Abstract
OBJECTIVES
To examine regional variation in health care utilization and outcomes during acute and chronic care of veterans following acute myocardial infarction (AMI), identifying potentially modifiable variables and processes of care that influence patient outcomes.
METHODS
Using national VA databases, we identified all veterans hospitalized at any VA Medical Center (VAMC) for AMI between October 1990 and September 1997. Demographic, inpatient, outpatient, mortality, and readmission data were extracted for 4 regions: Northeast, South, Midwest and West. Multivariable Cox proportional hazards regression models, controlled for comorbidity, were used to assess predictors of time to death and readmission.
RESULTS
We identified 67,889 patients with AMI. Patient demographic characteristics by region were similar. Patients in the Northeast had more comorbid conditions and longer lengths of stay during the index AMI hospitalization. Region of the country independently predicted time to death, with lower risk of death in the Northeast (hazard ratio [HR] = 0.875; 95% confidence interval [95% CI], 0.834 to 0.918; P < .0001) and West (HR = 0.856; 95%CI, 0.818 to 0.895; P = .0001) than in the South. Patients in the Northeast and West also had more cardiology or primary care follow-up within 60 days and at 1 year post-discharge than patients in the South and Midwest. Outpatient follow-up accounted for a significant portion of the variation in all-cause mortality.
CONCLUSION
Substantial geographic variation exists in subsequent clinical care and outcomes among veterans hospitalized in VAMCs for AMIs. Outpatient follow-up was highly variable and associated with decreased mortality. Further studies are needed to explore the causes of regional variation in processes of care and to determine the most effective strategies for improving outcomes after AMI.
Keywords: AMI, geographic variation, VA, mortality, readmission
The American Heart Association estimates that 1.1 million Americans suffer from acute myocardial infarction (AMI) each year, accounting for more than 2 million hospital admissions annually.1 About one third of these patients die within 1 year of their AMI, making it the leading cause of mortality and morbidity in the United States.2,3 The cost of cardiovascular disease annually exceeds $250 billion, and most is associated with AMI.1,4
Veterans are at increased risk for AMI, given their higher prevalence of multiple coronary risk factors. Studies conducted in the VA suggest that age, race, comorbid illnesses, availability of cardiac surgical services, and type of health insurance all play a role in determining interventions and outcomes during hospitalization for AMI.5–10 However, few data are available on the regional variation in health care utilization and outcomes following discharge after AMI in VA Medical Centers (VAMCs), which comprise the largest health care system in the United States. We capitalized on the VA's extensive data system11 to: (1) examine regional variation in mortality and health care utilization (both inpatient and outpatient) among veterans admitted to a VAMC for their index AMI and (2) determine predictors of subsequent mortality, readmission and health care utilization. These analyses may identify processes that could be improved to reduce morbid outcomes following AMI.
METHODS
Patient Study Cohort
We identified all veterans discharged from any VAMC with AMI (defined as having the International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] code 410 listed as the first discharge diagnosis) between October 1990 and September 1997. This strategy has at least 90% positive predictive value for identifying cases of AMI.12 We restricted our time frame to these years because major changes in AMI management such as the use of thrombolytics and acute coronary intervention teams occurred after October 1, 1990. For veterans with more than 1 admission with an eligible ICD-9-CM code during the study period, the first admission was considered the index admission. When patients were discharged and readmitted the same day, we assumed that this represented a transfer (a relatively common practice in the VA) and considered these events as part of a single hospitalization. Our eligibility criteria were similar to those utilized in a previously published study.13 We excluded patients whose length of stay during the index admission exceeded one year. These patients are typically in either VA long-term care or mental health units, and thus would have different post-myocardial infarction utilization. All patients were followed up for at least 1 year.
Data Sources, Patient Characteristics, and Outcome Measures
We extracted data from the centralized VA administrative data center in Austin, Texas. Once the patient cohort was assembled, we extracted data from the patient treatment file (PTF) regarding VA inpatient utilization throughout the index hospitalization. There is high agreement between PTF data and data extracted from patients' paper medical charts.14 We extracted the following variables as potentially predictive of regional variation in care and outcomes of myocardial infarction: patient age at the time of the index hospitalization, race (white, African American, other), comorbid conditions, discharge destination, year of index admission, and geographic region of the primary admitting hospital. Each hospitalization record in the PTF contains up to 10 discharge diagnosis codes. We used the discharge diagnoses codes 2 through 10 from the index admission to identify cardiac risk factors and to construct the Charlson Index, a well-validated comorbidity index that is predictive of subsequent mortality.15,16 Neither severity of the patient's AMI nor medications were available in the PTF. Regions of the country (Northeast, South, Midwest, West) were based on the 22 geographical locations of the hospital.17 We excluded VAMCs outside of the continental United States. All readmissions and readmission due to cardiac causes (AMI, angina, and congestive heart failure) to any VAMC were assessed at 60 days and 1 year following discharge from the index hospitalization.
For outpatient services, we extracted utilization data from the VA's outpatient clinic file, identifying visits to VA primary care medicine clinics, cardiology clinics, emergency units, and cardiac surgery clinics. No information was available for outpatient or inpatient utilization outside of the VA system (for which the VA is not financially responsible). We also extracted data concerning diagnostic tests and procedures, starting with the date of discharge and ending September 30, 1997. We identified the utilization of 4 major cardiac procedures if they occurred during or after the index admission for AMI: cardiac catheterization, coronary artery bypass grafting (CABG), percutaneous transluminal coronary angioplasty (PTCA), and other cardiac procedures and surgeries (pacemaker, implantable defibrillators, etc). Cardiac stenting was not identified as a separate procedure but was included under PTCA.
We used the Beneficiary Information and Resource Locator (BIRLS)18,19 to determine whether a date of death existed. BIRLS contains the date of death but not the cause of death. Hence, we assessed all-cause mortality and were unable to perform subanalyses for deaths due to cardiovascular causes.
Statistical Analysis
We compared patients' demographic and clinical characteristics between the 4 geographic regions using analysis of variance for continuous variables and χ2 tests for categorical variables. For analyses of outpatient utilization, we assessed whether primary care and/or cardiology outpatient follow-up occurred between discharge from the index AMI hospitalization and 60 days and 1 year later. Similarly, for cardiac procedures, we examined whether any cardiac procedures were performed during the index AMI hospitalization, within 60 days of discharge, and 1 year after discharge.
We employed multivariable logistic regression models to examine the effects of baseline and clinical characteristics on mortality within 60 days of the index admission. Predictors examined were: age, gender, race (white versus all others), comorbid diagnoses, number of discharge diagnoses, Charlson Index, cardiac procedures performed at the index admission, and geographic region (with South as the reference region).
We used Cox proportional hazards models to analyze time to death and time to readmission (all-cause and for cardiovascular problems). For these analyses, outpatient utilization and cardiac procedures performed within 60 days of the index hospitalization could be considered part of the index hospitalization. To avoid those biases, these analyses excluded deaths and hospitalizations that occurred within 60 days after the index hospitalization. Time to death was therefore analyzed only for those patients who survived more than 60 days. Similarly, we assessed hospital readmissions by excluding all hospitalizations that occurred within 60 days after discharge from the index hospitalization.
RESULTS
Baseline Characteristics
We identified 67,889 patients who were hospitalized in VAMCs for AMI between 1990 and 1997. Baseline demographic and clinical characteristics are represented in Table 1. As shown in Table 1, patients in this cohort were predominantly white (83.8%) and male (98.6%) with a mean age of 65 years. At discharge from the index hospitalization, the cohort had a mean of 5.6 discharge diagnoses. Ten percent of patients did not survive the index hospitalization while nearly 70% were discharged home. Diabetes and atrial fibrillation were more prevalent among patients in the Northeast while hyperlipidemia was more prevalent in the Midwest and West. Length of stay for AMI was longest in the Northeast and shortest in the West. Charlson Index scores were highest in the Northeast and lowest in the South. All-cause mortality during the index hospitalization was higher in the Northeast and South and lowest in the West. The percentage of patients receiving procedural interventions (CABG and PTCA) at the index admission was significantly different among the 4 regions, with more CABG performed in the West. More patients in the Northeast and Midwest were discharged to nursing homes. Importantly, fewer than 5% of the patients changed regions following their index hospitalization.
Table 1.
Baseline Demographic and Clinical Characteristics*
| Region | |||||
|---|---|---|---|---|---|
| NE | S | MW | W | Total | |
| Number of patients | 9,305 | 30,303 | 15,631 | 12,650 | 67,889 |
| Region of country, % | 13.7 | 44.6 | 23.0 | 18.6 | |
| Mean age, ±SD | 66.8 ± 10.6 | 64.5 ± 10.9 | 65.0 ± 10.8 | 64.8 ± 11 | 65.0 ± 10.9 |
| Gender, % male | 98.5 | 98.7 | 98.8 | 98.2 | 98.6 |
| Ethnicity, % white | 85.0 | 81.5 | 86.4 | 85.5 | 83.8 |
| Comorbid conditions, % | |||||
| Hypertension | 46.1 | 45.5 | 45.1 | 40.5 | 44.6 |
| Diabetes | 30.3 | 24.2 | 27.9 | 25.6 | 26.2 |
| Congestive heart failure | 24.9 | 20.2 | 22.2 | 22.5 | 21.7 |
| Hyperlipidemia | 13.1 | 13.3 | 16.0 | 16.6 | 14.5 |
| Atrial fibrillation | 10.5 | 8.3 | 8.8 | 9.8 | 9.0 |
| COPD | 19.4 | 18.8 | 21.4 | 18.3 | 19.4 |
| Stroke† | 1.1 | 1.1 | 1.1 | 1.0 | 1.1 |
| Mean number of discharge diagnoses at index hospitalization, ±SD | 5.9 ± 2.6 | 5.5 ± 2.5 | 5.7 ± 2.6 | 5.6 ± 2.5 | 5.6 ± 2.6 |
| Median length of index admission, days, mean ±SD | 13.8 ± 18.6 | 11.5 ± 13.0 | 11.0 ± 13.2 | 9.9 ± 10.7 | 11.4 ± 13.6 |
| Charlson Index, % | 2.6 ± 1.8 | 2.3 ± 1.7 | 2.4 ± 1.7 | 2.4 ± 1.7 | 2.4 ± 1.7 |
| 0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| 1 | 30.0 | 37.1 | 33.6 | 36.6 | 35.2 |
| 2 | 30.3 | 30.0 | 30.3 | 29.7 | 30.1 |
| >2 | 39.7 | 32.9 | 36.2 | 33.7 | 34.7 |
| Disposition at discharge from the index hospitalization, % | |||||
| Discharged home | 65.7 | 72.0 | 66.0 | 71.2 | 69.6 |
| Transfer to another hospital | 16.5 | 12.1 | 18.3 | 13.8 | 14.5 |
| Died | 10.7 | 10.9 | 9.7 | 9.0 | 10.3 |
| Nursing home | 3.4 | 2.3 | 3.5 | 3.2 | 2.9 |
| Other | 3.6 | 2.7 | 2.4 | 2.7 | 2.7 |
| Patients with procedures at index admission (%) | |||||
| Catheterization† | 25.9 | 27.0 | 26.7 | 26.4 | 26.7 |
| CABG | 11.4 | 10.8 | 10.5 | 12.8 | 11.2 |
| PTCA | 8.3 | 9.1 | 9.3 | 8.4 | 8.9 |
| CABG or PTCA | 18.3 | 18.7 | 18.3 | 19.8 | 18.7 |
P = .001 for comparisons between regions except where indicated.
P > .05 for comparisons between regions.
NE, Northeast; S, South; MW, Midwest; W, West; COPD, chronic obstructive pulmonary disease; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty.
Health Care Utilization
Inpatient and outpatient utilization for patients surviving the index admission is presented in Table 2. About 77% of the AMI patients in this cohort either died or had at least 1 readmission to a VAMC in the year following discharge from the index hospitalization. The proportion of patients undergoing cardiac procedures (mainly CABG) within 60 days and by 1 year following discharge from their index AMI hospitalization differed across regions. Patients in the Northeast and West received more post-discharge outpatient follow-up at a VAMC within 60 days and within 1 year following their index hospitalization compared to other regions. Outpatient follow-up was lowest at both 60 days and 1 year among patients in the South and Midwest: two thirds of patients in the South and the Midwest did not have any follow-up at a VAMC within 60 days following a discharge from the index hospitalization for AMI.
Table 2.
Inpatient and Outpatient Utilization After Index Admission*
| Region | |||||
|---|---|---|---|---|---|
| NE | S | MW | W | Total | |
| Patients surviving index admission | 7,968 | 26,184 | 13,742 | 11,167 | 59,061 |
| Outpatient utilization | |||||
| Patients with clinic visit within 60 days, % | |||||
| Cardiology and/or General Medicine | 38.4 | 33.1 | 32.6 | 45.7 | 36.1 |
| Both | 6.8 | 4.4 | 4.5 | 8.0 | 5.4 |
| Cardiology | 13.5 | 12.0 | 11.0 | 13.5 | 12.2 |
| General Medicine | 18.2 | 16.7 | 17.2 | 24.2 | 18.4 |
| Neither | 61.6 | 66.9 | 67.4 | 54.3 | 63.9 |
| Patients with clinic visit within 365 days, % | |||||
| Cardiology and/or General Medicine | 67.4 | 62.5 | 62.4 | 72.8 | 65.1 |
| Both | 27.3 | 21.7 | 20.4 | 28.9 | 23.5 |
| Cardiology | 14.9 | 16.1 | 14.2 | 12.9 | 14.9 |
| General Medicine | 25.2 | 24.7 | 27.8 | 31.0 | 26.7 |
| Neither | 32.6 | 37.5 | 37.6 | 27.2 | 34.9 |
| Inpatient utilization | |||||
| Patients with procedure within 60 days, % | |||||
| Cardiac catheterization† | 7.5 | 7.5 | 6.9 | 7.6 | 7.4 |
| CABG | 3.3 | 4.2 | 4.1 | 4.4 | 4.1 |
| PTCA | 2.7 | 2.8 | 2.7 | 2.9 | 2.8 |
| CABG or PTCA | 5.9 | 6.9 | 6.7 | 7.2 | 6.8 |
| Other cardiac procedures† | 7.3 | 7.3 | 7.6 | 7.8 | 7.5 |
| Patients with procedure within 365 days, % | |||||
| Cardiac catheterization | 13.7 | 16.2 | 14.4 | 15.4 | 15.3 |
| CABG | 5.9 | 7.1 | 6.3 | 7.7 | 6.8 |
| PTCA | 4.4 | 5.5 | 5.0 | 5.1 | 5.2 |
| CABG or PTCA | 9.8 | 12.1 | 10.8 | 12.4 | 11.5 |
| Other cardiac procedures† | 13.9 | 14.6 | 14.1 | 15.0 | 14.4 |
| Mean number of readmissions within 365 days, ±SD | 1.2 ± 1.6 | 1.2 ± 1.5 | 1.2 ± 1.6 | 1.2 ± 1.5 | 1.2 ± 1.6 |
| Mean number of cardiovascular readmissions within 365 days, ±SD† | 0.7 ± 1.1 | 0.7 ± 1.1 | 0.7 ± 1.1 | 0.7 ± 1.1 | 0.7 ± 1.1 |
| Patients who died | |||||
| Within 60 days, % | 4.5 | 4.1 | 4.7 | 4.1 | 4.3 |
| Within 1 year, % | 13.6 | 12.8 | 13.8 | 12.2 | 13.0 |
| During study period, % | 33.1 | 30.8 | 31.4 | 28.2 | 30.8 |
| Patients who died or had any readmission | |||||
| Within 60 days, % | 34.7 | 33.8 | 37.3 | 34.9 | 34.9 |
| Within 1 year, % | 60.9 | 59.7 | 61.7 | 59.4 | 60.3 |
| During study period, % | 77.7 | 76.4 | 77.2 | 75.0 | 76.5 |
| Patients who died or had cardiovascular readmission | |||||
| Within 60 days, % | 26.3 | 26.3 | 28.9 | 27.3 | 27.1 |
| Within 1 year, % | 48.1 | 48.5 | 49.6 | 48.1 | 48.6 |
| During study period, % | 67.4 | 67.4 | 67.7 | 65.4 | 67.1 |
| Patients who died or had any readmission more than 60 days after index admission | |||||
| Within 1 year, % | 46.1 | 44.9 | 44.7 | 43.6 | 44.8 |
| During study period, % | 69.9 | 68.4 | 67.7 | 66.0 | 68.0 |
| Patients who died or had cardiovascular readmission more than 60 days after index admission | |||||
| Within 1 year, % | 33.2 | 33.4 | 32.4 | 32.0 | 32.9 |
| During study period, % | 58.4 | 58.2 | 56.7 | 55.2 | 57.3 |
P = .001 for comparisons between regions except where indicated.
P > .05 for comparisons between regions.
NE, Northeast; S, South; MW, Midwest; W, West; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty.
Predictors of Mortality
Independent multivariable predictors of 60-day mortality are shown in Table 3. Higher age, white race, congestive heart failure, stroke, number of discharge diagnoses, Charlson Index >2, absence of hypertension and hyperlipidemia diagnoses, absence of cardiac catheterization, and CABG or PTCA at index admission were all associated with increased risk of death. Geographic region was not a significant predictor of 60-day mortality adjusted for the other factors.
Table 3.
Predictors of 60-day Mortality (Multivariable)
| OR | 95% CI | P Value | |
|---|---|---|---|
| Age | 1.034 | 1.030 to 1.039 | .0001 |
| Gender (male versus female) | 1.172 | 0.812 to 1.693 | .3966 |
| Race (white versus others) | 1.417 | 1.251 to 1.605 | .0001 |
| Hypertension | 0.790 | 0.726 to 0.861 | .0001 |
| Diabetes | 0.979 | 0.889 to 1.079 | .6736 |
| Congestive heart failure | 1.688 | 1.536 to 1.854 | .0001 |
| Hyperlipidemia | 0.683 | 0.590 to 0.790 | .0001 |
| Atrial fibrillation | 1.112 | 0.984 to 1.257 | .0880 |
| COPD | 0.947 | 0.857 to 1.046 | .2837 |
| Stroke | 1.682 | 1.238 to 2.286 | .0009 |
| Discharge diagnoses, n | 1.029 | 1.009 to 1.049 | .0043 |
| Charlson Index | 1.707 | 1.533 to 1.901 | .0001 |
| Cardiac catheterization at index | 0.546 | 0.477 to 0.624 | .0001 |
| CABG or PTCA at index | 0.517 | 0.435 to 0.614 | .0001 |
| Region | |||
| MW versus S | 1.069 | 0.965 to 1.185 | .2014 |
| NE versus S | 0.912 | 0.804 to 1.034 | .1515 |
| W versus S | 0.950 | 0.847 to 1.065 | .3747 |
COPD, chronic obstructive pulmonary disease; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty; MW, Midwest; NE, Northeast; S, South; W, West.
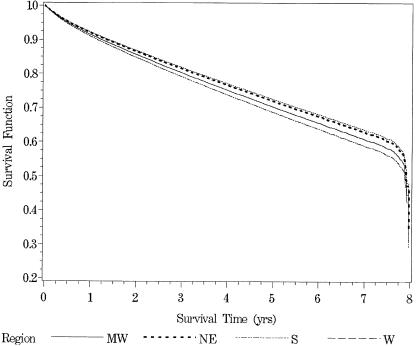
Predictors of time to death within the first year for patients alive 60 days after the index admission are shown in Table 4. Higher age, male gender, diabetes, congestive heart failure (CHF), atrial fibrillation, chronic obstructive pulmonary disease (COPD), absence of the diagnoses of hypertension and hyperlipidemia, number of discharge diagnoses, Charlson Index >2, absence of cardiac catheterization at the index hospitalization, absence of CABG and PTCA at the index hospitalization, and absence of clinic visits within 60 days were all associated with decreased time to death. Patients with both cardiology and general medicine clinic visits within 60 days of discharge from the index hospitalization had longer time to death than did patients with general medicine clinic visits alone, who had longer time to death than patients without clinic visits to either cardiology or general medicine. Region of the country was still significant even after adjusting for other factors, with patients in the South having the shortest survival time. Survival curves for the 4 regions are shown in Figure 1.
Table 4.
Predictors of Time to Death for Patients Alive 60 Days After Index Admission (Multivariable)
| Hazard Ratio | 95% CI | P Value | |
|---|---|---|---|
| Age | 1.039 | 1.037 to 1.041 | .0001 |
| Gender (male versus female) | 1.831 | 1.542 to 2.176 | .0001 |
| Race (white versus others) | 1.027 | 0.983 to 1.073 | .2271 |
| Hypertension | 0.936 | 0.906 to 0.967 | .0001 |
| Diabetes | 1.134 | 1.092 to 1.177 | .0001 |
| Congestive heart failure | 1.398 | 1.346 to 1.452 | .0001 |
| Hyperlipidemia | 0.697 | 0.658 to 0.738 | .0001 |
| Atrial fibrillation | 1.062 | 1.010 to 1.117 | .0184 |
| COPD | 1.224 | 1.177 to 1.272 | .0001 |
| Stroke | 0.980 | 0.847 to 1.135 | .7892 |
| Discharge diagnoses, n | 1.088 | 1.080 to 1.096 | .0001 |
| Charlson Index | 1.415 | 1.357 to 1.475 | .0001 |
| Cardiac catheterization at index | 0.856 | 0.821 to 0.893 | .0001 |
| CABG or PTCA at index | 0.641 | 0.602 to 0.681 | .0001 |
| CABG or PTCA within 60 days | 1.029 | 0.937 to 1.130 | .5495 |
| Clinic visits within 60 days* | |||
| Both versus none | 0.737 | 0.668 to 0.813 | .0001 |
| Cardiology versus none | 0.747 | 0.704 to 0.792 | .0001 |
| General Medicine versus none | 0.941 | 0.901 to 0.984 | .0073 |
| Region | |||
| MW versus S | 0.939 | 0.902 to 0.978 | .0023 |
| NE versus S | 0.875 | 0.834 to 0.918 | .0001 |
| W versus S | 0.856 | 0.818 to 0.895 | .0001 |
Interaction between Cardiology and General Medicine not significant; P = .4389.
COPD, chronic obstructive pulmonary disease; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty; MW, Midwest; NE, Northeast; S, South; W, West.
FIGURE 1.
Survival curves of the 4 regions (all-cause mortality). MW, Midwest; NE, Northeast; S, South; W, West.
Predictors of Time to Readmission
Table 5 shows the predictors of time to first hospital readmission and first cardiovascular readmission, excluding readmissions within 60 days of discharge from the index hospitalization. Higher age, male gender, nonwhite race, diabetes, CHF, COPD, number of discharge diagnoses, Charlson Index >2, cardiac catheterization at the index hospitalization, and CABG or PTCA at the index hospitalization were all associated with decreased time to the first readmission, while hypertension and hyperlipidemia, cardiology visit within 60 days, CABG or PTCA within 60 days after discharge from the index hospitalization, and Northeast or South region were associated with increased time to the first readmission. Higher age, male gender, nonwhite race, hypertension, diabetes, CHF, atrial fibrillation, COPD, number of discharge diagnoses, cardiac catheterization at the index hospitalization, CABG or PTCA at the index hospitalization, presence of cardiology clinic visits within 60 days, and South region were all associated with decreased time to the first cardiovascular readmission, whereas hyperlipidemia and CABG or PTCA within 60 days after index hospitalization were associated with increased time to the first cardiovascular readmission.
Table 5.
Predictors of Time to First Readmission More Than 60 Days After Index Admission for Patients Alive 60 Days After Index Admission (Multivariable)
| Any Readmission | Cardiovascular Readmission | |||||
|---|---|---|---|---|---|---|
| Hazard Ratio | 95% CI | P Value | Hazard Ratio | 95% CI | P Value | |
| Age | 1.009 | 1.008 to 1.010 | .0001 | 1.007 | 1.006 to 1.008 | .0001 |
| Gender (male versus female) | 1.299 | 1.172 to 1.439 | .0001 | 1.296 | 1.146 to 1.467 | .0001 |
| Race (white versus others) | 0.921 | 0.894 to 0.948 | .0001 | 0.885 | 0.856 to 0.916 | .0001 |
| Hypertension | 0.973 | 0.952 to 0.995 | .0153 | 1.036 | 1.009 to 1.063 | .0078 |
| Diabetes | 1.076 | 1.048 to 1.104 | .0001 | 1.102 | 1.068 to 1.136 | .0001 |
| Congestive heart failure | 1.144 | 1.111 to 1.179 | .0001 | 1.343 | 1.298 to 1.389 | .0001 |
| Hyperlipidemia | 0.814 | 0.789 to 0.840 | .0001 | 0.887 | 0.855 to 0.919 | .0001 |
| Atrial fibrillation | 1.016 | 0.977 to 1.056 | .4322 | 1.077 | 1.029 to 1.126 | .0013 |
| COPD | 1.136 | 1.104 to 1.169 | .0001 | 1.042 | 1.007 to 1.078 | .0184 |
| Stroke | 0.895 | 0.789 to 1.014 | .0824 | 0.930 | 0.800 to 1.080 | .3422 |
| Discharge diagnoses, n | 1.065 | 1.060 to 1.071 | .0001 | 1.061 | 1.055 to 1.067 | .0001 |
| Charlson Index | 1.112 | 1.080 to 1.144 | .0001 | 1.018 | 0.984 to 1.053 | .3003 |
| Cardiac catheterization at index | 2.032 | 1.979 to 2.085 | .0001 | 2.856 | 2.772 to 2.942 | .0001 |
| CABG or PTCA at index | 1.283 | 1.243 to 1.325 | .0001 | 1.475 | 1.426 to 1.527 | .0001 |
| CABG or PTCA within 60 days | 0.695 | 0.663 to 0.728 | .0001 | 0.544 | 0.516 to 0.574 | .0001 |
| Clinic visits within 60 days* | ||||||
| Cardiology and General Medicine versus none | 0.977 | 0.928 to 1.028 | .3727 | 1.081 | 1.019 to 1.147 | .0100 |
| Cardiology versus none | 0.937 | 0.906 to 0.969 | .0001 | 1.047 | 1.008 to 1.088 | .0189 |
| General Medicine versus none | 0.987 | 0.959 to 1.016 | .3691 | 1.033 | 0.998 to 1.068 | .0619 |
| Region | ||||||
| MW versus S | 0.975 | 0.949 to 1.002 | .0704 | 0.931 | 0.902 to 0.962 | .0001 |
| NE versus S | 0.951 | 0.921 to 0.983 | .0029 | 0.882 | 0.849 to 0.917 | .0001 |
| W versus S | 0.952 | 0.924 to 0.980 | .0010 | 0.924 | 0.893 to 0.957 | .0001 |
Interaction between Cardiology and General Medicine not significant; P = .0937 and .9968.
COPD, chronic obstructive pulmonary disease; CABG, coronary artery bypass grafting; PTCA, percutaneous transluminal coronary angioplasty; MW, Midwest; NE, Northeast; S, South; W, West.
DISCUSSION
We found substantial variation in both health care utilization and clinical outcomes in this national sample of veterans with AMI. This finding is consistent with the study of chronic medical conditions by Ashton et al.,17 who found significant regional variation in the use of inpatient and outpatient services. That study did not include AMI and had no outcome measures post-discharge.
Adjusting for age, demographic characteristics, and comorbid conditions, we found that the region of the country was an independent predictor of time to death among patients discharged alive with AMI. As has been reported for other conditions, patients in the Northeast were somewhat older and had more comorbid illnesses, whereas patients in the West tended to be younger and less chronically ill.17 Hence, as expected, patients in the Northeast had a longer length of stay and inpatient mortality during the index hospitalization compared to the West.20 Hypertension and hyperlipidemia, which are known coronary risk factors, had an inverse relationship with the risk of mortality in our data, which is similar to findings from other data-based studies21 and suggests that veterans with AMI who carry such diagnoses have had these conditions recognized and presumably treated. Another explanation is that when the number of coding slots is limited, it has been postulated that hypertension and hyperlipidemia are coded only when more serious conditions are not present, which could indicate a healthier subgroup of patients. Presence of CABG or PTCA at index admission was also associated with increased time to death. It is likely that this represented a healthier group of patients who could withstand surgery. One other explanation is that patients with AMI treated more aggressively with CABG following their AMI have better outcomes.22
Our main finding was a significantly greater risk of mortality and subsequent readmission in the South region compared to the Northeast and the West. It is intriguing that despite having a higher proportion of patients with diabetes and Charlson Index >2, patients in the Northeast had a lower adjusted mortality risk than those in the South. Unlike prior studies in the VA that found no clear pattern of regional variation in rates of outpatient follow-up for patients discharged with angina, we found that patients in the Northeast and West were more likely than patients in the South to have a primary care or cardiology visit following discharge. The significance of region after adjusting for outpatient follow-up indicates, however, that this is not the sole difference between regions in the risk of AMI patients dying or being readmitted. Also, the difference in survival among the regions starts to become apparent at 1 year post-discharge (Fig. 1), further emphasizing that longer term chronic care and follow-up of patients may be important in improving survival in patients with myocardial infarction. In their review of AMI patients, Martin et al.23 showed that mortality in patients without subsequent outpatient follow-up is extremely high. This could be due to missed opportunities for aggressive risk modification, for early identification of the need for surgical intervention, and for cardiac rehabilitation.
One might hypothesize that the sicker patients received more follow-up. However, if that were true, then patients in the West (who had lower mortality and readmission rates) should have received less outpatient follow-up, which was not the case. Although post-myocardial infarction follow-up was associated with better outcomes, more than half of the patients in our study had no primary care or cardiology follow-up at a VAMC within 60 days of discharge, and a third had no follow-up 1 year after discharge from their index AMI hospitalization, suggesting that there is substantial room for improvement in the care of veterans with AMI. It is possible that some of the patients not receiving follow-up outpatient care in the VA system received such care outside the VA system.14 Even if this were so, the findings in our study would suggest that greater follow up within the VA system (presumably where there is better communication between providers of care) was associated with better outcomes. We found variation in revascularization rates with CABG during and within 1 year post-discharge from the index AMI hospitalization among the 4 regions, similar to findings in non-VA hospitals.24,25 Hence, it is likely that the regional variation in mortality risk noted in our study was due to a combination of differential revascularization rates and outpatient follow-up among the different regions.
In the current study, we found an inverse relationship between outpatient follow-up and subsequent all-cause readmission, with greater rates of outpatient follow-up being associated with overall lower readmission rates. This is in contrast to the study by Weinberger et al.26 where more post-discharge outpatient follow-up with the primary care physicians was associated with increased rates of subsequent hospitalization. However their study did not specifically target follow-up after AMI. Moreover, their study was a randomized, controlled trial of providing primary care to patients discharged from VA medicine service who previously had not received VA-based primary care. The study by Piette and Moos5 also found that greater ambulatory follow-up post-AMI was associated with decreased mortality (as in our study) but was associated with increased odds of readmission. However, their study was limited to 1992 only. It appears that patients having follow-up outpatient cardiology care, especially if combined without primary care, had a higher risk of subsequent readmission for myocardial infarction. This may be because patients with worse cardiovascular disease (and prognosis) may have been referred to a VA cardiology clinic. As is known, typically, at a VAMC most of the patients with AMI are managed by a primary care physician, and only patients who have received procedural interventions at their admission for AMI are followed up in specialty clinics. There have been no studies that have demonstrated a regional variation in this practice.
Regional variation in the treatment of AMI has also been demonstrated in the non-VA population.25 However, geographic variation in the care and outcomes of patients in the VA system is an intriguing finding, given the VA's centralized administrative structure and policies. Differences in the prevalence or severity of disease cannot explain all of the differences we found, in that patients in the Northeast had a higher Charlson Index and a greater number of comorbid conditions but had better outcomes than patients in the South. The variation also cannot be explained on the basis of financial incentives, because all VA physicians are salaried and all VA facilities use the same system of reimbursement.
There are several limitations in our study. First, critical variables were unavailable in the administrative data we used (e.g., medications, smoking status, severity of AMI, socioeconomic status). Second, because we do not know the cause of death, we modeled all-cause mortality rather than death specifically related to AMI or other cardiovascular conditions. In addition, the use of ICD-9-CM codes is associated with some unavoidable errors. Yet, studies validating the accuracy of coding within the VA system have shown substantial reliability.27 Chart review of the same Austin PTF database by Wright et al. found 96% accuracy in coding for AMI. There is also no evidence that coding errors differ by region. We were also not able to assess the use of non-VA inpatient or outpatient health services, which may vary by geographic region. In addition, because most veterans are eligible for Medicare insurance and thus can be hospitalized for AMI at many non-VA facilities, our findings can only be generalized to veterans hospitalized with AMI at VAMCs. However, a recent study by Petersen et al. found no difference in 5-year mortality between Medicare and VA patients post-myocardial infarction.28,29 Wright et al. showed that about 70% of the VA users were admitted to non-VA Medicare hospitals for their AMI (S. Wright, PhD, written communication, July 2001).14 However, there have been no studies thus far demonstrating regional variability in the use of non-VA services. Moreover, given our large sample size, small differences may be statistically significant but not clinically relevant. Finally, this is a retrospective study of administrative data, and we cannot establish causation.
Despite the limitations, our findings are still an important initial step in identifying associations between clinical variables and treatment outcomes among veterans hospitalized in a VAMC for AMI. Our study is unique in that it captures patient and process of care data in a large stable cohort that rarely changes health care systems. Our finding of a substantial degree of regional variability suggests that both processes and outcomes of care post-AMI can be improved in the VA system. Further studies are needed to explore the possibility that increased outpatient care following AMI can improve outcomes. Also, it may be important to identify which differences in care among the different VA regions influence AMI outcomes and if there are any differences among the regions at the level of the hospital and its patient load.30,31 The link between process of care and outcomes is a critical step in understanding the significance of practice variation.22,32,33 This will provide a basis for designing effective strategies and interventions in the acute and chronic care of patients post-AMI that would improve patient outcomes.
Acknowledgments
This research was supported by a contract with Bristol Myers Squibb, Inc.
REFERENCES
- 1.American Heart Association Heart and Stroke Statistical Update. 1997. Washington DC: American Heart Association; 1997. [Google Scholar]
- 2.U.S. Department of Health and Human Services. Healthy People 2010. Undestanding and Improving Health. 2nd Ed. Washington, DC: U.S. Government Printing Office; 2000. [Google Scholar]
- 3.Benson V, Marano MA. Current estimates from the National Health Interview Survey (NHIS), 1995. Vital Health Stat. 1998;10:1–428. [PubMed] [Google Scholar]
- 4.Smith T, Melfi C, Keterson J, Sandmann B, Kotsanos J. Direct medical charges associated with myocardial infarction in patients with and without diabetes. Med Care. 1999;37:S4–S11. doi: 10.1097/00005650-199904001-00002. [DOI] [PubMed] [Google Scholar]
- 5.Piette JD, Moos RH. The influence of distance on ambulatory care use, death, and readmission following a myocardial infarction. Health Serv Res. 1996;31:573–91. [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen E, Wright SM, Daley J, Thibault GE. Racial variation in cardiac procedure use and survival following AMI in the department of veterans affairs. JAMA. 1994;271:1175–81. [PubMed] [Google Scholar]
- 7.Whittle JJ, Conigliaro J, Good CB, Lofren RP. Racial differences in the use of invasive cardiovascular procedures in the Department of Veterans Affairs medical system. N Engl J Med. 1993;329:621–7. doi: 10.1056/NEJM199308263290907. [DOI] [PubMed] [Google Scholar]
- 8.Wolinsky FD, Wyrwich KW, Gurney JG. Gender differences in the sequellae of hospitalization for AMI among older adults. J Am Geriatr Soc. 1999;47:151–8. doi: 10.1111/j.1532-5415.1999.tb04572.x. [DOI] [PubMed] [Google Scholar]
- 9.Asch SM, Sloss EM, Hogan C, Brook RH, Kravitz RL. Measuring underuse of necessary care among elderly medicare beneficiaries using inpatient and outpatient claims. JAMA. 2000;284:2325–33. doi: 10.1001/jama.284.18.2325. [DOI] [PubMed] [Google Scholar]
- 10.Guadagnoli E, Landrum MB, Peterson EA, Gahart MT, Ryan TJ, McNeil BJ. Appropriateness of coronary angiography after myocardial infarction among Medicare beneficiaries. Managed care versus fee for service. N Engl J Med. 2000;343:1460–6. doi: 10.1056/NEJM200011163432006. [DOI] [PubMed] [Google Scholar]
- 11.Iglehart JK. Reform of the Veterans Affairs health care system. N Engl J Med. 1996;335:1407–11. doi: 10.1056/NEJM199610313351821. [DOI] [PubMed] [Google Scholar]
- 12.Pladevall M, Goff DC, Nichaman MZ, et al. An assessment of the validity of ICD code 410 to identify hospital admissions for myocardial infarction. The Corpus Christi Heart Project. Int J Epidemiol. 1996;25:948–52. doi: 10.1093/ije/25.5.948. [DOI] [PubMed] [Google Scholar]
- 13.CAPRIE Steering Committee. A randomized, blinded trial of clopidogrel versus aspirin in patients at risk of ischemic events. Lancet. 1996;348:1329–39. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 14.Wright SM, Petersen LA, Lamkin RP, Daley J. Increasing use of Medicare services by veterans with AMI. Med Care. 1999;37:529–37. doi: 10.1097/00005650-199906000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 17.Ashton CM, Petersen NJ, Souchek J, et al. Geographic variation in utilization rates in veterans affairs hospitals and clinics. N Engl J Med. 1999;340:32–9. doi: 10.1056/NEJM199901073400106. [DOI] [PubMed] [Google Scholar]
- 18.Fleming C, Fisher ES, Chang CH, Bubolz TA, Malenka DJ. Studying outcomes and hospital utilization in the elderly: the advantages of a merged database for Medicare and Veterans Affairs hospitals. Med Care. 1992;30:377–91. doi: 10.1097/00005650-199205000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Fisher SG, Weber L, Goldberg J, Davis F. Mortality ascertainment in the veteran population: alternatives to the National Death Index. Am J Epidimiol. 1995;141:242–50. doi: 10.1093/oxfordjournals.aje.a117426. [DOI] [PubMed] [Google Scholar]
- 20.Matsui K, Goldman L, Johnson P, Kuntz K, Cook E, Lee T. Comorbidity as a correlate of length of stay for hospitalized patients with acute chest pain. J Gen Intern Med. 1996;11:262–9. doi: 10.1007/BF02598265. [DOI] [PubMed] [Google Scholar]
- 21.Tierney WM, McDonald CJ. Practice databases and their uses in clinical research. Stat Med. 1991;10:541–57. doi: 10.1002/sim.4780100406. [DOI] [PubMed] [Google Scholar]
- 22.Wright SM, Daley J, Peterson ED, Thibault GE. Outcomes of AMI in the Department of Veterans Affairs: does regionalization of health care work. Med Care. 1997;35:128–41. doi: 10.1097/00005650-199702000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Martin M, Nigel B, David G, Tracey Y, John H. Outcome and use of health services four years after admission for AMI. BMJ. 1999;319:230–1. doi: 10.1136/bmj.319.7204.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Cardiology Working Group. Cardiology and the quality of medical practice. JAMA. 1991;265:482–5. doi: 10.1001/jama.1991.03460040072032. [DOI] [PubMed] [Google Scholar]
- 25.Pilote L, Califf RM, Sapp S, Miller DP, Mark DB. Regional variation across the United States in the management of AMI. N Engl J Med. 1995;333:565–72. doi: 10.1056/NEJM199508313330907. [DOI] [PubMed] [Google Scholar]
- 26.Weinberger M, Oddone EZ, Henderson WG. Does increased access to primary care decrease hospital readmissions? N Engl J Med. 1996;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 27.Petersen LA, Wright SM, Normand SL, Kluiber S, Daley J. Positive predictive value of the diagnosis of AMI in an administrative database. J Gen Intern Med. 1999;14:555–8. doi: 10.1046/j.1525-1497.1999.10198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petersen LA, Normand SL, Daley J, McNeil BJ. Outcome of myocardial infarction in Veterans Health Administration patients as compared with Medicare patients. N Engl J Med. 2000;343:1934–41. doi: 10.1056/NEJM200012283432606. [DOI] [PubMed] [Google Scholar]
- 29.Rosenthal GE, Larimer DJ, Owens KE. Treatment of patients with AMI at a Veterans Affairs (VA) hospital and a non-VA hospital. J Gen Intern Med. 1994;9:455–8. doi: 10.1007/BF02599064. [DOI] [PubMed] [Google Scholar]
- 30.Krakauer HR, Skellan KJ. Evaluation of the HCFA model for the analysis of mortality following hospitalization. Health Serv Res. 1992;27:317–35. [PMC free article] [PubMed] [Google Scholar]
- 31.Hartz AJ, Krakauer HR, Kuhn EM, et al. Hospital characteristics and mortality rates. N Engl J Med. 1989;321:1720–5. doi: 10.1056/NEJM198912213212506. [DOI] [PubMed] [Google Scholar]
- 32.Wennberg JE. Unwanted variations in the rules of practice. JAMA. 1991;265:1306–7. [PubMed] [Google Scholar]
- 33.Wennberg JE, Freeman JL, Shelton RM, Bubollz TA. Hospital use and mortality among Medicare beneficiaries in Boston and New Haven. N Engl J Med. 1989;323:1168–73. doi: 10.1056/NEJM198910263211706. [DOI] [PubMed] [Google Scholar]