Abstract
OBJECTIVE
This study describes primary care discussions with patients who screened positive for at-risk drinking. In addition, discussions about alcohol use from 2 clinic firms, one with a provider-prompting intervention, are compared.
DESIGN
Cross-sectional analyses of audiotaped appointments collected over 6 months.
PARTICIPANTS AND SETTING
Male patients in a VA general medicine clinic were eligible if they screened positive for at-risk drinking and had a general medicine appointment with a consenting provider during the study period. Participating patients (N = 47) and providers (N = 17) were enrolled in 1 of 2 firms in the clinic (Intervention or Control) and were blinded to the study focus.
INTERVENTION
Intervention providers received patient-specific results of positive alcohol-screening tests at each visit.
MEASURES AND MAIN RESULTS
Of 68 visits taped, 39 (57.4%) included any mention of alcohol. Patient and provider utterances during discussions about alcohol use were coded using Motivational Interviewing Skills Codes. Providers contributed 58% of utterances during alcohol-related discussions with most coded as questions (24%), information giving (23%), or facilitation (34%). Advice, reflective listening, and supportive or affirming statements occurred infrequently (5%, 3%, and 5%, of provider utterances respectively). Providers offered alcohol-related advice during 21% of visits. Sixteen percent of patient utterances reflected “resistance” to change and 12% reflected readiness to change. On average, Intervention providers were more likely to discuss alcohol use than Control providers (82.4% vs 39.6% of visits; P = .026).
CONCLUSIONS
During discussions about alcohol, general medicine providers asked questions and offered information, but usually did not give explicit alcohol-related advice. Discussions about alcohol occurred more often when providers were prompted.
Keywords: alcohol, primary care, brief interventions, motivational interviewing
Over 21 million U.S. adults suffer from alcohol abuse or dependence,1 and many others drink at levels known to increase their risk for adverse psychosocial, legal, and health consequences.2,3 Each year, many of these patients see health care providers, but less than 20% report having received advice to change their drinking.4
A number of randomized controlled trials of brief primary care interventions with at-risk drinkers have demonstrated decreased alcohol consumption after brief counseling or advice.5–8 Although the exact intervention studied in each trial has varied, most trials taught providers to engage in empathetic, nonconfrontational, patient-centered discussions.9 Such discussions included assessment of the patient's drinking, alcohol-related problems, and readiness to change drinking, as well as feedback to patients on the relationship between their drinking and health. Explicit advice for patients to drink moderately or abstain has been included in most brief interventions found to be effective in randomized controlled trials.5–8,10
On the basis of these brief intervention trials and meta-analyses of their findings,9,11–13 leading academic and scientific review groups have urged clinicians to routinely screen all primary care patients for at-risk drinking and counsel those patients who screen positive.2,14,15 However, the actual effect of alcohol-screening programs on alcohol-related discussions during primary care appointments is not known. Exit interviews with patients,16,17 and reports by physicians,18 have been used to study alcohol-related discussions with primary care patients who screen positive for at-risk drinking, but no published study has directly observed or recorded primary care encounters with these patients.
We conducted a 6-month study evaluating the feasibility of audiotaping clinic visits of general medicine patients who screened positive for at-risk drinking. The study clinic included 2 firms, one of which had been randomly selected to receive a provider-prompting intervention as part of the Ambulatory Care Quality Improvement Project (ACQUIP) study. This report describes audiotaped discussions about alcohol use and compares rates of alcohol-related discussions in the Intervention and Control firms. We specifically sought to evaluate whether providers were including key components of brief interventions (e.g., feedback and advice) and if the style of these discussions was patient-centered.
METHODS
Setting and Participants
The study was carried out in 2 firms of a General Internal Medicine Clinic participating in the multi-site VA ACQUIP study.19 The ACQUIP trial used mailed alcohol-screening questionnaires to identify at-risk drinking and 5 other target conditions (depression, chronic lung disease, hypertension, coronary artery disease, and/or diabetes). Patients consented to participate in ACQUIP by completing and returning mailed questionnaires; all providers in the participating clinics were included in the ACQUIP trial. One of 2 firms at each site received the ACQUIP intervention. Providers in ACQUIP Intervention firms were prompted to address at-risk drinkers' alcohol use by receiving a detailed report of patients' alcohol-screening responses at each General Internal Medicine Clinic visit, along with reports for up to 5 other conditions. The audiotape study described in this report used ACQUIP's alcohol-screening data to identify at-risk drinkers and compared discussions about alcohol use in Intervention and Control firms at 1 of 7 ACQUIP sites. The 6-month audiotape study began several months after the start of the 2-year ACQUIP trial.
All General Internal Medicine Clinic providers who were not involved in the design and institutional approval of this audiotape study were eligible to participate. Each provider practiced in only 1 firm of the clinic. Patients of consenting providers were eligible for the audiotape study if they screened positive for at-risk drinking (defined below) and indicated on a mailed ACQUIP questionnaire that they were willing to consider participating in an audiotape study of patient-provider communication.
Patients screened positive for “at-risk drinking” if they reported on the ACQUIP Screening Questionnaire that they drank any alcohol in the past year and scored 1 or more points on an 8-item augmented CAGE questionnaire.20 This augmented CAGE included the 4 CAGE questions (1 point each), a question asking whether the patient had ever had a drinking problem (1 point), and AUDIT questions 1 through 3 about the quantity and frequency of typical or episodic heavy drinking (1 point if ≥14 drinks/week on questions 1 and 2, and 1 point if ≥5 drinks on an occasion on AUDIT questions 2 or 3).20 This 8-item screening questionnaire is very sensitive (92%) with moderate specificity (50%) compared with an interview diagnosis of past-year hazardous drinking or active alcohol abuse or dependence.
We attempted to audiotape all General Internal Medicine Clinic visits of consenting patients during the 6-month study period. Patients and providers were blinded regarding the focus of the study on alcohol-related discussions and regarding the principal investigator (KAB), whose research related exclusively to alcohol. The investigator who presented the study to providers (CHB) was not involved with the ACQUIP study and studied ethical issues in primary care discussions. The University of Washington Human Subjects Committee and the General Internal Medicine Clinic approved the study, and all participating patients and providers gave written informed consent to participate in the audiotape study. Informed consent was first sought from providers and explicit consent was obtained for review of audiotapes by unnamed investigators.
Measures
We used 2 systems to code each utterance of alcohol-related discussions. The Motivational Interviewing Skills Code (MISC) system, developed by Miller and colleagues,21 was used to measure specific provider tasks (e.g., advice or feedback) and patient-centered behaviors (e.g., affirmation or reflective listening), as well as patient motivation. The MISC coding system is described in more detail below (see also Appendix A). In addition, to better understand the content of primary care discussions about alcohol, each patient or provider utterance during alcohol-related discussions was coded from transcripts into 1 of 3 content categories: 1) alcohol consumption or drinking pattern, 2) alcohol-related consequences (medical or otherwise), or 3) change in drinking (Appendix A). The first 2 content categories captured provider assessment and patient reports of drinking practices and related problems. The “change” category, viewed as an essential component of brief interventions, included: discussion of past treatment or change; recommendations for, consideration of, barriers to, and strategies for change; referral to treatment; or plans for future follow-up discussions relating to changes in alcohol use. Many utterances did not fit into these content categories and were coded as “not explicitly alcohol-related” (Appendix A).
Motivational Interviewing Skills Codes
We collapsed Motivational Interviewing Skills Codes into the following components of brief interventions with at-risk drinkers: asking questions; giving advice; reflecting patient statements or feelings; providing information or education regarding drinking; facilitation; emphasizing patient control; affirmation or support; and raising concerns.9 In addition, less-patient-centered behaviors coded by the MISC system were retained: confrontation and giving direction. Whereas MISC codes for reflective listening included codes for “reflections” of patients' statements or emotions during the current encounter, there was no MISC code for reflections of patients' statements or emotions from previous encounters. We therefore added a code for these “historic” reflections.
The MISC system codes statements or questions by patients into 1 of 3 categories: 1) self-motivational utterances, 2) neutral or unclassifiable utterances, or 3) counter-motivational utterances (Appendix A). Self-motivational utterances were those that directly or indirectly showed evidence of moving toward change.21 Such statements reflected recognition that drinking was a problem, concern about current drinking, a desire or an intention to change drinking, or optimism regarding the possibility of change. Counter-motivational statements were those that reflected movement away from or resistance to change. Counter-motivational statements included: arguing, interrupting, negating (lack of problem recognition; or a reluctance to cooperate, accept responsibility, follow advice, or change), and not following the discussion (inattention, not answering a question, giving no audible response, or changing the subject).22
Coding Procedures
Two nonclinician research assistants (RAs) were trained in the MISC coding system by a certified Motivational Interviewing (MI) trainer (CWD). They began their training by watching a 7-video training series on MI,23 and reading the MISC coding manual adapted for this study. Subsequently, they received 8 hours of training that consisted primarily of coding practice and feedback, until they were able to assign codes appropriately.
Coders reviewed each audiotaped visit to identify visits in which alcohol was mentioned (concordance 100%). Each audiotaped visit with any mention of alcohol use was transcribed and an RA divided transcribed visits into utterances, defined in the MISC system as complete thoughts. Specifically, the coding manual noted, “Two utterances are often run together without interruption. If two consecutive sentences merit different codes (e.g., a reflection followed by a question), they are by definition separate utterances.21” Alcohol-related discussions were independently coded by 2 RAs who were blinded to each other's coding and who were unaware that differences between the firms would be evaluated. The coders generally were in agreement regarding whether utterances were part of discussions of alcohol use, but 322 of 26,309 utterances (1.2%) were coded by only 1 RA and were therefore omitted from analyses.
Questionnaire Measures
Patient demographic and clinical characteristics and alcohol-related data were obtained from mailed ACQUIP questionnaires. Participants were also asked to complete a brief self-administered survey after the audiotape study to evaluate blinding. The survey asked whether they thought the audiotape study was evaluating “whether providers ask about symptoms or signs of …diabetes, lung disease, heart disease, high blood pressure, back pain, alcohol problems, depression, chronic pain, or other?” Response options were “yes,”“no,” and “not sure” for each of the 9 options listed.
Alcohol-related Intervention
At each Intervention firm visit during the audiotape study, ACQUIP “Drinking Practices Reports” were given to providers of patients who had screened positive for at-risk drinking and returned an ACQUIP Drinking Practices Questionnaire. The patient-specific, computer-generated Drinking Practices Reports were designed to mimic interview assessments used in brief intervention trials. Therefore, Drinking Practices Reports summarized alcohol-related data from ACQUIP Questionnaires including: average and maximum drinks per drinking day, frequency of drinking ≥6 drinks, CAGE score (0–4), AUDIT score (0–40), past-year adverse consequences of alcohol use, readiness to change drinking, and prior alcohol treatment or attendance at Alcoholics Anonymous. Drinking Practices Reports were distributed with ACQUIP Reports for other conditions and general health status. ACQUIP Intervention providers received a mean of 2.2 condition-specific reports at each visit.
At the time of this study, both firms in the study clinic were implementing preventive screening mandated by the Department of Veterans Affairs. However, rates of documented alcohol screening at the study VA hospital, based on review of medical records, remained low (18%). Two months before audiotaping began, staff providers of both firms were invited to a single 45-minute educational session about alcohol screening and counseling as part of a weekly continuing medical education conference for general medicine providers. This slide presentation was completely didactic, without demonstration or role-plays, and was focused on interpretation of alcohol screening results and the content of effective brief interventions. One slide addressed components of motivational interviewing.
Analyses
Analyses reported here are based on utterances coded into the same category by both coders. Before research assistants coded the tapes, investigators pretested and adapted the coding system for a primary care setting. During this pretesting, on the basis of a review of discordant utterances, we concluded that a consensus could not be reached on the appropriate code for some utterances. For providers, this often resulted from fragmented, incomprehensible speech. For patients, the large number of discordant utterances reflected the inherent difficulty of attributing motivation to patients' utterances when discussions did not relate to change. Therefore, utterances with discordant codes were considered unclassifiable and omitted from analyses.
Rates of any alcohol-related discussion or any alcohol-related advice were calculated for all audiotaped visits. Rates of each type of alcohol-related utterance were also calculated as a proportion of all coded patient or provider utterances. In addition, to evaluate recruitment bias, we compared demographic and clinical characteristics of the taped and untaped patient (47 vs 793) and provider (17 vs 84) populations. To assess baseline differences between the firms, we also compared characteristics of the Intervention and Control firms.
Although this pilot study was not designed to have adequate power to compare rates of counseling in the 2 firms, we conducted secondary analyses comparing the 2 firms (Intervention and Control) to inform future design of alcohol intervention trials. Patients and providers were not strictly randomly assigned to the 2 firms, but there was no known clinically meaningful difference between the firms. Moreover, the demographic and clinical characteristics of audiotaped patients in the 2 firms were nearly identical (Table 1). We compared rates of alcohol-related discussions or advice in the Intervention and Control firms based on an “intention to treat” design. (Providers in the Intervention clinic were only prompted with Drinking Practices Reports if the patient returned a Drinking Practices Questionnaire, but all were included in the Intervention firm for the purpose of these analyses.) We used the χ2 or Fisher's exact test to compare dichotomous outcomes and the Permutation t test to compare mean rates. The Permutation t test is similar to the standard t test except that it does not require normality.24 It was chosen as the most conservative statistical test of differences in means at the level of the provider, or patient-provider pair, because we had inadequate sample size to conduct multivariate analyses accounting for clustering at the level of the provider, or patient-provider pair.
Table 1.
Characteristics of General Internal Medicine Clinic Patients Who Screened Positive for At-risk Drinking and the Subsample of Audiotaped Patients
| Patients Who Screened Positive for At-risk Drinking | Taped Patients | |||||
|---|---|---|---|---|---|---|
| Not Taped (N = 793) | Taped(N = 47) | P Value* | Intervention Firm (N = 17) | Control Firm (N = 30) | P Value* | |
| Mean age, y | 60.4 | 60.8 | .848 | 63.9 | 59.0 | .158 |
| Race, n (%)† | ||||||
| White | 545 (68.7) | 38 (80.9) | .080 | 14 (82.4) | 24 (80.0) | 1.000 |
| African American | 80 (10.1) | 5 (10.6) | .806 | 1 (5.9) | 4 (13.3) | .640 |
| Other | 143 (18.0) | 4 (8.5) | .095 | 2 (11.8) | 2 (6.7) | .613 |
| Marital status, n (%)† | ||||||
| Never married | 90 (11.3) | 3 (6.4) | .292 | 0 | 3 (10.0) | .292 |
| Married /widowed | 347 (43.8) | 21 (44.7) | .901 | 8 (47.1) | 13 (43.3) | .805 |
| Separated/divorced | 340 (42.9) | 23 (48.9) | .415 | 9 (52.9) | 14 (46.7) | .679 |
| Education–completed high school, n (%)† | 441 (55.9) | 28 (59.6) | .621 | 6 (35.3) | 22 (73.3) | .011 |
| Income <$20,000, n (%)† | 534 (67.7) | 31 (66.0) | .806 | 9 (52.9) | 22 (73.3) | .156 |
| Self-reported, n (%)† | ||||||
| Hypertension | 429 (54.1) | 20 (42.6) | .123 | 8 (47.1) | 12 (40.0) | .638 |
| COPD | 200 (25.2) | 18 (38.3) | .047 | 5 (29.4) | 13 (43.3) | .345 |
| Diabetes | 147 (18.5) | 10 (21.3) | .640 | 4 (23.5) | 6 (20.0) | 1.000 |
| Coronary artery disease | 104 (13.1) | 9 (19.1) | .239 | 2 (11.8) | 7 (23.3) | .455 |
| Liver disease | 70 (8.8) | 2 (4.3) | .420 | 0 | 2 (6.7) | .528 |
| PTSD | 154 (19.4) | 13 (27.7) | .169 | 4 (23.5) | 9 (30.0) | .743 |
| Past year smoking | 356 (44.9) | 18 (38.3) | .377 | 2 (11.8) | 16 (53.3) | .005 |
| Drug abuse | 55 (6.9) | 3 (6.4) | 1.000 | 1 (5.9) | 2 (6.7) | 1.000 |
| Depression screen positive, n (%)†,‡ | 240 (30.3) | 18 (38.3) | .246 | 4 (23.5) | 14 (46.7) | .117 |
| Screening questionnaire, n (%)† | ||||||
| ≥14 drinks per typical week | 238 (30.6) | 17 (37.0) | .364 | 7 (43.8) | 10 (33.3) | .486 |
| ≥6 drinks on an occasion, past year | 715 (90.2) | 40 (85.1) | .314 | 14 (82.4) | 26 (86.7) | .692 |
| AUDIT-C ≥8 | 167 (21.8) | 13 (28.3) | .303 | 6 (37.5) | 7 (23.3) | .328 |
| CAGE score ≥2 | 375 (47.3) | 23 (48.9) | .826 | 7 (41.2) | 16 (53.3) | .423 |
Two-tailed χ2 or t test.
Denominators vary for calculation of percentages due to missing data.
Based on the 5-item Mental Health Index (MHI-5).
COPD, chronic obstructive pulmonary disease; PTSD, post-traumatic stress disorder.
Patients with more-severe problems due to drinking may need and/or receive different types of primary care interventions than do patients with less-severe problems due to drinking. Secondary analyses therefore explored the relationship between the severity of problem drinking—as reflected by alcohol-screening questionnaires—and alcohol-related discussions. A previous study had shown that a CAGE score 2 was associated with increased primary care alcohol interventions,25 but our own studies have shown that the AUDIT-C ≥8 is a stronger predictor of past-year heavy drinking and active alcohol abuse or dependence than is the CAGE (positive likelihood ratio 5.9 vs 3.1),19,26 as well as of increased mortality27 among male VA medical outpatients. To evaluate the relationship of the severity of problem drinking to alcohol-related discussions, we therefore compared alcohol-related discussions between patients with AUDIT-C scores <8 and ≥8.
Analyses were conducted using SPSS for Windows (version 10.0.7; SPSS, Inc., Chicago, Ill), except Permutation t tests, which were calculated with SAS (version 8; SAS Institute, Inc. Cary, NC).
RESULTS
Participants
Of the 34 consenting providers (34% of eligible), 17 saw consenting patients during the study and were audiotaped (Table 2). Audiotaped providers did not differ from those who were not audio-taped on any measured covariate except training status. Taped providers were less likely to be residents or fellows (35% vs 65%; P = .026).
Table 2.
Characteristics of Eligible and Audiotaped Providers
| Eligible Providers | Taped Providers | |||||
|---|---|---|---|---|---|---|
| Not Taped (N = 84) | Taped (N = 17) | P Value* | Intervention Firm (N = 5) | Control Firm(N = 12) | P Value* | |
| Sex, n (%) | .396 | .593 | ||||
| Male | 38 (47.5) | 10 (58.8) | 2 (40.0) | 8 (66.7) | ||
| Female | 42 (52.5) | 7 (41.2) | 3 (60.0) | 4 (33.3) | ||
| Provider type, n (%) | ||||||
| Resident or Fellow MD | 54 (64.3) | 6 (35.3) | .026 | 0 | 6 (50.0) | .102 |
| Faculty/Staff MD | 13 (15.5) | 6 (35.3) | .057 | 2(40) | 4 (33.3) | 1.000 |
| Family nurse practitioner | 17 (20.2) | 5 (29.4) | 2.403 | 3 (60) | 2 (16.7) | .117 |
| Patients participating per provider (range), mean n | — | 2.8(1 to 9) | — | 3.6(1 to 8) | 2.5(1 to 9) | .455 |
Two-tailed χ2 or t test.
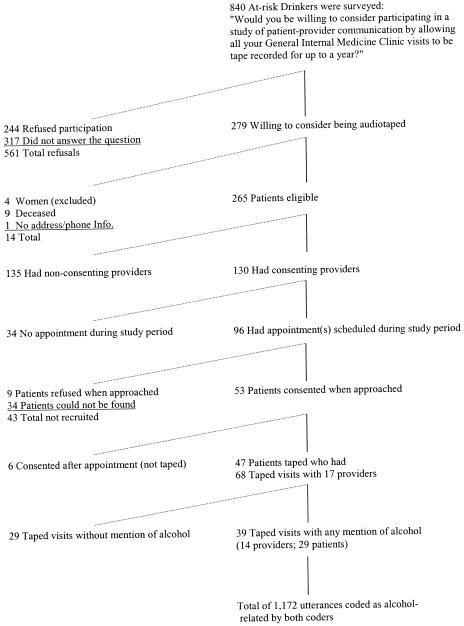
Of 840 patients who screened positive for at-risk drinking, 523 (62%) returned the questionnaire asking if they would be willing to consider being audiotaped, and 279 of respondents (53%) answered “yes” (Fig. 1). A large number of these 279 patients (n = 135) were not eligible because their providers did not consent; 4 women were excluded due to inadequate power to evaluate expected gender differences.25,28,29 Sixty-two eligible patients had appointments during the 6-month study period and were invited to participate, with 53 (85%) consenting (Fig. 1). Of consenting patients, 47 were audiotaped at least once (Table 1); 6 were never taped because they were enrolled in the study after an appointment and had no subsequent visit taped.
FIGURE 1.
Eligible and recruited at-risk drinkers.
Audiotaped patients had a mean age of 61 and a mean AUDIT score of 8.0, and were compared to nontaped patients with regard to 35 demographic and clinical characteristics, some of which are presented in Table 1. The 47 audiotaped at-risk drinkers differed from those not audiotaped (n = 793) only in the rate of chronic obstructive pulmonary disease, which was higher in the taped population (38% vs 25%; P = .05).
When surveyed after completion of the study, no patient or provider reported that the study was solely focused on problem drinking. Fifteen providers (88%) returned surveys after the audiotape study, and responded to a question asking whether they thought we were studying any of 6 listed ACQUIP conditions, “back pain,”“chronic pain,” or “other.” Ten providers (3 Intervention and 7 Control) responded “not sure” to all 9 response options. Two Control providers indicated “yes” to all 9 options, and 1 Intervention provider indicated “no” to all 9 options. These 13 providers, 76.4% of all participating providers, appear therefore to be completely blinded to the focus of the study on alcohol. Two providers—1 in the Intervention firm and 1 in the Control firm—indicated that the study was about 3 conditions by responding “yes” to problem drinking, depression, and chronic pain, and “no” or “not sure” to the 6 other options. Two nonrespondents were in the Control firm.
Discussions of Alcohol Use and Alcohol-related Advice
A total of 68 visits were taped over the 6-month study period (1 to 6 per patient and 1 to11 per provider). Thirty-nine taped visits (57%) included any mention of alcohol. Alcohol-related discussions lasted from 2 seconds (Provider: “And you're not drinking any anymore?” Patient: “Right-no.”) to 7 min 17 seconds (mean duration 1 min, 38 seconds). The longest alcohol-related discussion represented 33% of the duration of the visit. Fourteen (21%) of the taped visits included alcohol-related advice, and 12 (26%) of the 47 at-risk drinkers received alcohol-related advice during at least 1 taped visit.
Motivational Interviewing Skills
Motivational Interviewing Skills Code analyses included 1,157 utterances, 635 (55%) attributed to providers and 522 (45%) to patients (15 of 1,172 utterances were excluded from MISC analyses because coders could not determine if the patient or provider was speaking). Of the 635 alcohol-related provider utterances, 516 utterances were assigned the same MISC category code (81% agreement; κ = 0.77). Coders assigned the same MISC category code to 369 of 522 patient alcohol-related utterances (71% agreement; κ = 0.44).
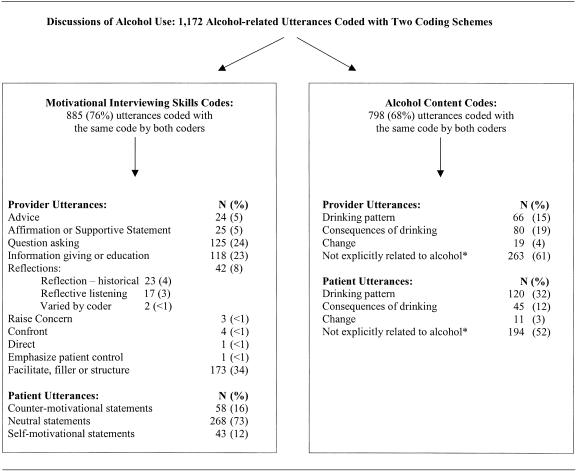
Provider utterances were coded most often as questions (24%), information giving (23%), or facilitation (34%), with only 24 (5%) of provider utterances coded as advice (Fig. 2). Of 125 questions, only 11 (9%) were coded as “open” questions by both coders; 12 others (10%) were standardized alcohol-screening questions (e.g., CAGE questions). Relatively few provider utterances were coded as affirmations or supportive statements (5%) or reflections of patients' statements or emotions (8%). Of the 42 utterances coded as “reflections,” only 17 provider utterances (3%) were coded as reflective listening by both coders. Twenty-three utterances (4%) were coded as “historical” reflections by both coders and did not represent reflective listening, and 2 reflections were assigned different reflection subcodes by the 2 coders. Less than 1% of all provider utterances were coded into each of the following codes: confrontation, giving the patient explicit directions, or raising concern about the patient's drinking. Providers varied considerably in the mean number and types of alcohol-related utterances per visit (Fig. 3).
FIGURE 2.
Alcohol-related utterances and their coding. *Utterances within alcohol-related discussions that were not explicitly related to alcohol or drinking.
FIGURE 3.
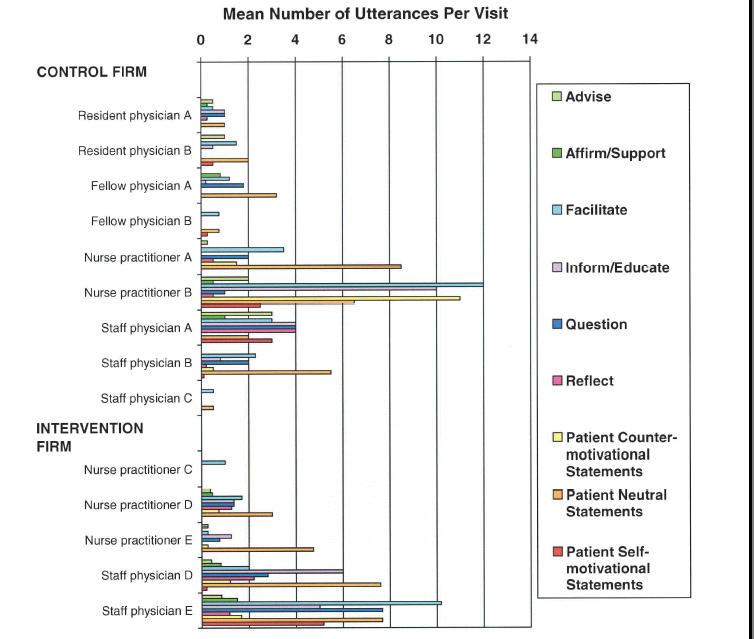
Mean number of alcohol-related utterances in each MISC code category per visit, by provider and firm. *Three providers in the Control firm did not discuss alcohol on any tape and are therefore omitted from the figure.
Of 369 patient utterances coded with the same MISC code by both coders, 43 (12%) reflected motivation toward change, whereas 58 (16%) were coded as counter-motivational statements or questions, indicative of resistance to change. Two hundred sixty-eight (73%) of the patient utterances were neutral (Fig. 2).
Alcohol-related Content
Coders assigned the same content code to 798 of 1,172 utterances during discussions about alcohol (68%; κ = 0.43). The majority of these utterances (57%) did not explicitly relate to alcohol (Fig. 2; Appendix A), while 23% and 16% related to alcohol consumption and alcohol-related consequences, respectively. Only 30 utterances (4%) related to change in drinking.
Comparison of Intervention and Control Firms
Audiotaped visits included alcohol-related discussions significantly more often in the Intervention than in the Control firm, irrespective of whether analyses were at the level of the visit, the patient, the provider, or the patient-provider pair (Table 3). A trend toward increased alcohol-related advice in the Intervention firm was also observed, but this did not reach statistical significance in the most conservative analyses (Table 3). The mean duration of alcohol-related discussions in the Intervention and Control firms were not significantly different, 1.38 and 1.37 minutes, respectively. This suggests that the intervention may have made alcohol-related discussions more likely to occur, but that it did not significantly increase the length of alcohol-related discussions.
Table 3.
Rates of Any Alcohol-related Discussion or Advice by Firm
| Intervention Firm | Control Firm | Total | P Value* | |
|---|---|---|---|---|
| Rates of any alcohol-related discussion, n (%) | ||||
| As a proportion of all taped visits | 22/27 (81.5) | 17/41 (41.5) | 39/68 (57.4) | .001 |
| As a proportion of patients taped | 15/17 (88.2) | 14/30 (46.7) | 29/47 (61.7) | .005 |
| Mean proportion of visits per provider† | — (82.4) | — (39.6) | — (52.2) | .026 |
| Mean proportion of visits per patient per provider† | — (81.3) | — (38.4) | — (51.0) | .027 |
| Rates of any alcohol-related advice, n (%) | ||||
| As a proportion of all taped visits | 9/27 (33.3) | 5/41 (12.2) | 14/68 (20.6) | .035 |
| As a proportion of patients taped | 7/17 (41.2) | 5/30 (16.6) | 12/47 (25.5) | .087 |
| Mean proportion of visits per provider† | — (29.2) | — (20.8) | —(23.3) | .643 |
| Mean proportion of visits per patient per provider† | — (30.3) | — (18.1) | — (21.8) | .510 |
Two-tailed χ2 or Permutation t test.
Five providers were in the Intervention firm; 12 were in the Control firm.
Several potential confounders of the association between firm assignment (Intervention or Control) and alcohol-related discussions were evaluated. A higher proportion of audiotaped providers in the Intervention firm were women (60% vs 33%) (Table 2), and we hypothesized that this could have accounted for the higher rate of alcohol discussions in that firm. However, female providers in this study were not significantly more likely than were male providers to discuss alcohol use (68% of visits for women verses 50% for men; P = .143). Fellows and residents (n = 6), all in the Control firm, had the lowest rate of alcohol-related discussions per visit, 40% of visits compared to 65% for other providers. However, rates of discussing alcohol use for trainees were not different from other Control providers, and when comparisons between the firms were repeated with trainees omitted, the magnitude of the differences in rates of alcohol-related discussions between Intervention and Control firms were smaller, but remained statistically significant. We also expected patients would be more likely to receive alcohol counseling if they were younger, of lower socioeconomic status, current smokers, or scored positive on the CAGE (≥2), potentially accounting for observed differences between the 2 firms.25 However, while Intervention firm patients reported less education (P = .011), more Control firm patients smoked (P = .006), and no other significant differences were observed (Table 1).
Severity of Problem Drinking and Alcohol-related Discussions
Audiotaped visits of patients with AUDIT-C scores ≥8 (n = 13) were more likely to include alcohol-related discussions than were those with AUDIT-C scores <8 (83.3% vs 45.8%; P = .006). Visits with patients with AUDIT-C scores ≥8 were also more likely to include alcohol-related advice, but the difference was not statistically significant (33.3% vs 14.6%; P = .161). Providers were significantly more likely to ask questions or offer affirming or supportive statements to patients with AUDIT-C scores ≥8 (Table 4). In addition, patients with AUDIT-C ≥8 were more likely to make self-motivational statements, less likely to make counter-motivational statements, and more likely to discuss change (Table 4). No other measure of alcohol-related discussions differed significantly between patients with AUDIT-C scores ≥8 or <8.
Table 4.
Relationship of AUDIT-C ≥8 to Alcohol-related Discussions
| AUDIT-C <8, n (%) | AUDIT-C ≥8, n (%) | P Value* | |
|---|---|---|---|
| Provider utterances coded with Motivational Interviewing Skills Codes (MISC) | |||
| Affirmation or supportive statement | 9 (1.8) | 16 (4.9) | .009 |
| Question asking | 60 (11.6) | 62 (18.4) | .004 |
| Provider utterances coded with Content Codes | |||
| Drinking pattern | 41 (19.1) | 20 (10.4) | .014 |
| Change | 4 (1.9) | 15 (7.8) | .005 |
| Patient utterances MISC | |||
| Counter-motivational statements | 44 (8.6) | 8 (2.4) | <.0005 |
| Neutral statements | 178 (34.6) | 85 (25.9) | .008 |
| Self-motivational statements | 17 (3.3) | 26 (7.9) | .003 |
| Patient utterances coded with Content Codes | |||
| Drinking pattern | 77 (36.2) | 37 (26.2) | .051 |
| Change | 1 (0.05) | 10 (7.1) | .001 |
Two-tailed χ2 or Fisher's exact test; the remainder of the MISC and Content codes were not significantly associated with AUDIT-C score.
DISCUSSION
This audiotape study of male VA patients' general medical appointments is the first to directly describe alcohol-related discussions during at-risk drinkers' primary care appointments. Over half of the taped visits included some discussion of alcohol use. During these discussions, providers primarily asked questions and gave patients information about alcohol use; only 21% of the taped visits included alcohol-related advice. Providers were rarely confrontational, but supportive statements and reflective listening also occurred relatively infrequently. Although 16% of patient statements during alcohol-related discussions reflected resistance to change, 12% suggested motivation toward change.
Research over the past 2 decades suggests that patient-centered, nonconfrontational interventions are most effective at promoting behavior change, including changes in drinking.22,30–32 While confrontation was rarely observed, important elements of effective brief interventions were missing from many alcohol-related discussions.8,9,22,33 Explicit advice to change drinking, reflective listening, and discussions of ambivalence toward change were observed infrequently. In addition, providers seldom asked open-ended questions about alcohol use, despite evidence that “closed” questions generally elicit less information from patients.34 Recent research showing that medical providers can increase use of open-ended questions and reflective listening after relatively brief educational interventions suggests that targeted education could improve these deficits.35
Patients who reported the heaviest alcohol consumption were more likely to engage in alcohol-related discussions with their providers than were those who reported lower consumption. This fact suggests that providers may focus their alcohol-related interventions on patients most likely to have alcohol use disorders. Future research will need to determine whether providers are missing preventive opportunities with patients with milder problem drinking who could benefit from brief interventions.5–8
Patients who consumed the most alcohol were also more likely to make statements reflecting motivation to change, and least likely to display resistance to change, compared with patients who drank less. An association between increased severity of drinking problems and increased readiness to change has been reported,36 but a relationship between the severity of drinking problems and patients' responses to alcohol interventions has not been described previously. Although this cross-sectional study cannot determine the cause of the observed association, several explanations are possible. First, patients with higher levels of alcohol consumption might be more motivated to change because they are more likely than those who drink at lower levels to have experienced adverse consequences of their drinking. Second, patients with more severe problem drinking might be more motivated to change because they are more likely to have been counseled about their drinking.25 Finally, the observed association between severity of problem drinking and motivation to change could reflect misclassification bias. Although research suggests that such misclassification by the AUDIT-C is minimal,20,27 some patients who resisted change because they were “in denial” about their drinking problems might have under-reported their alcohol consumption.
The rate of alcohol-related discussions observed in the Control firm in the present study (41.5%) was consistent with previous research. In 2 studies using patient exit interviews, 42% to 57% of at-risk drinking patients who received “usual care” reported alcohol-related discussions.16,17 In a study using simulated patient encounters, 36% to 77% of primary care providers asked about alcohol use when evaluating patients who drank over 1 drink daily and whose symptoms were not alcohol-related.37 Studies of patients with more severe problems due to drinking have reported higher rates of alcohol-related discussions (60% to 80%).38,39 Rates of alcohol counseling are lower in unselected primary care samples. When appointments have been directly observed or described by providers, family physicians counseled 2% to 10% of all patients about drinking, irrespective of whether the patients drank any alcohol.18,40 Three to fifteen percent of all VA patients report any alcohol counseling in the past year.41
In the Intervention firm of the study clinic, providers were prompted to address alcohol use when patients screened positive for at-risk drinking. Consistent with a previous study, the screening and prompting program was not associated with longer alcohol-related discussions.18 However, providers in the Intervention firm discussed alcohol use significantly more often than those in the Control firm (82% vs 40%). Given similar findings from a recent trial of a screening and prompting intervention,17 such provider prompts may be an important means of increasing primary care alcohol counseling. In a study showing no relationship between alcohol screening and rates of primary care alcohol discussions, screening did not assess adverse consequences of drinking or readiness to change.18
Several limitations of this study deserve emphasis. Despite our efforts to audiotape all visits during the study period, this 6-month study probably underestimates the proportion of study patients who received appropriate primary care alcohol-related interventions. Some visits were missed because patients could not be found before appointments. To increase the reliability of reported data, we analyzed only those utterances coded into the same MISC categories by both coders, potentially missing important alcohol-related utterances (e.g., advice). Since current recommendations are for annual alcohol screening and counseling, patients who did not receive alcohol counseling or advice during audiotaped visits could have discussed alcohol use with their providers during the months before or after the study.
A minority of at-risk drinking patients and providers agreed to participate in the study. Although we were unable to detect important differences between participants and nonparticipants, unmeasured differences between recruited and nonrecruited patients or providers may have existed. Providers who were more comfortable with their communication skills might have been more likely to agree to be audiotaped, potentially biasing our study toward increased alcohol-related discussions. This study also included older, male VA general medicine outpatients, seen in a clinic with 30-minute appointments. Alcohol counseling may be less likely in clinical settings with shorter appointments. Younger patient populations may receive more alcohol counseling.25
With regard to the association between firm assignment and rates of alcohol counseling, several limitations are important to note. Although 1 firm was randomly chosen to receive the intervention, providers and patients were not randomized to the 2 firms, and there were differences between the participating providers in the 2 firms. Therefore, although secondary analyses were unable to identify differences between the Intervention and Control firms with regard to 35 potential confounders, the observed associations between firm assignment and alcohol-related discussions could have resulted from unmeasured confounding. We lacked adequate sample size to use multivariate analyses, including analytic techniques that could have accounted for clustering of visits by patients and providers. While it is possible that providers in the Intervention firm increased counseling because they thought that the audiotape study was linked to ACQUIP, our analyses of blinding suggest otherwise.
Despite these limitations, this audiotape study of at-risk drinking patients' primary care appointments begins to address an important gap in our current understanding of primary care alcohol counseling. We found that primary care alcohol-related discussions were generally nonconfrontational and primarily included assessment and patient education. Explicit alcohol-related advice and reflective listening were notably missing from many encounters. Future research will need to address whether deficits observed at this single site exist elsewhere and if so, how to address them with improved educational programs. We also observed a strong association between provider prompts and rates of alcohol-related discussions. If this is confirmed in future studies, it will suggest that institutionalized alcohol screening and provider prompting offer an important, feasible method for increasing primary care alcohol counseling, potentially decreasing at-risk drinking and alcohol-related morbidity.
Acknowledgments
This research was supported by grants from the University of Washington Royalty Research Fund, and the Department of Veterans Affairs, Health Services Research and Development Service (SDR 96-002). Dr. Bradley is an investigator at the VA Puget Sound Health Care System, and is currently supported by National Institute of Alcohol Abuse and Alcoholism grant no. K23AA00313) and is a Robert Wood Johnson Foundation Generalist Physician Faculty Scholar. Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the University of Washington, the National Institute of Alcohol Abuse and Alcoholism, or the Robert Wood Johnson Foundation.
APPENDIX A
Examples of Utterances from Tapes Coded into Different Motivational Interviewing Skills Code (MISC) and Content Categories
| Provider utterances by Motivational Interviewing Skills Code | |
| Advice | • The most important thing is for you to remain sober |
| • But I thought it would be wise for you to cut down on your number of beers per day | |
| Affirmation or support | • And that's great you're able to stop |
| • I think this past year you've done a great job with staying off alcohol | |
| Facilitation | • Oh, I see |
| • I remember that now | |
| Question asking | • Have you ever had any DWIs or anything else like that? |
| • Do you drink at all? | |
| Information giving or education | • And a beer or two a day is probably okay …. |
| • It will cause your blood pressure to go up … and can cause problems for your liver | |
| Reflection–historic | • I think you were drinking four or five drinks a day |
| • And I know that you have done some drinking in the past | |
| Reflection | • And you were saying to me, Gee Doc, when you get to be my age, my beers are pretty enjoyable …. |
| • Yeah, that part of the day when you can sit down and relax …. | |
| Patient utterances by Motivational Interviewing Skills Code | |
| Counter-motivational statements | • And I—I enjoy it |
| • Well, just—it's not problematic for me | |
| Neutral statements | • I'm having a couple a day |
| • And then if I'm with somebody I may drink a little more | |
| Self-motivational statements | • I might do outpatient …. |
| • Well, I know I do drink more than I should | |
| Patient or provider utterances by Content Code | |
| Consumption | • Two or three beers a night or something like that (Patient) |
| • Are you drinking anything right now? (Provider) | |
| Problems due to drinking | • I think it's a combination of a little bit withdrawal (Patient) |
| • There is the issue of how it interacts with your diabetes (Provider) | |
| Change | • Talked with some people over at the Alcohol Treatment Center (Patient) |
| • Do you have some support out there? (Provider) | |
| Not explicitly related to alcohol | • Pretty much still in a lot of pain (Patient) |
| • Let me give you a slip here to check out (Provider) | |
REFERENCES
- 1.Grant BF, Harford TC, Dawson DA, Chou P, Dufour M, Pickering R. Prevalence of DSM-IV alcohol abuse and dependence, United States, 1992. Alcohol Health Res World. 1994;18:243–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Broadening the Base of Treatment for Alcohol Problems: A Report of the Committee for the Study of Treatment and Rehabilitation for Alcoholism. Washington DC: National Academy Press; 1990. [Google Scholar]
- 3.Secretary of Health and Human Services. Ninth Special Report to the US Congress on Alcohol and Health. Arlington, Va: Department of Health and Human Services; 1997. [Google Scholar]
- 4.Hasin D, Grant B, Dufour M, Endicott J. Alcohol problems increase while physician attention declines. Arch Intern Med. 1990;150:397–400. [PubMed] [Google Scholar]
- 5.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 6.Ockene JK, Adams A, Hurley TG, Wheeler EV, Hebert JR. Brief physician- and nurse practitioner–delivered counseling for high-risk drinkers. Arch Intern Med. 1999;159:2198–205. doi: 10.1001/archinte.159.18.2198. [DOI] [PubMed] [Google Scholar]
- 7.Wallace P, Cutler S, Haines A. Randomized controlled trial of general practitioner intervention in patients with excessive alcohol consumption. BMJ. 1988;297:663–8. doi: 10.1136/bmj.297.6649.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO Brief Intervention Study Group. A cross-national trial of brief interventions with heavy drinkers. Am J Public Health. 1996;86:948–55. doi: 10.2105/ajph.86.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bien TH, Miller WR, Tonigan S. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–36. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 10.Richmond R, Heather N, Wodak A, Kehoe L, Webster I. Controlled evaluation of a general practice–based brief intervention for excessive drinking. Addiction. 1995;90:119–32. doi: 10.1046/j.1360-0443.1995.90111915.x. [DOI] [PubMed] [Google Scholar]
- 11.Kahan M, Wilson L, Becker L. Effectiveness of physician-based interventions with problem drinkers. Can Med J Assoc. 1995;152:851–9. [PMC free article] [PubMed] [Google Scholar]
- 12.Poikolainen K. Effectiveness of brief interventions to reduce alcohol intake in primary health care populations: a meta-analysis. Prev Med. 1999;28:503–9. doi: 10.1006/pmed.1999.0467. [DOI] [PubMed] [Google Scholar]
- 13.Wilk AI, Jensen NM, Havighurst TC. Meta-analysis of randomized control trials addressing brief interventions in heavy alcohol drinkers. J Gen Intern Med. 1997;12:274–83. doi: 10.1046/j.1525-1497.1997.012005274.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute on Alcohol Abuse and Alcoholism. The physician's guide to helping patients with alcohol problems. Bethesda Md: U.S. Department of Health and Human Services, Public Health Service; National Institutes of Health (NIH publication #95-3769); 1995. pp. 1–12. [Google Scholar]
- 15.US Preventive Services Task Force. Guide to Clinical Preventive Services: Report of the US Preventive Services Task Force. 2nd ed. Baltimore: Williams and Wilkins; 1996. [Google Scholar]
- 16.Adams A, Okene JK, Wheele EV, Hurley TG. Alcohol counseling—physicians will do it. J Gen Intern Med. 1998;13:692–8. doi: 10.1046/j.1525-1497.1998.00206.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saitz R, Horton NJ, Sullivan LM, Moskowitz MA, Samet JH. Providing physicians with patient-specific information increases the likelihood of alcohol counseling and decreases patient drinking. J Gen Intern Med. 2001;16(suppl):216. [Google Scholar]
- 18.Vinson DC, Elder N, Werner JJ, Vorel LA, Nutting PA. Alcohol-related discussions in primary care—a report from ASPN. J Fam Pract. 2000;49:28–33. [PubMed] [Google Scholar]
- 19.Fihn SD, McDonnel MB, Diehr P, Au DH. Routine reporting of health status data does not improve general health or satisfaction. J Gen Intern Med. 2001;16(suppl):132. [Google Scholar]
- 20.Bradley KA, Kivlahan DR, Bush KR, McDonell MB, Fihn SD. Variations on the CAGE alcohol screening questionnaire: strengths and limitations in VA general medical patients. Alcohol Clin Exper Res. 2001;25:1472–8. doi: 10.1097/00000374-200110000-00010. [DOI] [PubMed] [Google Scholar]
- 21.Miller WR. Motivational Interviewing Skills Code Manual (MISC) Albuquerque, NM: University of New Mexico; 1998. [Google Scholar]
- 22.Miller WR, Benefield G, Tonigan JS. Enhancing motivation for change in problem drinking: a controlled comparison of two therapist styles. J Consult Clin Psychol. 1993;61:455–61. doi: 10.1037//0022-006x.61.3.455. [DOI] [PubMed] [Google Scholar]
- 23.Miller WR, Rollnick S, Moyers TB. Motivational Interviewing Professional Training Videotape Series. 1998.
- 24.Good P. Permutation Tests. New York: Springer Verlag; 1994. [Google Scholar]
- 25.Volk RJ, Steinbauer JR, Cantor SB. Patient factors influencing variation in the use of preventive interventions for alcohol abuse by primary care physicians. J Stud Alcohol. 1996;57:203–9. doi: 10.15288/jsa.1996.57.203. [DOI] [PubMed] [Google Scholar]
- 26.Bradley KA, Bush K, McDonell MB, Malone T, Fihn SD. Screening for problem drinking: comparison of CAGE and AUDIT. J Gen Intern Med. 1998;13:379–88. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PubMed] [Google Scholar]
- 27.Bradley KA, Maynard C, Kivlahan DR, McDonell MB, Fihn SD. The relationship between alcohol screening questionnaires and mortality among male VA outpatients. J Stud Alcohol. 2001;62:826–33. doi: 10.15288/jsa.2001.62.826. [DOI] [PubMed] [Google Scholar]
- 28.Buchsbaum DG, Buchanan RG, Poses RM, Schnoll SH, Lawton MJ. Physician detection of drinking problems in patients attending a general medicine practice. J Gen Intern Med. 1992;7:517–21. doi: 10.1007/BF02599456. [DOI] [PubMed] [Google Scholar]
- 29.Buchsbaum DG, Buchanan RG, Lawton MJ, Elswick RK, Jr, Schnoll SH. A program of screening and prompting improves short-term physician counseling of dependent and nondependent harmful drinkers. Arch Intern Med. 1993;153:1573–7. [PubMed] [Google Scholar]
- 30.Clark WD. Alcohol: an ounce of prevention? J Gen Intern Med. 1995;10:113–4. doi: 10.1007/BF02600241. [DOI] [PubMed] [Google Scholar]
- 31.Samet JH, Rollnick S, Barnes H. Beyond CAGE: a brief clinical approach after detection of substance abuse. Arch Intern Med. 1996;156:2287–93. doi: 10.1001/archinte.156.20.2287. [DOI] [PubMed] [Google Scholar]
- 32.Williams GC, Quill TE, Deci EL, Ryan RM. “The facts concerning the recent carnival of smoking in Connecticut” and elsewhere. Ann Intern Med. 1991;115:59–63. doi: 10.7326/0003-4819-115-1-59. [DOI] [PubMed] [Google Scholar]
- 33.Walsh DC, Hingson RW, Merrigan DM, et al. The impact of a physician's warning on recovery after alcoholism treatment. JAMA. 1992;267:663–7. [PubMed] [Google Scholar]
- 34.Roter DL, Hall JA. Physicians' interviewing styles and medical information obtained from patients. J Gen Intern Med. 1987;2:325–9. doi: 10.1007/BF02596168. [DOI] [PubMed] [Google Scholar]
- 35.Handmaker NS, Hester RK, Delaney HD. Videotaped training in alcohol counseling for obstetric care practitioners: a randomized controlled trial. Obstet Gynecol. 1999;93:213–8. doi: 10.1016/s0029-7844(98)00377-9. [DOI] [PubMed] [Google Scholar]
- 36.Maisto SA, Conigliaro J, McNeil M, Kraemer K, O'Connor M, Kelley ME. Factor structure of the SOCRATES in a sample of primary care patients. Addict Behav. 1999;24:879–92. doi: 10.1016/s0306-4603(99)00047-7. [DOI] [PubMed] [Google Scholar]
- 37.Wenrich MD, Paauw DS, Carline JD, Curtis JR, Ramsey PG. Do primary care physicians screen patients about alcohol intake using the CAGE questions? J Gen Intern Med. 1995;10:631–4. doi: 10.1007/BF02602748. [DOI] [PubMed] [Google Scholar]
- 38.Conigliaro J, Lofgren RP, Hanusa BH. Screening for problem drinking-impact on physician behavior and patient drinking habits. J Gen Intern Med. 1998;13:251–6. doi: 10.1046/j.1525-1497.1998.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schorling JB, Klas PT, Willems JP, Everett AS. Addressing alcohol use among primary care patients: differences between family medicine and internal medicine residents. J Gen Intern Med. 1994;9:248–54. doi: 10.1007/BF02599649. [DOI] [PubMed] [Google Scholar]
- 40.Stange KC, Zyznaski SJ, Smith TF, et al. How valid are medical records and patient questionnaires for physician profiling and health services research? Med Care. 1998;36:851–67. doi: 10.1097/00005650-199806000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Rabiner DJ, Branch LG, Sullivan RJ. The receipt of prevention services by veterans using VA versus non-VA facilities. Prev Med. 1998;27:690–6. doi: 10.1006/pmed.1998.0345. [DOI] [PubMed] [Google Scholar]