7974.11.3.538. [DOI] [PubMed] [Google Scholar]
- 29.Rossman ML. Should a doctor ask about a patient's spiritual beliefs? Adv Mind Body Med. 2001;17:101–3. [PubMed] [Google Scholar]