Abstract
BACKGROUND
Although mailed reminders have been used for prevention among general populations, few studies have evaluated their effectiveness among chronically ill populations.
OBJECTIVE
We evaluated the effectiveness of mailed reminders for improving diabetes management. The reminder included a letter from the individual's primary care physician (PCP), a self-care handbook, a preventive care checklist, and specific recommendations regarding receipt of routine monitoring and screening.
METHODS
Of 195 PCPs practicing with a large group practice, 111 agreed to have their adult patients with diabetes randomized to receive the reminder (n = 1,641) or usual care (n = 1,668). Using data from automated databases, we fit generalized estimating equations to evaluate the effect of reminder receipt on fasting lipid profile and glycated hemoglobin testing, dilated retinal exam receipt, and visit frequency during the 6 and 12 months following randomization, and glycated hemoglobin and cholesterol levels in the year following randomization.
RESULTS
Reminder and usual care recipients did not differ in sociodemographic, clinical, or prior testing characteristics. In the 6 months following randomization, reminder recipients were more likely to receive a retinal exam (odds ratio [OR], 1.29; 95% confidence interval [95% CI], 1.12 to 1.49) and diabetes visit (OR, 1.28; 95% CI, 1.12 to 1.47). In the 12 months following randomization, reminder recipients were more likely to receive a glycated hemoglobin test (OR, 1.21; 95% CI, 1.03 to 1.43), retinal exam (OR, 1.23; 95% CI, 1.07 to 1.41), and diabetes visit (OR, 1.25; 95% CI, 1.09 to 1.29). In the follow-up year, reminder recipients also tended to have a glycated hemoglobin test that did not reflect poor control (<9.5%).
CONCLUSIONS
We found small but significant improvements in the management of patients with diabetes receiving a computerized mailed reminder.
Keywords: diabetes, patient mailed reminders, prevention, health care use, chronic disease management
The American Diabetes Association (ADA) recommends routine monitoring and screening for the prevention of complications related to diabetes.1 Although the specific recommended frequency of testing and physician visits depends on the type of diabetes, blood glucose goals, changes in treatment, and presence of complications, it is recommended that all adults with diabetes minimally be screened for lipid and retinal disorders annually, and glycated hemoglobin control biannually. It is also recommended that all patients visit their physician at least biannually for routine diabetes care. Despite wide dissemination of these recommendations, studies nationwide illustrate that adherence to the recommended diabetes standards of care is less than optimal.2–11
Ensuring the receipt of recommended preventive care—be it primary, secondary, or tertiary prevention—is one of the many public health challenges of the 21st Century.12 As reflected in models of health behavior, providing patients with cues to action may promote appropriate use of health services, including preventive care.13 Some have proposed the use of mailed reminders to encourage receipt of preventive care services among the general population. Such reminders have been found to improve immunization rates among adults14–17 and mammography use among women.18–22 Yet, some studies have found mailed reminders to have no effect on immunization rates,23 or Pap smear24 or mammography25 use. Although the specific factors that influence the effectiveness of mailed reminders remain speculative, some have found that (1) recommendations tailored to individuals' screening and risk status are more effective than standard messages,16,18,19 (2) personalized letters from a patient's physician are more effective than generic mailings not from a patient's physician,16 and (3) the inclusion of educational brochures is more effective than standard mailed reminders.26
Despite relatively wide use of mailed reminders for primary and secondary prevention among the general population, we know of few published studies evaluating the effectiveness of mailed reminders in the management of chronic medical conditions. As computer technology becomes more available within health care settings, many primary care practices will be able to use such technology to track the receipt of routine services and facilitate the implementation of automated reminder systems for both well and chronically ill patients. In fact, when mailed reminders have been used among Medicaid patients with hypertension27 and diabetes28 to improve compliance with antihypertensive therapy and sulfonylurea therapy, respectively, they have been found effective.
We sought to evaluate the extent to which a mailed reminder packet improved the routine care delivered to adult patients with diabetes. The mailed reminder packet, which was developed and implemented using existing computerized technology available within an integrated delivery system, included a letter with tailored recommendations from the patient's primary care physician (PCP), a diabetes self-care handbook, and a preventive care checklist. Therefore, in addition to reminding patients with diabetes to receive recommended routine monitoring and screening tests, it also included educational material that could improve a patient's ability to engage in self-management. This paper presents results from a randomized trial evaluating the effectiveness of a mailed reminder packet in improving the rate of routine monitoring and screening among patients with diabetes as well as its impact on glycated hemoglobin (HbA1c) and low-density lipoprotein (LDL) levels.
METHODS
Study Population and Setting
The study population was drawn from patients aged 18 and over with diabetes who were aligned to one of 195 adult PCPs practicing within a 900-member multi-specialty, salaried group practice. Although this medical group provides care on both a fee-for-service and a capitated basis, to ensure as complete information as possible for both the mailed reminder program and the evaluation, we limited study eligibility to that half of their patient population enrolled in an affiliated health maintenance organization (HMO).
We attempted to implement each step of the research protocol in a manner that easily could be duplicated in a nonresearch environment. We used patient registry information available within a web-based Diabetes Care Management Support System29 to identify the HMO patients with diabetes aligned to one of the 195 adult PCPs practicing with the medical group. The patient registries within this system rely on automated visit and prescription claims data to identify patients with diabetes. Patients are included in the registry if they have had (1) at least two encounters with members of the group practice for their diabetes care or (2) at least one pharmacy claim for a diabetes-specific drug during the previous 24-month period. Inpatient and outpatient encounters are classified as being for diabetes care if an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code of 250.xx was associated with the encounter, regardless of whether the code reflected the primary diagnosis. Therapeutic codes used by First DataBank, a leading source of electronic drug information, are used to identify patients with a pharmacy claim for either insulin or oral hypoglycemics.
Because a 1-time mailing to all patients with diabetes treated by any given physician or medical group has the potential to overwhelm the delivery system, we elected to stagger mailings to intervention group members. Discussions regarding how best to stagger these mailings led to the decision to use a birthday greeting. However, in keeping with our desire to implement the research protocol in a manner that could be duplicated operationally, instead of identifying eligible patients weekly or monthly, we identified patients quarterly. In November of 1998, we identified patients in the registry with a January, February, or March birthday aligned to one of the 195 adult PCPs, and in February of 1999, we identified those patients with an April, May, or June birthday.
In November of 1998, a total of 4,021 HMO patients who were aligned to the 195 PCPs were identified. Lists of eligible patients, with a letter describing the mailed reminder program (including sample letters) and its evaluation were mailed to each PCP. Primary care physicians were asked their willingness to participate in the program, thereby enabling research staff to use their names in the mailed reminder letter. One hundred eleven physicians (57%) agreed to participate. These physicians were asked to identify who among their aligned patients was ineligible for inclusion due to an incorrect diagnosis, death, or other reason. Among the 2,252 potentially eligible patients aligned to them, these physicians identified 315 patients as ineligible. In February of 1999, the research team identified another 2,278 eligible patients who were aligned to the 111 physicians who originally agreed to participate. Upon mailing these physicians a list of their eligible patients (n = 1,807), 77 physicians (69%) responded and identified 416 patients as ineligible. To further ensure that no letters were sent to patients inappropriately, research team members confirmed the presence of a diagnosis of diabetes within an available electronic medical record for each patient a physician identified as eligible. Over the 6-month period, this medical record review process resulted in another 19 patients being identified as ineligible.
The final sample consisted of 3,309 patients aligned to 111 adult primary care physicians. Using the random number generator in SAS (Version 8.2; SAS Institute, Inc., Cary, NC), each month, each eligible patient with a birthday in the month was assigned to receive either the mailed reminder packet or usual care. The result was 1,641 patients randomized to receive the intervention and 1,668 patients randomized to receive usual care. The study protocol was reviewed and approved by our Institutional Review Board.
The Mailed Intervention
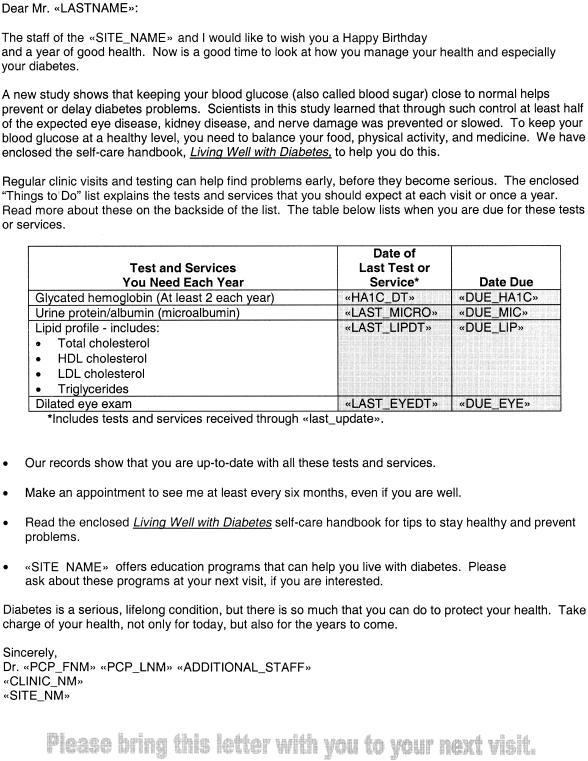
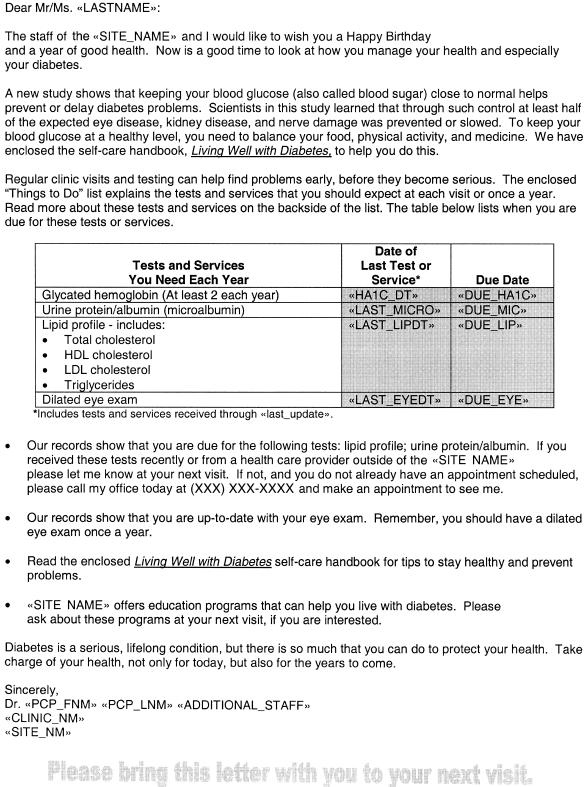
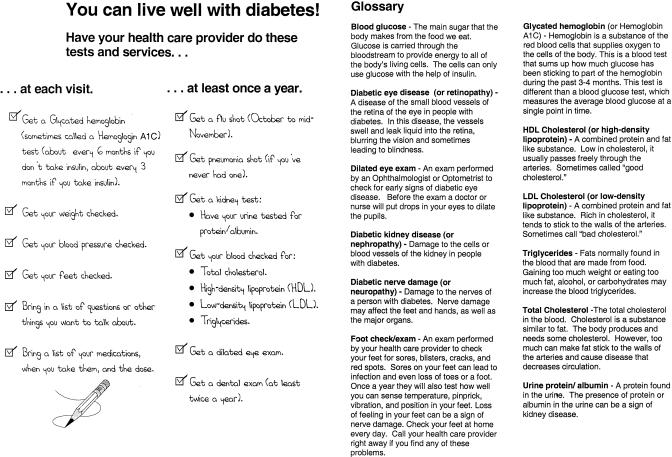
The mailed reminder packet included 3 things: a letter from the individual's PCP that included tailored recommendations for actions to be taken by the patient, a self-care handbook; and a preventive care checklist. The letter began by wishing the individual a happy birthday from their PCP and clinic staff. It then went on to emphasize the importance of routine screening and monitoring among patients with diabetes, and to encourage the patient to take responsibility for their own health. The remainder of the letter listed specific tests or exams, when they were last done, and when they were next due or if they were overdue. The letter concluded with specific action steps for the patient to take given his/her situation, including the need for regular appointments. Figure 1 presents an example of a letter that was mailed to a patient who was up to date on his/her routine screening, while Figure 2 illustrates the type of letter that was sent to patients who were overdue for a screen. A self-care handbook30 was included to reinforce the message and provide more detailed information on self-management. Among other things, this handbook discusses the importance of controlling glycated hemoglobin. Also enclosed was a 1-page checklist that summarized, on one side, the recommended routine monitoring and screening schedule for patients with diabetes, and, on the other side, provided easy-to-read explanations of these tests and services (Fig. 3). The reading level of the packet's contents ranged from fifth through eighth grade.
FIGURE 1.
Patient up-to-date letter.
FIGURE 2.
Patient due letter.
FIGURE 3.
Checklist for tests and services.
The intervention mailings were sent between December 1, 1998 and June 15, 1999. To enable the production and mailing of the reminders to occur in batches, the intervention was mailed twice a month, on the 1st and 15th, with arrival anticipated 2 to 4 weeks ahead of patients' birthdays.
Data Sources and Analytic Measures
Study data were compiled from automated clinical and administrative databases. Administrative records were used to compile demographic information (i.e., age, sex, race, and marital status), as well as each patient's street address. The latter, in combination with U.S. Census block data,31 was used to estimate household income for each patient. Automated encounter data were used to capture information on the number of ambulatory care visits, associated ICD-9-CM codes, and procedures received. Data on receipt of laboratory testing and test results were compiled from a comprehensive, computerized medical information management system, and pharmacy claims data were used to compile information on the use of insulin and oral agents. We used the ICD-9-CM codes associated with each patient's outpatient encounters to construct indicator variables reflective of cardiovascular disease, retinopathy, and nephropathy associated with diabetes. This was done using the classification scheme proposed by Selby et al.,32 collapsed to reflect that used by Greenfield et al.33 All data were compiled to reflect activity during the 12-month period prior to randomization.
Data on routine monitoring and screening receipt, as well as visits and laboratory testing results, were also compiled for the 6- and 12-month periods following randomization. Measures reflective of the diabetes-related routine monitoring and screening services received by patients were based on the American Diabetes Association Clinical Practice Recommendations' Standard of Medical Care for Patients with Diabetes.1 According to these guidelines, all adult patients regardless of diabetes type should (1) be tested annually for lipid disorders with a fasting lipid profile; (2) receive a glycated hemoglobin test at least 2 times per year; and (3) receive an annual dilated retinal exam. For analyses, patients were classified as having received or not received each test during both the 6-month and the 12-month period following their birthday. For each of the same 2 periods, we also constructed indicator variables reflecting whether all 3 of the diabetes-related services (glycated hemoglobin testing, LDL cholesterol testing, and retinal exam) were received, and whether or not an ambulatory care visit for diabetes was incurred. In addition to these measures of service receipt, for the 12-month period only, we constructed 2 additional variables. The first reflected whether or not 2 HbA1c tests were received and the second reflected whether or not 2 ambulatory care visits for diabetes occurred.
Finally, to determine whether the mailed reminder program had any effect on HbA1c and LDL cholesterol control, we constructed variables reflective of HbA1c and LDL cholesterol levels in the 12-month period following randomization. These variables were constructed using the last recorded HbA1c and LDL cholesterol level available in the 12-month period. We constructed 4 variables. The first two reflect the Comprehensive Diabetes Care Measures set forth in the National Committee for Quality Assurance's Health Plan Employer Data and Information Set: (1) HbA1c poorly controlled (>9.5%) or not tested and (2) lipids tested and controlled (LDL <130 mg/dL).34 The second two reflect more stringent control levels and are consistent with ADA guidelines: (1) HbA1c tested and <8% and (2) lipids tested and <100 mg/dL.1 Patients for whom such values were not available (i.e., those who did not receive any test in the 12-month period following randomization) were classified as not within the recommended range (e.g., HbA1c >9.5%).
Statistical Analyses
The adequacy of the randomization process was assessed using χ2 tests and t tests, as appropriate. Patients randomized to receive the mailed reminder were compared to those randomized to usual care in terms of sociodemographic characteristics (age, sex, race, marital status, and estimated household income), diabetes-related complications and comorbidities, and prescription drug use as well as visit, screening, and laboratory testing result history.
To assess the effect of mailed reminder receipt, we fit both unadjusted and adjusted logistic regression models. The unadjusted models included only an indicator reflective of whether the mailed reminder was received. In the adjusted models, we also included measures reflective of the patient's sociodemographic characteristics, diabetes-related complications and comorbidities, prescription drug use, and visit, screening, and laboratory testing result history. As outlined in Table 1, we fit a total of 16 logistic regression models: 5 reflected receipt of routine testing and screening in the 6-month period following randomization; 7 reflected receipt of routine testing and screening in the 12-month period following randomization; and 4 reflected LDL cholesterol and HbA1c control during the 12-month period following randomization.
Table 1.
Effectiveness Measures Evaluated
| 6 Months following randomization |
| Process measures |
| Lipid profile performed |
| HbA1c performed |
| Dilated eye exam performed |
| Lipid profile, HbA1c and eye exam performed |
| Outpatient visit for diabetes |
| 12 Months following randomization |
| Process measures |
| Lipid profile performed |
| HbA1c performed |
| 2 HbA1cs performed |
| Dilated eye exam performed |
| Lipid profile, HbA1c and eye exam performed |
| Outpatient visit for diabetes |
| 2 Outpatient visits for diabetes |
| Outcome measures |
| HbA1c poorly controlled (>9.5%) |
| HbA1c ≤8% |
| Lipids controlled |
| LDL <130 mg/dL |
| LDL <100mg/dL |
HbA1c, hemoglobin A1c; LDL, low-density lipoprotein.
Because it may be inappropriate to treat patients receiving their care from the same PCP as independent observations for statistical estimation, we assessed the intraclass correlation, or similarity, among study patients receiving care from the same PCP during the 6- and 12-month periods preceding randomization. This was done using the analysis of variance estimator for intraclass correlation35 as proposed by Elston for use with binary outcomes.36 Using this method, we found intraclass correlation coefficients that ranged from a low of 0.01 (for receipt of a diabetes visit in the 12-month period preceding randomization and receipt of a retinal exam in the 6-month period preceding randomization) to a high of 0.09 (for receipt of 2 HbA1c tests and 1 lipid profile in the 12-month period preceding randomization). Although these intraclass correlation coefficients are relatively small, to ensure that significance levels were not overstated, we used generalized estimating equation approaches to fit each of the logistic regression equations of interest.37 All models were fit using PROC GENMOD within the SAS System.38
RESULTS
Patient Characteristics
Table 2 presents the characteristics of the patients randomized to receive the mailed reminder program and those randomized to receive usual care. With the exception of estimated household income, which we were not able to compute with available address information for 108 patients, no study data were missing. As indicated in the table, patients were on average almost 60 years old, just over half were female, and just over half were white. Almost 60% of the study population received an HbA1c test in the 6 months preceding the mailed reminder program, and approximately half received a lipid profile and a retinal exam in the 12 months preceding the mailed reminder program. We found no statistically significant differences in these and the other characteristics listed in Table 2 between patients randomized to receive the mailed reminder program or usual care.
Table 2.
Baseline Year Patient Characteristics by Study Arm
| Mailed Reminder (N = 1,641) | Usual Care (N = 1,668) | |
|---|---|---|
| Sociodemographics | ||
| Average age, y | 59.9 | 59.6 |
| Male, % | 48.5 | 47.0 |
| White, % | 54.1 | 53.7 |
| Married, % | 62.3 | 62.2 |
| Average household income, $ | 39,208 | 39,211 |
| Comorbidities, % | ||
| Eye comorbidity | 6.2 | 5.7 |
| Cardiac comorbidity | 39.6 | 40.9 |
| Renal comorbidity | 6.9 | 6.2 |
| HbA1c testing in prior 6 months, % | ||
| No HbA1c Test | 37.8 | 40.2 |
| HbA1c ≥10% | 11.0 | 10.8 |
| HbA1c 8–10% | 18.9 | 18.4 |
| HbA1c ≤8% | 32.2 | 30.6 |
| Lipid profile testing in prior 12 months, % | ||
| No LDL Test | 52.0 | 55.3 |
| LDL ≥100 | 35.2 | 32.0 |
| LDL <100 | 12.8 | 12.8 |
| Prescription drug use in prior 12 months, % | ||
| Oral agent only | 45.3 | 43.2 |
| Insulin | 28.4 | 26.9 |
| Neither | 26.3 | 29.9 |
| Retinal exams and office visits in prior 12 months | ||
| Dilated retinal exam, % | 49.9 | 47.1 |
| Average number diabetes visits | 3.2 | 3.0 |
| Average number other visits | 8.5 | 8.5 |
Note: All comparisons between mailed reminder and usual care group were not statistically significant (i.e., P > .10). HbA1c, hemoglobin A1c; LDL, low-density lipoprotein.
Effectiveness of the Mailed Reminder Program
In the 6 months following randomization, patients who received the mailed reminder were more likely to receive each of the 5 services of interest (Table 3). Three of these differences were statistically significant (receipt of a retinal examination, all 3 tests, and an office visit for diabetes care), with patients who received the mailed reminder more likely than their counterparts to receive the service of interest during the 6-month period following reminder receipt. In the 12 months following reminder receipt, patients who received the mailed reminder were more likely to receive each of the services of interest (Table 3). As with the 6-month period, patients who received the mailed reminder were significantly more likely to receive a retinal exam, all 3 tests, and a visit for diabetes care within the 12-month period following randomization. Within the 12-month period, patients were also significantly (P < .05) more likely to receive at least 1 HbA1c test. Despite these findings of statistical significance, the differences in the rates of service receipt between the mailed reminder and usual care groups was relatively small. At no time did we find absolute differences in the rate of service receipt greater than 6% between those who did and did not receive the mailed reminder packet.
Table 3.
Unadjusted Rates of Service Receipt by Study Arm
| Mailed Reminder N = 1,641 | Usual Care N = 1,668 | Odds Ratio | 95% CI | |
|---|---|---|---|---|
| 6 Months from randomization | ||||
| 1 HbA1c | 61.6 | 58.9 | 1.12 | 0.98 to 1.27‡ |
| 1 Retinal exam | 31.4 | 26.2 | 1.29 | 1.12 to 1.49§ |
| 1 Fasting lipid profile | 35.2 | 33.3 | 1.09 | 0.93 to 1.26 |
| All 3 tests* | 13.6 | 10.9 | 1.30 | 1.04 to 1.61‖ |
| 1 Diabetes visit | 66.4 | 60.6 | 1.28 | 1.12 to 1.47§ |
| 12 Months from randomization | ||||
| 1 HbA1c | 76.6 | 72.9 | 1.21 | 1.03 to 1.43‖ |
| 2 HbA1c | 50.3 | 49.3 | 1.04 | 0.91 to 1.19 |
| 1 Retinal exam | 43.8 | 38.8 | 1.23 | 1.07 to 1.41§ |
| 1 Fasting lipid profile | 54.3 | 51.1 | 1.14 | 0.99 to 1.31‡ |
| All 3 tests† | 21.6 | 18.1 | 1.25 | 1.06 to 1.48§ |
| 1 Diabetes visit | 77.2 | 72.9 | 1.25 | 1.09 to 1.44§ |
| 2 Diabetes visits | 61.9 | 58.8 | 1.13 | 0.99 to 1.29‡ |
| HbA1c poorly controlled (>9.5%) | 37.5 | 41.9 | .83 | 0.73 to .96§ |
| HbA1c ≤8% | 45.3 | 42.1 | 1.14 | 1.00 to 1.31‡ |
| Lipids controlled | ||||
| LDL <130 mg/dL | 33.9 | 31.5 | 1.11 | 0.97 to 1.29 |
| LDL <100 mg/dL | 17.0 | 15.8 | 1.09 | 0.90 to 1.33 |
1 HbA1c, 1 retinal exam and 1 lipid profile.
2 HbA1c, 1 retinal exam and 1 lipid profile.
P < .10.
P < .01.
P < .05.
HbA1c, hemoglobin A1c; LDL, low-density lipoprotein.
Findings from the adjusted models (data not shown) generally confirmed these findings—both in terms of statistical significance and the magnitude of the estimated effects—with one exception. Once the other patient factors (i.e., those listed in Table 2) were controlled, at the 12-month period following randomization, there was not a significant difference in the receipt of 1 HbA1c test.
As shown in Table 3, patients with diabetes who received the mailed reminder were also more likely to have an LDL or HbA1c test within recommended ranges—although the magnitude of these differences, as with testing rates, is quite small. We did find mailed reminder recipients significantly more likely to have had an HbA1c test that did not reflect poor control (i.e., HbA1c >9.5%). We, however, found no statistically significant difference in the likelihood of having an HbA1c and LDL cholesterol test within recommended ranges between those receiving the mailed reminder and those receiving usual care. The adjusted model results (data not shown) again confirmed these findings.
DISCUSSION
We tested the effectiveness of a computerized mailed reminder packet from an individual's PCP for improving the management of patients with diabetes. We found the use of mailed reminders for patients with diabetes generally improved the rate of routine monitoring and screening receipt both in the short term (6 months), and the longer term (12 months) and tended to improve the proportion of patients with an HbA1c test that was not reflective of poor control. However, at no time did we find the use of mailed reminders to increase service receipt more than 6% over usual care. Similarly, the improvement in the proportion of patients with an HbA1c test that did not reflect poor control between intervention and usual care recipients was small.
Mailed reminders often have relatively small effects.16,39,40 We know of 2 published studies that have evaluated the use of mailed reminders to improve routine monitoring and screening among patients with diabetes. Both of these studies focused on the use of dilated retinal exams and both found that mailed reminders achieved a significant, albeit small, improvement in rates of dilated retinal exam receipt.39,40 At times, the low cost of such interventions relative to their potential benefits has been argued to justify their use, regardless of these small overall effects.16 In the case considered here, mailed reminders to patients with diabetes improved screening rates marginally and appeared to have a small effect on HbA1c levels. Given that 1% decreases in HbA1c levels have been found to be associated with 7% decreases in expected medical care costs, with specific cost reductions being more for individuals with chronic conditions and with higher initial levels of HbA1c,41 the cost-effectiveness of such programs deserves further exploration. Should additional studies continue to find substantial cost reductions associated with relatively small changes in HbA1c levels, the appeal of interventions such as the one evaluated here will only increase.
We developed the mailed reminder program as an extension to a web-based care management support system.29 This system, which includes registries of patients with diabetes, information about their care, and other critical information, was used to identify those patients eligible to receive the mailed reminder. Such systems, which often serve as the foundation for population-based interventions, are useful tools for establishing reminders and prompts for providers and patients to do appropriate routine monitoring and screening based on age, sex, specific conditions, or risk factors. Although successful chronic disease care includes the use of such supportive information systems and tools, such tools are only one component of what is thought to be necessary to ensure that the needs of patients with chronic diseases, such as diabetes, are met. As reflected in Wagner et al.'s model of chronic disease management, successful chronic care includes the use of explicit plans and protocols, practice redesign, attention to patient educational needs, ready access to necessary expertise, and supportive information systems.42 Thus, successful chronic disease management requires attention to system, provider, and patient factors.
A patient mailed reminder program obviously addresses only one such factor: the patient. Therefore, the effect of the intervention many have been attenuated in a system that does not address other systems and barriers. In other words, educating patients and getting them into the office (the percent with at least 1 diabetes visit 6 months following randomization was 66.4% in the intervention group versus 60.6% in the control group) may not be enough to have a large effect on diabetes management without addressing other system and physician issues related to the office visit itself.43 Within a more comprehensive disease management program, the greatest use of mailed reminders may be as outreach to those patients who are not routinely being seen in an office setting. This is particularly true in that other analyses conducted by us (not reported here) showed that well over half the patients who lapse in routine monitoring and screening have been seen in the clinic within the past 12 months.
There are a number of potential limitations to our study. First, we in effect gave physicians the option of participating or not in the study. That is, some physicians chose not to return their list of patients, thus effectively opting out of the study. While we can only speculate as to whether we would have seen a different effect among patients of physicians who elected not to participate, if one assumes that those physicians who elected to participate have a greater interest in diabetes care management/improvement, it may be reasonable to assume that findings here are conservative. Furthermore, we gave participating physicians the opportunity to remove names from the list of eligible patients. Although this ensured that patients were not inappropriately sent a mailed reminder, it added costs to the intervention process and introduced potential selectivity bias into our sample. Physicians did not routinely provide us with their reason(s) for excluding a patient. Those who did often indicated that they were not currently the patient's PCP. Second, because not everyone received an HbA1c and LDL cholesterol test in the follow-up year, we evaluated the effect of the intervention on the proportion of individuals “known to be in control.” That is, we assumed that individuals who were not tested were not achieving ideal HbA1c or LDL cholesterol levels. If those who were not tested differed significantly between groups, such an approach may have caused the data to reflect inaccurately the effectiveness of the intervention on HbA1c and LDL cholesterol levels. Third, whether this process is feasible within or these results generalize to other delivery settings is not known. Given that the informatic capability within delivery settings is growing, it is hopefully only a matter of time before the capability is readily available. Finally, any care patients received outside of the medical group is not reflected in our analyses. Although this may result in an underreporting of care receipt, it is problematic to evaluation results only if one believes that outside use occurred differentially among treatment and control group patients.
We found the use of a patient mailed reminder to increase the rate of diabetes-related routine monitoring and screening and to tend to improve HbA1c levels among patients with diabetes. However, improvements at the population level were modest. As is the case nationwide, the management of patients with diabetes within this study setting has been improving over time.44 Yet as reflected in these data and those nationwide,44 substantial room for improvement remains. Further research is needed to understand the role that mailed reminders can play in chronic disease management, and assuming that they continue to be found effective, the cost-effectiveness of their inclusion in comprehensive disease management programs.
Acknowledgments
We wish to thank Dr. Fred Whitehouse for his valuable comments and suggestions during the development of the mailed reminder, and Ms. Kim Sadlocha for her keen eye for design, organizational skills, and patience. Without their contributions this work would not have been possible.
REFERENCES
- 1.American Diabetes Association. Clinical practice recommendations–1998. Diabetes Care. 1998;21:1S–95S. [PubMed] [Google Scholar]
- 2.Wisdom K, Fryzek JP, Havstad SL, Anderson RM, Dreiling MC, Tilley BC. Comparison of laboratory test frequency and test results between African-Americans and Caucasians with diabetes: opportunity for improvement. Diabetes Care. 1997;20:971–7. doi: 10.2337/diacare.20.6.971. [DOI] [PubMed] [Google Scholar]
- 3.Harris MI. Medical care for patients with diabetes: epidemiological aspects. Arch Intern Med. 1996;124:117–22. doi: 10.7326/0003-4819-124-1_part_2-199601011-00007. [DOI] [PubMed] [Google Scholar]
- 4.Hiss RG. Barriers to care in non-insulin-dependent diabetes mellitus: the Michigan experience. Arch Intern Med. 1996;124:146–8. doi: 10.7326/0003-4819-124-1_part_2-199601011-00012. [DOI] [PubMed] [Google Scholar]
- 5.Weiner JP, Parente ST, Garnick DW, Fowles J, Lawthers AG, Palmer H. Variation in office-based quality. A claims-based profile of care provided to Medicare patients with diabetes. JAMA. 1995;273:1503–8. doi: 10.1001/jama.273.19.1503. [DOI] [PubMed] [Google Scholar]
- 6.Kenny SJ, Smith PJ, Goldschmid MG, Newman JM, Herman WH. Survey of physician practice behaviors related to diabetes mellitus in the U.S. Physician Adherence to Consensus recommendations. Diabetes Care. 1993;16:1507–10. doi: 10.2337/diacare.16.11.1507. [DOI] [PubMed] [Google Scholar]
- 7.Brechner RJ, Cowie CC, Howie JL, Herman WH. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993;270:1714–8. [PubMed] [Google Scholar]
- 8.Peterson KA. Diabetes care by primary care physicians in Minnesota and Wisconsin. J Fam Pract. 1994;38:361–7. [PubMed] [Google Scholar]
- 9.Martin TL, Selby JV, Zhang D. Physician and patient prevention practices in NIDDM in a large urban managed-care organization. Diabetes Care. 1995;18:1124–32. doi: 10.2337/diacare.18.8.1124. [DOI] [PubMed] [Google Scholar]
- 10.Marshal CL, Bluestein M, Chapin C, et al. Outpatient management of diabetes mellitus in five Arizona Medicare managed care plans. Am J Med Qual. 1996;11:87–93. doi: 10.1177/0885713X9601100206. [DOI] [PubMed] [Google Scholar]
- 11.Elston Lafata J, Martin S, Morlock R, Divine GW, Xi H. Provider type and the receipt of general and diabetes related preventive health services among patients with diabetes. Med Care. 2000;39:491–9. doi: 10.1097/00005650-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 12.U.S. Department of Health and Human Services. Understanding and Improving Health. Washington, DC: U.S. Government Printing Office; 2000. Healthy People 2010. [Google Scholar]
- 13.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 14.Szilagyi PG, Bordley C, Vann JC, et al. Effect of patient reminder/recall interventions on immunization rates. A review. JAMA. 2000;284:1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 15.Pearson D, Jackson LA, Winkler B, Foss B, Wagener B. Use of an automated pharmacy system and patient registries to recruit HMO enrollees for an influenza campaign. Eff Clin Pract. 1999;2:17–22. [PubMed] [Google Scholar]
- 16.Baker AM, McCarthy BD, Gurley VF, Ulcickas Yood M. Influenza immunization in a managed care organization. J Gen Intern Med. 1998;13:469–75. doi: 10.1046/j.1525-1497.1998.00136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith DM, Zhou XH, Weinberger M, Smith F, McDonald RC. Mailed reminders for area-wide influenza immunization: a randomized controlled trial. J Am Geriatr Soc. 1999;47:1–5. doi: 10.1111/j.1532-5415.1999.tb01893.x. [DOI] [PubMed] [Google Scholar]
- 18.Skinner CS, Strecher VJ, Hospers H. Physicians' recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–9. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wagner TH. The effectiveness of mailed patient reminders on mammography screening: a meta-analysis. Am J Prev Med. 1998;14:64–70. doi: 10.1016/s0749-3797(97)00003-2. [DOI] [PubMed] [Google Scholar]
- 20.Margolis K, Menart TC. A test of two interventions to improve compliance with scheduled mammography appointments. J Gen Intern Med. 1996;11:539–41. doi: 10.1007/BF02599601. [DOI] [PubMed] [Google Scholar]
- 21.Mayer JA, Bartholomew S, Clapp EJ, Elder J. Facility-based inreach strategies to promote annual mammograms. Am J Prev Med. 1994;10:353–6. [PubMed] [Google Scholar]
- 22.Richardson A, Williams S, Elmwood M, Bahr M, Medicott T. Participation in breast cancer screening: randomised controlled trials of doctors' letters and of telephone reminders. Aust J Public Health. 1994;18:290–2. doi: 10.1111/j.1753-6405.1994.tb00247.x. [DOI] [PubMed] [Google Scholar]
- 23.Clayton AE, McNutt LA, Homestead HL, Hartman TW, Senecal S. Public health in managed care: a randomized controlled trial of the effectiveness of postcard reminders. Am J Public Health. 1999;89:1235–7. doi: 10.2105/ajph.89.8.1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Burack RC, Gimotty PA, McBride S, et al. How reminders given to patients and physicians affected pap smear use in a health maintenance organization. Results of a randomized controlled trial. Cancer. 1998;82:2391–400. doi: 10.1002/(sici)1097-0142(19980615)82:12<2391::aid-cncr13>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 25.O'Connor AM, Griffiths CJ, Underwood MR, Eldridge S. Can postal prompts from general practitioners improve the uptake of breast screening? A randomised controlled trial in one east London general practice. J Med Screen. 1997;5:49–52. doi: 10.1136/jms.5.1.49. [DOI] [PubMed] [Google Scholar]
- 26.Armstrong K, Berlin M, Schwartz JS, Propert K, Ubel PA. Educational content and the effectiveness of influenza vaccination reminders. J Gen Intern Med. 1999;14:695–8. doi: 10.1046/j.1525-1497.1999.11098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Skaer TL, Sclar DA, Markowski DJ, Won JKH. Effect of value-added utilities on prescription refill compliance and health care expenditures for hypertension. J Hum Hypertens. 1993;7:515–8. [PubMed] [Google Scholar]
- 28.Skaer TL, Sclar DA, Markowski DJ, Won JKH. Effect of value-added utilities on prescription refill compliance and medicaid health care expenditures–a study of patients with non-insulin-dependent diabetes mellitus. J Clin Pharm Ther. 1993;18:295–9. doi: 10.1111/j.1365-2710.1993.tb00591.x. [DOI] [PubMed] [Google Scholar]
- 29.Baker AM, Elston Lafata J, Ward RE, Whitehouse FW, Divine G. A web-based diabetes care management support system. J Comm J Qual Improv. 2001;27:179–90. doi: 10.1016/s1070-3241(01)27016-3. [DOI] [PubMed] [Google Scholar]
- 30.Channing L. Bete Co., Inc. Living Well with Diabetes. A Handbook for People with Diabetes and Their Families. South Deerfield, Mass: Channing L. Bete, Co., Inc.; 1998. [Google Scholar]
- 31.U.S. Bureau of the Census. Census of Population and Housing, 1990: Summary tape file 3 on CD-ROM. Washington, DC: U.S. Census Bureau; 1992. [Google Scholar]
- 32.Selby JV, Thomas Ray G, Zhang D, Colby CJ. Excess costs of medical care for patients with diabetes in a managed care population. Diabetes Care. 1998;20:1396–402. doi: 10.2337/diacare.20.9.1396. [DOI] [PubMed] [Google Scholar]
- 33.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin-dependent diabetes mellitus treated by different systems and specialties: results from the medical outcomes study. JAMA. 1995;274:1436–44. [PubMed] [Google Scholar]
- 34.National Committee on Quality Assurance. The State of Managed Care Quality, 2001. Comprehensive Diabetes Care. Available at: http://www.ncqa.org/somc2001/DIABETES/ SOMC_2001_CDIAB.html. Accessed December 20, 2001.
- 35.Ridout MS, Demetrio CGB, Firth D. Estimating intraclass correlation for binary data. Biometrics. 1999;55:137–48. doi: 10.1111/j.0006-341x.1999.00137.x. [DOI] [PubMed] [Google Scholar]
- 36.Elston RC. Comments on estimating heritability of a dichotomous trait. Biometrics. 1977;33:232–3. [PubMed] [Google Scholar]
- 37.Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]
- 38.SAS Institute Inc. SAS/STAT Software: Changes and Enhancements for Release 6.12. Cary, NC: SAS Institute Inc.; 1996. [Google Scholar]
- 39.Legorreta AP, Hasan MM, Peters AL, Pelletier KR, Leung KM. An intervention for enhancing compliance with screening recommendations for diabetic retinopathy. Diabetes Care. 1997;20:520–3. doi: 10.2337/diacare.20.4.520. [DOI] [PubMed] [Google Scholar]
- 40.Halbert RJ, Nichol JM, Kwan-Moon L, Legorreta A. Effect of multiple patient reminders in improving diabetic retinopathy screening. A randomized trial. Diabetes Care. 1999;22:752–5. doi: 10.2337/diacare.22.5.752. [DOI] [PubMed] [Google Scholar]
- 41.Gilmer TP, O'Connor PJ, Manning WG, Rush WA. The cost to health plans of poor glycemic control. Diabetes Care. 1997;20:1847–53. doi: 10.2337/diacare.20.12.1847. [DOI] [PubMed] [Google Scholar]
- 42.Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 43.Cabana MD, Rand CS, Powe NR, et al. Why don't physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 44.National Committee on Quality Assurance. The State of Managed Care Quality, 2001. Key Findings. Available at: http://www.ncqa.org/somc2001/DIABETES/SOMC_2001_KEY.html. Accessed December 20, 2001. [Google Scholar]