Abstract
OBJECTIVE
Cross-cultural ethical conflicts are common. However, little is known about how and to what extent acculturation changes attitudes toward end-of-life care and advance care planning. We compared attitudes toward end-of-life care among Japanese Americans and Japanese in Japan.
DESIGN
Self-administered questionnaire in English and Japanese.
SETTING AND PARTICIPANTS
Community-based samples of Japanese Americans in Los Angeles and Japanese in Nagoya, Japan: 539 English-speaking Japanese Americans (EJA), 340 Japanese-speaking Japanese Americans (JJA), and 304 Japanese living in Japan (JJ).
MEASUREMENTS AND MAIN RESULTS
Few subjects (6% to 11%) had discussed end-of-life issues with physicians, while many (EJA, 40%; JJA, 55%; JJ, 54%) desired to do so. Most preferred group surrogate decision making (EJA, 75%; JJA, 57%; JJ, 69%). After adjustment for demographics and health status, desire for informing the patient of a terminal prognosis using words increased significantly with acculturation (EJA, odds ratio [OR] 8.85; 95% confidence interval, [95% CI] 5.4 to 14.3; JJA, OR 2.8; 95% CI 1.8 to 4.4; JJ, OR 1.0). EJA had more-positive attitudes toward forgoing care, advance care planning, and autonomous decision making.
CONCLUSION
Preference for disclosure, willingness to forgo care, and views of advance care planning shift toward western values as Japanese Americans acculturate. However, the desire for group decision making is preserved. Recognition of the variability and acculturation gradient of end-of-life attitudes among Japanese Americans may facilitate decision making and minimize conflicts. Group decision making should be an option for Japanese Americans.
Keywords: cross-cultural comparison, acculturation, terminal care, advance directives, decision making
In the United States, advance care planning is promoted to facilitate medical care toward the end of life.1–3 Advance care planning, the process of considering the patient's preferences in deciding on a plan for future care, often employs an advance directive to specify care preferences and a surrogate to make decisions if the patient is unable to do so. Studies in the United States reveal that patients and the general public desire to discuss end-of-life issues with their physicians, and endorse advance directives.4–7 Acceptance of advance care planning among non-whites, however, is lower than among whites,8–10 and advance directives may not meet the needs of some ethnic groups.8,11–13 This is illustrated in the many cross-cultural difficulties with end-of-life care decision making.12–17
Clinicians in culturally diverse settings commonly describe ethical dilemmas due to cultural variation in end-of-life preferences and perceptions of how decisions should be made. Examples include families and patients that block information disclosure, variable locus of decision-making authority, and unusual views about acceptable permanent health states. As the U.S. population becomes more diverse, investigation into cultural diversity is increasing.8,12–18
Although understanding cross-cultural variation in decision-making attitudes and preferences would facilitate clinical decisions, there has been little investigation into the decision-making models of ethnic groups and within-group variation due to factors such as acculturation. The objective of this study is to investigate how and to what extent acculturation influences attitudes toward end-of-life care among individuals of Japanese descent. Japanese culture, which traditionally emphasizes familial harmony, engenders end-of-life practices and communication styles that differ substantially from those in the United States.11,19–33 For example, in Japan, a fatal diagnosis and prognosis, especially cancer, often are not disclosed to the patient,23–27 and the family is preeminent in the decision-making process.27–30 Furthermore, the concept of advance care planning is unfamiliar in Japan.27,29,31–33 In addition, the long history of Japanese immigration to the United States yields a wide range of generations, from first to fifth, with multiple levels of acculturation.34,35 In this study, we examine the association between acculturation of Japanese Americans and Japanese in Japan regarding 1) desires to discuss end-of-life issues with a physician, 2) preferred decision-making model, 3) disclosure of bad news, and 4) attitudes toward forgoing care and advance care planning.
METHODS
Study Population
To explore attitudes toward end-of-life care, we targeted older Japanese Americans and Japanese. We identified 2 Japanese-American cohorts with different levels of acculturation and 1 cohort in Japan. As a proxy measure of acculturation, we used Japanese language fluency as a sampling frame. A more-acculturated cohort, English-speaking Japanese Americans (EJA) were randomly sampled from the member lists of 3 geographically different Japanese-American community centers in the greater Los Angeles area. A less-acculturated cohort of Japanese Americans, Japanese-speaking Japanese Americans (JJA), were derived from the residents of 2 apartment complexes for Japanese elderly in Little Tokyo, Los Angeles, members of the 2 social clubs for Japanese elderly, and the Japanese staff of 2 Japanese-American social organizations in Los Angeles. The Japanese cohort in Japan was sampled from a social club for the elderly and older family members of workers at a hospital in Nagoya, Japan.
Questionnaire Development and Translation
The self-administered questionnaire developed for this study includes both previously validated8,12,36 and newly designed scales. First, an English language instrument was developed on the basis of the findings from 9 focus groups with English-speaking Japanese Americans, 5 focus groups of Japanese-speaking Japanese Americans in Los Angeles, and 5 focus groups in Tokyo, Japan.37 Survey items were modified and newly developed on the basis of these findings.
In order to create the Japanese language survey, we employed forward and backward translation. Two bilingual translators, native speakers of Japanese, independently translated the English questionnaire into Japanese. Another bilingual translator reviewed these Japanese translations, reconciled differences, and created a draft Japanese questionnaire. Subsequently, a bilingual translator, who is a native speaker of English, translated this Japanese questionnaire back into English. The English back-translation was compared to the original English questionnaire. No major contextual differences were found; minor changes were made to clarify meaning and ensure congruence of items. Included in the survey were the SF-12 Health Survey38 derived from a previously validated Japanese version of the SF-36 Health Survey,39,40 and Ende's autonomy preference index.41,42 We pretested the Japanese language questionnaire items among 10 bilingual Japanese Americans living in Los Angeles. This pilot revealed that the English and Japanese language surveys took approximately 20 minutes to complete.
Survey Contents
The survey consists of demographic questions, questions about health status, and questions about end-of-life decision making. Demographic items queried age, gender, annual household income, years of education, marital status, residential status, religiosity, religious affiliation, and health insurance status. Measures of health and health care included a count of chronic health conditions and health-related quality of life (HRQOL) using the SF-12 Health Survey, hospitalization in the past 6 months, having a regular doctor, and experience of visiting an intensive care unit (ICU). The household income for Japanese in Japan was converted to dollars using $1 = ¥140, based on comparative price levels of both countries in 1999.43
Acculturation
In order to characterize Japanese Americans in a detail exceeding generational descriptions (i.e., Issei = first generation), we asked questions to assess respondents' degree of acculturation. The 6-item scale for measuring acculturation among Japanese Americans, modified from the Suinn-Lew Asian Self-Identity Acculturation Scale,44,45 yielded acculturation scores ranging from 0 to 100 (100 = most acculturated). These items included preferred language, self-designated ethnicity, location of respondent's birth and rearing, and the number of foreign-born parents and grandparents.46
End-of-life Decision Making, Disclosure, and Attitudes
To understand end-of-life communication with one's physician, we asked, “Has a doctor ever talked to you about your wishes for medical care in the event that you become severely ill with a life-threatening illness?” Those who answered “No” were then asked, “Would you like to discuss this with your doctor?” The preferred decision-making model was elicited by asking, “If you had a life-threatening illness and could not make decisions for yourself, who would you want to make decisions about using life-sustaining machines?” For respondents desiring a group of family or friends to make surrogate decisions, we asked whether they would be willing to choose a single individual.
To investigate preferences for disclosure of bad news, we offered a modified version of a case scenario used in a prior cross-cultural study by Blackhall et al.8,12 We asked the respondent whether the physician should disclose “the patient has a cancer” (cancer diagnosis), “the patient will probably die from cancer” (terminal prognosis), and who should make decisions. On the basis of focus group findings, disclosure using “non-verbal communication” was added as an option to the terminal prognosis scenario.
Attitudes toward end-of-life care were measured with 4 multi-item scales. Two 3-item scales measured willingness to use medical care to maintain survival in a permanent coma (Chronbach's α = 0.83) and willingness to withdraw care (α = 0.68). A 5-item scale assessed attitudes toward advance care planning (α = 0.88). These 3 scales were modified from items of Blackhall et al.8 The autonomy preference scale measured subjects' interest in making decisions for themselves (α = 0.89).
Survey Procedure
The self-administered survey was carried out in 1997 for EJA, and in 1998 for JJA and Japanese living in Japan (JJ). The survey was mailed to EJA and JJA samples. The JJ sample received hand-delivered surveys. A follow-up postcard reminder and repeat survey mailing was sent to all nonrespondents. The Institutional Review Board at University of California, Los Angeles approved the survey protocol.
Statistical Analysis
Differences in categorical variables across the 3 cohorts were assessed using Pearson χ2 tests. Because age and gender differed significantly across the cohorts, all comparisons were adjusted for age and gender using logistic regression. The adjusted results for categorical variables are presented using the predicted probability from a model including age, gender, and cohort dummies.
We used logistic regression to evaluate the independent effect of each cohort on the dependent variables of end-of-life discussion with a physician, decision-making model, and disclosure. End-of-life discussion with a physician was evaluated by dichotomizing “discussed or desired to discuss” versus “would not desire to discuss.” The 26% of respondents who chose “do not know” were excluded from this analysis. A repeat analysis performed after collapsing those who chose “do not know” and “would not desire to discuss” did not substantially change the model. For the end-of-life decision-making model variables, those who answered “physician alone” and “one individual” were grouped together, and compared to those who preferred a “group.” The variables for disclosure of terminal prognosis to the patient and to the family were dichotomized by collapsing nondisclosure with nonverbal disclosure, because neither is a standard practice in U.S. end-of-life care. Independent variables in the logistic models included: age, gender, marital status, years of education, household income, whether the subject lives alone, working status, religiosity, religious affiliation (Christian versus non-Christian), physical and mental HRQOL scores (0 to 100), whether the subject had 2 or more chronic illnesses, whether the subject had a regular physician, hospitalization in the past 6 months, and having ever visited an ICU.
Regression models of multi-item attitude variables used the same set of independent variables employed in the logistic regression models. Results were expressed as the adjusted mean of each cohort from this model. The comparison of adjusted values across the cohorts was conducted using Tukey-Kramer multiple comparison. All statistical analyses were performed using SAS, Version 6.47
RESULTS
Five hundred thirty-nine EJA, 340 JJA, and 304 JJ responded to the survey with a response rate of 92%, 82% and 91%, respectively. EJA received more education than the other groups. JJA were more likely to be female, older, widowed, and to have lower household income and live alone. JJ were less likely to describe themselves as religious. The percentage of Christians decreased stepwise from EJA to JJ, while the proportion of Buddhists increased. Most EJA were Nisei (second generation) and Sansei (third generation), whereas JJA were mainly Issei/Shin-issei (first generation) and Kibei (second generation raised in Japan). On the 0 to 100 acculturation score, EJA had a mean score of 69 and JJA had a mean score of 26. Japanese Americans reported more chronic conditions than Japanese in Japan. The mean physical and mental HRQOL scores gradually decreased from EJA to JJ. About half of EJA and JJA were covered by private insurance; all residents in Japan have universal insurance coverage. Despite universal coverage, JJ were less likely to report having a regular doctor (Table 1).
Table 1.
Characteristics of Respondents
| English-speaking Japanese Americans | Japanese-speaking Japanese Americans | Japanese Living in Japan | |
|---|---|---|---|
| Respondents/total sample | 539/589 | 340/415 | 304/335 |
| Response rate, % | 92 | 82 | 91 |
| Mean age (SD)* | 62.8 (14.3) | 74.3 (10.0) | 64.3 (8.7) |
| Range | 17 to 95 | 24 to 98 | 31 to 90 |
| Male, %* | 61.1 | 35.7 | 46.5 |
| Marital status, %* | |||
| Married | 70.1 | 50.2 | 77.3 |
| Divorced/separated | 5.7 | 10.6 | 5.3 |
| Widowed | 19.3 | 33.5 | 13.4 |
| Single | 5.1 | 5.7 | 4.0 |
| Lives alone, %* | 15.9 | 44.4 | 10.9 |
| Household income, %*,† | |||
| ≤$50.000 | 55.3 | 84.4 | 57.5 |
| >$50.000 | 44.7 | 15.6 | 42.5 |
| Working, %* | 47.8 | 24.8 | 43.5 |
| Mean y of education (SD)* | 14.3 (2.9) | 11.5 (2.7) | 11.5 (2.6) |
| Self-described religious person, %* | 50.3 | 54.6 | 39.5 |
| Religion, %* | |||
| Christian | 36.7 | 13.8 | 1.7 |
| Buddhist | 46.2 | 60.7 | 67.3 |
| Other/no religion | 17.1 | 25.4 | 31.0 |
| Generation status*‡ | |||
| Issei/Shin-issei/Kibei | 15.9 | 85.3 | — |
| Nisei | 48.1 | 7.0 | — |
| Sansei/other | 40.0 | 7.7 | — |
| Mean acculturation score (SD)*,§ | 68.7 (23.5) | 25.8 (23.7) | — |
| Mean no chronic illnesses (SD)‖ | 2.1 (1.7) | 2.0 (1.7) | 1.7 (1.5) |
| HRQOL from SF-12, mean (SD)¶ | |||
| Physical summary score* | 49.4 (9.4) | 47.4 (8.7) | 45.7 (7.8) |
| Mental summary score* | 53.4 (8.0) | 49.9 (9.1) | 47.4 (7.7) |
| Health Insurance, %* | |||
| National insurance | — | — | 100 |
| Private | 58.8 | 47.7 | — |
| Medicare | 37.9 | 32.3 | — |
| Medicaid alone | 0.8 | 16.3 | — |
| No insurance | 1.7 | 2.1 | – |
| Have a regular doctor, %* | 96.6 | 92.1 | 59.9 |
| Hospitalization in past 6 mo, %* | 5.4 | 11.6 | 7.7 |
| Experienced an ICU visit, %* | 69.0 | 40.1 | 39.6 |
P < .001
Japanese yen converted to U.S. dollars ($1 = 140 yen).
Issei, 1st generation; Shin-issei, 1st generation immigrated after WWII; Kibei, 2nd generation raised in Japan during WW II; Nisei, 2nd generation; Sansei, 3rd generation; others are later generations.
Acculturation score ranges from 0 to 100; higher score indicates more acculturation.
P < .05
HRQOL, Health-related quality of life measured by SF-12 on 0 to 100 scale; higher score is better.
Discussion of End-of-life Care with Physician
Only 11% of EJA, 9% of JJA, and 6% of JJ had ever discussed end-of-life care with a physician, while 40% of EJA, 55% of JJA, and 54% of JJ desired such a discussion. Overall, similar proportions of each group had either discussed end-of-life care with a physician, or desired to do so. A substantial minority, 18% of EJA, 16% of JJA, and 23% of JJ said they did not want to discuss end-of-life care with their physicians; 31% of EJA, 20% of JJA, and 23% of JJ said that they “do not know” if they desired to discuss end-of-life care.
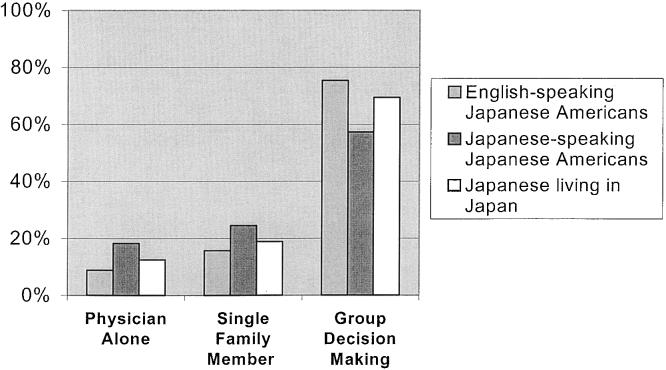
Preferred Surrogate Decision-making Model for End-of-life Care
As seen in Figure 1, 9% of EJA, 18% of JJA, and 12% of JJ would want the physician alone to make end-of-life care decisions if the respondents had a life-threatening illness and could not make decisions for themselves. A majority of each cohort preferred group surrogate decision making for life-sustaining treatments (75% of EJA, 57% of JJA, and 69% of JJ). However, JJA were somewhat more likely to want a single individual to make end-of-life care decisions (16% of EJA, 25% of JJA, and 19% of JJ).
FIGURE 1.
Preferred surrogate decision maker for end-of-life care. Results adjusted for age and gender.
Disclosing Bad News and Decision Making: The Case Scenario
More-acculturated respondents had much greater desire for informing patients of bad news. Compared to JJ, more EJA and JJA desired informing a patient of a cancer diagnosis. In contrast, almost all respondents desired informing family members of the diagnosis. These differences were accentuated in responses to the scenario of a terminal prognosis. Eighty-five percent of EJA desired informing the patient of impending death using words, compared to 63% of JJA and 36% of JJ. Consistent with the focus group findings, only 11% of EJA wanted the physician to use nonverbal communication in disclosing this information, whereas 23% of JJA and 31% of JJ chose this option. In contrast to Japanese Americans, about one third of JJ preferred to withhold the terminal prognosis from the patient. Most respondents desired that the family be informed of the prognosis; JJA and JJ more often wanted this done nonverbally (Table 2).
Table 2.
Disclosure of Bad News: The Case Scenario*
| English-speaking Japanese Americans | Japanese-speaking Japanese Americans | Japanese Living in Japan | |
|---|---|---|---|
| Cancer diagnosis | |||
| A doctor diagnoses a 60-year-old man as having stomach cancer that has spread to his lungs and liver. The cancer cannot be cured. | |||
| Should the doctor tell the patient that he has a cancer?† | |||
| Yes, tell the patient | 92.7 | 88.0 | 63.4 |
| No, don't tell the patient | 7.2 | 12.0 | 36.5 |
| Should the doctor tell the family members about a cancer? | |||
| Yes, tell one or more family members | 95.4 | 96.9 | 97.1 |
| No, don't tell the family | 4.6 | 3.1 | 2.9 |
| Terminal prognosis | |||
| The doctor believes that the patient will die from the cancer in the next few months. | |||
| Should the doctor tell the patient that he will probably die from the cancer?† | |||
| Yes, tell the patient using words | 84.6 | 62.7 | 35.6 |
| Yes, tell the patient using nonverbal communication | 10.7 | 23.2 | 31.2 |
| No, don't tell the patient | 4.7 | 14.1 | 33.2 |
| Should the doctor tell the patient's family that the patient will probably die from the cancer?† | |||
| Yes, tell the family using words | 92.5 | 84.0 | 81.5 |
| Yes, tell the family using nonverbal communication | 5.4 | 11.3 | 12.7 |
| No, don't tell the family | 2.1 | 4.6 | 5.7 |
| Decision making about life-sustaining treatment | |||
| The patient becomes ill but can still make decisions. A decision must be made whether to put him on a breathing machine. The machine will prolong the patient's life for a little while, but not cure the illness, and may be uncomfortable. Who should make decisions about use of the breathing machine?† | |||
| Patient alone | 30.9 | 28.3 | 23.4 |
| Patient and physician | 8.8 | 12.9 | 12.8 |
| Patient and family | 18.7 | 13.1 | 14.4 |
| Physician, patient, and family | 33.1 | 28.2 | 27.6 |
| Physician and family | 5.0 | 10.9 | 18.6 |
| Family alone | 1.2 | 0.7 | 1.0 |
| Physician alone | 0.8 | 2.7 | 2.1 |
All values adjusted for age and gender.
P < .001.
The scenario also asked respondents who should make a life-sustaining treatment decision for the patient with a terminal prognosis. Acculturation was associated with a greater preference for the patient to participate in decision making (EJA, 93%; JJA, 86%; JJ, 78%). However, most respondents preferred some kind of group decision making (Table 2).
Using logistic regression, we evaluated desire for an end-of-life discussion with a physician, surrogate decision-making model, and disclosure of a terminal prognosis to the patient and family after adjustment for demographic characteristics, health status, having a regular physician, recent hospitalization, and prior ICU visit (Table 3). After adjustment, there were no significant differences between cohorts in desire to discuss end-of-life care with a physician. EJA and JJ were equally likely to prefer a group surrogate decision-making model, whereas JJA were less likely to elect this model (odds ratio, 0.63; 95% confidence interval, 0.41 to 0.97), choosing physician alone or single surrogates more often. After adjustment, greater disclosure was associated with higher acculturation; compared to JJ, EJA had nearly 9 times the odds and JJA had nearly 3 times the odds of desiring that a terminal prognosis be communicated to the patient using words. With regard to disclosure to the family, EJA were more likely to desire disclosure of a terminal prognosis to the family using words than JJ, but JJA were not different from JJ.
Table 3.
Comparison of Physician Discussion, Decision making and Disclosure between English-speaking Japanese Americans, Japanese-speaking Japanese Americans, and Japanese Living in Japan, After Adjustment*,†
| English-speaking Japanese Americans, OR (95% CI) | Japanese-speaking Japanese Americans, OR (95% CI) | Japanese living in Japan, OR | |
|---|---|---|---|
| Discuss end of life with a physician | 0.73 (0.41 to 1.31) | 1.10 (0.62 to 1.94) | 1.0 |
| Group decision-making model | 1.11 (0.70 to 1.74) | 0.63 (0.41 to 0.97) | 1.0 |
| Terminal prognosis disclosure to the patient using words | 8.79 (5.42 to 14.3) | 2.80 (1.79 to 4.37) | 1.0 |
| Terminal prognosis disclosure to the family using words | 2.01 (1.05 to 3.88) | 1.03 (0.58 to 1.83) | 1.0 |
In addition to the cohort variable, the logistic regression model included the following variables: age, gender, marital status, residential status, years of education, household income, religiosity, religious group, physical and mental health–related quality of life, number of chronic conditions, have a regular physician, hospitalization in the past 6 months, and visit to an intensive care unit.
Reference group: Japanese living in Japan.
OR, odds ratio; CI, confidence interval.
End-of-life Attitudes
Attitudes toward end-of-life care varied with acculturation, with EJA having more-positive attitudes toward forgoing care and advance care planning. However, JJA displayed attitudes more aligned with traditional Japanese culture than even JJ respondents. Controlling for age and other demographics, EJA desired significantly less care to preserve permanent coma than did JJA (1.3 vs 1.7 on a 3-point scale; P < .001). EJA were more willing to withdraw care than were JJA and JJ (3.9 vs 3.3 vs 3.4, respectively on a 5-point scale; P < .001). JJA desired more care in adverse health states and were less willing to withdraw care compared to JJ, but the latter did not reach statistical significance.
EJA had significantly more-positive attitudes toward advance care planning, and JJA had significantly less-positive attitudes compared to JJ (4.7 vs 3.7 vs 4.1, respectively on a 5-point scale; P < .001). The scores on the autonomy preference index, where a higher score indicates a greater preference for autonomy in decision making, showed EJA desire significantly more autonomy than JJ, whereas JJA desired significantly less (Table 4).
Table 4.
Comparison of End-of-life Attitudes Between English-speaking Japanese Americans, Japanese-speaking Japanese Americans, and Japanese Living in Japan, After Adjustment*
| English-speaking Japanese Americans | Japanese-speaking Japanese Americans | Japanese living in Japan | |
|---|---|---|---|
| Attitudes toward forgoing care, adjusted mean values | |||
| Preserve survival in permanent coma | 1.33† | 1.66‡ | 1.42 |
| Willingness to withdraw care | 3.91†,‡ | 3.27 | 3.44 |
| Attitudes toward advance care planning, adjusted mean values | |||
| Willingness to participate in advance care planning | 4.69†,‡ | 3.66§ | 4.09 |
| Autonomy in decision making | 3.07†,‡ | 2.03‡ | 2.40 |
Attitude scores for multi-item scales computed as follows: preserve survival in permanent coma: 3-point scale (3 = desires care to preserve life in coma); willingness to withdraw life-sustaining care: 5-point scale (5 = more willing to withdraw care); willingness to participate in advance care planning: 5-point scale (5 = more willing to participate); autonomy in decision making: 5-point scale (5 = more autonomy). Adjustment included age, gender, marital status, household income, residential status, years of education, religiosity, religious group, have a regular physician, physical and mental health–related quality of life scores, number of chronic conditions, hospitalization in the past 6 months, and visit to an intensive care unit.
Pair-wise comparison versus Japanese-speaking Japanese Americans, P < .001.
Pair-wise comparison versus Japanese living in Japan, P <.001.
Pair-wise comparison versus Japanese living in Japan, P < .01.
DISCUSSION
There is no universal ethical standard for end-of-life care. In many countries, physicians rarely disclose a cancer diagnosis to patients, whereas disclosure is standard care in the United States.48–50 Desire for nondisclosure also is found among ethnic minorities in the United States.12 Controversy may develop when a minority patient or family acts on culturally-based values that are at variance with the U.S. norm. Japanese culture, which values harmonious group consensus and tacit agreement without verbal communication, contrasts sharply with the American values of self-determination and open discussion.20,24–33 Our cross-cultural survey revealed that, despite acculturation, people of Japanese cultural heritage retain some traditional Japanese attitudes that influence end-of-life care and decision making, while they gradually adopt some U.S. norms.
Irrespective of nationality or acculturation, few respondents had discussed end-of-life care with their physician, although about half of subjects desired to do so. Unlike cultures that are averse to end-of-life discussions,51,52 our results indicated that Japanese and Japanese Americans alike accept the notion of communication about end-of-life care. The fact that few subjects had communicated with physicians, similar to the pattern in mainstream U.S. samples,4,53 suggests that fundamental barriers to end-of-life discussion exist. One possible explanation is that discussing end-of-life issues is desirable but not a high priority for patients in the routine encounter.53 Another possibility is physician incapacity to address end-of-life issues because of time constraints, lack of education, or psychological barriers to this sensitive topic. These barriers may transcend culture rather than being transcultural obstacles.
All cohorts preferred a group decision-making model. Physicians should be aware that group decision making may be preferred when they treat patients of Japanese background. This family or group decision-making model is common throughout many cultures, especially in Asian cultures.12,54,55 Even among mainstream U.S. samples, older individuals may prefer family group decision making,56 and the importance of familial group integrity in end-of-life decision making is gaining recognition.28,57–59 Conflicts may arise if a single surrogate decision-making model, as suggested in typical proxy directives, is imposed on Japanese-American families. Advance care planning should be flexible enough to allow the option of family and group involvement in decision making.
Surprisingly, JJA, the less acculturated U.S. cohort, were more likely to designate a single decision maker than EJA. This may be due in part to this population's uniqueness as early immigrants, mainly first or second generation, who are less likely to have many relatives around them to form a group decision unit. Guided by traditional Japanese values of reservation and self-sacrifice, JJA, who were older and more likely to be widowed, may have hesitated to be a burden on rather distant relatives or acculturated children. Alternatively, JJA, due to their relative isolation in America, may have preserved the Japanese value structure in place at the time of emigration while the norms of JJ continued to evolve over the past several decades. Furthermore, because of language barriers, JJA may feel incapable of participating in decisions and thus entrust their physicians as proxy decision makers. The attitudes and decision-making model of JJA show that physicians must not simply assume that such older Japanese-speaking Japanese Americans desire family or friends to make their decisions. Inquiry about the patient's wishes is essential.
Desire for disclosure of bad news dramatically increased with acculturation. Not only whether news should be disclosed but also how it should be disclosed differed greatly among cohorts. In contrast to EJA, nearly one quarter of JJA preferred nonverbal disclosure of a terminal prognosis, and among JJ about one third desired nonverbal disclosure and another third wanted information to be withheld from the patient altogether. These results illustrate the complexity in communicating with the dying patient of Japanese descent. Withholding information about a terminal diagnosis from a patient epitomizes Japanese end-of-life care.23–27,48–50 In addition, Japanese culture emphasizes “tacit agreement based on implicit communication (ishin-denshin)” with extensive use of nonverbal cues, such as silence, pauses between words, eye-contact, affective posture, and nuance and tone in communication about unrelated topics. This nonverbal communication is especially important in end-of-life care for Japanese.20,26,28 It is critical for physicians to recognize that culturally competent interaction requires attention to the multidimensional aspects of communication.60
Our results suggest that disclosure preference changes with acculturation but that wide variability exists within groups. For example, a 70-year-old Japanese-speaking female patient with terminal cancer may expect nonverbal disclosure while her acculturated son desires explicit disclosure and her husband demands protective nondisclosure. If American physicians are unaware of preferences for nonverbal disclosure among less-acculturated Japanese Americans or fail to provide explicit information to more-acculturated Japanese Americans, then miscommunication may occur, perhaps leading to conflict across generations or within the family. Yet, it is impractical to expect U.S. physicians to decipher the acculturation level and subtle preferences of Japanese Americans and in turn employ cues and nuances in disclosure of bad news. In addition, as our results suggest, stereotyping from generation and language imperfectly predicts communication preferences. The value of recognizing the vast cultural variation in disclosure and decision making lies in the chance to query these preferences before bad news must be revealed and before decisions are imminent. Prospectively asking patients in an open-ended, nonthreatening way (with translation help from a non–family member, if needed) can direct later physician communication. For instance, a physician (and translator) might approach a patient when family is not present and prior to a scheduled biopsy to say: “Many patients want their family directly involved in their important medical care decisions. I noticed that you like to have your important medical information shared with your family and for them to help in making decisions. When there is important medical information and decisions to be made, should I first come to speak with you alone, or to only your family, or everyone together?” The physician might proceed to ask about disclosure of bad news in similar terms. This method retains respect for the patient (and the integrity of the clinician) while preserving the preferred cultural end-of-life care models.
We found acculturated Japanese Americans to be more willing to withdraw care and to have a more-positive attitude toward advance care planning. Our findings are consistent with previous anecdotal reports about Japanese attitudes toward death20,61 and Japanese physicians' attitudes toward continuing life-sustaining treatment.62 Unwillingness to withdraw care is a common attitude of many ethnic groups63–65; as demonstrated in our study, these attitudes may evolve with acculturation.
Although the group decision-making model was preserved, EJA had greater desire for autonomy in decision making and had more-positive attitudes toward advance care planning. For this more-acculturated group, physicians' promotion of advance care planning may facilitate end-of-life care. Because of the strong preference for a group decision-making model, however, current forms of advance directives may be inadequate. A family consensus–based approach66 to advance directive development and administration is needed for Japanese Americans and other group-oriented cultures.
Our study has several limitations. First, there may be measurement differences between the English language and the Japanese language questionnaires despite efforts to eliminate contextual differences. Second, the survey asks theoretical questions that may not elicit subjects' authentic preferences about end-of-life care. However, the expected relationships of attitudes with acculturation and age provide some predictive validity, and there is little reason to expect differential validity of responses across groups. Third, our samples are not representative of all Japanese Americans and Japanese. The EJA sample was derived from community centers in the greater Los Angeles area, where Japanese Americans are highly concentrated. These individuals may be less acculturated than Japanese Americans living outside the area or nonmembers. Our sampling strategy would be expected to reduce the differences seen between EJA and JJ. Furthermore, JJA mainly consist of individuals from earlier generations living in the Japanese enclave, Little Tokyo. They may be a special group of Japanese Americans who, in many ways, appear to hold attitudes more consistent with classical Japanese culture than do the JJ. This hypothesis requires further exploration. However, the glimpse into this group's perspective reveals attitudes that may produce conflicts with mainstream U.S. health care providers.
These limitations are not unexpected in a multinational study of cross-cultural attitudes toward end-of-life care. Our data reveal that acculturation does not cause a complete conversion to the western model of end-of-life attitudes. Instead, preferences and attitudes change incrementally and unevenly. In addition, individuals of the same heritage may retain a wide range of views. Our findings suggest that a 65-year-old male of Japanese descent presenting as a patient to a U.S. physician may be a Sansei (third generation) Japanese American, a Shin-issei (first generation) Japanese American living in the United States for 30 years, or a businessman recently arrived from Japan. Each would likely have different attitudes toward end-of-life care, yet retain a group decision-making model. A case-by-case approach enriched with an understanding of traditional Japanese values and the effects of acculturation can guide the interaction with patients of Japanese heritage. Individualized assessment and early discussion about preferences for decision making and disclosure will facilitate later communication and decisions.
Acknowledgments
The authors appreciate the collaboration of Takashi Makinodan, PhD, Nancy Harada, PhD, Robert Oye, MD, and Lisa Meredith, PhD. We thank the Japanese American Community Centers and social clubs for help in collecting the Japanese-American samples and Ichiro Takai, MD for help in collecting the samples in Japan. We also thank Martin Shapiro, MD for insightful critical review and input on this project.
This study was supported in part by a grant from the VA/UCLA/RAND Medical Treatment Effectiveness Program (MEDTEP) Center for Asians and Pacific Islanders that was funded by Agency for Health Care Policy Research (P50HS07370). Additional project support was provided by Pfizer Foundation Grants to Support Joint International Research Projects in Japan.
REFERENCES
- 1.President's Commission for the Study of Ethical Problems in Medicine and Biomedical Research. Deciding to Forgo Life-Sustaining Treatment: A Report On The Ethical, Medical and Legal Issues In Treatment Decisions. Washington, DC: U.S. Government Printing Office; 1983. [Google Scholar]
- 2.The Hastings Center. Guidelines on the Termination of Life-Sustaining Treatment and the Care of the Dying: A Report. Briarcliff Manor, NY: The Hastings Center; 1987. [Google Scholar]
- 3.Field MJ, Cassel CK, editors. Approaching Death: Improving Care at the End of Life. Washington, DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 4.Frankl D, Oye RK, Bellamy PE. Attitudes of hospitalized patients toward life support: a survey of 200 medical inpatients. Am J Med. 1989;86:645–8. [PubMed] [Google Scholar]
- 5.Emanuel LL, Barry MJ, Stoeckle JD, Ettelson LM, Emanuel EJ. Advance directives for medical care—a case for greater use. N Engl J Med. 1991;324:889–95. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- 6.Reilly BM, Wagner M, Magnussen CR, Ross J, Papa L, Ash J. Promoting inpatient directives about life-sustaining treatments in a community hospital: results of a 3-years time series intervention trial. Arch Intern Med. 1995;155:2317–23. [PubMed] [Google Scholar]
- 7.Broadwell AW, Boisaubin EV, Dunn JK, Engelhardt HT., Jr Advance directives on hospital admission: a survey of patient attitudes. South Med J. 1993;86:165–8. doi: 10.1097/00007611-199302000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Murphy ST, Palmer JM, Azen S, Frank G, Michel V, Blackhall LJ. Ethnicity and advance care directives. J Law Med Ethics. 1996;24:108–17. doi: 10.1111/j.1748-720x.1996.tb01843.x. [DOI] [PubMed] [Google Scholar]
- 9.Teno J, Fleishman J, Brock DW, Mor V. The use of formal prior directives among patients with HIV-related diseases. J Gen Intern Med. 1990;5:490–4. doi: 10.1007/BF02600877. [DOI] [PubMed] [Google Scholar]
- 10.McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. J Gen Intern Med. 1996;11:651–6. doi: 10.1007/BF02600155. [DOI] [PubMed] [Google Scholar]
- 11.Sehgal AR, Weisheit C, Miura Y, Butzlaff M, Kielstein R, Taguchi Y. Advance directives and withdrawal of dialysis in the United States, Germany, and Japan. JAMA. 1996;276:1652–6. [PubMed] [Google Scholar]
- 12.Blackhall LJ, Murphy ST, Frank G, Michel V, Azen S. Ethnicity and attitudes toward patient autonomy. JAMA. 1995;274:820–5. [PubMed] [Google Scholar]
- 13.Ersek M, Kagawa-Singer M, Barnes D, Blackhall L, Koenig BA. Multicultural considerations in the use of advance directives. Oncol Nurs Forum. 1998;25:1683–90. [PubMed] [Google Scholar]
- 14.Oppemheim A, Sprung CL. Cross-cultural ethical decision-making in critical care. Crit Care Med. 1998;26:423–4. doi: 10.1097/00003246-199803000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Orr RD, Marshall PA, Osborn J. Cross-cultural considerations in clinical ethics consultations. Arch Fam Med. 1995;4:159–64. doi: 10.1001/archfami.4.2.159. [DOI] [PubMed] [Google Scholar]
- 16.Klessig J. Cross-cultural medicine, a decade later: the effect of values and culture on life-support decisions. West J Med. 1992;157:316–22. [PMC free article] [PubMed] [Google Scholar]
- 17.Carrillo JE, Green AR, Betancourt JR. Cross-cultural primary care: a patient-based approach. Ann Intern Med. 1999;130:829–34. doi: 10.7326/0003-4819-130-10-199905180-00017. [DOI] [PubMed] [Google Scholar]
- 18.Spector RE. Cultural Diversity in Health and Illness. 4th Ed. Norwalk, Conn: Appleton and Lange; 1996. [DOI] [PubMed] [Google Scholar]
- 19.Ishiwata R, Sakai A. The physician-patient relationship and medical ethics in Japan. Camb Q Healthc Ethics. 1994;3:60–6. [PubMed] [Google Scholar]
- 20.Kimura R. Death and dying in Japan. Kennedy Inst Ethics J. 1996;6:374–8. doi: 10.1353/ken.1996.0038. [DOI] [PubMed] [Google Scholar]
- 21.Ohnuki-Tierney E. Illness and Culture in Contemporary Japan: An Anthropological View. New York: Cambridge University Press; 1992. [Google Scholar]
- 22.Lock M. Contesting the natural in Japan: moral dilemmas and technologies of dying. Cult Med Psychiatry. 1995;19:2–38. doi: 10.1007/BF01388247. [DOI] [PubMed] [Google Scholar]
- 23.Long SO, Long BD. Curable cancer and fatal ulcers. Attitude toward cancer in Japan. Soc Sci Med. 1982;16:2101–8. doi: 10.1016/0277-9536(82)90259-3. [DOI] [PubMed] [Google Scholar]
- 24.Tanida N. Japanese attitude towards truth disclosure in cancer. Scand J Soc Med. 1994;22:50–7. doi: 10.1177/140349489402200109. [DOI] [PubMed] [Google Scholar]
- 25.Uchitomi Y, Yamawaki S. Truth-telling practice in cancer care in Japan. Ann NY Acad Sci. 1997;809:290–9. doi: 10.1111/j.1749-6632.1997.tb48092.x. [DOI] [PubMed] [Google Scholar]
- 26.Elwyn TS, Fetters MD, Gorenflo DW, Tsuda T. Cancer disclosure in Japan: historical comparisons, current practices. Soc Sci Med. 1998;46:1151–63. doi: 10.1016/s0277-9536(97)10042-9. [DOI] [PubMed] [Google Scholar]
- 27.Akabayashi A, Fetters MD, Elwyn TS. Family consent, communication, and advance directives for cancer disclosure: a Japanese case and discussion. J Med Ethics. 1999;25:296–304. doi: 10.1136/jme.25.4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fetters MD. The family in medical decision making: Japanese perspectives. J Clin Ethics. 1998;9:132–46. [PubMed] [Google Scholar]
- 29.Asai A, Fukuhara S, Inosita O, Miura Y, Tanabe N, Kurokawa K. Medical decisions concerning the end of life: a discussion with Japanese physicians. J Med Ethics. 1997;23:323–7. doi: 10.1136/jme.23.5.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hoshino K, editor. Japanese and Western Bioethics: Studies in Moral Diversity. Dordrecht, Boston: Kluwer Academic Publishers; 1997. [Google Scholar]
- 31.Long SO. Living poorly or dying well: cultural decisions about life-supporting treatment for American and Japanese patients. J Clin Ethics. 2000;11:236–50. [PubMed] [Google Scholar]
- 32.Fetters MD, Masuda Y. Japanese patients' preferences for receiving cancer test results while in the United States: introducing an advance directive for cancer disclosure. J Pallit Med. 2000;3:361–74. doi: 10.1089/jpm.2000.3.361. [DOI] [PubMed] [Google Scholar]
- 33.Masuda Y, Fetters MD, Shimokata H, et al. Outcomes of written living wills in Japan: a survey of the deceased families. Bioethics Forum. 2001;17:41–52. [PubMed] [Google Scholar]
- 34.Kitano HH. Generation and Identity: The Japanese American. Needham Heights, Mass: Ginn Press; 1993. [Google Scholar]
- 35.Connor JW. Tradition and Change in Three Generations of Japanese Americans. Chicago: Nelson-Hall; 1977. [Google Scholar]
- 36.SUPPORT Principal investigators. A controlled trial to improve care for seriously ill hospitalized patients: the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. JAMA. 1995;274:1591–8. [PubMed] [Google Scholar]
- 37.Bito S, Matsumura S, Fukuhara S, Wenger NS. Acculturation and end-of-life decision making: focus group comparison of Japanese and Japanese-Americans. J Gen Intern Med. 1998;13(suppl 1):93. [Google Scholar]
- 38.Ware JE, Kosinski M, Keller SD. SF12: How to Score the SF-12 Physical and Mental Health Summary Scales. 2nd Ed. Boston, Mass: New England Medical Center, The Health Institute; 1995. [Google Scholar]
- 39.Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, Mass: New England Medical Center, The Health Institute; 1993. [Google Scholar]
- 40.Fukuhara S, Bito S, Green J, Hsiao A, Kurokawa K. Translation, adaptation, and validation of the SF36 Health Survey for use in Japan. J Clin Epidemiol. 1998;51:1037–44. doi: 10.1016/s0895-4356(98)00095-x. [DOI] [PubMed] [Google Scholar]
- 41.Ende J, Kazis L, Ash A, Moskowitz MA. Measuring patients' desire for autonomy: decision making and information-seeking preferences among medical patients. J Gen Intern Med. 1989;4:23–30. doi: 10.1007/BF02596485. [DOI] [PubMed] [Google Scholar]
- 42.Ohki M, Fukuhara S. Development and validation of the autonomy preference index for Japanese subjects. Japan Health Psychol. 1995;3:11–24. [Google Scholar]
- 43.OECD. Purchasing power parity. consumer price levels http://www.oecd.org/pdf/M00009000/M00009294.pdf 2001. Accessed May 16, 2002.
- 44.Suinn RM, Rickard-Figueroa K, Lew S, Vigil P. The Suinn-Lew Asian Self-Identity Acculturation Scale: an initial report. Edu Psychol Meas. 1987;47:401–7. [Google Scholar]
- 45.Suinn RM, Ahuna C, Khoo G. The Suinn-Lew Asian Self-Identity Acculturation Scale: concurrent and factorial validation. Edu Psychol Meas. 1992;52:1041–6. [Google Scholar]
- 46.Meredith LS, Wenger NS, Harada N, Liu HH, Kahn KL. Development of a brief scale to measure acculturation among Japanese Americans. J Comm Psych. 2000;28:103–13. [Google Scholar]
- 47.SAS Institute Inc. SAS/STAT User's Guide, Version 6. 4th Ed. Cary, NC: SAS Institute Inc; 1994. [Google Scholar]
- 48.Mitchell JL. Cross-cultural issues in the disclosure of cancer. Cancer Pract. 1998;6:153–60. doi: 10.1046/j.1523-5394.1998.006003153.x. [DOI] [PubMed] [Google Scholar]
- 49.Holland JC, Geary N, Marchini A, Tross S. An international survey of physician attitudes and practice in regard to revealing the diagnosis of cancer. Cancer Invest. 1987;5:151–4. doi: 10.3109/07357908709018468. [DOI] [PubMed] [Google Scholar]
- 50.Thomsen OØ, Wulff HR, Martin A, Singer PA. What do gastroenterologists in Europe tell cancer patients. Lancet. 1993;341:473–6. doi: 10.1016/0140-6736(93)90218-6. [DOI] [PubMed] [Google Scholar]
- 51.Braun KL. Death and dying in four Asian American cultures: a descriptive study. Death Stud. 1997;21:327–59. doi: 10.1080/074811897201877. [DOI] [PubMed] [Google Scholar]
- 52.Carrese JA, Rhodes LA. Western bioethics on the Navajo reservation: benefit or harm? JAMA. 1995;274:826–9. [PubMed] [Google Scholar]
- 53.Layson RT, Adelman HM, Wallach PM, Pfeifer MP, Johnston S, McNutt RA End-of-life Study Group. Discussion about the use of life-sustaining treatments: a literature review of physicians' and patients' attitudes and practices. J Clin Ethics. 1994;5:195–203. [PubMed] [Google Scholar]
- 54.Muller JH, Desmond B. Cross-cultural medicine. A decade later. Ethical dilemmas in a cross-cultural context. A Chinese Example. West J Med. 1992;157:323–7. [PMC free article] [PubMed] [Google Scholar]
- 55.Yeo G. Ethical considerations in Asian and Pacific Island elders. Clin Geriatr Med. 1995;11:139–52. [PubMed] [Google Scholar]
- 56.Miles SH, Koepp R, Weber EP. Advance end-of-life treatment planning: a research review. Arch Intern Med. 1996;156:1062–8. [PubMed] [Google Scholar]
- 57.Rothchild E. Family dynamics in end-of-life treatment decisions. Gen Hosp Psychiatry. 1994;16:251–8. doi: 10.1016/0163-8343(94)90004-3. [DOI] [PubMed] [Google Scholar]
- 58.Singer PA, Martin DK, Lavery JV, Thiel EC, Kelner M, Mendelssohn DC. Reconceptualizing advance care planning from the patient's perspective. Arch Intern Med. 1998;158:879–84. doi: 10.1001/archinte.158.8.879. [DOI] [PubMed] [Google Scholar]
- 59.Hines SC, Glover JJ, Holley JL, Babrow AS, Badzek LA, Moss AH. Dialysis patients' preferences for family-based advance care planning. Ann Intern Med. 1999;130:825–8. doi: 10.7326/0003-4819-130-10-199905180-00016. [DOI] [PubMed] [Google Scholar]
- 60.Kagawa-Singer M, Blackhall LJ. Negotiating cross-cultural issues at the end of life. JAMA. 2001;286:2993–3001. doi: 10.1001/jama.286.23.2993. [DOI] [PubMed] [Google Scholar]
- 61.Rothenberg LS, Merz JF, Wenger NS, et al. The relationship of clinical and legal perspectives regarding medical treatment decision-making in four cultures. Annu Rev Law Ethics. 1996;4:335–79. [Google Scholar]
- 62.Asai A, Fukuhara S, Lo B. Attitudes of Japanese and Japanese-American physicians towards life-sustaining treatment. Lancet. 1995;346:356–9. doi: 10.1016/s0140-6736(95)92230-x. [DOI] [PubMed] [Google Scholar]
- 63.Caralis PV, Davis B, Wright K, Marcial E. The influence of ethnicity and race on attitudes toward advance directives, life-prolonging treatments, and euthanasia. J Clin Ethics. 1993;4:155–65. [PubMed] [Google Scholar]
- 64.Frank G, Blackhall LJ, Michel V, Murphy ST, Azen SP, Park K. A discourse of relationships in bioethics: patient autonomy and end-of-life decision making among elderly Korean Americans. Med Anthropol Q. 1998;12:403–23. doi: 10.1525/maq.1998.12.4.403. [DOI] [PubMed] [Google Scholar]
- 65.Sprung CL, Eidelman LA. Worldwide similarities and differences in the forgoing of life-sustaining treatments. Intensive Care Med. 1996;22:1003–5. doi: 10.1007/BF01699218. [DOI] [PubMed] [Google Scholar]
- 66.Karlawish JHT, Quill T, Meier DE for the ACP-ASIM End-of-life Care Consensus Panel. A consensus-based approach to providing palliative care to patients who lack decision-making capacity. Ann Intern Med. 1999;130:835–40. doi: 10.7326/0003-4819-130-10-199905180-00018. [DOI] [PubMed] [Google Scholar]