Abstract
OBJECTIVE
We developed an instructional program to teach aspiration and injection techniques of the knee and shoulder to medical students and residents.
METHODS
Residents and fourth-year medical students participating in a rheumatology elective were assigned by deterministic allocation into 3 groups: the Traditional group received no specific instruction in arthrocentesis but simply rotated through rheumatology, learning injection techniques only if they saw patients who required them; the Lecture-only group received only the didactic lecture and did not have the opportunity to practice on the models; the Program group participated in the newly developed program of instruction that combined a didactic lecture and a hands-on workshop using the anatomic models to practice arthrocentesis techniques.
RESULTS
The scores on the written examination for those in the Program group (mean score 37.46 out of 40 possible) and the Lecture-only group (mean 37.75) were significantly higher than those of the Traditional group (mean 33.15) (P < .05). The scores on the practical examination for those in the Program group (mean score 24.08 out of 26 possible) were significantly higher than those of the Lecture-only (mean 20.50) and Traditional (mean 17.33) (P < .05)
CONCLUSION
The addition of this type of instruction to supplement a traditional internal medicine rotation can enhance a learner's ability to perform joint/soft-tissue injection and aspiration.
Keywords: arthrocentesis, medical education
Joint/soft-tissue injection and aspiration (JSIA) are procedures frequently performed by both specialists and primary care providers. Seventy-two percent of general internists and 87% of family physicians use these procedures in their practice.1,2 Instruction in injection techniques should be a part of residency training. When queried however, only 36% of internal medicine residency program directors reported that all of their residents master JSIA compared to 87% for blood gas analysis and 83% for ECG interpretation.3 Traditionally, JSIA is taught without the benefit of an organized approach. Experience in JSIA depends on whether a patient is seen who requires JSIA, and whether the staff physician feels comfortable supervising a learner. It is possible under such a system for a learner to complete his/her training without adequate instruction or experience in JSIA. Elnicki et al. have noted that, unfortunately, only a minority of office-level procedures are taught by faculty in medical training settings.4
How then should teaching JSIA be approached? Instruction in core procedural skills is an essential component of almost all residencies. Since the didactic lecture format is not well suited for the acquisition of complex manual operations, these skills have been primarily taught through demonstration, followed by supervised performance on patients. However, concerns regarding the safety of patients and the lack of readily available faculty and patient populations limit the utility of such an approach. For this reason, there is a need for an instructional alternative that allows the learner an opportunity to practice procedural skills within an instructionally relevant format without risk to the patient. In fields other than medicine, simulations are widely used when safety considerations place limits on the training environment (i.e., aviation). Simulations, animal workshops, and cadavers have been used successfully to teach and practice invasive medical procedures.5,6,7 Manikins or models using synthetic material also have been used successfully and are considered more convenient.8
We developed an instructional program to teach aspiration and injection techniques of the knee and shoulder (glenohumeral joint, biceps tendon sheath, subacromial bursa, and acromioclavicular joint) to medical students and residents. This program combines both a didactic lecture and a practical, hands-on workshop using anatomically correct models made of synthetic materials. We hypothesized that such a program would be more effective in developing skills to perform arthrocentesis than the traditional “see one, do one, teach one” approach. The objective of the research was to compare the outcomes from 3 instructional methods for teaching joint/soft-tissue injection and aspiration. Of particular interest is how the educational interventions differentially impacted performance and knowledge across the 3 groups. The central null hypothesis was that the impact of the educational programs would be the same.
METHODS
Educational objectives, curriculum design and testing criteria were developed by expert consensus by answering the question “What would a primary care physician need to know to be able to aspirate or inject the knee and shoulder successfully?” The knee and shoulder were selected for several reasons: 1) JSIA is frequently performed on knees and shoulders in primary care, 2) anatomic models of the knee and shoulder were available, and 3) limiting the educational program to 2 anatomic areas kept the material to be taught and tested at a manageable level. An expert panel of physicians consisting of general internists, family physicians, rheumatologists, and orthopedists at the University of Iowa reviewed the objectives, curriculum, and tests. After a consensus was reached (educational objectives are listed in Table 1), anatomic models of the knee and shoulder were purchased for the program from Limbs and Things Limited (Bristol, England). The models are unique in that they have a synthetic “skin” that allows palpation of underlying anatomic landmarks and repeated needle sticks. In addition, they are constructed with simulated subcutaneous tissue, bone, and joint capsule. The joint capsule of the knee holds fluid that can be aspirated, and the shoulder has electrodes that illuminate a panel when the appropriate anatomic structures have been entered with a needle.
Table 1.
Educational Objectives
| • Know at least 3 diagnoses for which joint aspiration would be very important in establishing the diagnosis. |
| • Know at least 3 therapeutic indications for doing joint aspiration. |
| • Know 4 (relative) contraindications to doing arthrocentesis. |
| • Know 4 (relative) contraindications to injecting corticosteroids into a joint or soft-tissue area. |
| • Be able to give a rough estimate of the efficacy for soft-tissue and intra-articular corticosteroid injections. |
| • Know at least 5 adverse effects of injecting corticosteroids into a joint or soft-tissue. |
| • Know the approximate risk for joint infection after arthrocentesis. |
| • Know the anatomic landmarks and structures of the knee and shoulder. |
| • Know the frequency with which joints and soft-tissue can be injected with corticosteroids. |
| • Know which tests to routinely perform on synovial fluid. |
| • Know the features and characteristics of normal, noninflammatory, inflammatory, septic and hemorrhagic synovial fluid. |
| • Know the clinical importance of water solubility of the corticosteroid preparation. |
| • Know at least 3 reasons to use local anesthetics when injecting corticosteroids. |
| • Be able to aspirate/inject these areas: |
| ✓ Medial approach to the knee |
| ✓ Lateral approach to the knee |
| ✓ Posterior approach to the shoulder joint |
| ✓ Anterior approach to the shoulder joint |
| ✓ Lateral approach to the subacromial bursa |
| ✓ Anterior approach to the biceps tendon sheath |
| ✓ Acromioclavicular joint |
Evaluation Plan
All available residents (first-, second-, and third-year internal medicine residents, first-year orthopedic residents, and first-year family practice residents) and fourth-year medical students participating in a rheumatology elective during the 1997–1998 academic year were deterministically allocated to 3 instructional units on the basis of educational scheduling considerations. The study authors could identify no probable mechanism by which scheduling influences systematically impacted student characteristics. Members of each group received both a written test and a practical test at the end of their 1-month, university-based rheumatology rotation. The written test (see Appendix A at www.blackwellscience.com/jgi) consisted of questions about knee and shoulder anatomy, risks and benefits of arthrocentesis (and steroid injection), as well as corticosteroid selection. During the practical test (see Appendix B at www.blackwellscience.com/jgi), a blinded observer (TMK) assessed learner skills in identifying knee and shoulder anatomic landmarks and performing arthrocentesis at the 7 anatomic locations on the manikin (medial approach to knee, lateral approach to knee, anterior approach to glenohumeral joint, posterior approach to glenohumeral joint, biceps tendon, acromioclavicular joint, and lateral approach to the subacromial bursa).
Forty-four participants were enrolled. The “testable material” in the program was thought to be insufficient for both a pre-test and a post-test. Therefore, an approximation of baseline knowledge was assessed by selecting a random sample of 10 participants (pre-test group) who were tested (written and practical test) before receiving any instruction. They were not tested again. Thirteen participants (Traditional group) received no specific instruction in arthrocentesis but simply rotated through rheumatology, learning injection techniques only if they saw patients who required them. Eight participants (Lecture-only group) received only the didactic lecture and did not have the opportunity to practice on the models. Thirteen participants (Program group) received the newly developed program of instruction that consisted of a didactic lecture and a hands-on workshop using the anatomic models to practice arthrocentesis techniques. Those in the Program group interacted with the models twice (workshop and practical exam). All others interacted with the models only once during the practical exam. All participants in each of the 4 groups assessed their confidence levels in performing the individual aspiration/injection procedures at the end of the rotation (see Appendix C at www.blackwellscience.com/jgi).
Analysis of variance (ANOVA) and Student-Newman-Keuls follow-up tests controlling type I error rates SAS software (SAS Institute Inc., Cary, NC) and Proprietary Software Version 7 (TS P1) were used to analyze test performance and confidence measures from the 4 groups.
Educational Intervention
The JSIA lecture was 60 minutes long and specifically followed the objectives of the workshop, including indications, contraindications, risks, and benefits of JSIA. Anatomy of the shoulder and knee were reviewed, and different corticosteroid preparations were examined with a rationale developed for selection. The anatomy review was interactive and was directed toward the anatomic landmarks learners would need to identify as a part of the hands-on workshop. The hands-on practical session with the models took place usually 2 days later (lectures were Tuesday and Thursday mornings before clinic) and took approximately 1 hour. These 2 sessions were part of the usual 13 curricular lectures presented during the rotation. Learners who did not participate in the JSIA lecture or workshop were given 2 other lectures on rheumatologic topics. A typical 1-month rotation included 1 to 4 residents and 1 to 4 fourth-year medical students. At the beginning of the rotation, learners were given an orientation, a set of educational objectives, required reading list, a bibliography of key articles, and a self-assessment test to be completed before the end of the rotation. Learners typically spent 1 week with the rheumatology consult service seeing approximately 3 to 6 new patients per day (including inpatients). Three weeks were spent in the outpatient clinic that included 9 half-day clinics per week (1 new patient and 3 to 4 follow-up patients per clinic). The attendings on the consult service and in the outpatient clinic were unaware of group assignment within the study. Numbers of aspirations and injections actually performed on patients by the learners were not systematically recorded. At the end of the rotation, all learners completed an anonymous exit questionnaire evaluating the entire rotation.
RESULTS
Performance on both the practical and written test for each of the 4 groups is presented in Table 2. Results from the ANOVA shown at the bottom of the table display highly significant F statistics for both the written and practical examinations. Student-Newman-Keuls follow-up tests controlling type I error rates revealed significant differences between groups for both the written and practical examination (written examination: F = 13.48, P < .0001; practical examination: F = 9.23, P < .0001). Specifically on the written examination, the Program and Lecture-only groups outperformed the pre-test and Traditional groups (P < .05). On the practical examination, the Program group was superior to the pre-test, Traditional, and Lecture-only groups (P < .05). Importantly, the difference displayed in the Traditional and Program groups on the practical examination displayed a large and practically significant effect size of almost 2.2. In addition, the Traditional and Lecture-only groups outperformed the pre-test group (P < .05).
Table 2.
Comparison of Mean Scores on the Written Examination (40 Total Possible Points) and Practical Examination (26 Total Possible Points) by Educational Intervention
| Pre-test* | Traditional† | Lecture-only‡ | Program§ | |
|---|---|---|---|---|
| N | 10 | 13 | 8 | 13 |
| Written | 32.50 | 33.15 | 37.75 | 37.46 |
| SD | 2.01 | 3.63 | 1.16 | 1.80 |
| Range | 29 to 35 | 26 to 37 | 30 to 39 | 35 to 40 |
| Practical | 16.3 | 17.33 | 20.50 | 24.08 |
| SD | 5.14 | 4.94 | 2.62 | 1.31 |
| Range | 6 to 23 | 11 to 25 | 11 to 24 | 24 to 25 |
Group was tested before any instruction.
Group received no specific instruction in joint injection/aspiration.
Group received only the didactic lecture.
Group was given the didactic lecture and participated in the hands-on workshop.
Fwritten = (13.48, P < .0001; Lect-only and Program > Traditional and pre-test, P < .05; Fpractical = 9.23, P < .0001; Program > Traditional and Lecture-only; Traditional and Lecture-only > pre-test. P < .05.
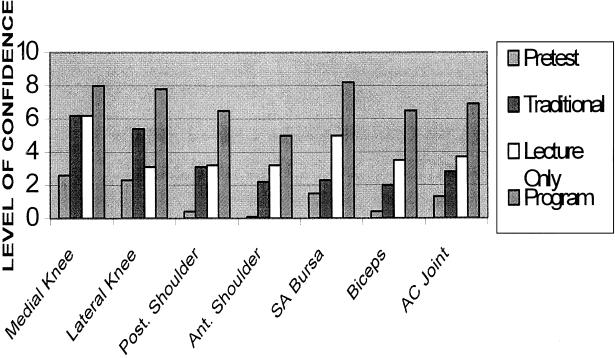
Those who participated in the lecture and workshop felt more confident in their ability to perform these procedures. Figure 1 displays the mean reported confidence for performing each of the 7 aspiration/injection techniques. The scale ranged from 0 to 10, with 0 representing no confidence in performing the procedure and 10 signifying a high level of confidence. In addition, confidence levels appeared to be predictive of the level of skill demonstrated in performing the procedures. There was a strong positive correlation between performance (as measured on the practical examination) and the learner's overall level of confidence in performing the procedures (r = .68; P < .0001).
FIGURE 1.
Self-reported confidence levels in performing injections.
Those in the Program group rated the usefulness of the lecture and practicing on the manikins on a 0- to10- point scale with 0 equal to “not helpful at all” and 10 equal to “very helpful.” The mean scores for the usefulness of the lecture (Program and Lecture-only groups) and the manikins (Program group) were 8.1 (SD, 1.86; range, 5 to 10) and 8.6 (SD, 1.38; range 6 to 10), respectively.
DISCUSSION
After participating in this educational program, residents and students performed better on both a practical test and a written test that assessed risks, benefits, indications, contraindications, anatomy, and choice of medications for joint/soft tissue aspiration and injections. In addition, their confidence to perform these procedures substantially improved. Better performance on the written test correlated with participating in the lecture, and better performance on the practical test correlated with participating in the hands-on workshop. We believe both the didactic lecture and the hands-on practice are important and need to be included in any comprehensive approach to teaching JSIA. It is tempting to say that the students and residents who were taught in the traditional fashion were not significantly better than the students and residents who were pre-tested; however, our study was not designed to assess any difference between these two groups. Students' and residents' confidence in performing JSIA correlated with their performance on the practical test.
There was no statistically significant difference between groups in training levels (i.e., medical students versus residents). There was, however, a negative but not significant correlation between level of training and the performance on the written and practical tests (r = −.07 and −.09; P = .58 and .60, respectively). The absence of a positive trend may have been due to the fact that medical students were closer to anatomy review than the residents, who likely had not reviewed musculoskeletal anatomy since medical school.
There are several limitations to our study. We measured performance on the manikin, which may not strictly generalize to performance on a live patient. Performance on live patients was not assessed. However, we believe practicing on the manikin represents a close approximation to practicing on a real patient, represents a good test of instructional effectiveness, and allows a learner to practice an invasive procedure without risk to a live patient. Our study numbers are small and although there appeared to be no difference between groups in training levels, larger numbers of participants would be required to support this statistically. Pretesting all participants would have been preferable, since it would likely have provided a more convincing measure of baseline knowledge. Nevertheless, the Traditional group (with no lecture or hands-on practice) did not do significantly better than the pre-test group, suggesting an accurate reflection of baseline knowledge.
CONCLUSION
Residents who participated in this program developed important baseline knowledge necessary to perform JSIA safely and effectively. They had better skills than their counterparts who learned “on the job,” and their confidence to perform the procedure was better. The hands-on experience seemed to be particularly useful, but the lecture was also necessary for acquiring the appropriate knowledge base. It is important to teach JSIA in an organized manner that allows learners to practice invasive techniques without risk to a patient. The addition of this type of instruction to supplement a traditional internal medicine rotation can enhance a learner's ability to perform JSIA successfully.
Acknowledgments
This research was supported by a grant from the Office of Consultation and Research in Medical Education, University of Iowa.
REFERENCES
- 1.Wigton RS, Niolas JA, Blank LL. Procedural skills of the general internist: A survey of 2500 physicians. Ann Intern Med. 1989;111:1023–34. doi: 10.7326/0003-4819-111-12-1023. [DOI] [PubMed] [Google Scholar]
- 2.Norris TE, Felmar E, Tolleson G. Which procedures should be currently taught in family practice residency programs. Fam Med. 1997;29:99–104. [PubMed] [Google Scholar]
- 3.Wigton RS, Blank LL, Nicolas JA, Tape TG. Procedural skills training in internal medicine residencies: a survey of program directors. Ann Intern Med. 1989;111:932–8. doi: 10.7326/0003-4819-111-11-932. [DOI] [PubMed] [Google Scholar]
- 4.Elnicki DM, Shumway JM, Halbritter KA, Morris DK. Interpretive and procedural skills of the internal medicine clerkship: performance and supervision. South Med J. 1996;89:603–8. doi: 10.1097/00007611-199606000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Olshaker JS, Brown CK, Arthur DC, Tek D. Animal procedure laboratory surveys: use of the animal laboratory to improve physician confidence and ability. J Emerg Med. 1989;7:593–7. doi: 10.1016/0736-4679(89)90003-6. [DOI] [PubMed] [Google Scholar]
- 6.Gillies D, Haritsis A, Williams C. Computer simulation for teaching endoscopic procedures. Endoscopy. 1992;(suppl 2):544–8. doi: 10.1055/s-2007-1010541. [DOI] [PubMed] [Google Scholar]
- 7.Brattebo G, Seim SH. Teaching and training of invasive procedures on cadavers. Lancet. 1988;2:1078–9. doi: 10.1016/s0140-6736(88)90098-0. [DOI] [PubMed] [Google Scholar]
- 8.Pilgrim C, Lannon C, Harris RP, Cogburn W, Fletcher SW. Improving clinical breast examination training in a medical school: a randomized controlled trial. J Gen Intern Med. 1993;8:685–8. doi: 10.1007/BF02598289. [DOI] [PubMed] [Google Scholar]