Abstract
OBJECTIVES
This study examines how specific attributes of managed health plans influence patients' relationships with their primary care practitioners (PCPs) and determines whether these effects are mediated by access to, continuity with, or perceived choice of PCPs.
DESIGN, SETTING, PATIENTS
The data source was the nationally representative 1996/97 Community Tracking Study Household Survey (cumulative response rate 65%). The study population (N = 19,415) was composed of 18- to 64-year-old adults whose most recent visit in the past 12 months was made to their primary care delivery site.
MAIN OUTCOME MEASURE
Patients' ratings of their interpersonal relationships with their PCPs as measured by a 7-item scale.
RESULTS
Gatekeeping arrangements that require patients to select a primary care physician or obtain authorization for specialty referrals were associated with lower ratings of the patient-PCP relationship. Health plan use of a provider network had no effect on the patient-PCP scale score. Although there were no significant differences across any insurance payer categories, uninsured adults rated their relationships with PCPs as significantly poorer than did their insured counterparts. Shorter office waits, having a specific clinician at the primary care site, better perceived choice of PCPs, and a longer duration of relationship with the primary care practitioner were associated with higher ratings of the patient-PCP relationship. Perceived choice of primary care practitioners, but not access to or continuity with PCPs, attenuated some of the negative effects of gatekeeping arrangements on patients' relationships with their primary care practitioners.
CONCLUSIONS
Managed health plans that loosen restrictions on provider choice, relax gatekeeping arrangements, or promote access to and continuity with PCPs, are likely to experience higher patient satisfaction with their primary care practitioner relationships. Lack of health insurance impedes the development of patients' relationships with their primary care practitioners.
Keywords: managed care, patient-physician relationship, primary care, access, continuity of care, uninsured
A sustained partnership distinguishes the patient-physician relationship in primary care from other settings.1 These partnership relationships are characterized by practitioners' providing support and empathy, co-participatory communication, mutual trust, and a physician's whole-person knowledge of the patient.2 Continuous, long-term relationships foster the familiarity between patients and practitioners that forms the bedrock of a sustained partnership.2,3
The ubiquitous presence of managed health plans has raised questions about their effects on patients' relationships with primary care practitioners (PCPs). Little is known about the trade-offs between cost containment and quality of care among managed health plans. Because sustained partnerships with PCPs are central to patients' healthcare experiences,4 consumers are likely to evaluate the success or failure of managed care according to its impact on the patient-PCP relationship. Patients' trust in their primary care practitioners can be directly undermined by gatekeeping arrangements that discourage referral to specialty services.5 On the other hand, managed care proponents note the important roles that gatekeepers play in coordinating services and reducing inefficient healthcare.
In one study, privately insured persons enrolled in health maintenance organizations (HMOs) reported poorer communication with and lower trust in all their physicians than those in non-HMO plans.6 This study, however, did not specifically examine patients' relationships with their primary care practitioners. The long-term nature of the patient-primary care physician relationship makes it qualitatively different from most relationships patients have with specialists,1 which tend to be time limited and focused on management of a specific disease.
Selective provider contracting produces a provider network, the hallmark feature of managed health plans.7 Provider networks limit patients' choice of PCPs and, consequently, may lead to patient dissatisfaction with practitioners. Given free choice of providers, patients will switch physicians if dissatisfied with their relationships. Restricted provider networks increase the chances that when patients switch plans, they must also change PCPs. During a 2- to 3-year interval, 25% to 30% of managed care enrollees experience forced discontinuity with their PCPs.8,9 This occurs because employers move employees into health plans that do not include their PCPs in the provider network. Patients may invest less energy and time in the patient-PCP relationship if they anticipate frequent plan switching.10 Limited provider choice therefore threatens the successful development of patients' sustained partnerships with PCPs.8 Empirical evidence suggests that better choice of PCPs is associated with higher levels of satisfaction with the patient-physician relationship,11 even in group-model HMOs.12
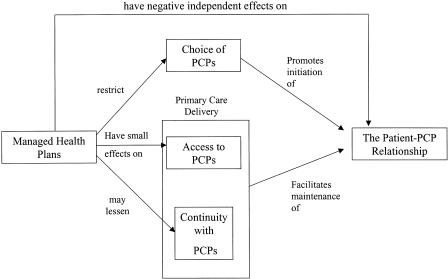
The aims of this study were (1) to provide a better understanding of how gatekeeping arrangements and presence of a provider network influence the patient-PCP relationship, (2) to examine the effects of these managed health plan attributes on primary care delivery and provider choice, and (3) to determine whether the effects of managed care on the patient-PCP relationship are mediated by access to, continuity with, and choice of primary care practitioners. Our hypotheses are summarized in the conceptual framework presented in Figure 1.
FIGURE 1.
Conceptual framework. Managed health plans are hypothesized to negatively affect the patient-PCP relationship through 3 pathways: (1) one dependent on access to and continuity with primary care practitioners, 2 attributes of primary care delivery; (2) another mediated by an effect on choice of PCP; and, (3) an independent pathway in which managed health plan attributes have a direct impact on the patient-PCP relationship.
CONCEPTUAL FRAMEWORK
We hypothesized that managed health plans negatively affect the patient-PCP relationship through 3 pathways. The first is via managed care's effect on choice of PCP. Selective contracting limits patients' choice of PCPs, thereby reducing the likelihood that patients will choose a PCP with whom they can develop a sustained partnership. The second is a pathway dependent on access to and continuity with primary care practitioners, 2 attributes of primary care delivery. Better access to and continuity with PCPs increase the chances that patients will use their PCP, rather than other practitioners, for new and continuing health problems.13 Finally, we hypothesized that there is an independent pathway in which managed health plan attributes have a direct impact on the patient-PCP relationship.
The literature suggests that managed health plans are associated with better financial accessibility and possibly poorer organizational access than nonmanaged health plans.14,15 As a consequence, the overall effect of managed care on access to primary care practitioners may be small or even mixed. Patients enrolled in managed health plans have less continuity with PCPs than do their counterparts, largely because of forced health plan switching.8,9 On the other hand, requiring that patients select a specific physician, a common requirement of health maintenance organizations, could lessen this effect.
Patients trust their physicians more than they trust their health plans.11 Because gatekeeping arrangements place primary care physicians in the role of cost controller, patients may see them as fiduciary agents of the health plan. Intertwining physicians' clinical roles with gatekeeping arrangements could have the effect of displacing patients' mistrust with their health plans onto their PCPs.10 Difficulty obtaining specialty referrals has been associated with lower trust and confidence in primary care physicians5 and a desire to change plans.16 Utilization management may also threaten the patient-physician relationship. Patients who do not receive the care their physicians recommend because of health plan denials may lose faith in their physicians' abilities to act as their advocates.10
Our conceptualization of the patient-physician relationship is based on Emanuel and Dubler's model.17 The model posits that the interpersonal aspects of this relationship include communication, compassion, competence, and trust. Similar concepts have been identified in qualitative studies on aspects of the patient-physician relationship that individuals value most.18,19 These interactions benefit from accessible and continuous relationships and are threatened by managed care constraints that deter physicians from acting on their patients' behalf. When health plans deny services, patients may lose confidence in their physicians' technical proficiencies.10
METHODS
Data Source
Data for this study come come from the 1996–1997 Community Tracking Study Household Survey. The purpose of this survey is to monitor the effects of health system change on health care among civilian, noninstitutionalized persons in the contiguous 48 states of the United States. The survey was administered to a nationally representative sample of people from 60 local health care markets, which were randomly selected using stratified sampling with probability proportional to population size. To improve precision of national estimates, a supplemental sample was obtained using simple random sampling of individuals constituting about 10% of the total sample. A multistage probability sampling strategy was used to select households.
The survey was administered by telephone using random-digit-dialing sampling. Families without a working telephone were included in the sample: field staff used cellular telephones to enable families to complete interviews. A family informant completed the majority of the survey. Information was gathered on up to 8 adults in the household (mean 2.7 persons/household). Sixty-eight percent of the random-digit-dialing and field samples completed the household composition questions, and 95% of that sample completed the insurance questions for a cumulative response rate of 65%. Survey methodology is described in detail elsewhere.20–22
Study Sample
Several exclusion criteria were employed to obtain the study sample. First, to examine the effects of access to and continuity with primary care practitioners, the sample was restricted to people whose last visit in the past 12 months was made to their usual source of care—the “place they usually go to when [they] are sick or need advice about [their] health.” We made this restriction because some of the patient-physician relationship items were linked to the practitioner whom the individual last visited. We equated the usual source of care with the primary care practitioner, because having a place or clinician to go to for routine and illness care is the hallmark feature of primary care.23 Second, we excluded children ages <18 years from the study sample, because information on some of the patient-physician relationship items was not collected for this age group. Third, because of small sample sizes, adults aged 18 to 64 years with military or public insurance coverage that was not Medicare or Medicaid were excluded. Fourth, we excluded persons older than age 64 years, because of the substantial differences in health care financing between elderly and nonelderly adults. Finally, we excluded insured persons whose last visit was not covered by their current health plan.
These selection criteria resulted in a final, unweighted sample size of 19,415, 45.6% of all nonelderly adults in the original sample.
Patient-PCP Relationship Scale
Because we used items that were linked to patients' reports about visits made with their PCPs, we called this measure the patient-PCP relationship scale. The scale was constructed from the 7 items in the survey instrument that were related to the patient-practitioner relationship. Four items assessed patients' trust. The instructions for the trust items asked respondents to think about the “doctor [they] usually see when [they] are sick or need advice.” Each item had 5 response options that ranged from strongly agree to strongly disagree. The items asked respondents whether they “think [their] doctor may not refer [them] to a specialist when needed,” whether they “trust [their] doctor to put [their] medical needs above all other considerations,” whether they “think [their] doctor is strongly influenced by health insurance company rules when making decisions about medical care,” and whether they “sometimes think that [their] doctor might perform unnecessary tests or procedures.”
The remaining 3 items were asked about the physician seen during the last medical visit. Regarding patient-physician communication, the second content area represented in the scale, respondents rated from poor to excellent “how well [their] doctor listened to [them]” and “how well the doctor explained things.” Finally, respondents rated the doctor's competence: “how would you rate the thoroughness and carefulness of the examination and treatment you received.”
Items were given equal weight for the scale. A scale score was obtained if no more than 2 of the items were missing. The scale had a Cronbach's α of 0.80. Principal component factor analysis revealed that the 7-item scale could be separated into 2 subscales, one containing the trust items only and the other containing the communication and competence items. In sensitivity analyses that compared findings from the 2 subscales with the combined scale, we found similar effect sizes and statistical conclusion validity for all analyses done with the combined scale. Thus, for simplicity, we elected to present results for the combined scale only.
Managed Care and Primary Care Variables
Managed health plan characteristics included respondents' perceptions of whether their plan (1) used a provider network, (2) required patients to select a primary care practitioner, and (3) required patients to obtain authorization for specialty referrals from a primary care practitioner. These items were coded as yes/no responses. The payer variable had 5 categories: Medicare, Medicaid, Employer-Based Health Insurance, Individually Purchased Health Insurance, and Uninsured.
All individuals in the study sample had a usual source of care, which was considered their primary care delivery site.23 Continuity with the primary care site was examined using 2 items. The first divided individuals into those who usually see the same clinician at the primary care site versus those who do not. Research has shown that having a specific clinician at the primary care site is associated with better quality of care24 and lower risk of hospitalization,25 than not having a single clinician at the primary care delivery site. The second item separated the sample into persons whose relationship with their primary care source was <12 months and ≥12 months. The evidence for a positive impact on quality of care due to longitudinal relationships between patients and physicians is compelling and extensive.23
Access to care was assessed by travel time to the primary care site (geographic access) and 2 organizational access measures—the length of time the individual waited for an appointment and the length of the office wait. Each of these items was linked to the person's last visit, which for all members of the study sample had been made with their primary care delivery site. We dichotomized these three variables at logical cut-points based on their empirical distributions: 30 minutes for travel time and office wait and 5 days for appointment wait. These cut-points are consistent with prior research on access to primary care practitioners.13
The measure we used for perceived choice of primary care practitioners was based on respondents' satisfaction with “the choice [they] have for primary care doctors.” The variable was dichotomized into those very satisfied versus those who were somewhat satisfied or dissatisfied.
Data Analysis
Data were weighted to provide estimates representative of the continental United States and to account for nonresponse. We used SUDAAN software (release 7.50; Research Triangle Institute, Research Triangle Park, NC) to calculate parameter estimates that accounted for the sampling weights and complex sample design.26 The use of SUDAAN allowed us to correct for the correlation of responses within markets and households.
The central questions addressed in this study were concerned with managed care effects on primary care delivery and the patient-PCP relationship. Model specification was based on those variables that Reschovsky proposed for minimizing selection bias in insurance studies using the Community Tracking Study.22
Differences in populations across markets were controlled by using dummy variables for the 60 local health care markets that formed the core of the survey sample (the reference population was composed of individuals in the supplemental sample). Personal characteristics of individuals were adjusted for using a set of health status and sociodemographic variables. Health status was assessed by entering indicator variables for all 12 items of the SF-12 Physical and Mental Health Summary Scales.27 Sociodemographics included age, age-squared, gender, race/ethnicity (white, African American, Hispanic), education (less than high school, high school, some college, bachelor's degree, graduate school), marital status (yes/no), family income, family income ≤200% of the federal poverty line, family spent more than five percent of the household income on out-of pocket health care costs (yes/no), presence of a family member in fair/poor health, and number of people in the family.
Individual preferences for health care may be related to both selection of type of health plan and patients' assessments of their relationships with their primary care practitioners. We therefore controlled for these preferences using 2 items, both measures on a 5-point Likert scale. The first assessed risk aversion: “I'm more likely to take risks than the average person.” The second assessed willingness to trade off between out-of-pocket costs and choice of providers: “I would be willing to accept a limited choice of physicians and hospitals if I could save money on my out-of-pocket costs for health care.”
Using logistic regression, we tested the relationship between each of the 3 managed health plan attributes and access to primary care, continuity, and perceived choice of primary care physicians. These analyses controlled for population and geographic variables as described above. Because the outcomes in these analyses were relatively common and odds ratios are biased for responses with frequencies greater than 10%,28 we transformed the log odds parameter estimates into probabilities.29 The adjusted probabilities were of magnitude similar to that of the unadjusted proportions. Statistical significance for the managed health plan variables was obtained from the Wald χ2 test of their β coefficients.
Three multivariable linear regression models were sequentially developed to assess managed care effects on the patient-PCP relationship. The first model tested the association of the managed health plan characteristics and insurance payer on the patient-PCP scale score. The second determined if the managed health plan effects changed with addition of the access and continuity variables. The third examined how addition of the choice of primary care physicians variable influenced the size of the managed health plan effects. We expected parameter estimates to move closer to zero with the addition of the primary care and choice variables, if they mediated the effect of managed care and had a positive effect on the patient-PCP relationship.
RESULTS
The mean age of the study population was 41 years (SD, 12 years), and 57% was female. Hispanics constituted 9% and African Americans 13% of the sample. The median household income was $41,000. Most (73%) of the study population had employer-based health insurance, 7% had individually purchased private insurance, 5% had Medicare, and 5% had Medicaid. Adults included in the study population were less likely to be uninsured than adults excluded because of the selection criteria (10% vs 21%; P < .001). Annual out-of-pocket medical costs that exceeded 5% of household income were reported by 14% of the sample. The mean patient-PCP scale score was 4.10 (range 1–5), and the median was 4.29.
Eighty-one percent of respondents had travel times to their PCP's office <30 minutes, 68% had office waits <30 minutes, and 59% had appointment waits <5 days. Eighty-six percent identified a specific clinician they usually see at the primary care site, and 87% had a relationship longer than 12 months with their primary care practitioner.
The most commonly reported managed health plan characteristic was the requirement that members use a provider network (64%), followed by the need for physician referral authorization (55%), and select a primary care physician (47%). Most adults (73%) in the study sample reported that their health plan had at least 1 of these 3 managed care characteristics. Similar prevalences of these managed care characteristics were found among insured adults excluded from the study population.
None of the 3 managed care variables was statistically associated with all 3 access variables (Table 1). Each of the managed care variables was positively associated with presence of a specific clinician at patients' primary care delivery sites. However, all 3 managed care variables had negative associations with the duration of patients' relationships with their PCPs. The probability of patients being very satisfied with their choice of PCPs was reduced by all 3 managed care variables.
Table 1.
Managed Care Effects on Primary Care*
| Access to PCP | Continuity with PCP | Choice of PCP | |||||
|---|---|---|---|---|---|---|---|
| Managed Care Characteristic | Weighted, n (1,000s) | Travel Time to PCP <30 min, % | PCP Office Wait <30 min, % | PCP Appointment Wait <5 days, % | Have a Specific Clinician, % | Duration of Relationship with PCP >12 months, % | Very Satisfied with Choice of PCP, % |
| Plan uses provider network | |||||||
| Yes | 46,521 | 81.2 | 68.5 | 59.0 | 87.0 | 85.9 | 68.0 |
| No | 25,799 | 80.1 | 66.2 | 59.1 | 83.9 | 88.6 | 70.2 |
| Difference | NS | 2.3† | NS | 3.1‡ | −2.7‡ | −2.2§ | |
| Members required to select a PCP | |||||||
| Yes | 33,639 | 81.3 | 67.8 | 57.5 | 87.1 | 85.5 | 66.2 |
| No | 38,681 | 80.4 | 67.5 | 60.3 | 84.8 | 88.2 | 71.0 |
| Difference | NS | NS | −2.8‡ | 2.3‡ | −2.7‡ | −4.8‡ | |
| PCP authorizes specialty referrals | |||||||
| Yes | 39,445 | 81.1 | 67.8 | 58.1 | 86.5 | 85.4 | 67.1 |
| No | 32,875 | 80.4 | 67.5 | 60.2 | 85.2 | 88.8 | 70.8 |
| Difference | NS | NS | −2.1§ | 1.3* | −3.4‡ | −3.7‡ | |
The table presents probabilities adjusted for population differences due to health care market location and personal characteristics, including sociodemographics, health status, and individual preferences.
.001 ≤ P < .01.
P > .001.
.01 ≤ P < .05.
PCP, primary care practioner; NS, not significant.
Table 2 shows results from 3 regression models in which the patient-PCP scale was regressed on managed care, primary care, and controlling variables. In Model 1, use of a provider network was not significantly associated with the patient-PCP relationship, and requirements that patients select a primary care physician were associated with the greatest reduction in scale scores. Uninsured adults had significantly lower patient-PCP relationship scale scores than insured counterparts.
Table 2.
Managed Care, Primary Care, and Patients' Relationships with Primary Care Practitioners (PCPs)*
| Dependent Variable is Patient-PCP Relationship Scale Score | |||
|---|---|---|---|
| Covariates | Model 1: β (SE) | Model 2: β (SE) | Model 3 β (SE) |
| Intercept | 4.49 (0.16) | 3.96 (0.17) | 3.39 (0.16) |
| Managed care characteristics | |||
| Plan uses provider network | 0.00 (0.02) | 0.00 (0.02) | −0.01 (0.01) |
| Members required to select PCP | −0.12 (0.02)† | −0.12 (0.02)† | −0.08 (0.01)† |
| PCP authorizes specialty referrals | −0.05 (0.02)‡ | −0.04 (0.02)§ | −0.03 (0.01)§ |
| Payer | |||
| Medicare | 0.03 (0.04) | 0.04 (0.04) | 0.01 (0.03) |
| Employer-based private insurance | ref | ref | ref |
| Individually purchased private insurance | −0.01 (0.03) | 0.00 (0.03) | 0.00 (0.02) |
| Medicaid | 0.04 (0.04) | 0.08 (0.04)§ | 0.03 (0.03) |
| Uninsured | −0.15 (0.02)† | −0.10 (0.03)† | −0.06 (0.02)§ |
| PCP characteristics | |||
| Access to PCP | |||
| Travel time to PCP <30m | 0.02 (0.01) | 0.02 (0.01) | |
| PCP office wait <30m | 0.30 (0.01)† | 0.22 (0.01)† | |
| PCP appointment wait <5d | 0.02 (0.01) | 0.00 (0.01) | |
| Continuity with PCP | |||
| PCP is a specific clinician | 0.28 (0.02)† | 0.17 (0.02)† | |
| Duration of relationship with PCP ≥12 months | 0.12 (0.02)† | 0.05 (0.02)‡ | |
| Choice of PCP | |||
| Very satisfied with choice of PCP | 0.72 (0.01)† | ||
| R2 for model | 0.12 | 0.17 | 0.34 |
Regression models controlled for population differences due to health care market location and personal characteristics, including socio-demographics, health status, and individual preferences.
P > .001.
.001 ≤ P < .01.
.01 ≤ P < .05.
ref, reference group.
The addition of primary care variables in Model 2 improved the explanatory power of the model from 11% to 17%. Shorter office waits, having a specific clinician at the primary care site, and longer relationships with primary care practitioners were associated with higher scale scores. Primary care did not appear to mediate health plan effects, because the size of the managed care variable coefficients changed little between Models 2 and 1. However, the effect size for no insurance moved closer to zero, suggesting that the poorer patient-PCP relationships among uninsured adults were mediated in part by less access to and continuity with primary care practitioners.
Addition of the perceived choice of primary care doctors variable (Model 3) had a substantial effect on the explanatory power of the model, increasing it from 17% to 34% of variance explained by the linear predictors. Higher satisfaction with choice of primary care doctors was associated with substantially higher ratings of the patient-PCP relationship. Holding the effect of primary care physician choice constant, the β coefficients for managed care characteristics move closer to zero. However, the amount of change in the β coefficients suggests that the health plan effects on the patient-physician relationship are only partly mediated by reduced provider choice. The no insurance parameter estimate also moved closer to zero, suggesting that uninsured adults have poorer choice of primary care practitioners than do their insured counterparts.
DISCUSSION
This study provides new information on the mechanisms by which managed care influences patients' relationships with their primary care practitioners. Gatekeeping arrangements, as measured by requirements that patients select a primary care physician or specialty referral authorization requirements, were associated with lower ratings of the patient-PCP relationship. Presence of a provider network had no association with the patient-PCP relationship. Our hypotheses regarding managed care effects on primary care were partially supported by study results. We found few differences in access to PCPs by managed care characteristics. Managed care had mixed effects on measures of continuity of care. Patients in managed health plans were more likely to have continuity with a specific clinician at the primary care delivery site, but less likely to have had a relationship longer than 12 months with the primary care site, compared with counterparts. Gatekeeping arrangements link patients with a specific practitioner, which is a potential benefit of managed health care. However, forced health plan switching, which is more common among managed compared with nonmanaged care plan enrollees,8,9 may explain the poorer longitudinal continuity with a practitioner.
The absence of a strong effect of managed care on primary care delivery is supported by other studies that have found few differences in primary care experiences due to managed care for patients who obtained services from physicians in network-model HMOs.9,14,30 Those differences that do exist between managed and indemnity health plans can be attributed to poorer primary care performance among group-model and staff-model HMOs.14,30 It is important to note that the primary care measures included in the Community Tracking Study covered only 2 core delivery functions of primary care—access and continuity. We did not assess the effects of managed health plans on other primary care attributes such as first-contact care, provision of a comprehensive set of services, or coordination of services between providers or across time.
Poorer perceived choice of primary care doctors among patients in managed health plans was an important mediator of the managed care effects on the patient-physician relationship. However, the managed care effects were not mediated by access to or continuity with primary care practitioners. Even after controlling for patient, primary care, and PCP choice variables, managed care had a negative effect on the patient-PCP relationship. This direct effect of managed care on the patient-physician relationship may be mediated through behavioral changes in physician communication style.11
This study relied on respondents' reports of their health plans to form the managed care variables. The validity of these responses may be suspect.31 A study by Kao et al. provides information on the direction of this potential respondent bias.11 Only one third of 2,086 adults could correctly identify their physician's method of payment as salary, capitation, or fee-for-service. Although actual physician payment method in that study was a stronger correlate of patients' trust in their physicians, perceived physician payment showed the same trends. Thus, using patient perceptions of their health plan characteristics probably biases findings regarding effects on the patient-PCP relationship toward the null, suggesting that the effect sizes in this study may be underestimated.
This study employed a cross-sectional study design and provided evidence for statistical association between managed health plan characteristics and the patient-PCP relationship. The cross-sectional study design, however, limits the strength of causal inferences. For instance, patients who experience better relationships with their primary care practitioners may be more likely to evaluate their choice of primary care doctors favorably. Longitudinal studies or intervention trials are needed to determine if changes in health plan restrictions qualitatively or quantitatively influence the patient-PCP relationship.
Shorter office waits, having a specific clinician as the PCP, longer relationships, and better perceived choice of primary care physicians have beneficial effects on the patient-PCP relationship. Others have also reported that the duration of the patient-physician relationship and physician choice were positively associated with trust in physicians.11 Promoting these aspects of primary care, therefore, is likely to facilitate the development of stronger partnership relationships between patients and their primary care practitioners.
However, health care systems that reorganize to promote the doctor-patient relationship must take into consideration not only the effects of managed care and primary care delivery but also the interviewing skills of their physicians. The evolution of medicine from paternalism to a patient-centered approach is well-documented.32 Patient-centered medicine recognizes the value of patient autonomy and explicitly incorporates patient values and preferences into medical decisions.33 Effective methods for teaching these skills have been demonstrated in a randomized controlled trial.34,35 The patient-centered approach to the patient-practitioner relationship enhances patient satisfaction,36 continuity of care,37 and health outcomes.38 Improving doctors' interviewing skills is a necessary first step toward strengthening the doctor-patient relationship, and may even attenuate any negative effects that result from health system change.
We found no differences in patients' relationships with their primary care practitioners among patients with employer or privately financed insurance or those with either Medicaid or Medicare. A striking finding, however, was the poorer experiences that uninsured patients had with their primary care practitioners compared with those of their insured counterparts. Much of this effect was mediated by the uninsured's poorer access, continuity, and provider choice. Lack of insurance appears to prevent individuals from forming satisfying relationships with PCPs (because of limited choice) and maintaining those relationships if they are fortunate enough to form one (because of poorer access and continuity). Thus, this study adds to the large body of evidence regarding the importance of insurance to the quality of health care delivery.
In part as a response to the managed care backlash, health insurance plans have been loosening restrictions on patients' access to practitioners. Managed health plans that loosen restrictions on provider choice or relax gatekeeping arrangements will likely experience higher patient satisfaction with their primary care practitioner relationships. Policymakers must recognize that these organizational changes may enhance the quality of the patient-practitioner relationship, while simultaneously weakening cost containment efforts. This type of cost–quality trade-off is one of the central managed care policy challenges now facing the nation.
Acknowledgments
This research was supported by Robert Wood Johnson Foundation grant no. 036484.
REFERENCES
- 1.Donaldson MS, Yordy KD, Lohr KN, Vanselow N, editors. Primary Care: America's Health in a New Era. Washington D.C.: National Academy Press; 1996. [PubMed] [Google Scholar]
- 2.Leopold N, Cooper J, Clancy C. Sustained partnership in primary care. J Fam Pract. 1996;42:129–37. [PubMed] [Google Scholar]
- 3.Hjortdahl P, Laerum E. Continuity of care in general practice: effect on patient satisfaction. BMJ. 1992;304:1287–90. doi: 10.1136/bmj.304.6837.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Emanuel EJ, Brett AS. Managed competition and the patient-physician relationship. N Engl J Med. 1993;329:879–82. doi: 10.1056/NEJM199309163291213. [DOI] [PubMed] [Google Scholar]
- 5.Grumbach K, Selby JV, Damberg C, et al. Resolving the gatekeeper conundrum: what patients value in primary care and referrals to specialists. JAMA. 1999;282:261–6. doi: 10.1001/jama.282.3.261. [DOI] [PubMed] [Google Scholar]
- 6.Lake T. Do HMOs make a difference? Consumer assessments of health care. Inquiry. 1999;36:411–8. [PubMed] [Google Scholar]
- 7.Miller RH, Luft HS. Managed care plans: characteristics, growth and premium performance. Annu Rev Public Health. 1994;15:437–59. doi: 10.1146/annurev.pu.15.050194.002253. [DOI] [PubMed] [Google Scholar]
- 8.Davis K, Collins KS, Schoen C, Morris C. Choice matters: enrollees' views of their health plans. Health Aff (Millwood) 1995;14:100–12. doi: 10.1377/hlthaff.14.2.99. [DOI] [PubMed] [Google Scholar]
- 9.Flocke SA, Stange KC, Zyzanski SJ. The impact of insurance type and forced discontinuity on the delivery of primary care. J Fam Pract. 1997;45:129–35. [PubMed] [Google Scholar]
- 10.Mechanic D, Schlesinger M. The impact of managed care on patients' trust in medical care and their physicians. JAMA. 1996;275:1693–7. [PubMed] [Google Scholar]
- 11.Kao AC, Green DC, Zaslavsky AM, Koplan JP, Cleary PD. The relationship between method of physician payment and patient trust. JAMA. 1998;280:1708–14. doi: 10.1001/jama.280.19.1708. [DOI] [PubMed] [Google Scholar]
- 12.Schmittdiel J, Selby JV, Grumbach K, Quesenberry CP., Jr Choice of a personal physician and patient satisfaction in a health maintenance organization. JAMA. 1997;278:1596–9. [PubMed] [Google Scholar]
- 13.Forrest CB, Starfield B. Entry into primary care and continuity: the effects of access. Am J Public Health. 1998;88:1330–6. doi: 10.2105/ajph.88.9.1330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Safran DG, Tarlov AR, Rogers WH. Primary care performance in fee-for-service and prepaid health care systems: results from the Medical Outcomes Study. JAMA. 1994;271:1579–86. [PubMed] [Google Scholar]
- 15.Mark T, Mueller C. Access to care in HMOs and traditional insurance plans. Health Aff. 1996;15:81–7. doi: 10.1377/hlthaff.15.4.81. [DOI] [PubMed] [Google Scholar]
- 16.Kerr EA, Hays RD, Lee ML, Siu AL. Does dissatisfaction with access to specialists affect the desire to leave a managed care plan? Med Care Res Rev. 1998;55:138–51. doi: 10.1177/107755879805500104. [DOI] [PubMed] [Google Scholar]
- 17.Emanuel EJ, Dubler NN. Preserving the physician-patient relationship in the era of managed care. JAMA. 1995;273:323–9. [PubMed] [Google Scholar]
- 18.Thom DH, Campbell B. Patient-physician trust: an exploratory study. J Fam Pract. 1997;44:169–76. [PubMed] [Google Scholar]
- 19.O'Malley AS, Forrest CB, O'Malley PG. Low-income women's priorities for primary care: a qualitative study. J Fam Pract. 2000;49:141–6. [PubMed] [Google Scholar]
- 20.Kemper P, Blumenthal D, Corrigan JM, et al. The design of the Community Tracking Study: a longitudinal study of health system change and its effects on people. Inquiry. 1996;33:195–206. [PubMed] [Google Scholar]
- 21.Metcalf CE, Kemper P, Kohn LT, Pickereign JD. Site Definition and Sample Design for the Community Tracking Study (Technical Publication I) Washington, DC: Center for Studying Health System Change; 1996. [Google Scholar]
- 22.Reschovsky JD. Do HMOs make a difference? Data and methods. Inquiry. 1999;36:378–89. [PubMed] [Google Scholar]
- 23.Starfield B. Primary Care: Balancing Health Needs, Services, and Technology. New York: Oxford University Press; 1998. [Google Scholar]
- 24.Lambrew JM, DeFrisse GH, Carey TS, Ricketts TC, Biddle AK. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–51. doi: 10.1097/00005650-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Mainous AG, Gill JM. The importance of continuity of care in the likelihood of future hospitalization: is site of care equivalent to a primary care clinician? Am J Public Health. 1998;88:1539–41. doi: 10.2105/ajph.88.10.1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shah BV, Barnwell BG, Bieler GS. SUDAAN User's Manual Release 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997. [Google Scholar]
- 27.Ware JE, Kosinski M, Keller SD. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd Ed. Boston, Mass: The Health Institute, New England Medical Center; 1995. [Google Scholar]
- 28.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 29.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: John Wiley and Sons; 1989. [Google Scholar]
- 30.Safran DG, Rogers WH, Tarlov AR, et al. Organizational and financial characteristics of health plans: are they related to primary care performance? Arch Intern Med. 2000;160:69–76. doi: 10.1001/archinte.160.1.69. [DOI] [PubMed] [Google Scholar]
- 31.Nelson DE, Thompson BL, Davenport NJ, Penaloza LJ. What people really know about their health insurance: a comparison of information obtained from individuals and their insurers. Am J Public Health. 2000;90:924–8. doi: 10.2105/ajph.90.6.924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laine C, Davidoff F. Patient-centered medicine: a professional evolution. JAMA. 1996;275:152–6. [PubMed] [Google Scholar]
- 33.Quill TE, Brody H. Physician recommendations and patient autonomy: finding a balance between physician power and patient choice. Ann Intern Med. 1996;125:763–9. doi: 10.7326/0003-4819-125-9-199611010-00010. [DOI] [PubMed] [Google Scholar]
- 34.Smith RC, Lyles JS, Mettler J, et al. The effectiveness of intensive training for residents in interviewing. Ann Intern Med. 1998;128:118–26. doi: 10.7326/0003-4819-128-2-199801150-00008. [DOI] [PubMed] [Google Scholar]
- 35.Smith RC, Marshall-Dorsey AA, Osborn GG, et al. Evidence-based guidelines for teaching patient-centered interviewing. Patient Educ Couns. 2000;39:27–36. doi: 10.1016/s0738-3991(99)00088-9. [DOI] [PubMed] [Google Scholar]
- 36.Hall JA, Roter DL, Katz NR. Meta-analysis of correlates of provider behavior in medical encounters. Med Care. 1988;26:657–75. doi: 10.1097/00005650-198807000-00002. [DOI] [PubMed] [Google Scholar]
- 37.Kasteler J, Kane RL, Olsen DM, Thetford C. Issues underlying prevalence of “doctor shopping” behavior. J Health Soc Behav. 1976;17:328–39. [PubMed] [Google Scholar]
- 38.Kaplan SH, Greenfield S, Ware JE. Impact of the doctor-patient relationship on the outcomes of chronic disease. In: Stewart M, Roter D, editors. Communicating with Medical Patients. London: Sage Publications; 1989. [Google Scholar]