Abstract
OBJECTIVE
A frequently cited obstacle to universal insurance is the lack of consensus about what benefits to offer in an affordable insurance package. This study was conducted to assess the feasibility of providing uninsured patients the opportunity to define their own benefit package within cost constraints.
DESIGN
Structured group exercises
SETTING
Community setting
PARTICIPANTS
Uninsured individuals recruited from clinical and community settings in central North Carolina.
MEASUREMENTS
Insurance choices were measured using a simulation exercise, CHAT (Choosing Healthplans All Together). Participants designed managed care plans, individually and as groups, by selecting from 15 service categories having varied levels of restriction (e.g., formulary, copayments) within the constraints of a fixed monthly premium comparable to the typical per member/per month managed care premium paid by U.S. employers.
MAIN RESULTS
Two hundred thirty-four individuals who were predominantly male (70%), African American (55%), and socioeconomically disadvantaged (53% earned <$15,000 annually) participated in 22 groups and were able to design health benefit packages individually and in groups. All 22 groups chose to cover hospitalization, pharmacy, dental, and specialty care, and 21 groups chose primary care and mental health. Although individuals' choices differed from their groups' selections, 86% of participants were willing to abide by group choices.
CONCLUSIONS
Groups of low-income uninsured individuals are able to identify acceptable benefit packages that are comparable in cost but differ in benefit design from managed care contracts offered to many U.S. employees today.
Keywords: medically uninsured; managed care programs; insurance, health; Medicaid; financing, government; health care rationing; health care reform; health policy
The number of uninsured Americans has been stubbornly stable or increasing for the last decade despite a healthy U.S. economy.1,2 The escalating cost of health insurance, medical care, and medications makes it increasingly difficult to find affordable solutions for broadening insurance coverage.3,4
A variety of options currently are being explored for expanding coverage, including tax credits,5 expansion of public programs,6 and combinations of public and private financing.7,8 Many states are enacting individual and small-group market reforms and many are hoping to expand coverage by broadening Medicaid eligibility in order to increase access to health insurance.9,10 All these initiatives are likely to offer insurance that is tightly restricted to conserve resources. How to restrain costs however, has been hotly debated. Without agreement on how to control the “bottomless pit” of healthcare costs, the political will to enact health care reform that offers coverage for the uninsured is likely to remain absent. Restrictions on access to specialists, pharmaceuticals, and diagnostic tests, among other means of controlling utilization, have frustrated consumers, while the cost of insurance has continued to increase despite these measures.3 One potential way to facilitate cost containment efforts and contribute to awareness of the tradeoffs necessitated by limited resources is to give consumers greater control, or voice, in benefit design.
We used a recently designed exercise that allows groups of individuals to identify their preferred health insurance package under cost constraints to demonstrate various managed care insurance packages that are likely to be acceptable to uninsured individuals.
METHODS
Participants
Residents of central North Carolina without health insurance were purposively recruited from ambulatory care and community settings. In the ambulatory care setting, uninsured patients who had recurring encounters with physicians at internal medicine and family practice clinics of several teaching hospitals for the prevention, diagnosis, or treatment of any medical condition were recruited by research assistants using a posted notice or solicitation as they came into the clinic waiting area. In community settings, volunteers were recruited through invitations at a long-term residential shelter, as well as through advertisements in local newspapers, fliers, word of mouth, and posters on mailboxes. Participants were paid $75 to compensate for their time.
Study Instruments
This study involves structured small-group exercises utilizing CHAT (Choosing Healthplans All Together), a simulation exercise designed to allow groups of laypersons to construct health plans within the constraint of limited resources. 11 Group sessions are led by a trained facilitator and last approximately 2.5 hours.
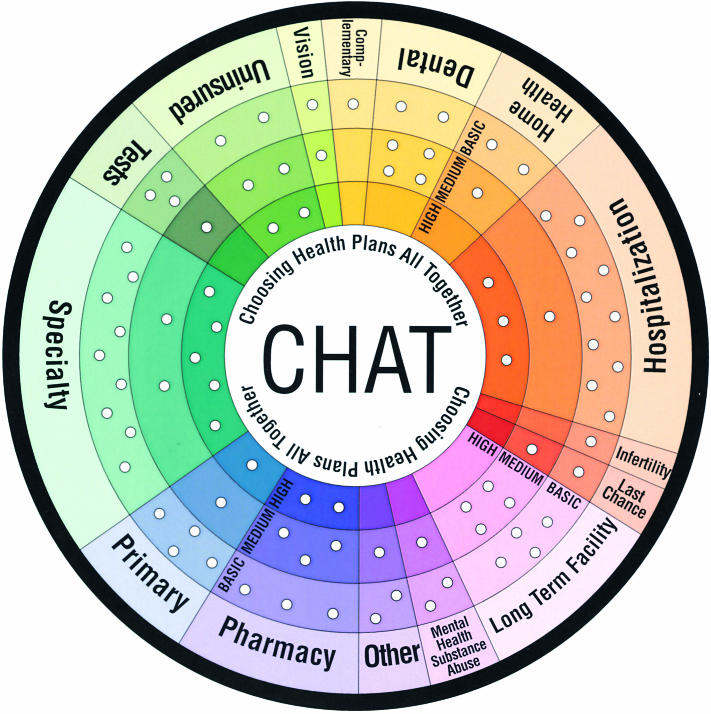
The first step of the exercise utilizes a game board shaped like a pie chart in which 15 insurance benefit categories are represented in slices around the pie (Fig. 1). Participants select their insurance package by distributing pegs among the holes on the board. Participants can select Basic, Medium, or High options for each benefit category or can forgo a category. An instruction manual is provided to describe the benefit categories and associated options (Table 1). All materials are written to be understood at a 6th-grade reading level.
FIGURE 1.
The CHAT board is shown with the number of pegs for each service type and coverage level visible as holes around the board. Each peg represents 2% of the PMPM cost of coverage.
Table 1.
Details of Benefits
| Level of Coverage | |||
|---|---|---|---|
| Type of Coverage | Basic | Medium | High |
| Complementary | |||
| (Pays for “alternative” treatments) | 1 peg: Covers “alternative” services including acupuncture (for pain), chiropractic (for back, neck or bone problems), and therapeutic massage. | ||
| Dental | |||
| (Pays for care of your teeth) | 2 pegs: You get regular cleanings and x-rays every 6 months. You have cavities filled and bad teeth extracted. You get minimal dental care. | 2 + 4 pegs: You get regular cleanings and x-rays every 6 months. You have cavities filled and bad teeth extracted. You get complete dental care including repairs and crowns. | |
| Home health | |||
| (Pays for in-home care if you are chronically ill or too disabled to care for yourself) | 2 pegs: Your insurance pays in full for up to: 2 weekly visits from a nurse OR 2, 1/2 hr daily care from a nurse's aide. | 2 + 1 pegs: Your insurance pays in full for up to: 4 weekly visits from a nurse OR 5 hr daily care from a nurse's aide. | |
| Hospitalization | |||
| (Pays for hospital bills) Note: except in an emergency, you need your insurance plan's approval before the hospital will admit you. | 10 pegs: You pay $50 per day for your first 5 days in the hospital. You have little choice about your hospital (i.e., it could be far from your home). There is pressure on your doctor to discharge you as soon as possible. | 10 + 1 pegs: You pay nothing per day. You have a large selection of hospitals. There is probably one near your home. You have many special facilities to choose from. There is pressure on your doctor to discharge you as soon as possible. | 10 + 1 + 3 pegs: You pay nothing per day. You have a large selection of hospitals. There's probably one near your home. You have many special facilities to choose from. Your doctor can keep you in the hospital as long as he/she wants. |
| Infertility | |||
| (Pays for tests and special procedures for someone having trouble getting pregnant) | 1 peg: Infertility services are in the plan. However, expensive tests or procedures may require the insurance company's approval. | ||
| Last chance | |||
| (Pays for special treatment in life-threatening situations like organ failure or extreme illness) | 1 peg: Organ transplants are paid for by your plan. | 1 + 1 pegs: Organ transplants are paid for by your plan. If you don't get better with current treatments, your insurance will pay for you to take part in research. You may get new treatments that are being tested. | |
| Long-term | |||
| (Pays for your care over a long period of time in a residential or nursing home) | 4 pegs: Half your cost is paid for room and board in an average nursing home. | 4 + 4 pegs: All your cost is paid for room and board in an average nursing home. | |
| Mental health and substance abuse | |||
| (Pays for counseling and therapy, treatment of mental illness, and alcohol and drug abuse) | 2 pegs: Your plan pays for up to 30 visits per year to a therapist. You pay $10 per visit. Your plan pays for up to 30 days per year in a hospital for mental illness or drug abuse. You pay $50 for each day in the hospital. | 2 + 1 pegs: Your plan pays for an unlimited number of visits to a therapist or counselor. You pay nothing per visit. Your visits are free. Your plan pays for an unlimited number of days in a hospital for mental illness or drug abuse. You pay nothing for each day in the hospital. | |
| Other medical | |||
| (Pays for services and equipment like physical therapy, occupational therapy, ambulance service, wheel chair, hospital beds, and artificial limbs) | 2 pegs: Your health insurance company reviews your need first. Then it decides if it will pay for all, some, or none of the services or equipment requested. | 2 + 1 pegs: There is no review process. Your health plan pays in full for all services and equipment. | |
| Pharmacy | |||
| (Pays for medicines your doctor prescribes) | 3 pegs: Your health plan only pays for medicines on its approved list (formulary). If your are prescribed a medicine not on this list, either your doctor has to change it or you pay for it. Your pharmacist must give you a generic medicine if he/she has it. You pay $15 per prescription. | 3 + 3 pegs: Your health plan only pays for medicines on its formulary. If you are prescribed a medicine not on this list, either your doctor has to change it or you pay for it. Your pharmacist may use either generic or brand name medicines for your prescriptions. You pay $5 for generic drugs or $10 for brand name drugs. | 3 + 3 + 2 pegs: Your health plan is not limited by the formulary. Your pharmacist may use either generic or brand name medicines for your prescriptions. You pay $5 per prescription. |
| Primary | |||
| (Pays for regular care from your primary or “family” doctor and staff. Your primary doctor can refer you to other doctors, order special services, and coordinate your care) | 4 pegs: You pay $10 per visit. You wait about 4 weeks for a routine appointment and about 48 hours for an urgent problem. You pay $25 per emergency room visit. There are few doctors from which to choose. It may be difficult to see the doctor you have now, or to pick a female or a minority doctor, or a doctor who speaks your language. You may sometimes see a nurse or physician's assistant instead of a doctor. | 4 + 1 pegs: You pay $10 per visit. You wait about 2 weeks for a routine appointment. You wait about 24 hours for an urgent problem. You pay nothing for emergency room visits. You have more doctors to choose from. You have a better chance of seeing the doctor you have now, or to pick a female or a minority doctor, or a doctor who speaks your language. You'll usually see a doctor rather than a nurse or physician's assistant. | 4 + 1 + 1 pegs: Your plan has all the medium levels plus wellness and prevention benefits such as stop smoking programs, diet programs, automatic cancer screening, and stress management. |
| Specialty | |||
| (Pays for special problems your primary doctor and staff don't handle) | 9 pegs: You need your primary doctor's referral to see a specialist in your plan. You wait about 45 days for an appointment. There are few specialists available. You have little choice of which doctor you see. You pay $10 a visit. If you visit a specialist outside of your plan or go without a referral, you pay for it. | 9 + 2 pegs: You may see a specialist in your plan without a referral from your primary doctor. You wait about 25 days for an appointment. There are more specialists available. You have more choice of which doctor you see. You pay $10 a visit. If you visit a specialist outside of your plan or go without a referral, you pay half. | 9 + 2 + 5 pegs: You may see a specialist without a referral from your primary doctor. You wait only a few days for an appointment. There are many specialties available. You may go to almost any specialist in your area. You pay $10 per visit. |
| Tests | |||
| (Pays for blood work, x-rays, or other tests you need) | 3 pegs: Your doctor needs to get expensive tests approved before ordering them. You might need the test done at a lab far away from your doctor's office. | 3 + 1 pegs: Your doctor can order any tests for you without getting approval. You can have the tests done at or near your doctor's office. | |
| Uninsured | |||
| (17% of the people in your community have no health insurance. This may be because they work for a small company, are self-employed, work part time, have lost their jobs or cannot afford it for other reasons. This option lets some of them buy in to your health plan at half price. People who were in the plan but lost their insurance coverage get the first chance. Next are people with the lowest incomes. Other insurance companies in your area are considering similar plans. Your's would be the first) | 2 pegs: 30% of uninsured people in your community can buy health insurance at half price. | 2 + 2 pegs: 60% of uninsured people in your community can buy health insurance at half price. | 2 + 2 + 2 pegs: 90% of uninsured people in your community can buy health insurance at half price. |
| Vision | |||
| (Pays for eye exams, glasses, and contact lenses) | 1 peg: You get an eye exam every 2 years. | 1 + 1 peg: You get an eye exam every 2 years. You pay $5 per visit. You receive $75 for lenses and frames if needed every 2 years. | |
Participants are given a total of 50 pegs to permit them to allocate a quantity of funds comparable to a typical per-member-per-month (PMPM) premium paid by U.S. employers for managed care plans, excluding administrative costs (based on 1997 estimates).12 Each peg represents 2% of the PMPM premium. Because the national average for an employer-sponsored managed care plan in 1997 was $130 with $19 spent on administrative costs, the 50 pegs may be considered to represent the remaining $111, and with rounding to the closest dollar, each peg may also be assumed to have a value of $2.
Actuarial costs for individual services are estimated on the basis of a breakdown of standard managed care benefit plan costs for major medical categories (inpatient, outpatient, primary care, specialist, radiologic and laboratory tests, other medical services, pharmacy, mental health); these relative costs are rounded to the nearest 2% so that they can be selected using the pegs. Costs for additional categories not routinely included in a typical employee-funded, managed care package, such as dental services and long-term care, were determined as a product of the expected utilization frequency per member and the estimated cost of the service utilization. For example, if a service was expected to be used by 1 out of 1,000 members on a monthly basis and the cost of providing this service was estimated to be $4,000, then the estimated cost of providing this service was estimated to be 1/1,000 × $4,000 or $4.00 per member per month. Costs then were rounded to the nearest 2% or $2 increment, in order to be represented in pegs, which in this example would be 2 pegs. The fifteen services were assigned a total of 83 holes on the game board; the 50 pegs thus permit coverage of 60% of the services offered in the exercise (Fig. 1).
In the second step of the exercise, participants spin a roulette wheel that has the 15 services listed around the circumference, and receive health event cards related to the category on which the roulette ball lands. Event cards each describe an illness scenario and the associated consequences of coverage choices including out-of-pocket payment responsibilities, access, and choice of provider or treatment.
These 2 steps comprise 1 cycle. During the game the cycle is conducted 4 times to allow participants to make choices and face consequences 1) alone, 2) in groups of three, 3) as an entire group, and 4) once again alone. This sequence promotes group decision making13 and allows comparison of individual and group choices. Data were collected on recording sheets at the conclusion of each cycle except cycle 2 because this cycle was primarily conducted to facilitate the group process. (For more information contact the authors).
Self-administered questionnaires were given to participants before and after playing the exercise. The pregame questionnaire included: a) sociodemographic items, health status of participant and his/her immediate family, and experience with chronic illness in the family; b) relative importance (from 1 = very unimportant to 5 = very important) of cost, flexibility, proximity, and physician choice in selection of health insurance14–16; and c) self-reported health services use and out-of-pocket health care expenditures during the prior 12 months. The postgame questionnaire asked participants their views on the group decision, group process and information adequacy, and whether they would be willing to abide by choices made by the group. It also asked whether the participants found the CHAT game understandable and easy to do on a 4-point scale (for example: 1 = very easy, 2 = fairly easy, 3 = fairly hard, and 4 = very hard).
This project was exempted from Institutional Review Board (IRB) review by the Office of Human Subjects Research at the Clinical Center of the National Institutes of Health, and received approval by the IRBs at the University of Michigan, the University of North Carolina at Chapel Hill, and Duke University. During the game, participants were given an alias to preserve their anonymity.
Statistical Analysis
Descriptive statistics were employed to describe the study participants and their attitudes toward characteristics of health insurance coverage, types of coverage, and coverage restrictions. The choice of basic, medium, or high coverage was considered a measure of the degree of coverage restriction selected by participants and was scored on a 3-point scale with 1 for basic coverage, 2 for medium coverage, and 3 for high coverage. The overall degree of restrictiveness for the selected insurance package was calculated as the average of the restrictiveness scores for each of the benefits selected by the individual or group.
Analyses included χ2 statistics and Fisher's exact test for the analysis of categorical variables and the calculation of means and standard deviations, and Student t tests for continuous variables. The Mantel-Haenszel χ2 statistic17 was used to examine linear relationships between pairs of ordinal variables. McNemar's χ2 test18 was employed to assess the degree of agreement between individual health care coverage choices made during the first and fourth cycles of the game. To use McNemar's test, coverage choice for each of the 15 service types was recoded into a dichotomous indicator (i.e., coverage was either selected or not selected). Results are reported as statistically significant if P < .05. All analyses were conducted using SAS statistical software, version 6.12 (SAS Institute, Cary, NC).
Individual responses at the beginning of the exercise (results of the pregame questionnaire and cycle 1 choices) were analyzed with the assumption that they represented independent observations. Individual responses in cycle 4 and the postgame questionnaire were not assumed to be independent and therefore corrections were made for intraclass correlations by adjusting the standard error using STATA, version 7.0 (STATA Corp., College Station, Tex). Intraclass correlations of ≥0.10 were observed for all cycle 4 benefit choices except last chance, infertility, dental, and other services, and several of the postgame questions (whether individuals' views were considered, and whether the group's decision and the way the decision was made were fair to all group members).
RESULTS
Study Subjects
Two hundred thirty-four individuals in 22 groups participated in the exercise between December 1999 and June 2000 (average group size, 12; range, 9 to 15). Participants were predominantly male, minority, and socioeconomically disadvantaged (Table 2). Educational level varied widely, with 84% having at least a high school education. Reported employment status included unemployed (22%), self-employed (14%), employed by others (47%), and other categories (students, retired, disabled). Over half had a household income of less than $15,000/year. Respondents reported health status ranging evenly from fair to excellent with only 1.7% reporting poor health. Ninety-three percent of participants reported a visit to the doctor by someone in their household at least 1 time during the previous 6 months. Although 27% of the sample reported no out-of-pocket payments during the past year, 9% reported out-of-pocket payments of at least $2,000.
Table 2.
Sociodemographic Characteristics and Health Status of Study Participants (N = 234)
| Characteristic | n | %* or Mean ± SD |
|---|---|---|
| Age, y | – | 39.5 ± 11.1 |
| Female | 71 | 31.1 |
| Race | ||
| White | 91 | 39.6 |
| Other/unknown | 13 | 5.6 |
| Black or African American | 126 | 54.8 |
| Hispanic or Latino | 4 | 1.8 |
| Marital status | ||
| Married | 32 | 13.7 |
| Single or never married | 123 | 53.0 |
| Widowed/divorced/separated | 77 | 33.2 |
| Educational attainment | ||
| Less than high school | 36 | 15.6 |
| High school graduate or GED | 80 | 34.6 |
| Some college | 61 | 26.4 |
| College graduate or more | 54 | 23.4 |
| Household Income | ||
| $0–<$7,500 | 80 | 34.2 |
| $7,500–<$15,000 | 45 | 19.2 |
| $15,000–<$35,000 | 50 | 21.4 |
| $35,000 or more | 29 | 12.4 |
| Unknown or not reported | 30 | 12.8 |
| Live alone | 64 | 27.4 |
| Health status | ||
| Excellent | 48 | 20.6 |
| Very good | 74 | 31.8 |
| Good | 70 | 30.0 |
| Fair | 37 | 15.9 |
| Poor | 4 | 1.7 |
| Chronic illness in household in past year | 69 | 31.8 |
| Member of household hospitalized during past 6 months | 46 | 20.4 |
| Proportion living in household with ≥1 physician visits during past 6 months | 218 | 93.2 |
| Out-of-pocket payments during past 12 months | ||
| $0 | 63 | 26.9 |
| <$500 | 58 | 24.8 |
| $500–<$2,000 | 41 | 17.5 |
| $2,000 or more | 21 | 9.0 |
| Unknown | 51 | 21.8 |
Percentages do not always add to 100 due to unknowns and rounding. The number of individuals with unknown values ranges from 1 to 4. Where larger than that, unknowns are reported as separate categories.
Individual Insurance Preferences
More than 70% of participants responded in the pregame questionnaire that the ability to get an appointment quickly, to have low fees and small copayments to visit a physician, to have the flexibility to choose a physician, and the ability to seek specialty care without prior approval, were important or very important.
In both the first and last cycles of the exercise, when selecting on their own, individual participants chose to include an average of 10 of the 15 offered services, with intermediate restrictiveness as indicated by a score of 1.7 (Table 3). Specialty care, last chance treatments (organ transplantation and experimental treatments), and tests were selected more frequently and complementary medicine was selected less frequently in the concluding cycle.
Table 3.
Individual Coverage Choices During Initial and Final Cycles of Game
| Proportion of Participants Selecting Coverage, % | ||
|---|---|---|
| Service Type* | Initial (Cycle 1) | Final (Cycle 4) |
| Hospitalization | 98.7 | 99.6 |
| Dental | 96.1 | 93.0 |
| Pharmacy | 93.1 | 96.1 |
| Vision | 83.3 | 80.7 |
| Primary care | 81.4 | 86.4 |
| Tests† | 81.1 | 88.1 |
| Specialty† | 69.6 | 81.4 |
| Mental health | 59.0 | 65.2 |
| Home health | 58.4 | 64.2 |
| Last chance† | 49.8 | 59.1 |
| Other services | 56.7 | 56.2 |
| Uninsured | 50.2 | 56.0 |
| Long-term care | 53.3 | 55.7 |
| Complementary medicine† | 59.0 | 50.6 |
| Infertility | 18.4 | 13.7 |
| Mean number of services selected | 10.0 | 10.3 |
| Mean restrictiveness score‡ | 1.8 | 1.7 |
See Table 1 for detailed description of services. Services are listed in descending order of preference by initial choice (Cycle 1).
MacNemar's test significant: complementary medicine, P = .037; last chance, P = .013; specialty, P = .001; tests, P = .005.
Package restrictiveness score calculated as the sum of the restrictiveness for the individual coverages selected (1 = basic, 2 = medium, 3 = high) as described in Methods section.
The only participant characteristic associated with benefit selection was employment status. Participants who reported being employed were less likely to select mental health coverage (corrected P = .048).
Group Preferences
During the group selection cycle, the 22 groups selected an average of 12.3 services (SD, 0.4; range, 9 to 15) with a restrictiveness score of 1.4 (range, 1.14 to 1.78) (Table 4). All 22 groups selected coverage for hospitalization, pharmacy, specialty care, and dental services. Twenty-one of the 22 groups selected primary care and mental health services. The only services selected at higher than the basic level by more than half the groups were hospitalization and primary care. No 2 groups selected the exact same constellation of coverage, but there was considerable overlap between groups, and all were able to select packages within the resource constraints imposed by the game.
Table 4.
Group Coverage Choices in Order of Decreasing Frequency (N = 22)
| Groups Selecting Coverage, n | ||||
|---|---|---|---|---|
| Service Type* | At All | Basic | Medium | High |
| Hospitalization | 22 | 3 | 16† | 3 |
| Pharmacy | 22 | 12† | 6 | 4 |
| Dental | 22 | 20† | 2 | — |
| Specialty | 22 | 16† | 6 | 0 |
| Primary care | 21 | 6 | 12† | 3 |
| Mental health | 21 | 15† | 6 | — |
| Tests‡ | 20 | 11† | 9 | — |
| Uninsured | 19 | 14† | 3 | 2 |
| Home health | 19 | 15† | 4 | — |
| Long-term care | 19 | 17† | 2 | — |
| Vision | 18 | 14† | 4 | — |
| Other services | 16 | 14† | 2 | — |
| Last chance | 16 | 15† | 1 | — |
| Complementary medicine | 11 | 11† | — | — |
| Infertility | 2 | 2 | — | — |
See Table 1 for a detailed description of services.
Coverage selected by at least half of all groups (“Majority” policy).
Coverage selection missing for one group.
(—), This coverage level not offered.
The vast majority of individual participants, 196 of 227 individuals (86.3%), indicated that they would be willing to abide by the health care plan developed by their groups. Seven individuals did not answer this question. With the exception that unmarried individuals were less willing to abide by their group's plan (χ2mh = 6.51; P = .011), individual sociodemographic characteristics were not associated with the degree of willingness to abide by the group decision.
Group choices and individual choices, at both the beginning and end of the exercise, were compared for the 31 participants who indicated that they were unwilling to accept the coverage selections of their groups. No significant differences were observed after correction for intraclass correlation. Although we did not find sociodemographic or insurance preference differences between those who were and those who were not willing to abide by the group's decision, we did find differences in their views about the group process. Those who were not willing to abide were more likely to disagree with the statement, “The group's decision was favorable for me” (23% vs 8%; P = .0007), and were more likely to indicate that their own choices were different from their group's choices, although their choices did not actually differ significantly from their group's choices.
Regarding the game process, 97% found the game either fairly or very easy to do, and 97% found the game either fairly or very understandable.
DISCUSSION
Low-income uninsured participants in this study chose a range of insurance packages. Many groups picked benefit packages that differed from those currently offered by employers by including dental and long-term care.19,20 Group selections included a larger number of services and incorporated more restrictions than packages selected by individuals, but the vast majority of individuals were willing to abide by group selections.
The approach we use to identify benefit packages offers several advantages. It allows the lay public to voice their views about the design of their insurance benefits and thus is likely to make the resulting plan(s) more acceptable to them through the process of participatory decision making.21,22 It acknowledges that there are limits, based on medical prudence, financial concerns, and public health concerns, which must be used to guide the lay public in making their choices. It allows a broad array of choices among types of service, including some not traditionally offered by most health insurers. It provides a mechanism for connecting choices to actuarial data that can translate choices into policies. In contrast to prioritization strategies that attempt to define specific conditions and treatments to be covered, such as those used in Oregon,23 it utilizes allocation strategies such as preauthorization requirements, or limits on choice of providers, pharmaceuticals, or co-payments.
The results we report yield several noteworthy comparisons with evidence and perspectives in the literature on public priority setting. One contrasting view derives from studies in several countries indicating that the public is very reluctant to participate in priority setting,24,25 and believes priority setting to be unnecessary.26 Our findings are more consistent with studies showing that, with adequate time and information, the public is willing and able to engage in allocation of finite resources27 and that incorporation of economic features of decision making leads to more accurate conclusions about preferences.28 While some research suggests that the public places a priority on life-saving technologies rather than lower technology interventions such as community and mental health services,29 other evidence suggests that the public is quite likely to make many decisions that are similar to those of insurance benefit officers30 and to recognize the need for low-technology services such as long-term care. While the public is thought to stigmatize mental illness, and mental health coverage does not have parity with other medical benefits in many managed care plans,31,32 nearly all groups in this study chose to include mental health coverage in their plans. We speculate that the more frequent selection of mental health benefits by the unemployed during the individual round of benefit selection may be due to more frequent personal experience with mental illness in those who were unemployed.
Several limitations of the work must be acknowledged. The method is based on the assumption that actuarial weights assigned to benefit options are likely to have some influence on participant choices, and the validity of the results is contingent on the accuracy of the actuarial estimates. Estimates of the relative cost of services were limited by available actuarial data, such as a lack of information about alternative/complementary services, the need to simplify presentation for laypersons by rounding to the nearest 2%, and an inability to tailor costs and illness scenarios to individual groups or geographic regions. Nonetheless, these estimates serve to provide a mechanism for permitting the conversion of individual and group choices into rationing decisions in a way that would not otherwise be possible. Ongoing research is aimed at refining actuarial assumptions. Finally, the study population was not a random sample because recruitment for participation in scheduled group simulation exercises precludes random sampling techniques. Thus, while the sample is parallel to the U.S. uninsured as a whole, in which nearly two thirds of the uninsured have incomes less than 200% of the poverty line and of these more than half are minority,33 the study should be reproduced before the findings can be said to reflect the uninsured population in the United States. If there had been more women and more individuals with dependents, for instance, participant and group choices might have differed.
The findings here have several possible implications. The varied choices of groups reported here suggest that the strategy of using a standard package to promote consumer decisions based on price and quality is not necessarily a desirable approach from the consumer perspective.20 The finding that low-income, uninsured individuals participating in this exercise were willing to accept some out-of-pocket expenses to broaden the scope of services covered in their insurance suggests that the strategy used in Medicaid risk contracts, which assumes that any services not fully insured would be less available to the poor, may not be an assumption that is preferred by low-income individuals. However, it remains to be examined whether choices made during a simulation exercise are preferable in reality. While the study design reported here does not permit us to examine the feasibility of using this decision process for actual insurance design, current research involving the development of electronic and web-based versions of the CHAT exercise will make it more feasible in the future to explore the incorporation of consumer decision exercises into the actual design of benefit plans.
This study of the insurance preferences of the low-income uninsured is intended to promote the feasibility of ultimately financing their medical care through more universal insurance in the United States. As strategies for universal coverage are explored, policy makers need to find solutions that offer equitable financing arrangements along with efforts to identify benefit preferences.
Acknowledgments
The authors wish to acknowledge the invaluable help of Yin Yiu, FSA, MAAA, Dan Spillane, FSA, MAAA, James Springrose, MD, Richard Duke, PhD, and Charlie Hall of Multilogue Corporation; and Glenn Klipp and Vana Prewitt whose expertise made this project possible. CHAT Copyright 1999 University of Michigan, All Rights Reserved.
This project was supported by funding from the National Institutes of Health, the Picker Commonwealth Foundation, and the Robert Wood Johnson Foundation.
The opinions expressed here are the authors' and do not represent official policy of the National Institutes of Health or the Department of Health and Human Services.
REFERENCES
- 1.Bureau USC. Health insurance coverage. 1999 Vol. 2001: http://www.census.gov/hhes/www/hlthin99. Accessed February 26, 2001.
- 2.Grumbach K. Insuring the uninsured: time to end the aura of invisibility. JAMA. 2000;284:2114–6. doi: 10.1001/jama.284.16.2114. [DOI] [PubMed] [Google Scholar]
- 3.Hellander I. A review of data on the health sector of the United States. Int J Health Serv. 2000;30:641–53. doi: 10.2190/0ALW-410B-72XJ-X25G. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal D. Controlling health care expenditures. N Engl J Med. 2001;344:766–9. doi: 10.1056/NEJM200103083441012. [DOI] [PubMed] [Google Scholar]
- 5.Pauly M, Herring B. Expanding coverage via tax credits: trade-offs and outcomes. Health Aff (Millwood) 2001;20:9–26. doi: 10.1377/hlthaff.20.1.9. [DOI] [PubMed] [Google Scholar]
- 6.Feder J, Levitt L, O'Brien E, Rowland D. Covering the low-income uninsured: the case for expanding public programs. Health Aff (Millwood) 2001;20:27–39. doi: 10.1377/hlthaff.20.1.27. [DOI] [PubMed] [Google Scholar]
- 7.Kahn C, III, Pollack R. Building a consensus for expanding health coverage. Health Aff (Millwood) 2001;20:40–8. doi: 10.1377/hlthaff.20.1.40. [DOI] [PubMed] [Google Scholar]
- 8.Davis K, Schoen C, Schoenbaum S. A 2020 vision for American health care. Arch Intern Med. 2000;160:3357–62. doi: 10.1001/archinte.160.22.3357. [DOI] [PubMed] [Google Scholar]
- 9.Kaiser E, Plaza C. Finance issue brief: insurance reform. Issue Brief Health Policy Tracking Serv. 1999;6:1–13. [PubMed] [Google Scholar]
- 10.Pear R. Governors offer ‘radical’ revision of Medicaid plan. New York Times; p. A1. February 26, 2001. [Google Scholar]
- 11.Goold S, Biddle A, Danis M. Choosing Healthplans All Together': A game to assess consumer values and preferences for health insurance. J of Gen Intern Med. 2000;15:68–9. [Google Scholar]
- 12.Milliman and Robertson Inc. HMO Intercompany Rate Survey. Brookfield, Wis: Milliman and Robertson, Inc.; 1997. [Google Scholar]
- 13.Duke R, Greenblat C. Principles and Practices of Gaming Simulation. Newbury Park: Sage Publications; 1981. [Google Scholar]
- 14.Berki S, Ashcroft M. HMO enrollment: who joins what and why. A review of the literature. Milbank Mem Fund Q Health Soc. 1980;58:588–632. [PubMed] [Google Scholar]
- 15.Mechanic D, Ettel T, Davis D. Choosing among health insurance options: a study of new employees. Inquiry. 1990;27:14–23. [PubMed] [Google Scholar]
- 16.Grazier K. Factors affecting choice of health care plans. Health Serv Res. 1986;20:659–82. [PMC free article] [PubMed] [Google Scholar]
- 17.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Am Statistical Assoc. 1959;58:690–700. [PubMed] [Google Scholar]
- 18.McNemar Q. Note on the sampling error of the difference between correlated proportions of percentages. Psychometrika. 1947;12:153–7. doi: 10.1007/BF02295996. [DOI] [PubMed] [Google Scholar]
- 19.Hoy E, Wicks E, Forland R. A guide to facilitating consumer choice. Health Aff (Millwood) 1996;15:9–30. doi: 10.1377/hlthaff.15.4.9. [DOI] [PubMed] [Google Scholar]
- 20.Berghold L. Benefit design choices under managed care competition. Health Aff (Millwood) 1993;12:99–109. doi: 10.1377/hlthaff.12.suppl_1.99. [DOI] [PubMed] [Google Scholar]
- 21.Fleck L. Just caring: health reform and health care rationing. J Med Philos. 1994;19:435–43. doi: 10.1093/jmp/19.5.435. [DOI] [PubMed] [Google Scholar]
- 22.Steinberg Schone B, Cooper P. Assessing the impact of health plan choice. Health Aff (Millwood) 2001;20:267–75. doi: 10.1377/hlthaff.20.1.267. [DOI] [PubMed] [Google Scholar]
- 23.Jacobs L, Marmor T, Oberlander J. The Oregon Health Plan and the political paradox of rationing: what advocates and critics have claimed and what Oregon did. J Health Polit Policy Law. 1999;24:161–80. doi: 10.1215/03616878-24-1-161. [DOI] [PubMed] [Google Scholar]
- 24.Abelson J, Lomas J, Eyles J, Birch S, Veenstra G. Does the community want devolved authority? Results from deliberative polling in Ontario. Can Med Assoc J. 1995;153:403–12. [PMC free article] [PubMed] [Google Scholar]
- 25.Dicker A, Armstrong D. Patients' views of priority setting in health care: an interview survey in one practice. BMJ. 1995;311:1137–9. doi: 10.1136/bmj.311.7013.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Busse R. Priority-setting and rationing in German health care. Health Policy. 1999;50:71–90. doi: 10.1016/s0168-8510(99)00065-2. [DOI] [PubMed] [Google Scholar]
- 27.Lenaghan J. Involving the public in rationing decisions. The experience of citizen juries. Health Policy. 1999;49:45–61. doi: 10.1016/s0168-8510(99)00042-1. [DOI] [PubMed] [Google Scholar]
- 28.Eckerlund I, Ekhof J, Nathorst-Boos J. Patient preferences or cost effectiveness? Priorities are highly affected by introduction of economic dimension. Lakartidningen. 2000;97:5782–6. [PubMed] [Google Scholar]
- 29.Bowling A, Jacobson B, Southgate L. Health service priorities. Soc Sci Med. 1993;37:851–7. doi: 10.1016/0277-9536(93)90138-t. [DOI] [PubMed] [Google Scholar]
- 30.Fowler F, Berwick D, Roman A, Massagali M. Measuring public priorities for insurable health care. Med Care. 1994;32:625–39. doi: 10.1097/00005650-199406000-00007. [DOI] [PubMed] [Google Scholar]
- 31.Satcher D. Mental Health: A Report of the Surgeon General. Vol. 2001. Washington, D.C.: Department of Health and Human Services; 1999. [Google Scholar]
- 32.Levinson C, Druss B. The evolution of mental health parity in American politics. Admin Policy Ment Health. 2000;28:139–46. doi: 10.1023/a:1026659524228. [DOI] [PubMed] [Google Scholar]
- 33.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 1999 Current Population Survey. EBRI Issue Brief. 2000;217:1–26. [PubMed] [Google Scholar]