Abstract
Smokers try to quit only once every 2 to 3 years and most do not use proven treatments. Repeated, brief, diplomatic advice increases quit rates. Such advice should include a clear request to quit, reinforcing personal risks of smoking and their reversibility, offering solutions to barriers to quitting, and offering treatment. All smokers should be encouraged to use both medications and counseling. Scientifically proven, first-line medications are nicotine gum, inhaler, lozenge, and patch plus the nonnicotine medication bupropion. Proven second-line medications are clonidine, nicotine nasal spray, and nortriptyline. These medications are equally effective and safe and the incidence of dependence is very small. The proven psychosocial therapies are behavioral and supportive therapies. These are as effective as medications and are effective via individual counseling, group, and telephone formats.
The writing of this article was supported in part by Senior Scientist Award DA-00450 from the National Institute on Drug Abuse.
Keywords: nicotine, smoking, tobacco use disorders, treatment
EPIDEMIOLOGY OF SMOKING CESSATION
About 40% of current smokers attempt to quit each year1 and 4% to 6% are successful2; thus each year about 2% of smokers quit for good.1 Most smokers make multiple attempts, such that half eventually quit smoking.1 Beginning in the 1990s, rates of cessation began to stall1 due to both no increase in the frequency of quit attempts and no increase in the success of a given quit attempt.3 Some, but not all, believe this is because those who have quit thus far have been the “easy quitters” leaving the more dependent, less psychologically stable, and less advantaged smokers who want to quit but are unable.3 Two-thirds of self-quitters relapse within 2 days4; thus, the major focus of smoking cessation interventions must be in the first few days.
MISPERCEPTIONS ABOUT SMOKING CESSATION
One misperception by clinicians, smokers, and nonsmokers is “all smokers can quit smoking, if they are just motivated enough.” This statement is similar to statements made about alcohol and depression problems in the early 1900s. We now know that many persons with these problems are able to “self-cure,” but also that many are unable to improve without treatment. The same is true for tobacco use.5
A related statement is that “95% of all smokers who quit do so on their own.” In fact, with all the new treatments, one-third of smokers who quit now do so via treatment,6 a rate of treatment use greater than that for alcoholism or obesity.7 Some clinicians do not believe brief advice is effective; however, many randomized trials indicate that even brief advice increases quit rates.8,9 Some clinicians do not believe they have the time to provide advice; however, the major role clinicians play is to motivate smokers to quit, which can take as little as 3 minutes (Table 1).8 Some clinicians fear they may embarrass their patients by discussing the topic; however, exit polls suggest that most smokers state doctors who do not ask about their smoking habits are less competent doctors.
Table 1.
General Principles of Requests/Advice About Smoking Cessation
| Content |
| State your concern about their smoking |
| Discuss risks and rewards of smoking |
| Discuss roadblocks to quitting |
| Clearly state a request to consider stopping |
| Style |
| Empathic |
| Diplomatic and noncoercive |
| Avoid arguments |
| Optimism about change |
| Repeat at intervals |
METHODS FOR MOTIVATING SMOKERS TO STOP
Helping smokers to quit involves 2 processes—motivating them to attempt to quit and helping them to stop once they try. At any given time, only about 10% of smokers are planning to quit in the next month, 30% are contemplating to quit in the next 6 months, 30% plan to quit at some unknown time, and 30% have no plans to quit10; thus, the large majority of clinician interventions involve motivating smokers to try to stop.
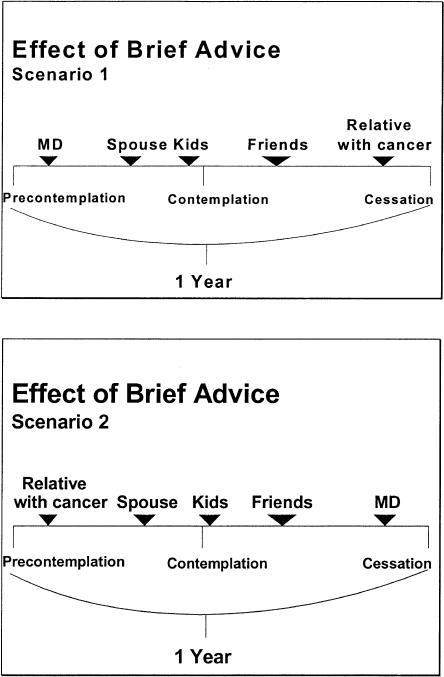
Most requests to stop smoking may appear to have little or no effect; however, consider the scenario in Figure 1, Scenario 1. A clinician asks a smoker to stop and the smoker does not. Then the smoker's spouse asks the smoker to stop; then his/her kids ask; then his/her friends ask; then a year after the clinician first gave advice, the smoker's uncle who is dying of lung cancer asks and the smoker decides to quit. Now the clinician may conclude that his/her advice was not effective and it took the scare of a relative with cancer to motivate a quit attempt. However, consider the scenario in which the clinician's advice and the uncle's cancer switch places (Figure 1, Scenario 2). Here many prior requests for smoking have preceded clinician advice and when the clinician asks, the smoker now agrees to quit. In this scenario, the clinician may believe he/she is especially effective but in reality it is the cumulative effect of prior requests that is important. Thus, the clinician should not expect any given piece of advice to have much of an immediate effect. Rather, the clinician should give the advice, knowing that it will move a smoker that much closer to a quit attempt.
Figure 1.
Two scenarios of the natural history of brief advice and subsequent cessation.
The 3 most commonly cited approaches to making requests or giving advice about smoking are the U.S. Public Health Service's (USPHS) 5 As/5Rs,8 motivational interviewing,11 and Stage of Change12 models. The 5 As outlined in the recent USPHS guideline are: ask about tobacco use, advise to quit, assess willingness to make attempt to quit, assist with treatments, and arrange follow-up.8 The major emphasis in this model is a clear statement advising the smoker to quit. If upon assessment in the 5 A program the smoker is unwilling to quit, one is to motivate the smoker using the 5 Rs; i.e., focus on personally relevant information on, risks of smoking, rewards of stopping, roadblocks to quitting, and repeating this advice.
There is substantial evidence from randomized trials that brief advice based on these models is effective.8 In the most recent meta-analyses, even 3 minutes of such advice done in a systematic and diplomatic manner (Table 2) increases quit rates by a factor of 1.3 to 1.7.8,9
Table 2.
Validated Cessation Treatments
| First-Line Therapies | Availability | Efficacy (Odds Ratio) |
|---|---|---|
| Bupropion | Rx | 2.1 |
| Nicotine gum | OTC | 1.5 |
| Nicotine patch | OTC | 1.9 |
| Nicotine inhaler | Rx | 2.5 |
| Nicotine lozenge | OTC | 1.7 |
| Behavior therapy | Group, individual, or telephone | 1.5 |
| Supportive therapy | Group, individual, or telephone | 1.5 |
| Second-line therapies | ||
| Nicotine nasal spray | Rx | 2.7 |
| Clonidine | Rx | 2.1 |
| Nortriptyline | Rx | 2.7 |
Rx, prescription; OTC, over the counter.
Unfortunately, half of smokers never quit.13 Three strategies have been proposed to help reduce tobacco risks for these recalcitrant smokers: switching to low-tar cigarettes, switching to pipes, cigars, or smokeless tobacco, or reducing the amount smoked. Currently, none of these have solid evidence of benefit either to raise quit rates or to improve long-term health.14
Pharmacological Therapies
The 8 scientifically proven medications for smoking cessation are nicotine gum, inhaler, lozenge, patch, and nasal spray and the nonnicotine medications bupropion, clonidine, and nortriptyline.8,15 All are equally effective; i.e., they increase quit rates by a factor of 1.5 to 2.7 (Table 2). However, clonidine, nicotine nasal spray, and nortriptyline appear to have more side effects and thus are considered second line. Because we have no scientifically proven method to match patients to a specific treatment, most experts suggest patients themselves should decide which treatment should be used. Some have suggested that these medications will not work if used without psychosocial therapies. However, multiple randomized trials of use of over-the-counter (OTC) medications with no psychosocial therapy indicate this is effective.8,15 However, combining psychosocial and pharmacological treatments clearly increases success (Table 3).
Table 3.
Percent of Quitters Who Use Each Cessation Therapy and Long-term Quit Rates Among Those Who Use the Therapy*
| Psychological Therapy | ||||
|---|---|---|---|---|
| No Therapy,†% | Brief Therapy,‡% | Intensive Therapy,§% | Total, % | |
| No medication | 72 use/4 quit | 7 use/6 quit | 1 use/12 quit | 80 use/4 to 12 quit |
| Medication|| | 11 use/8 quit | 8 use/12 quit | 1 use/25 quit | 20 use/8 to 25 quit |
| Total | 83 use/4 to 8 quit | 15 use/6 to 12 quit | 2 use/12 to 25 quit | |
Based on various epidemiological and meta-analytic data cited in text.
Includes self-help materials.
MD advice (3–10 min) telephone counseling.
Individual or group tx 30 min and multiple sessions.
OTC use = 85% and prescription use = 15% of medication use.
Nicotine replacement therapies (NRTs) appear to work because they relieve withdrawal symptoms of anxiety, depression, difficulty concentrating, insomnia, irritability, restlessness, and nicotine craving.8 Because NRTs provide much lower levels of nicotine than does smoking and because the nicotine is absorbed more slowly than it is from cigarettes, they do not appear to cause cardiovascular harm and their dependence potential is very small (<2%).16
Four types of NRTs use ad-libitum dosing: nicotine gum, inhaler, lozenge, and nasal spray. Their major advantage is they can be used to cope with situationally induced cravings or withdrawal. Their disadvantage is the need to use multiple doses per day, the need to avoid acidic beverages when using the product, and possible embarrassment with use.
Nicotine gum is an OTC medication that is available in 2 mg (<25 cigarettes/day smoker) and 4 mg (>25 cigarettes/day smoker) doses.8,15 The recent provision of mint and citrus flavors has significantly improved the taste of the gum. Side effects include jaw ache, nausea, and stomach ache.
The nicotine patch, or transdermal nicotine, is available OTC as a 24-hour patch in doses of 21, 14, and 7 mg, and as a 16-hour patch at a 15-mg dose.8,15 The major advantage of the patch is that it requires only a once per day dosage and it is more socially acceptable and confidential than the gum. The major disadvantage is that it cannot be used for sudden cravings. Whether 24-hour versus 16-hour patch use or whether tapering doses improves quit rates is unclear. Side effects include insomnia and skin rash.
The nicotine inhaler consists of a plug impregnated with nicotine in a plastic rod.8,15 When warm air is pulled through the rod, nicotine is absorbed. The inhaler is available as a prescription (Rx) item in a single dose. Although labeled an inhaler, this product actually delivers nicotine not via the lungs but through the mouth, like gum. The major advantage of the inhaler is that it replicates the habit feature of smoking. Its major disadvantage is the need for multiple puffs to obtain sufficient nicotine. The main side effect is throat irritation.
The nicotine nasal spray is available Rx as a single dose. The major advantage of the spray is that it provides higher and more rapid nicotine doses compared to other NRTs8,15; however, this still is less than one-tenth the arterial nicotine levels seen with cigarettes. Its major disadvantage is that nasal irritation, lacrimation, rhinitis, coughing, sneezing, and facial flushing are experienced by more than 75% of users.
Finally, a nicotine lozenge has just become available as an OTC medication in the U.S. in a 2-mg dose for those smoking their first cigarette after 30 minutes of arising and a 4-mg dose for those smoking less than 30 minutes after arising. The lozenge produces nicotine levels, efficacy, and side effects similar to nicotine gum but may be more acceptable.17
Although current FDA-approved labeling advises against combining NRTs, adding ad-lib use of nicotine gum, inhaler, nasal spray, and probably lozenge to the nicotine patch does increase quit rates without increased side effects.8,15
Buproprion is an Rx medication first used as an antidepressant.8,15 Bupropion's efficacy for smoking is unrelated to its antidepressant effects—it works equally well in smokers with and without a history of depression. The major advantages of bupropion are that many smokers prefer a nonnicotine medication. Side effects include seizure (risk < 1/1,000), insomnia, dry mouth, and nausea. Bupropion combined with NRT increased quit rates slightly in 1 study.18
Both clonidine and nortriptyline appear to be as effective as bupropion and NRT but appear to have more side effects than first-line therapies.8,15 Clonidine can cause hypotension and drowsiness; nortriptyline can cause sedation, nausea, dry mouth, constipation, and urinary retention.
Current labeling calls for physicians to decide if the above medications should be used in pregnant women or smokers with heart disease.8,15 Stopping smoking in the first 2 trimesters of pregnancy reverses most of the risk of smoking to the fetus. How much of the harmful effects of smoking in pregnancy are due to nicotine, carbon monoxide, or other constituents is unclear.16 Since NRT produces lower levels of nicotine and no carbon monoxide, recent reviews have suggested using NRT in pregnant women who cannot quit on their own. The major remaining concern is the role of nicotine in Sudden Infant Death Syndrome.16
Despite initial concerns, many studies have demonstrated that NRT in patients with active heart disease is not especially risky.19 Concurrent use of NRT and cigarettes also does not substantially increase the risk of heart or other diseases.19
Psychosocial Treatments
Behavioral therapy8 focuses on building skills to resist relapse such as developing incompatible behaviors (e.g., exercise), coping thoughts, refusal skills, etc.20 This therapy increases quit rates by a factor of 1.5 to 2.1.8,21,22
Social support identifies persons who will be encouraging about cessation, finds “buddies” who are also either trying to quit or have done so, etc. Social support increases quit rates by a factor of 1.3 to 1.5.8
Behavioral and supportive therapies were developed initially for use in individual or group therapy formats. However, less than 5% of smokers will attend such therapy (Table 3).21 Written materials do not appear to be effective8,23; however, delivering behavior therapy via the telephone increases quit rates by a factor of 1.2.8,24 Although less effective, this format is so much more acceptable that it has a bigger impact than group or individual counseling. Whether therapy could be delivered via the Internet is being tested. Acupuncture, hypnosis, inpatient treatment, and Twelve-Step therapy (Nicotine Anonymous) have not been shown effective thus far.8
SPECIFIC ISSUES IN SMOKING CESSATION
Although many experts recommend abrupt cessation methods, gradual reduction is as effective.8 However, all experts believe setting a firm date by which one is to become tobacco free is important.
Smoking decreases blood levels of a number of medications; thus, stopping smoking substantially increases these blood levels, i.e., often by 20% to 50%.23 Patients often need to have their dosage of these medications monitored and adjusted when they stop smoking.
Smokers weigh less than nonsmokers because nicotine suppresses appetite and increases energy expenditure.25 Smokers gain an average of 4 kg when they stop smoking.25 Studies of teaching smokers to diet to keep off weight gain to increase quit rates found just the opposite —dieting caused more relapse.25 Early studies suggest postcessation exercise not only prevents weight gain but also aids cessation.23 Also, both NRT and bupropion prevent weight gain while they are used.8 Thus, one option is to encourage exercise and to use a medication initially. Dieting (if necessary) could then be postponed until abstinence is well established and medication is decreased.25
The little research that has been done on treatment for those with psychiatric disorders,26 adolescents,27 or smokeless tobacco users8 suggests these groups should be treated similarly to adult cigarette users until special programs for these groups are validated.8
CONCLUDING REMARKS
The most important aspect to smoking cessation is maintaining the motivation to make multiple attempts. Thus, quit attempts should be thought of like practice sessions in learning a new skill—at some point one hopes to “get it right,” but one should not put undue hope on any single given quit attempt, and take solace in knowing the probability of success increases with each try.
Given that 1) stopping smoking is the single most important thing one can do to improve their health; 2) smoking cessation treatment doubles or triples quit rates; and 3) smoking treatment is the “gold standard” of cost-effective treatments,28 smoking cessation is not the time to try to reduce costs by allocating treatments only to those with special difficulties. All smokers should be encouraged to access a treatment. Typically, state health departments are the best source of information on local cessation resources. In addition, since the efficacy of brief advice, pharmacotherapies, and psychological therapies all are dose related—the more intense the treatment, the greater the success rate8—smokers should be encouraged to participate in as intensive therapies as possible.
REFERENCES
- 1.Center for Disease Control and Prevention. Cigarette smoking among adults—United States, 1998. Morb Mortal Wkly Rep. 2000;49:881–4. [PubMed] [Google Scholar]
- 2.Cohen S, Lichtenstein E, Prochaska JO, et al. Debunking myths about self-quitting. Am Psychol. 1989;44:1355–65. doi: 10.1037//0003-066x.44.11.1355. [DOI] [PubMed] [Google Scholar]
- 3.Hughes JR. The evidence for hardeningIs the target hardening? NCI Smoking and Tobacco Control Monograph. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2001. [Google Scholar]
- 4.Hughes JR, Gulliver SB, Fenwick JW, et al. Smoking cessation among self-quitters. Health Psychol. 1992;11:331–4. doi: 10.1037//0278-6133.11.5.331. [DOI] [PubMed] [Google Scholar]
- 5.Hughes JR. Four beliefs that may impede progress in the treatment of smoking. Tob Control. 1999;8:323–6. doi: 10.1136/tc.8.3.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes JR, Burns DM. Population Based Smoking Cessation. Bethesda, MD: National Cancer Institute;; 2001. Impact of medications on smoking cessation; pp. 155–64. Proceedings of a Conference on What Works to Influence Cessation in the General Population, Smoking and Tobacco Control, Monograph No. 12. [Google Scholar]
- 7.Klingemann H, Sobell L, Barker J, et al. Promoting Self-Change from Problem Substance Use: Practical Implications for Policy, Prevention and Treatment. Dordrecht, The Netherlands: Kluwer Academic Publications; 2001. [Google Scholar]
- 8.Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and DependenceClinical Practice Guideline. Rockville, MD: Public Health Service; 2000. [Google Scholar]
- 9.Silagy C, Ketteridge S. Physician Advice for Smoking Cessation. 1999. The Cochrane Library, Issue 4 Updated Software;
- 10.Etter JF, Perneger TV, Ronchi A. Distributions of smokers by stage: international comparison and association with smoking prevalence. Prev Med. 1997;26:580–5. doi: 10.1006/pmed.1997.0179. [DOI] [PubMed] [Google Scholar]
- 11.Emmons KM, Rollnick S. Motivational interviewing in health care settings. Opportunities and limitations. Am J Prev Med. 2001;20:68–74. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- 12.Prochaska JO, Goldstein MG. Process of smoking cessation: implications for clinicians. Clin Chest Med. 1991;12:727–35. [PubMed] [Google Scholar]
- 13.Burns DM, Anderson C, Major J, Vaughn J, Shanks T. Population Impact of Smoking Cessation. Bethesda, MD: National Cancer Institute; 2000. Cessation and cessation measures among adult daily smokers: national and state-specific data; pp. 25–98. Proceedings of a Conference on What Works to Influence Cessation in the General Population, Smoking and Tobacco Control, Monograph No. 12. [Google Scholar]
- 14.Hughes JR. Harm reduction approaches to smoking: the need for data. Am J Prev Med. 1998;15:78–9. doi: 10.1016/s0749-3797(98)00033-6. [DOI] [PubMed] [Google Scholar]
- 15.Hughes JR, Goldstein MG, Hurt RD, Shiffman S. Recent advances in the pharmacotherapy of smoking. JAMA. 1999;281:72–6. doi: 10.1001/jama.281.1.72. [DOI] [PubMed] [Google Scholar]
- 16.Benowitz NL. Nicotine Safety and Toxicity. New York: Oxford University Press; 1998. [Google Scholar]
- 17.Shiffman S, Dresler CA, Hajek P, Gilburt SJA, Targett DA, Strahs KR. Efficacy of a nicotine lozenge for smoking cessation. Arch Intern Med. 2002;162:1267–76. doi: 10.1001/archinte.162.11.1267. [DOI] [PubMed] [Google Scholar]
- 18.Jorenby DE, Leischow SJ, Nides MA, et al. A controlled trial of sustained-release bupropion, a nicotine patch, or both for smoking cessation. N Engl J Med. 1999;340:685–91. doi: 10.1056/NEJM199903043400903. [DOI] [PubMed] [Google Scholar]
- 19.Benowitz NL, Gourlay SG. Cardiovascular toxicity of nicotine: implications for nicotine replacement therapy. J Am Coll Cardiol. 1997;29:1422–31. doi: 10.1016/s0735-1097(97)00079-x. [DOI] [PubMed] [Google Scholar]
- 20.Hughes JR. Behavioral support programs for smoking cessation. Mod Med. 1994;62:22–7. [Google Scholar]
- 21.Lancaster T, Stead LF. Individual Behavioural Counselling for Smoking Cessation. 2002. The Cochrane Library, Issue 3, Updated Software; [DOI] [PubMed]
- 22.Stead LF, Lancaster T. Group Behaviour Therapy Programmes for Smoking Cessation. 2002. The Cochrane Library, Issue 3, Updated Software; [DOI] [PubMed]
- 23.Lancaster T, Stead LF. Self-help Interventions for Smoking Cessation. 2002. The Cochrane Library, Issue 3, Updated Software; [DOI] [PubMed]
- 24.Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ. Telephone counseling for smoking cessation: rationales and review of evidence. Hlth Educ Res. 1996;11:243–57. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- 25.Perkins KA. Weight gain following smoking cessation. J Consult Clin Psychol. 1993;61:768–77. doi: 10.1037//0022-006x.61.5.768. [DOI] [PubMed] [Google Scholar]
- 26.Hughes JR, Zarin DA, Pincus HA. Treating nicotine dependence in mental health settings. J Prac Psych Behav Hlth. 1997:250–4. [Google Scholar]
- 27.Sussman S. Effects of sixty six adolescent tobacco use cessation trials and seventeen prospective studies of self-initiated quitting. Tob Induced Dis. 2002;1:35–81. doi: 10.1186/1617-9625-1-1-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Warner KE, Luce BR. Cost-Benefit and Cost-Effectiveness Analyses in Health Care: Principles, Practice, and Potential. Ann Arbor, MI: Health Administration Press; 1983. [Google Scholar]