Abstract
OBJECTIVE
To examine the effect of Spanish interpretation method on satisfaction with care.
DESIGN
Self-administered post-visit questionnaire.
SETTING
Urban, university-affiliated walk-in clinic.
PARTICIPANTS
Adult, English- and Spanish-speaking patients presenting for acute care of non-emergent medical problems.
MEASUREMENTS AND MAIN RESULTS
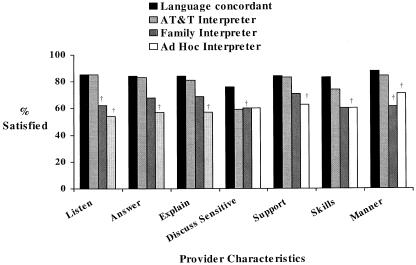
Satisfaction with overall clinic visit and with 7 provider characteristics was evaluated by multiple logistic regression, controlling for age, gender, ethnicity, education, insurance status, having a routine source of medical care, and baseline health. “Language-concordant” patients, defined as Spanish-speaking patients seen by Spanish-speaking providers and English-speaking patients, and patients using AT&T telephone interpreters reported identical overall visit satisfaction (77%; P = .57), while those using family or ad hoc interpreters were significantly less satisfied (54% and 49%; P < .01 and P = .007, respectively). AT&T interpreter use and language concordance also yielded similar satisfaction rates for provider characteristics (P > .2 for all values). Compared to language-concordant patients, patients who had family members interpret were less satisfied with provider listening (62% vs 85%; P = .003), discussion of sensitive issues (60% vs 76%; P = .02), and manner (62% vs 89%; P = .005). Patients who used ad hoc interpreters were less satisfied with provider skills (60% vs 83%; P = .02), manner (71% vs 89%; P = .02), listening (54% vs 85%; P = .002), explanations (57% vs 84%; P = .02), answers (57% vs 84%; P = .05), and support (63% vs 84%; P = .02).
CONCLUSIONS
Spanish-speaking patients using AT&T telephone interpretation are as satisfied with care as those seeing language-concordant providers, while patients using family or ad hoc interpreters are less satisfied. Clinics serving a large population of Spanish-speaking patients can enhance patient satisfaction by avoiding the use of untrained interpreters, such as family or ad hoc interpreters.
Keywords: patient satisfaction, Hispanic, language, communication, interpretation
According to the 1990 U.S. Census, 13 million adults living in the United States speak Spanish as their primary language. Over half of this group is limited English proficient.1 Because America's current health care system is geared toward English-speaking patients, delivering quality care to this large population with limited English skills has become an increasing challenge for the medical community.
There is also a legal obligation to provide for appropriate interpretation. Title VI of the Civil Rights Act prohibits discrimination by federally funded entities based on race, color, or national origin. Compliance is mandatory for all public and private entities that receive Department of Health and Human Services federal financial assistance. Title VI has been interpreted such that, to fully comply, covered entities must provide language assistance that results in accurate and effective communication at no cost to the patient.
The effectiveness of provided language assistance can, in part, be measured through patient satisfaction with the method used, since patient satisfaction is an important indicator of quality of care.2 Patient dissatisfaction has been linked to lower rates of compliance, more frequent “doctor-shopping,” and poorer health outcomes.3,4 Spanish-speaking patients have been found to be less satisfied with health care than English-speaking patients, with research suggesting that provider–patient communication difficulties may play a significant role.5,6 Additionally, several studies have demonstrated that language barriers may have a direct negative impact on patient care.7–10
Many strategies exist for improving communication with non–English speaking patients, including professional interpreters, interpretation through family or friends, ad hoc interpreters (i.e., bilingual employees such as clerks, custodial staff, or technicians), telephone interpretation services, and bilingual providers. However, none of these solutions is ideal. For instance, providing on-site professional interpreters in busy clinics may be expensive and lead to long delays in care, while using family, friends, or ad hoc interpreters compromises patient confidentiality and may result in interpretation errors. While bilingual providers might be optimal, the pool of potential providers is often not adequate. Telephone interpretation can aid in providing timely delivery of care, but Spanish-speaking patients may not prefer this method of communication.11 In response to these concerns, we undertook this study to determine the impact on patient satisfaction of different methods of Spanish interpretation.
Only 2 previous studies have examined which method of interpretation patients themselves find most satisfactory. In a study by Hornberger et al., new mothers presenting with their infants for a series of well-baby visits rated remote-simultaneous interpretation services, in which patients communicated with providers using special headsets linked to off-site trained interpreters, superior to in-person professional interpreters at the end of a 6-month study period.12 Using a previsit survey to assess primary care patients' prior experiences with Spanish interpretation, Kuo and Fagan found high satisfaction rates for use of both professional interpreters (92%) and family and friends (85%), but lower satisfaction with telephone interpretation (53%).11 No study to date has evaluated the effect of interpretation method on patient satisfaction with care immediately after a clinic visit, when problems with recall bias are minimized.
The goal of this study was to compare satisfaction with care among patients communicating with providers in their primary language versus patients using (i) telephone interpretation, (ii) untrained interpreters such as family members, or (iii) ad hoc interpreters. We hypothesized that language concordance between patient and provider would yield the greatest satisfaction, while interpretation through family members or friends would result in slightly higher satisfaction than use of a telephone language line.
METHODS
Study Setting
This study was conducted at the Walk-in Clinic (WIC) at Denver Health Medical Center, the urgent care clinic of a university-affiliated public hospital that serves the adult indigent patients of Denver, Colorado. Patients seen in the WIC present directly for care or are referred from the Emergency Department or one of the hospital's community clinics. More than 3,000 patients are seen annually, the majority of whom are uninsured, low-income minority individuals. Hispanics account for over 50% of the patient population, and slightly over 20% of all patients are able to communicate adequately only in Spanish. Within the clinic, patients are seen by Internal Medicine attending physicians who also supervise care provided to patients by residents at various stages of training in Obstetrics/Gynecology, Internal Medicine, and Family Practice, and nurse practitioners. There is no attempt made to triage certain patient complaints to certain providers.
Study Patients
Patients were eligible for the study if they were 18 years of age or older, spoke English or Spanish, and did not have an emergent medical condition requiring immediate evaluation by a health provider.
Methods of Interpretation
Patients are provided interpretation services based on their implied preference. When the patient's provider is not fluent in Spanish, the majority of interpretation is done through the AT&T language line. AT&T telephone interpreters are requested by the provider through the Denver Health Medical Center operator and are accessed via speakerphones present in every exam room. AT&T interpreters function in the same capacity as professional interpreters but are not physically present during the clinic encounter. If a patient prefers to have a family member or friend interpret and the interpretation appears adequate to the provider, then this method is utilized. In addition, ad hoc interpreters, which include support staff such as nurses, clerks, and technicians who are bilingual but not formally trained as interpreters, are occasionally used. During the course of the study there was no change in the overall use of AT&T language line services in either direction, as measured by the total cost of telephone interpreter services per month corrected for patient volume.
Patient Recruitment
Patients were enrolled for this study during a 4-month period from July to October 2000. Questionnaires were placed on the charts of all monolingual Spanish-speaking patients and every fifth English-speaking patient during the triage process. The patient's language was determined by the triage technicians at the WIC. Patients were considered Spanish-speaking if they initiated the conversation in Spanish and were only able to communicate adequately regarding their medical problem in Spanish. At the conclusion of the clinic visit, the provider or medical assistant handed the patient the questionnaire, asking him or her to complete it and leave it in the exam room or in a box at the front of the clinic. Use of a proxy such as a patient's family member to aid in filling out the survey was allowed. The study and survey tool were approved by the Colorado Multiple Institutional Review Board.
Survey Instrument
The survey tool was developed from previously published questionnaires.11,13,14 The survey was anonymous and did not contain any patient identifying information. Information was collected on patient demographic characteristics (age, gender, ethnicity, insurance status, education level, and presence or absence of a regular source of medical care) and current health status (SF-12), concordance between patient and provider language, method of interpretation, and satisfaction with the clinic visit. Satisfaction questions assessed provider communication and medical skills and overall visit satisfaction. A 5-point Likert scale ranging from poor to excellent was used to rate patient satisfaction. The Spanish language version of this questionnaire was developed through direct translation and reviewed for content by a native Spanish speaker who has experience in translating surveys. The study instrument is available from the authors upon request.
Statistical Analysis
Patients were grouped by language concordance and method of interpretation. The “language-concordant” group included Spanish-speaking patients seen by Spanish-speaking providers and English-speaking patients. The “language-discordant” group comprised all other Spanish-speaking patients utilizing 1 of 3 interpretation methods: AT&T telephone language line (speakerphones), family interpreters, or ad hoc interpreters. Differences in demographic characteristics and health status between the language-concordant and language-discordant patients were examined using χ2 analysis.
Satisfaction scores were initially analyzed as continuous variables and then were dichotomized on the basis of the distribution of responses, so that patients were considered “satisfied” if they rated their satisfaction as excellent or very good. Post hoc analysis was also conducted evaluating satisfaction as a continuous variable, comparing mean satisfaction scores across study groups. The association between different methods of interpretation and satisfaction was evaluated by multiple logistic regression. To control for potentially confounding variables, age (18–25 years, 26–40 years, or >40 years), gender, ethnicity (Hispanic or non-Hispanic), education (greater than high school or completed high school or less), insurance status, having a routine source of medical care, and baseline health (excellent and very good or good, fair, and poor) were included in all multivariate models.
The designed study sample size was sufficient to detect a 20% difference in the primary outcome, percent satisfied, between language-concordant patients and language-discordant patients in each of the interpretation method groups, assuming a 2-tailed α = 0.05 and power = 80%.
RESULTS
Patient Characteristics
A total of 233 English-speaking patients and 303 Spanish-speaking patients agreed to participate in the study and completed questionnaires. Forty-two percent (n = 128) of Spanish-speaking respondents were seen by language-concordant providers, while the remainder received interpretation through AT&T telephone interpreters (19%; n = 59), family members (23%; n = 69), or ad hoc interpreters (16%; n = 47). Language-concordant patients and language-discordant patients did not differ in age, gender, insurance status, or education level (Table 1). Compared with language-concordant respondents, language-discordant respondents were more likely to be Hispanic (95% vs 59%; P < .0001) and were less likely to have a routine source of medical care (49% vs 62%; P < .01) or describe their health as “excellent or very good” (15% vs 34%; P < .0001).
Table 1.
Patient Characteristics by Language Concordance
| Characteristic | Language Concordant† (n = 361) | Language Discordant (n = 175) | P Value* |
|---|---|---|---|
| Median age, y (range) | 32 (18–88) | 32 (18–83) | NS |
| Female, % | 66 | 63 | NS |
| Hispanic, % | 59 | 95 | <.0001 |
| Insurance status, % | |||
| None | 72 | 76 | NS |
| Private, Medicaid, Medicare | 28 | 24 | |
| Education, % | |||
| High school or less | 61 | 69 | NS |
| More than high school | 39 | 31 | |
| Routine source of care, % | 62 | 49 | <.01 |
| Excellent or very good health status, % | 34 | 15 | <.0001 |
NS indicates not significant.
Language-concordant patients included 233 English-speaking patients and 128 Spanish-speaking patients.
Overall Visit Satisfaction
Seventy-seven percent (n = 264) of language-concordant respondents were satisfied with their overall clinic visit. English-speaking patients and Spanish-speaking patients seen by Spanish-speaking providers did not differ in their reported rates of satisfaction. Among language-discordant respondents, use of AT&T interpreters was associated with the greatest satisfaction, followed by family interpreters and ad hoc interpreters. The proportion of patients utilizing AT&T interpreters who were satisfied with their clinic visit was identical to that of language-concordant respondents (77%; n = 44). However, only 54% (n = 35) of patients using family interpreters and fewer than half (49%; n = 18) of those using ad hoc interpreters were satisfied with their visit overall. In a multivariate analysis controlling for possible confounding variables, patients receiving interpretation though family interpreters or ad hoc interpreters were significantly less satisfied than language-concordant patients (54% and 49% vs 77%; P < .01 and P = .007, respectively).
Several covariates were found to be significantly associated with higher overall visit satisfaction. These included age >40 years (odds ratio [OR] 2.17; 95% confidence interval [CI], 1.09 to 4.35), excellent or very good baseline health status (OR 3.72; 95% CI, 1.81 to 7.65), and lack of medical insurance (OR 2.19; 95% CI, 1.26 to 3.82). Gender, education level, race, and having a regular source of medical care were not independent predictors of satisfaction.
Satisfaction with Provider Characteristics
Satisfaction with 7 provider characteristics (listening, answers, explanations, support, discussion of sensitive issues, skills, and manner) was evaluated. Language-concordant respondents and those using AT&T telephone interpreters did not differ significantly in satisfaction rates for any of the characteristics (Fig. 1), and these results did not differ when satisfaction was considered as a continuous variable. Compared to language-concordant respondents, patients who had family interpreters were less satisfied with all 7 of the provider characteristics evaluated (Fig. 1), and the results did not differ when satisfaction was considered as a continuous variable. However, only differences in satisfaction with provider listening (62% vs 85%; P = .003), discussion of sensitive issues (60% vs 76%; P = .02), and manner (62% vs 89%; P = .005) attained statistical significance in the multivariate analysis. Patients who utilized ad hoc interpreters also reported lower satisfaction with each provider characteristic (Fig. 1). Differences in satisfaction were statistically significant for provider listening (54% vs 85%; P = .002), answers (57% vs 84%; P = .05), explanations (57% vs 84%; P = .02), support (63% vs 84%; P = .02), skills (60% vs 83%; P = .02), and manner (71% vs 89%; P = .02). When satisfaction was considered as a continuous variable, the results were unchanged except for “manner,” which did not retain a statistically significant difference from language-concordant (P = .1220). The only other factor consistently associated with higher satisfaction with all provider characteristics was excellent or very good health status (OR range 2.12 to 5.88; CI range 1.04 to 14.97). Results did not differ when satisfaction was evaluated as a continuous rather than dichotomous variable.
FIGURE 1.
Satisfaction with provider characteristics evaluated by multiple logistic regression, controlling for age, gender, ethnicity, education, insurance status, having a routine source of medical care, and baseline health. No significant differences were seen between the language-concordant group and the AT&T interpreter group (P > .05 for all comparisons), but the language-concordant group was more satisfied than the family and ad hoc interpreter groups. †Indicates P ≤ .05.
DISCUSSION
In this study, we sought to determine the effect of language concordance and method of interpretation on patient satisfaction with overall clinic visit and with various provider characteristics. Four routes of communication were assessed: provider-patient language concordance, AT&T telephone interpretation, interpretation through family members, and interpretation through ad hoc interpreters.
Patients utilizing AT&T interpreters reported overall visit satisfaction identical to that of language-concordant patients, while those employing family or ad hoc interpreters were less satisfied. These differences were significant even after controlling for potentially confounding variables. Use of AT&T interpreters and language concordance were associated with comparable rates of satisfaction for all 7 of the provider characteristics evaluated; multivariate analysis did not reveal any significant differences between the two groups. Language-concordant patients tended to be more satisfied with each of the provider characteristics than either the family or other interpretation groups, but not all findings reached statistical significance. For patients receiving interpretation through family members, satisfaction was significantly less for provider listening, discussion of sensitive issues, and manner. Patients employing ad hoc interpreters were significantly less likely to be satisfied with provider listening, answers, explanations, support, skills, and manner.
Our findings confirm the association between language barriers and patient satisfaction established in prior research. In a study of emergency department patients, Carrasquillo et al. showed that non–English speaking patients were less satisfied, less likely to return to the same emergency department, and more likely to report problems with care, communication, and testing compared to English speakers.6 Morales et al. showed that Spanish-speaking Latino patients were more dissatisfied than English-speaking Latinos or non-Latino whites with medical staff listening, answering questions, providing support, and explaining medicines, procedures, and test results.5 Baker et al. found that Spanish-speaking patients who felt an interpreter was needed but was not used rated their providers as less friendly, less concerned for them as a person, and less likely to make them feel comfortable.15 Given the previously demonstrated link between dissatisfaction with care and poorer health outcomes, these findings suggest that Spanish-speaking patients not provided with an adequate means of communication with their health provider may be at particular risk.3,4 Our results indicate that language barriers can be overcome and patient satisfaction enhanced through the use of bilingual providers and adequate interpretation services.
While it would be ideal to have all patients without English proficiency see providers who spoke their native tongue, language-concordant providers are not always available. For instance, our walk-in clinic serves a large population of monolingual Spanish speakers, but only 1 out of every 5 providers can speak Spanish. In situations in which other means of communication must be employed, our study suggests that telephone interpreters may be equally effective at providing high levels of satisfactory care. In contrast, using untrained interpreters such as family or ad hoc interpreters seems to be a less acceptable way of overcoming language barriers. Proficiency of such untrained interpreters in both English and Spanish, particularly with respect to use of medical terminology, is not ensured. In addition, confidentiality issues may exist, especially when using family members.
The results of our study contrast with those of the only previous study to examine satisfaction with bilingual providers, as well as trained and untrained interpreters, among Spanish-speaking patients. Using a previsit questionnaire distributed at a primary care clinic, Kuo and Fagan asked patients to rate their past experiences with language interpretation and found the highest level of satisfaction for professional interpreters, followed by family/friend interpreters, language-concordant providers, telephone interpreters, and ad hoc interpreters.11 Several possible explanations may account for the differences in our study findings. Patients seen at an acute care clinic may have expectations regarding the role of family members in patient-provider interactions that are different from those of patients seen at a continuity clinic. Variations in provider ability to speak Spanish and mechanics of telephone interpreter use (i.e., having speakerphones available versus passing a handset back and forth) may also have existed. Assessing interpretation services after a specific clinic visit as opposed to evaluating past experiences may have led to differences in satisfaction ratings. Finally, employing a survey instrument different from that used by Kuo and Fagan may have had an impact on our study results.
The high level of satisfaction with telephone interpreters seen in our study indicates that the physical presence of a trained interpreter in the exam room may not be necessary to provide satisfactory interpretation services. This finding is consistent with the results of Hornberger et al., in which mothers at well-baby clinic visits rated remote-simultaneous interpretation superior to in-room professional interpreters.12
There are several limitations to our study. We did not examine satisfaction with professional interpreters because they were not readily available as a mode of interpretation at the time of our data collection. Furthermore, the method of interpretation used was not randomized and was determined by patient self-report. The Spanish version of our survey was not back translated from Spanish into English or tested or validated in Spanish, which may have resulted in less than optimal translation and limited its validity in our patient population. Because we evaluated walk-in clinic patients seeking care for presumably urgent needs, our findings may not be generalizable to other practice settings such as primary care, subspecialty, or surgical clinics. Data on the number of nonparticipants and how they might have differed from our study population was unavailable, but two spot checks done during the first and last month of the study showed that about half of the distributed surveys were completed and returned. We did not control for provider age, gender, level of training, specialty, or Spanish language aptitude, all of which might have influenced patient satisfaction. Because the surveys were done anonymously, we could not control for certain covariates, such as reason for and acuity of the clinic visit, that might be related to both the choice of interpretation method and satisfaction outcome. In addition, no provider-level information was collected during the survey process, so it was not possible to control for the concordance of gender and ethnicity between patient and provider. A prior study on patient satisfaction in both English- and Spanish-speaking patients did find that female gender was positively associated with patient satisfaction in women, but not men.16 Also, we did not restrict the use of proxies to assist patients in filling out the survey, and information on whether this occurred was not collected. Finally, placing surveys on patient charts prior to the patients being seen might have led to bias in how these patients were treated by their providers. However, we would have expected this to be consistent across both language-concordant and language-discordant patient-provider pairs.
Dealing with language barriers that may impact satisfaction among patients with limited English proficiency remains an increasing struggle in the medical community. It remains a challenge because of the need to provide quality care for patients, as well as to comply with Title VI. Our study suggests that bilingual providers and telephone interpreters enhance patient satisfaction compared to untrained interpreters. Further research examining satisfaction with professional interpreters versus telephone interpreters and comparing the cost per encounter for each method will help to further elucidate how best to serve this growing population of patients.
Acknowledgments
This research was funded by the Division of General Internal Medicine, University of Colorado Health Sciences Center.
REFERENCES
- 1.Statistical Abstract of the United States 1999. 117 ed. Washington, DC: US Bureau of the Census; 1999. [Google Scholar]
- 2.Blumenthal D. Part 1: Quality of care—what is it? N Engl J Med. 1996;335:891–4. doi: 10.1056/NEJM199609193351213. [DOI] [PubMed] [Google Scholar]
- 3.Harris LE, Luft FC, Rudy DW, Tierney WM. Correlates of health care satisfaction in inner-city patients with hypertension and chronic renal insufficiency. Soc Sci Med. 1995;41:1639–45. doi: 10.1016/0277-9536(95)00073-g. [DOI] [PubMed] [Google Scholar]
- 4.Rubin HR, Gandek B, Rogers WH, Kosinski M, McHorney CA, Ware JE., Jr Patients' ratings of outpatient visits in different practice settings. Results from the Medical Outcomes Study. JAMA. 1993;270:835–40. [PubMed] [Google Scholar]
- 5.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers. J Gen Intern Med. 1999;14:409–17. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carrasquillo O, Orav EJ, Brennan TA, Burstin HR. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–7. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 7.Manson A. Language concordance as a determinant of patient compliance and emergency room use in patients with asthma. Med Care. 1988;26:1119–28. doi: 10.1097/00005650-198812000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Perez-Stable EJ, Napoles-Springer A, Miramontes JM. The effects of ethnicity and language on medical outcomes of patients with hypertension or diabetes. Med Care. 1997;35:1212–9. doi: 10.1097/00005650-199712000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269:1537–9. [PubMed] [Google Scholar]
- 10.Crane JA. Patient comprehension of doctor-patient communication on discharge from the emergency department. J Emerg Med. 1997;15:1–7. doi: 10.1016/s0736-4679(96)00261-2. [DOI] [PubMed] [Google Scholar]
- 11.Kuo D, Fagan MJ. Satisfaction with methods of Spanish interpretation in an ambulatory care clinic. J Gen Intern Med. 1999;14:547–50. doi: 10.1046/j.1525-1497.1999.07258.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hornberger JC, Gibson CD, Jr, Wood W, et al. Eliminating language barriers for non-English speaking patients. Med Care. 1996;34:845–56. doi: 10.1097/00005650-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Froehlich GW, Welch HG. Meeting walk-in patients' expectations for testing. Effects on satisfaction. J Gen Intern Med. 1996;11:470–4. doi: 10.1007/BF02599041. [DOI] [PubMed] [Google Scholar]
- 14.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–33. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Baker DW, Hayes R, Fortier JP. Interpreter use and satisfaction with interpersonal aspects of care for Spanish-speaking patients. Med Care. 1998;36:1461–70. doi: 10.1097/00005650-199810000-00004. [DOI] [PubMed] [Google Scholar]
- 16.Derose KP, Hays RD, McCaffrey DF, Baker DW. Does physician gender affect satisfaction of men and women visiting the emergency department. J Gen Intern Med. 2001;16:218–26. doi: 10.1046/j.1525-1497.2001.016004218.x. [DOI] [PMC free article] [PubMed] [Google Scholar]