Abstract
OBJECTIVE
To assess the effect of providing structured information about the benefits and harms of mammography in differing frames on women's perceptions of screening.
DESIGN
Randomized control trial.
SETTING
General internal medicine academic practice.
PARTICIPANTS
One hundred seventy-nine women aged 35 through 49.
INTERVENTION
Women received 1 of 3 5-minute videos about the benefits and harms of screening mammography in women aged 40 to 49. These videos differed only in the way the probabilities of potential outcomes were framed (positive, neutral, or negative).
MEASUREMENTS AND MAIN RESULTS
We measured the change in accurate responses to questions about potential benefits and harms of mammography, and the change in the proportion of participants who perceived that the benefits of mammography were more important than the harms. Before seeing the videos, women's knowledge about the benefits and harms of mammography was inaccurate (82% responded incorrectly to all 3 knowledge questions). After seeing the videos, the proportion that answered correctly increased by 52%, 43%, and 30% for the 3 knowledge questions, respectively, but there were no differences between video frames. At baseline, most women thought the benefits of mammography outweighed the harms (79% positive frame, 80% neutral frame, and 85% negative frame). After the videos, these proportions were similar among the 3 groups (84%, 81%, 83%, P = .93).
CONCLUSIONS
Women improved the accuracy of their responses to questions about the benefits and harms of mammography after seeing the videos, but this change was not affected by the framing of information. Women strongly perceived that the benefits of mammography outweighed the harms, and providing accurate information had no effect on these perceptions, regardless of how it was framed.
Keywords: decision making, informed consent, mammography, physician-patient relations
Controversy surrounds the use of screening mammography in women aged 40 to 49.1–4 On average, for women in their forties, the magnitude of the benefits and harms do not differ greatly. Making blanket recommendations for mammography screening for women in this age range has been difficult.5,6 Consequently, women must weigh the likelihood and value of potential outcomes in deciding whether or not to get screening mammograms. Because the value women place on these outcomes varies, many experts suggest that women and their providers decide together, after an informed discussion about the potential benefits and harms.7–10 Despite these recommendations, little empiric evidence exists about how physicians should present this information to women or how women perceive this information.11,12
Adequately informing women about the benefits and harms of mammography may challenge providers for several reasons.4,11 First, women have preconceived ideas about breast cancer risk and the benefits of mammography, some of which may be inaccurate.13–15 Second, lay articles in the popular press may increase women's fear of breast cancer.16–18 And finally, to precisely inform women about the benefits and harms, physicians must present probabilistic information. Women's understanding of such information will be influenced by their “numeracy,” or ability to understand quantitative information.19
Standardized presentations of information about mammography can help to overcome these barriers. Tailored information for women aged 40 to 45 and 50 to 55 improved women's knowledge about mammography and increased adherence to screening.20 A decision aid about mammography for women over age 50 demonstrated that women of various educational levels were able to comprehend information about the risks and benefits of mammography.12 Neither of these studies addressed whether the framing of information influenced perceptions or decisions about mammography.
Presenting equivalent information in terms of the chance of an outcome occurring versus the chance of an outcome not occurring is one way that information can be framed. This type of framing has not consistently been shown to affect decision making in clinical settings.21,22 In McNeil's classic study, more people given a choice between surgery and radiation for lung cancer chose radiation if the mortality from surgery was presented as a 10% chance of dying versus a 90% chance of survival.23 However, other studies in clinical settings have not shown that alternative presentations of probabilities for potential outcomes affected decisions.24–26 These disparate findings may be attributable to the differing contexts of these clinical decisions.26 Therefore, framing may be important for some clinical decisions, requiring physicians to carefully inform patients about potential outcomes using balanced probabilities, while other decisions may not be affected by framing, allowing physicians to use a less-structured approach in their discussions with patients.
We undertook this study to determine whether the presentation of information about mammography in women aged 40 to 49 was subject to a framing effect. In this study, we first examined the preexisting knowledge women have about the potential benefits and harms of mammography for women in their forties. We then assessed the effect of providing women with evidence-based information about the benefits and harms in differing frames on their ability to accurately recall the information and on their perceptions of the balance between the harms and benefits of regular screening.
METHODS
Setting and Patients
We conducted this study in the General Internal Medicine practice at the University of North Carolina from July 1999 to May 2000. Eligible women were aged 35 to 49, had no history of breast cancer, and were able to read and write English. Although screening mammography is not recommended for women aged 35 to 39, we chose to include women of these ages (25% of our sample) because a recent study found that 25% of women in their thirties reported having had a mammogram and intended to get another in the next year.27 Therefore, many women in their thirties may benefit from information about the risks and benefits before they commit to screening.
A research assistant identified potentially eligible participants by reviewing the physicians' daily clinic schedules and approached them prior to the visit with their provider. We did not collect data from women who refused or were not approached. The Committee on the Protection of the Rights of Human Subjects at the University of North Carolina at Chapel Hill approved the study.
Randomization
We generated random assignments using STATA 5.0 (STATA Corp., College Station, TX). Assignments were placed in opaque, sealed envelopes that were numbered sequentially. The research assistant opened sequential envelopes once eligibility and agreement to participate were confirmed. Participants were blinded to the video assignment.
Intervention Development
First, we searched the relevant literature to identify information necessary for women to make an informed decision about mammography. Three key pieces of information emerged: the chance of having one's life extended with mammography; the risk of false positives; and the effect of false positives on women's psychological health.4,8–10,28–30 We identified the probabilities for each of these outcomes in the following articles. For the chance of having one's life extended by mammography, Harris and Leininger9 and Fletcher8 used data from randomized control trials and estimated that for 1,000 women in their forties who undergo screening for 10 years, 1 life would be extended. For the risk of false positives, the Elmore et al. study of women aged 40 to 69 who were members of an HMO found that about one third of women would experience a false positive after 10 years of screening biennially.28 For the consequences of false positives, Lerman et al. demonstrated that more than one third of women with a false positive continued to worry about having breast cancer even after they were aware that the result was a false positive.29 We described a false positive in the videos as “an abnormal mammogram when there is nothing actually wrong, but the result may require more tests or a biopsy to find out that there was no cancer.” We rounded these estimates to whole numbers to make it easier for women to remember the information. We chose to present the information in the videos in the X per 1,000 format because previous research suggests that it is better understood than the 1 in X or NNT format.31
We pretested the presentation of this information in an iterative process with 15 women recruited from the research site, assessing women's understanding of the information with probing questions. As we obtained feedback, we revised the information to make it more understandable.
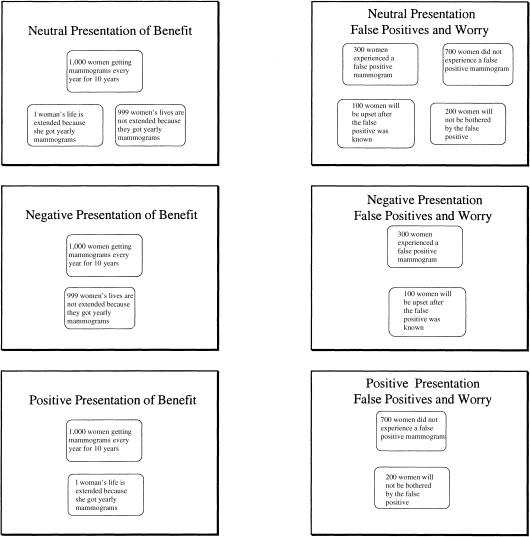
In each video, the same female physician narrator conveyed the messages, while diagrams similar to those shown in Figure 1 were displayed on the screen to reinforce the verbal presentations. Each video lasted approximately 5 minutes.
Figure 1.
Presentations of the benefits and harms of mammography by video.
Based on their random assignment, participants viewed 1 of 3 videos that described the benefits and harms of screening mammography in an imaginary cohort of 1,000 women aged 40 through 49 who undergo 10 years of regular screening. The 3 videos were logically equivalent but differed in the way the probabilities of potential outcomes were framed (Fig. 1). For the positively framed video, women were given information that reported the mortality benefit as the number of lives extended and the false positive information as the number who would not experience the harm. In the negatively framed video, the number of lives not extended and the number of women who would be expected to experience the harm were reported. The neutrally framed video gave both presentations.
Outcome Measures
Women completed baseline questionnaires before viewing the videos and similar questionnaires afterward. The baseline questionnaire assessed demographic information, personal breast cancer risk factors, and history of previous mammography screening. Women's numeracy was measured using a question requiring women to change 40% into 4 out of 10. Women who gave the correct response were considered numerate.
Before we assessed the change in women's perceptions of the benefits and harms of mammography, we wanted to determine whether women “understood” the information. As a proxy for understanding, we measured the change in accurate responses to multiple-choice questions about the potential benefits and harms of mammography. Before and after seeing the videos, women responded to 1 question about the number of lives extended with mammography, 1 question about the number of false positives expected, and 1 question about the number of women who would remain upset by a false positive. All participants received questionnaires with the same set of potential responses. Because the presentation of the benefits and harms differed in each video, some participants were exposed directly to the correct answers in the video, while others were not. Thus, some participants only had to choose the number they heard to get the correct answer on the postvideo questionnaire (direct presentation), while others had to perform subtraction to determine the correct response (indirect presentation). For example, participants receiving the positively framed video saw that mammography led to “1 life extended.” Those receiving the negatively framed video saw “999 lives not extended,” but the response offered to all participants was “1 life extended,” Thus, those who saw the negatively framed video needed to subtract 999 from 1,000 to get the correct answer.
We assessed women's perceptions of mammography before and after the video with a 5-point Likert scale. We asked, “are the benefits of mammography much more (somewhat more) important than the downsides, are the benefits and downsides about equal, are the downsides of mammography somewhat more (much more) important than the benefits?” We assessed 2 main outcomes:
1) The change in the proportion of accurate responses to questions about the potential benefits and harms of mammography; and 2) The change in the proportion of participants who responded that the benefits of mammography were more important than the harms.
Sample Size Calculation
We estimated that approximately 80% of women would believe that the benefits of mammography exceeded the harms before getting the information. To detect a minimum difference of 25% in the beliefs of women who viewed the positive versus the negative videos, we estimated that we would need approximately 54 participants in each arm, given 80% power and 2-sided alpha of 0.05.
Statistical Analysis
We used STATA statistical software, version 5.0, for data analysis and reported characteristics of the participants as frequencies and means. From each woman's self-reported breast cancer risk factors, we calculated for each participant their individual 5-year risk of breast cancer using the Gail model risk equations.32–34 This model estimates breast cancer risk using the following risk factors: age, ethnic group, number of first-degree relatives with breast cancer, age at menarche, age at first live birth, number of breast biopsies, and presence of atypical hyperplasia in the biopsy.
To measure the change in accurate responses to questions about the potential benefits and harms of mammography, we reported the proportion who answered correctly before and after the videos and compared these groups using McNemar's χ2 tests. To compare the correct χ2 responses between the video groups after the video, we used Pearson's χ2 tests.
To determine whether women's perceptions of the balance between the benefits and harms differed after viewing the different frames of information in the 3 videos, we combined Likert responses into 2 categories. Women responding that they somewhat or strongly agree that the benefits were more important than the harms were combined to “agree.” Women who responded that they somewhat or strongly disagree or felt that the benefits and harms were about equal were combined to “disagree.” We compared the proportions of women who agreed that the benefits were more important than the harms with Pearson's χ2 tests. We also assessed the change in these perceptions by performing logistic regression that controlled for baseline perceptions and compared perceptions across videos (positive, negative, and neutral).
To determine whether women who were numerate changed their perceptions more than those who were not, we again used logistic regression controlling for baseline perceptions and compared perceptions after the videos between numerate women and nonnumerate women. We repeated similar analyses for women who answered knowledge questions correctly (those answering 2 or 3 questions correctly versus 0 or 1 questions correctly), for women who had previous mammograms (compared to those who did not), and for women with a 5-year risk of breast cancer greater than or equal to 1.67% (compared to those with a risk of less than 1.67%). We chose a risk of 1.67% because the Breast Cancer Prevention Trial considered women having a 5-year risk of 1.67% or more to be at high risk.35 We calculated corrected relative risks from the odds ratios using methods described by Zhang and Yu.36
This research was supported by the American Cancer Society and the University of North Carolina Lineberger Comprehensive Cancer Center. The funding sources had no role in the design, conduct, or reporting of the study.
RESULTS
We approached 325 women who were potentially eligible to participate. Of these, 109 refused to participate and 36 were found to be ineligible after agreeing to participate. The remaining 180 were randomized to 1 of the 3 videos, but 1 participant was subsequently excluded after it was discovered that she was under 35 years of age. Therefore, 179 questionnaires were analyzed (99.5% of those random-ized, 62% of those eligible; 55% of those approached). Participants were predominantly white (60%), insured (78%), and high school graduates (86%) (Table 1). Most reported having had a mammogram (75%) and a majority (55%) had 1 in the last 2 years. Most women (91%) were not at high risk for breast cancer as calculated by the Gail model. Nearly two thirds (63%) correctly converted 40% to 4 out of 10 and were considered numerate.
Table 1.
Characteristics of Participants by Video Framing
| Positive Video N = 64 | Neutral Video N = 54 | Negative Video N = 60 | P Value | |
|---|---|---|---|---|
| Mean age, y | 43 | 44 | 44 | .9 |
| Race, % | .3 | |||
| White | 55 | 65 | 59 | |
| Black | 42 | 35 | 41 | |
| Hispanic | 3 | |||
| Insured, % | 84 | 81 | 70 | .4 |
| Education, % | .1 | |||
| Did not finish high school | 8 | 15 | 20 | |
| High school graduate | 22 | 12 | 31 | |
| Some college | 37 | 40 | 25 | |
| College graduate | 33 | 33 | 24 | |
| Numerate, % | 64 | 68 | 58 | .6 |
| Family history of breast cancer, % | 20 | 7 | 16 | .1 |
| Five-year breast cancer risk, % | .9 | |||
| Less than 1.67% | 90 | 92 | 91 | |
| Ever had a mammogram, % | 73 | 74 | 78 | .7 |
| Mammogram last 2 years, % | 55 | 55 | 55 | 1.0 |
Preintervention Findings
Before seeing the videos, women's responses to questions about the benefits and harms of mammography were inaccurate (Table 2). Most women responded incorrectly to all 3 questions (82%). Only 3% correctly responded that 1 life would be extended out of 1,000 with mammography. Most (76%) women greatly overestimated the benefit, endorsing incorrect responses that 300 women or 500 women out of 1,000 would live longer because of mammography. Women also underestimated the risk of having a false positive: 47% responded incorrectly that either 1 out of 1,000 or 10 out of 1,000 women would experience a false positive rather than the correct response of 300 out of 1,000 women. When women were asked about balancing the risks and benefits of mammography most women (81%) thought the benefits were more important than the harms (75% much more important; 6% somewhat more important) (Table 3). The results were similar among the 3 groups.
Table 2.
Changes in Accurate Responses to Questions About Mammography Before and After Videos (%)
| Out of 1,000 women just like you who undergo yearly mammograms for 10 years | Positive Video | 95% CI | Neutral Video | 95% CI | Negative Video | 95% CI | P Value* | |
|---|---|---|---|---|---|---|---|---|
| How many women would live longer because of screening? | prevideo | 2 | 6 | 2 | ||||
| postvideo | 61 | 61 | 44† | |||||
| change | 59 | 45 to 73 | 54 | 39 to 70 | 42 | 28 to 56 | .12 | |
| How many women would have a false positive? | prevideo | 16 | 9 | 20 | ||||
| postvideo | 40† | 65 | 68 | |||||
| change | 24 | 6 to 42 | 55 | 37 to 72 | 49 | 33 to 65 | .003 | |
| How many women would be upset by a false positive even after it was known that there was nothing wrong? | prevideo | 22 | 17 | 21 | ||||
| postvideo | 32† | 56 | 62 | |||||
| change | 8 | −7 to 23 | 39 | 22 to 57 | 44 | 29 to 60 | .003 |
P value, differences in knowledge change across the 3 videos.
Indirect presentation/subtraction required.
Table 3.
Women Who Agree the Benefits Are More Important by Accuracy to Knowledge Questions, Numeracy, Mammography, and Breast Cancer Risk Factors
| Agree before Videos n | Agree after Videos n | RR* | 95% CI | |
|---|---|---|---|---|
| 2 or 3 knowledge questions correct | 74 | 76 | 1.1 | 0.82 to 1.2 |
| 0 or 1 knowledge questions correct | 64 | 67 | ||
| Numerate | 99 | 103 | 1.2 | 1.1 to 1.2 |
| Nonnumerate | 28 | 28 | ||
| Ever had a mammogram | 109 | 111 | 1.1 | 0.70 to 1.2 |
| Never had a mammogram | 29 | 32 | ||
| Mammogram in last 2 years | 83 | 81 | 0.90 | 0.55 to 1.1 |
| No mammogram in last 2 years | 55 | 62 | ||
| Breast cancer risk ≥ 1.67% | 13 | 13 | 1.1 | 0.41 to 1.2 |
| Breast cancer risk < 1.67% | 123 | 123 |
Estimated relative risks calculated from odds ratios controlling for baseline responses36 RR, relative risk.
Postintervention Findings
Effect of the Videos on the Accuracy of Women's Responses to Knowledge Questions
In order to assess changes in the accuracy of women's responses to the 3 knowledge questions, we first examined the effect of the presentation in the video in comparison to response options offered. Depending upon the frame of the video, the responses offered for each question were either answers taken directly from the information in the video (direct) or subtraction was required from the number given in the video to obtain the correct answer (indirect). The accuracy of responses differed for 2 of the 3 questions comparing direct versus indirect presentations (Table 2). To assess the effect of framing, we compared responses for the 2 video frames with direct presentations for each question. For these comparisons, improvement in the proportion of women giving accurate responses was similar for the 3 questions.
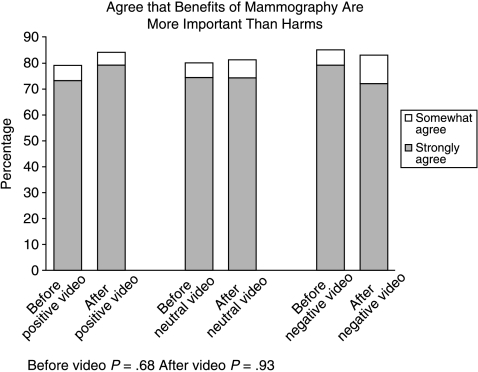
Effect of the Videos on the Balance of Benefits and Harms
Women's perceptions of the balance between the benefits and harms showed little change after seeing the videos (Fig. 2). Overall, 83% agreed that the benefits were more important (75% benefits much more important; 8% benefits somewhat more important). These results did not change when we controlled for baseline perceptions. The relative risk (RR) for agreeing that the benefits were more important than the harms for the positive video versus the negative video was RR = 1.11 (95% CI, 0.76 to 1.12), for the positive video versus the neutral video was RR = 1.1 (95% CI, 0.75 to 1.2), and for the negative video versus the neutral video was RR = 1.0 (95% CI, 0.63 to 1.2).36
Figure 2.
Women's perceptions of benefits and harms.
Overall, 10% of women changed their perceptions after seeing the videos. Ten women initially responded that the harms were more important than the benefits, and after the video changed their responses to the benefits were more important than the harms (5 for the positive video, 2 for the neutral video, and 3 for the negative video). Six women changed in the opposite direction (2 for the positive video, 1 for the neutral video, and 3 for the negative video). Additionally, the change in women's perceptions of the benefits and harms did not differ when we compared women by their accuracy in answering our knowledge questions, whether they had previous mammography, or their 5-year breast cancer risk as calculated by the Gail model (Table 3), but the numbers in these subgroup analyses were small. There were small differences seen with numeracy.
DISCUSSION
We found that women were more accurate in their responses to questions about the benefits and harms of mammography after receiving structured information, but the improvement was not affected by the framing of the information. Women's perceptions of the balance between the harms and benefits of mammography did not change after receiving structured information, regardless of which video they received.
Several reasons may explain why we found no effect on women's perceptions of the benefits and harms. One potential explanation for these findings is that participants did not understand the information presented. The improvement in women's knowledge showed that they received some information from the videos; whether this reflects true understanding is not clear.37
Another potential explanation is that women understood the information, but did not believe it. Women may have not believed the information we presented in the videos because the chance of benefiting from screening was low. Information that conveys small risks is seen as less credible.38 The benefit of extending 1 life over the course of 10 years may have appeared too small to be believable. Furthermore, this small risk contradicts other messages women are receiving. Stories of young women diagnosed with breast cancer are disproportionately reported in the popular press,18 making it appear that developing and dying from breast cancer for young women is more common than it actually is. Reeducating women about breast cancer risk has had limited success,14,39 indicating that beliefs about breast cancer risk are difficult to modify.
A final potential explanation is that participants may have understood and believed the information in the videos, but decided that the benefits of mammography still outweighed the harms. Several theories of health behavior, such as the health belief model, protection motivation theory, and the theory of reasoned action, suggest that decision makers consider the severity of the outcome and the likelihood of it occurring, and then balance these with the negative consequences of adopting the behavior.40 Women consider breast cancer a common and serious disease.15 For women deciding about mammography screening, they would balance these perceptions against the consequences of a false positive mammogram or other perceived harms. In support of these theories, women's readiness to obtain screening has been shown to be associated with their perceptions of the balance between the pros and cons of mammography.41
All women may not follow a rational process of weighing the potential benefits and harms. Other important emotional or psychological aspects may influence women's beliefs about breast cancer risk and make the information in the videos seem less important. The “availability heuristic” may affect women who know others close to them who have developed breast cancer when they were in their forties.42 Other influences, such as social desirability and the fear of regret, may also be important influences on women's perceptions.
It is also possible that women who had received mammograms dismissed the information they received to avoid psychological inconsistencies (cognitive dissonance) that could occur if their beliefs did not match their behavior.43 Because the purpose of this study was to determine the effect of giving women information on women's perceptions, we did not address these types of cognitive effects, but future studies may find that these are important in women's decisions about mammography.
Most (75%) women in our study had undergone screening despite the controversy about whether the benefits outweigh the risks. This proportion does not differ greatly from the population at large. In 2000, 64% of women aged 40 to 49 reported having had a mammogram in the last 2 years.44 About 10% of our sample had a calculated breast cancer risk of 1.67% or greater. In other primary care practices in North Carolina, we have found that 9% of women aged 40 to 49 (unpublished data) were above this risk threshold. A study using claims data in North Carolina found that 3% of women aged 40 to 45 were above the threshold.45 Given that we included women from ages 35 to 49, the average breast cancer risk for the women in this study is likely to be a bit higher than the general population, perhaps indicating that women who were concerned about the possibility of cancer given their risk factors were more likely to participate.
Our study demonstrated that women had very positive attitudes about mammography at baseline and these attitudes were not changed with information about the potential harms of screening. These findings are consistent with previous research that has shown that women greatly overestimate the risk of breast cancer,13,39 view mammography very positively,15 and are not particularly concerned about the risk of false positives. In one study, only 38% wanted to consider false positives in their decisions about mammography and 63% would tolerate 500 or more false positives for each life saved.46 Qualitative information also supports these findings. Women younger than age 50 reported that the benefits of screening far outweighed the risks.47 Women in their forties appear to have embraced mammography despite the ongoing controversy about whether or not it provides them any benefit.
Where does this leave physicians who are trying to inform women about mammography? Because this study and others have demonstrated that women's perceptions about the benefits and harms of mammography are inaccurate,14,20 clinicians' attempts at education are warranted and supported by the ethical standards of informed consent. Whether framing influences women's perceptions is still uncertain, because women's perceptions did not change in our study. Clinical decisions may be less prone to a framing effect because the information is “salient” to the decision maker, as opposed to hypothetical or indirect information, which has been tested in some settings.26 This may be particularly true for information about breast cancer because women are very aware of the risks of breast cancer. Whether a framing effect could be demonstrated in other cancer screening decisions, such as colon cancer, where attitudes about screening are less positive, is uncertain. For mammography, we suspect that women's enthusiasm would overwhelm further attempts at assessing framing in this situation, unless women who have not decided about mammography or were neutral at baseline were recruited for study. Nevertheless, physicians may want to take care to present women who are undecided about mammography with balanced probabilities because a framing effect has been demonstrated in some other clinical decisions.
We acknowledge limitations to our study. First, we did not measure intent to get screened or screening behavior after the intervention. Instead, we measured change in women's perceptions of the balance of the benefits and harms, and this may not reflect actual intent for screening or screening behavior. However, women's strong belief in mammography suggests that many will be screened. We also did not measure change in the perception of the benefits and harms separately, so we were unable to determine whether these 2 factors changed independently with the information given. Additionally, most women (75%) in this study had undergone mammography. The results in women who had not previously been screened did not differ, but the sample was small. We did not attempt to explain all the potential harms associated with mammography nor did we discuss the detection and treatment of ductal carcinomas in situ, although women may want to consider this information in their decisions.46 The women in this study were recruited from an academic internal medicine practice and over 50% of the women in our sample had some college education. Generalizing to different populations or settings may not be appropriate. Finally, the information we tested was designed for women aged 40 to 49 at average risk for breast cancer making decisions about breast cancer screening. This information is not appropriate for women in other age groups or those aged 40 to 49 who are at increased risk for breast cancer.
In summary, we found that women's knowledge about the benefits and harms of mammography was poor at baseline. After seeing the videos, women improved the accuracy of their responses to questions about the benefits and harms, but this change was not affected by the framing of the information. Women perceived that the benefits of mammography outweighed the harms, and providing accurate information had no effect on these perceptions, regardless of how it was framed.
Acknowledgments
Grant support: This study was supported by the University of North Carolina Lineberger Comprehensive Cancer Center. Drs. Lewis (grant number #00-180-01) and Pignone are supported by the American Cancer Society Cancer Control Career Development Award for Primary Care Physicians. Dr. Sheridan was supported by National Research Services Award PHS#14001–14.
The authors thank David F. Ransohoff, MD and Russell Harris, MD, MPH for their invaluable assistance with this project.
REFERENCES
- 1.Wells J, Marshall P, Crawley B, Dickersin K. Newspaper reporting of screening mammography. Ann Intern Med. 2001;135:1029–37. doi: 10.7326/0003-4819-135-12-200112180-00006. [DOI] [PubMed] [Google Scholar]
- 2.Ernster VL. Mammography screening for women aged 40 through 49—a guidelines saga and a clarion call for informed decision making. Am J Public Health. 1997;87:1103–6. doi: 10.2105/ajph.87.7.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Humphrey LL, Helfand M, Chan BK, Woolf SH. Breast cancer screening: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2002;137:347–60. doi: 10.7326/0003-4819-137-5_part_1-200209030-00012. [DOI] [PubMed] [Google Scholar]
- 4.Ransohoff DF, Harris RP. Lessons from the mammography screening controversy: can we improve the debate? Ann Intern Med. 1997;127:1029–34. doi: 10.7326/0003-4819-127-11-199712010-00016. [DOI] [PubMed] [Google Scholar]
- 5.Pauker SG, Kassirer JP. Contentious screening decisions: does the choice matter? N Engl J Med. 1997;336:1243–4. doi: 10.1056/NEJM199704243361708. [DOI] [PubMed] [Google Scholar]
- 6.Kerlikowske K. Efficacy of screening mammography among women aged 40–49 years and 50–69 years: comparison of relative and absolute benefit. J Natl Cancer Inst Monogr. 1997;22:79–86. doi: 10.1093/jncimono/1997.22.79. [DOI] [PubMed] [Google Scholar]
- 7.Napoli M. What do women want to know? J Natl Cancer Inst Monogr. 1997;22:11–3. doi: 10.1093/jncimono/1997.22.11. [DOI] [PubMed] [Google Scholar]
- 8.Fletcher SW. Breast cancer screening among women in their forties: an overview of the issues. J Natl Cancer Inst Monogr. 1997;22:5–9. doi: 10.1093/jncimono/1997.22.5. [DOI] [PubMed] [Google Scholar]
- 9.Harris R, Leininger L. Clinical strategies for breast cancer screening: weighing and using the evidence. Ann Intern Med. 1995;122:539–47. doi: 10.7326/0003-4819-122-7-199504010-00011. [DOI] [PubMed] [Google Scholar]
- 10.Rimer BK. Putting the ‘informed’ in informed consent about mammography. J Natl Cancer Inst. 1995;87:703–4. doi: 10.1093/jnci/87.10.703. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz LM, Woloshin S, Welch HG. Risk communication in clinical practice: putting cancer in context. J Natl Cancer Inst Monogr. 1999;25:124–33. doi: 10.1093/oxfordjournals.jncimonographs.a024187. [DOI] [PubMed] [Google Scholar]
- 12.Lawrence VA, Streiner D, Hazuda HP, Naylor R, Levine M, Gafni A. A cross-cultural consumer-based decision aid for screening mammography. Prev Med. 2000;30:200–8. doi: 10.1006/pmed.1999.0620. [DOI] [PubMed] [Google Scholar]
- 13.Black WC, Nease RF, Tosteson ANA. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. J Natl Cancer Inst. 1995;87:720–31. doi: 10.1093/jnci/87.10.720. [DOI] [PubMed] [Google Scholar]
- 14.Lerman C, Lustbader E, Rimer B, et al. Effects of individualized breast cancer risk counseling: a randomized trial. J Natl Cancer Inst. 1995;87:286–92. doi: 10.1093/jnci/87.4.286. [DOI] [PubMed] [Google Scholar]
- 15.Silverman E, Woloshin S, Schwartz LM, Byram SJ, Welch HG, Fischhoff B. Women's views on breast cancer risk and screening mammography: a qualitative interview study. Med Decis Making. 2001;21:231–40. doi: 10.1177/0272989X0102100308. [DOI] [PubMed] [Google Scholar]
- 16.Rubin R. The breast cancer scare. US News & World Report. 1993:68–72. [Google Scholar]
- 17.Slaytor EK, Ward JE. How risks of breast cancer and benefits of screening are communicated to women: analysis of 58 pamphlets. BMJ. 1998;317:263–4. doi: 10.1136/bmj.317.7153.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burke W, Olsen AH, Pinsky LE, Reynolds SE, Press NA. Misleading presentation of breast cancer in popular magazines. Eff Clin Pract. 2001;4:58–64. [PubMed] [Google Scholar]
- 19.Schwartz LM, Woloshin S, Black WC, Welch HG. The role of numeracy in understanding the benefit of screening mammography. Ann Intern Med. 1997;127:966–72. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- 20.Rimer BK, Halabi S, Sugg Skinner C, et al. The short-term impact of tailored mammography decision-making interventions. Patient Educ Couns. 2001;43:269–85. doi: 10.1016/s0738-3991(00)00172-5. [DOI] [PubMed] [Google Scholar]
- 21.Edwards A, Elwyn G, Covey J, Matthews E, Pill R. Presenting risk information—a review of the effects of ‘framing’ and other manipulations on patient outcomes. J Health Commun. 2001;6:61–82. doi: 10.1080/10810730150501413. [DOI] [PubMed] [Google Scholar]
- 22.Levin IP, Schneider SL, Gaeth GJ. All frames are not created equal: a typology and critical analysis of framing effects. Organ Behav Hum Decis Process. 1998;76:149–88. doi: 10.1006/obhd.1998.2804. [DOI] [PubMed] [Google Scholar]
- 23.McNeil BJ, Pauker SG, Sox HC, Jr, Tversky A. On the elicitation of preferences for alternative therapies. N Engl J Med. 1982;306:1259–62. doi: 10.1056/NEJM198205273062103. [DOI] [PubMed] [Google Scholar]
- 24.O'Connor AM, Pennie RA, Dales RE. Framing effects on expectations, decisions, and side effects experienced: the case of influenza immunization. J Clin Epidemiol. 1996;49:1271–6. doi: 10.1016/s0895-4356(96)00177-1. [DOI] [PubMed] [Google Scholar]
- 25.Jacoby A, Baker G, Chadwick D, Johnson A. The impact of counselling with a practical statistical model on patients' decision-making about treatment for epilepsy: findings from a pilot study. Epilepsy Res. 1993;16:207–14. doi: 10.1016/0920-1211(93)90081-h. [DOI] [PubMed] [Google Scholar]
- 26.Llewellyn-Thomas HA, McGreal MJ, Thiel EC. Cancer patients' decision making and trial-entry preferences: the effects of ‘framing’ information about short-term toxicity and long-term survival. Med Decis Making. 1995;15:4–12. doi: 10.1177/0272989X9501500103. [DOI] [PubMed] [Google Scholar]
- 27.Friedman LC, Neff NE, Webb JA, Latham CK. Age-related differences in mammography use and in breast cancer knowledge, attitudes, and behaviors. J Cancer Educ. 1998;13:26–30. doi: 10.1080/08858199809528507. [DOI] [PubMed] [Google Scholar]
- 28.Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998;338:1089–96. doi: 10.1056/NEJM199804163381601. [DOI] [PubMed] [Google Scholar]
- 29.Lerman C, Trock B, Rimer B, Jepson C, Brody D, Boyce A. Psychological side effects of breast cancer screening. Health Psychol. 1991;10:259–67. doi: 10.1037//0278-6133.10.4.259. [DOI] [PubMed] [Google Scholar]
- 30.NIH, Consensus Statement. Breast cancer screening for women ages. 1997. pp. 40–49. [PubMed]
- 31.Grimes DA, Snively GR. Patients' understanding of medical risks: implications for genetic counseling. Obstet Gynecol. 1999;93:910–4. doi: 10.1016/s0029-7844(98)00567-5. [DOI] [PubMed] [Google Scholar]
- 32.Costantino JP, Gail MP, Pee D, et al. Validation studies for models projecting the risk of invasive and total breast cancer incidence. J Natl Cancer Inst. 1999;91:1541–8. doi: 10.1093/jnci/91.18.1541. [DOI] [PubMed] [Google Scholar]
- 33.Gail MH, Brinton LA, Byar DP, et al. Projecting individualized probabilities of developing breast cancer for white females who are being examined annually. J Natl Cancer Inst. 1989;81:1879–86. doi: 10.1093/jnci/81.24.1879. [DOI] [PubMed] [Google Scholar]
- 34.Rockhill B, Spiegelman D, Byrne C, Hunter DJ, Colditz GA, et al. Validation of the Gail. model for breast cancer risk prediction and implications for chemoprevention. J Natl Cancer Inst. 2001;93:358–66. doi: 10.1093/jnci/93.5.358. [DOI] [PubMed] [Google Scholar]
- 35.Fisher B, Costantino JP, Wickerham DL, et al. Tamoxifen for prevention of breast cancer: report of the National Surgical Adjuvant Breast and Bowel Project P-1 Study. J Natl Cancer Inst. 1998;90:1371–88. doi: 10.1093/jnci/90.18.1371. [DOI] [PubMed] [Google Scholar]
- 36.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 37.Weinstein ND. What does it mean to understand a risk? Evaluating risk comprehension. J Natl Cancer Inst Monogr. 1999;25:15–20. doi: 10.1093/oxfordjournals.jncimonographs.a024192. [DOI] [PubMed] [Google Scholar]
- 38.Johnson BB, Slovic P. Presenting uncertainty in health risk assessment: initial studies of its effects on risk perception and trust. Risk Anal. 1995;15:485–94. doi: 10.1111/j.1539-6924.1995.tb00341.x. [DOI] [PubMed] [Google Scholar]
- 39.Alexander NE, Ross J, Sumner W, Nease RF, Jr, Littenberg B. The effect of an educational intervention on the perceived risk of breast cancer. J Gen Intern Med. 1996;11:92–7. doi: 10.1007/BF02599584. [DOI] [PubMed] [Google Scholar]
- 40.Weinstein ND. Testing four competing theories of health-protective behavior. Health Psychol. 1993;12:324–33. doi: 10.1037//0278-6133.12.4.324. [DOI] [PubMed] [Google Scholar]
- 41.Rakowski W, Dube CE, Marcus BH, Prochaska JO, Velicer WF, Abrams DB. Assessing elements of women's decisions about mammography. Health Psychol. 1992;11:111–8. doi: 10.1037//0278-6133.11.2.111. [DOI] [PubMed] [Google Scholar]
- 42.Bogardus ST, Jr, Holmboe E, Jekel JF. Perils, pitfalls, and possibilities in talking about medical risk. JAMA. 1999;281:1037–41. doi: 10.1001/jama.281.11.1037. [DOI] [PubMed] [Google Scholar]
- 43.Plous S. The Psychology of Judgement and Decision Making. New York: McGraw-Hill; 1993. pp. 22–3. [Google Scholar]
- 44.National Center for Health Statistics. Health, United States. 2002. Available at: http://www.cdc.gov/nchs/products/pubs/pubd/hus/listables.pdf# 82. Accessed 26 March 2003.
- 45.Bastian L, Lipkus I, Kuchibhatla M, et al. Women's interest in chemoprevention for breast cancer. Arch Intern Med. 2000;161:1639–44. doi: 10.1001/archinte.161.13.1639. [DOI] [PubMed] [Google Scholar]
- 46.Schwartz LM, Woloshin S, Sox HC, Fischhoff B, Welch HG. US women's attitudes to false-positive mammography results and detection of ductal carcinoma in situ: cross-sectional survey. West J Med. 2000;173:307–12. doi: 10.1136/ewjm.173.5.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nekhlyudov L, Ross-Degnan D, Fletcher SW. Beliefs and expectations of women under 50 years old regarding screening mammography. J Gen Intern Med. 2003;18:182–9. doi: 10.1046/j.1525-1497.2003.20112.x. [DOI] [PMC free article] [PubMed] [Google Scholar]