Abstract
OBJECTIVE
To examine the characteristics and outcomes of physician-referred weight management patients relative to self-referred patients.
DESIGN
Review of clinic records of all individuals contacting a weight control program during a 2-year period with follow-up throughout consecutive levels of treatment (i.e., enrollment, completion, and outcome).
SETTING
Medical school weight management center.
PARTICIPANTS
A consecutive sample (N = 1,392) of overweight and obese callers was categorized as physician-initiated (n = 345), media (n = 653), or personal (n = 394) referrals. Attendees at initial consultation (n = 571) were age 41.7 ± 12.8 years, weight 113.9 ± 36.1 kilograms, and body mass index (BMI) 40.3 ± 11.3 kg/m2 (data expressed as mean ± standard deviation).
INTERVENTIONS
Low-calorie-diet and very-low-calorie-diet programs.
MAIN OUTCOME MEASURES
Gender comparisons, attendance at initial consultation, body mass index, motivation, comorbidities, enrollment and completion rates, and weight loss.
RESULTS
Compared to callers from other referral sources, physician referrals included a larger minority of males (25.2%) and were more likely to attend an initial consultation (63.5%; P < .001). Among consultation attendees, physician referrals were heavier (mean BMI = 44.8), reported more comorbidities, were less likely to join programs (16.9%), and scored as less motivated than other referrals (P < .007). Completion rates for physician referrals were higher than for self-referrals in the very-low-calorie-diet program (85.7%; P < .04) but not in the low-calorie-diet program (P > .05). Among completers, physician referrals did not differ on weight loss in either program (P > .05).
CONCLUSIONS
Compared to self-referrals, physician-referred individuals are in greater need of weight loss, less motivated, less likely to enter treatment, but equally likely to profit from it. Therefore, physician referral for weight loss is beneficial for at least some patients and should be encouraged.
Keywords: obesity, referral and consultation, weight reduction, diet, reducing
The pandemic of obesity has reached alarming proportions and has become a major health problem worldwide.1,2 The continued increase in prevalence of obesity in the last 10 years, coupled with its link to significant and life-threatening comorbidities and mortality,3,4 has led some researchers to conclude that obesity should be considered a chronic disease that requires chronic medical management.5 An increasing emphasis has been on the primary care physician's role in this mission. Research in this area has focused on several topics including 1) improving the physician's ability to deliver direct weight management counseling,6–10 2) identifying physicians' attitudes toward their obese patients that may interfere with appropriate patient care,11,12 and 3) examining intervention and referral patterns for weight loss treatment.13–15
Regarding physician patterns of intervention in obesity, a survey of physicians by Kristellar and Hoerr14 examined factors affecting the likelihood that physicians would discuss obesity with their patients. They reported that likelihood increased with both the degree of obesity (19% non-obese, 42% mildly obese, and 94% severely obese) and with the presence of significant comorbidities.
Large population-based studies examining physician practices have also been carried out. With a nationally representative, nonclinical telephone sample of over 3,000 women, O'Neil et al.16 found that a third of all subjects reported that they had ever been advised to lose weight by their physician, with greater likelihood among subjects with higher reported lifetime body mass index (BMI) (BMI = 18 to 25, 5.6%; BMI = 25 to 30, 31.1%; BMI = 30 to 35, 65.7%; BMI >35, 84.1%). Similarly, Galuska et al.13 examined a large sample from the Behavioral Risk Factor Surveillance System 1996 Telephone Survey to investigate health professionals' practices with obese patients. Among obese respondents who had seen their physician in the previous 12 months, 42% reported that they had been advised to lose weight by a healthcare provider. The best predictors for receiving such advice were being female, middle-aged, more obese, having diabetes mellitus, or reporting poorer perceived health.
Wadden et al.15 assessed patient perceptions of physician weight management practices and attitudes among 259 obese women who sought treatment in randomized weight loss trials. A third of patients indicated that their physician discussed weight control with them at least at every other visit, 39% reported that such discussion took place only occasionally, and 28% reported that their physician never discussed weight control with them. In addition, nearly half of the patients reported that their physician had not prescribed any of the 10 listed weight control methods.
Another issue is what physicians do to help patients to lose weight once they have offered advice to do so. Each of the previously outlined studies addressed the issue of treatment options used by physicians with their obese patients. Kristellar and Hoerr14 reported that, across all specialty groups, 34% of physicians said they would treat patients themselves, 29% would make direct referrals, and about 25% would provide recommendation without specific referral. O'Neil et al.16 reported that patients who were advised to lose weight reported 3 main intervention methods by the advising physician: diet (54%), medication (16%), and referral to a weight loss program (14%). In Wadden et al.,15 the intervention methods used by the largest number of physicians were: prescribing a diet plan (23%), commercial program (Weight Watchers; 18.5%), medication (17%), readings (15%), and an exercise plan (13%).
Although there are several methods of intervention both available and utilized by physicians in primary care, a variety of factors including time limitations and physician beliefs concerning their own competency in managing obesity may lead some physicians to refer to weight management programs.17 However, little research has been done to investigate the role that physician referral, as compared to self-referral (i.e., media, word of mouth) may play in patients' decisions to either initiate contact with weight management programs and/or attend treatment. Similarly, few data exist on the relationship between referral source and treatment outcome.
A comprehensive literature review using both medline and Psych-Info databases located only 1 study that specifically investigated the relationship between referral source and treatment outcome. Baran and Alain18 examined the relationship between referral source and weight loss treatment outcome as part of a study designed to examine other possible mediating variables in treatment outcome. Subjects were 93 adults attending a weight management clinic in Quebec, Canada. On the basis of self-report, patients were classified as self-referred (n = 64) or referred by a physician (n = 29). Those who were referred by a physician were older (mean = 48.69 vs mean = 39.55 years) and required a larger weight loss to achieve the goal weight (mean = 17.6 vs 15.5 kg). Physician-referred patients achieved a significantly smaller percentage of their weight loss goal (mean = 44.6%) than did their self-referred counterparts (mean = 68.8%). Some limitations with the study are noteworthy. The study only considered a 12-week very-low-calorie-diet (VLCD) program of 500 kcal per day, which was both shorter and more restrictive than the majority of weight management programs. Also, other differences between referral groups (i.e., comorbidities) were not considered.
The present study sought to examine comprehensively the relationship between type of referral source (i.e., physician, media, word of mouth) and outcomes of several levels of contact with a weight loss program from initial telephone contact through treatment program completion. The initial sample consisted of all individuals who telephoned a medical school weight management center to inquire about programs during a 2-year period. Referral source was examined in relation to a number of variables including patient characteristics, motivation, self-reported comorbidities, program initiation, program completion, and weight loss in both low-calorie-diet (LCD) and VLCD programs.
METHODS
Participants
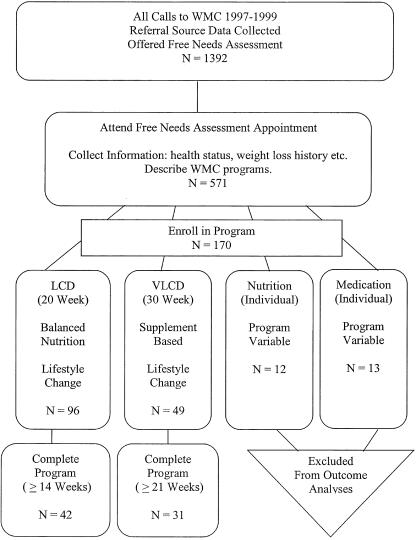
For an overview of the subject selection and data collection process, see Figure 1. The initial sample consisted of all people who telephoned the Medical University of South Carolina Weight Management Center (WMC) during 1997 and 1998 to inquire about available programs. This telephone sample consisted of 1,133 females and 259 males (N = 1,392). At the time of the telephone contact, data concerning gender and referral source were obtained. No additional data (i.e., race, age, weight) were collected during the telephone contact. All data were reviewed retrospectively.
FIGURE 1.
Breakdown of data collection.
All individuals who called were offered a free 30-minute needs assessment consultation with a clinical staff member in which information regarding health, weight status, demographic information and history were elicited, appropriate programs were described and offered, and fee schedules were discussed. Of the sample, 571 people attended a needs assessment session. The descriptive characteristics of the needs assessment attendee subsample can be found in Table 1.
Table 1.
Characteristics of Those Callers Attending a Free 30-minute Needs Assessment (N = 571)
| Range | Mean (SD) | n (%) | |
|---|---|---|---|
| Age, y | 18 to 85 | 41.7 (12.81) | — |
| BMI, kg/m2 | 20.7 to 96.5 | 40.3 (11.28) | — |
| Weight, kg | 52.5 to 340.9 | 113.93 (36.08) | — |
| Gender | |||
| Male | — | — | 136 (23.8) |
| Female | — | — | 435 (76.2) |
| Race | |||
| White | — | — | 352 (61.6) |
| Black | — | — | 140 (24.5) |
| Other | — | — | 79 (13.8) |
| Media referral, | — | — | 163 (28.6) |
| Personal referral, | — | — | 189 (33.1) |
| Physician referral | — | — | 219 (38.3) |
BMI, body mass index.
Of those subjects attending a needs assessment, 170 enrolled in 1 of 4 available programs (i.e., LCD, VLCD, medication, and nutritional counseling). Patients enrolled in the nutritional (n = 12), and medication (n = 13) counseling programs were not included in the analyses of outcome data because of the individual nature of the interventions and the open-ended duration of these treatments. This left for analysis, 96 LCD and 49 VLCD (N = 145) program enrollees. Weight loss data were obtained on patients who completed either of the programs.
The Medical University of South Carolina, Institutional Review Board for Human Research chairperson concurred with exempt designation # 4 on February 01, 2000.
Treatment Programs
Both the LCD and VLCD programs are provided on a fee-for-service basis and feature structured curriculum-based weekly small-group meetings providing instruction in dietary and exercise change and behavioral and cognitive techniques for initiating and sustaining these changes. The 20-week LCD program utilizes a balanced deficit food plan providing at least 1,200 kcal/day and is open to people of all weights. The VLCD program spans 30 weeks, with the initial 12 weeks on a supplement-based, 800 kcal/day diet program that can be extended up to a total of 20 weeks, depending on patient status and desire. A structured transition nutrition plan moves the patient from the VLCD to a balanced LCD or maintenance diet. A minimum BMI of 30 is required for the VLCD program.
Measures
Referral Source
During initial telephone contact, caller gender was identified and noted and callers were questioned as to the source of their referral to WMC (e.g., “How did you hear about us?”). Referral sources were categorized as: 1) “Media,” which included newspaper, television and radio advertising, Yellow Pages, newspaper or television reports, promotional mailings, internet, and public appearances by program representatives (in person or through the media); 2) “Personal,” including persons reporting direct contact with either WMC staff or patients, repeat patients, university employees, and other personal communications (e.g., word of mouth); 3) “MD,” which were referrals by an identified physician.
BMI and Health Status
Height, weight, and information relevant to current health status were gathered as part of the needs assessment. Patients were asked on a self-report questionnaire about the presence of the following medical conditions often considered to be obesity-related: previous heart attack, previous stroke, diabetes, hypertension, gallbladder disease, shortness of breath, orthopedic/joint problems, and high cholesterol/triglycerides. Self-reported health status information was considered both in terms of individual conditions and combined into a summary score of the total number of comorbidities reported.
Motivation
At the needs assessment, before meeting with a staff member, patients answered 3 questionnaire items adapted from the Dieting Readiness Test19 addressing motivation-related factors, rating them on a 5-point Likert scale (1 = not at all to 5 = extremely). The questions were: 1) “Compared to previous attempts, how motivated to lose weight are you this time?” (“Motivation”); 2) “How certain are you that you will stay committed to a weight loss program for the time it will take to reach your goal?” (“Commitment”); 3) “Consider all outside factors at this time in your life (the stress you're feeling at work, your family obligations, etc.). To what extent can you tolerate the effort required to stick to a diet?” (“Effort”).
Program Enrollment
All patients who enrolled in treatment programs at any time from the time of the needs assessment until the data extraction process began (October, 1999) were identified from enrollment records and grouped according to the type of program joined (LCD, VLCD, medication, nutritional counseling).
Program Completion
For patients enrolling in programs, program completion was determined from clinical record and was defined as continued attendance for at least 70% of the treatment program duration (attendance through week 14 for the LCD 20-week program and through week 21 for the VLCD 30-week program), with limited absences during the period of attendance.
Weight Loss
Weight loss was measured as the difference between body weight at week 1 of the treatment program and the last weight obtained. Weight change was expressed as kilograms lost, change in BMI, and percentage of body weight lost.
Statistical Analyses
Statistical analyses were performed using the Statistical Package for the Social Sciences for Windows 95 (Version 10.0; SPSS, Inc., Chicago, Ill). Referral category differences in program enrollment rates and program completion rates were examined for the initial telephone sample, the first subsample who attended needs assessment, the second subsample who enrolled in WMC programs, and the third subsample who completed either the LCD or VLCD program. Race and gender differences in enrollment rates and referral category were also considered. BMI, age, total number of comorbidities reported, individual physical disorders, and motivation (3 questions) were examined to determine group differences according to referral category.
Weight change data were analyzed separately for the LCD and VLCD program completers. For these analyses, because of small numbers, referral category groupings for Media and Personal, were combined to form a category of self-referred (SR) while maintaining the original MD category.
Nonparametric statistics (χ2) were used to analyze all categorical data. All noncategorical data were examined using analysis of variance (ANOVA) unless otherwise stated. When ANOVAs were significant, post hoc analyses using the Bonferroni correction were carried out. With the subsample who attended needs assessment, t tests for independent samples (program enrollees versus nonenrollees) were performed to determine if a relationship existed between the motivation questions and enrolling in WMC programs.
RESULTS
Telephone Sample
Of the entire sample that called WMC (N = 1,392), 46.9% (n = 653) were Media referrals, 28.3% (n = 394) were Personal, and 24.8% (n = 345) were MD. Although females predominated in each referral group, the ratio of males to females was higher in the MD group than in each of the other referral groups (χ2 = 13.32, P < .001; Media: females [n = 544], 83.3%, males [n = 109], 16.7%; Personal: females [n = 331], 84%, males [n = 63], 16%; MD: females [n = 258], 74.8%, males [n = 87], 25.2%).
Needs Assessment Sample
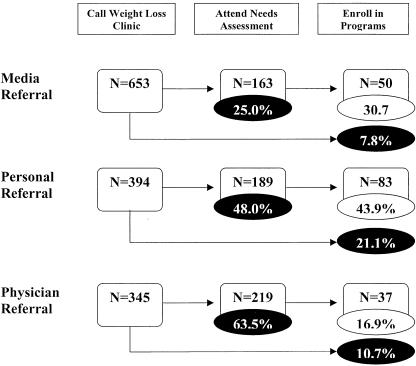
Comparing referral categories on likelihood of attending needs assessment, MD referrals were more likely (63.5%) to attend than were Media (25%) and Personal referrals (48%) (χ2 = 149.389, P < .001; Fig. 2). Males were more likely to attend needs assessment than were their female counterparts, regardless of referral category (52.5% vs 38.4%; χ2 = 17.363, P < .001).
FIGURE 2.
Levels of program involvement by referral source. X2s by referral group, all P < .001. Percentages in shaded ovals refer to percent of original callers. Percentages in nonshaded ovals refer to percent of needs assessment attendees.
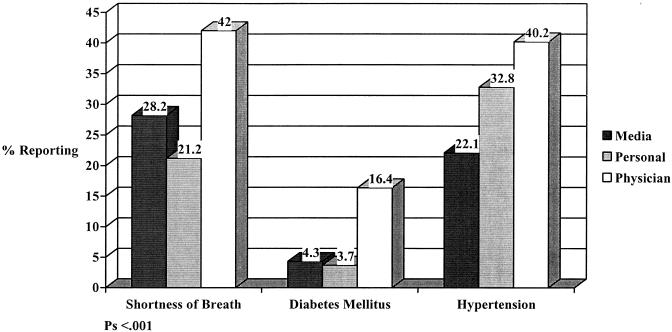
For the sample attending needs assessment, one-way ANOVAs revealed significant differences for weight among referral categories (F2,568 = 30.475, P < .001; Media, mean = 104.2 ± 30.37 kg; Personal, mean = 104.9 ± 30.75 kg; MD, mean = 128.1 ± 39.67 kg) and BMI, (F2,515 = 27.650, P < .001; Media, mean = 37.17 ± 9.93 kg/m2; Personal, mean = 37.90 ± 9.44 kg/m2; MD, mean = 44.77 ± 12.29 kg/m2). Post hoc analyses indicated that physician referrals were significantly heavier and had higher BMI than both other categories. Referral categories did not differ on age. Significant differences were noted for total number of comorbidities reported by referral category (F2,568 = 9.481, P < .001). Post hoc analyses indicated that MD referrals reported significantly more comorbidities (mean = 1.56 ± 1.31) than both personal (mean = 1.14 ± 1.17) and media referrals (mean = 1.07 ± 1.16). Examination of individual health conditions by referral category (Fig. 3) indicated that MD subjects reported a higher prevalence of diabetes mellitus (16.4%; χ2 = 26.602, P < .001) than either other referral category (Media 4.3%, Personal 3.7%). MD referrals also reported greater prevalence of hypertension (MD 40.2%, Media 22.1%, Personal 32.8%; χ2 = 13.941, P < .001), and shortness of breath (MD 42.0%, Media 28.2%, Personal 21.2%; χ2 = 21.472, P < .001). The total number of health conditions reported was not related to signing up for programs (P > .05).
FIGURE 3.
Health conditions reported at needs assessment.
Significant referral group differences on both the Motivation and Effort questions were noted (Fs2,568 = 5.23 and 5.05, P < .006 and .007, respectively). On the Motivation question, MD-referred subjects scored significantly lower (mean = 3.71 ± 1.52) than media-referred subjects (mean = 4.15, ± 1.22) but did not differ from personal referrals (mean = 3.99 ± 1.32). On the Effort question, subjects in the MD group scored lower (mean = 3.27 ± 1.28) than subjects in both the Media (mean = 3.63 ± 1.09) and Personal (mean = 3.56 ± 1.14) groups. Groups did not differ on the Commitment question.
Enrollment Rates
Comparisons by referral category among needs assessment attendees revealed that MD referrals were less likely to enroll for treatment programs than Media and Personal referrals (χ2 = 35.520, P < .001). In fact, the enrollment rate for MD-referred attendees was barely half that of each of the other groups (Media, 30.7%; Personal, 43.9%; MD, 16.9%) (Fig. 2). Referral-group comparisons of enrollment rates based on the initial telephone sample also differed significantly (χ2 = 41.108, P < .001) with personal referrals enrolling in programs at nearly twice the rate of both media and MD referrals (Media, 7.8%; Personal, 21.1%; MD, 10.7%). Males and females did not differ in terms of likelihood of enrolling (χ2 = 0.114, P > .05). Blacks were significantly less likely (χ2 = 29.649, P < .001) to enroll in treatment programs (White, 39.8%; Black, 14.3%).
Analysis of the Motivation questions also revealed that those who enrolled in programs scored higher than did nonenrollees on all 3 questions: Motivation (F1,569 = 6.690, P < .01; mean = 4.16 ± 1.23 vs 3.83 ± 1.44, respectively), Committed (F1,569 = 8.813, P < .003; mean = 3.99 ± 1.11 vs 3.62 ± 1.46, respectively), and Effort (F1,569 = 9.477, P < .002; mean = 3.70 ± 1.03 vs 3.37 ± 1.24, respectively).
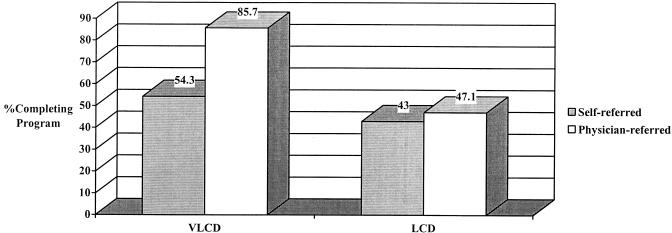
LCD and VLCD Program Completers
Because of smaller numbers, Media and Personal groups were combined into a Self-referred group (LCD, n = 79; VLCD, n = 35) and compared to the MD group (LCD, n = 17; VLCD, n = 14) for examinations of treatment completion and outcome. In the VLCD program, MD referrals had a higher completion rate than self-referrals (χ2 = 4.250, P < .04; MD, 85.7%; SR, 54.3%). Completion rates did not differ between groups in the LCD program (χ2 = .092, P > .05; MD, 47.1%; SR, 43%) (Fig. 4). Age, weight, BMI, and gender were not related to program completion for either program.
FIGURE 4.
Program completion rates for VLCD and LCD programs by referral source. Note: self-referred versus physician-referred, P < .04 in VLCD, not significant in LCD. VLCD, very-low-calorie diet program; LCD, low-calorie diet program. See “Methods” for completion criteria.
In neither the LCD nor the VLCD program did the 2 referral category groups differ on any weight loss measure (all P > .10) (weight change, BMI change, % change). Overall, among VLCD completers (n = 31), mean weight loss was 21.9 kg (±13.64), percent weight loss was 17.31% (±10.11), and BMI change was 7.47 kg/m2 (±4.57). For LCD completers (n = 42), mean weight loss was 3.96 kg (±4.5), percent weight loss was 4.27% (±4.55), and BMI change was 1.44 kg/m2 (±1.58).
DISCUSSION
Obese persons referred by their physicians to a university weight management program, compared to obese persons from other referral sources, differ in some important ways at initial contact and as they progress through the stages of enrollment and treatment. However, among those who do complete treatment, no differences are seen in treatment outcome.
Results suggest that physician referrals are heavier (weight and BMI) and more likely to report having comorbid conditions, especially hypertension, diabetes, and shortness of breath. This is consistent with surveys of both patients and physicians regarding which patients receive weight loss advice.13,14,16 However, unlike other studies,13,18 no age differences were observed. Although most people in all referral categories were female, MD referrals included a greater percentage of males than did other, self-referring groups.
Physician referrals were far more likely to attend a complimentary consultation session than were self-referrals. However, those physician-referral attendees were less likely to enroll in treatment programs than were needs assessment attendees from other referral sources. Further, considering program enrollment rates among the entire group of initial callers (i.e., percentages of initial telephone calls in each referral category that resulted in program enrollments), physician referrals, despite their greater attendance rate at needs assessment sessions, did not enroll in programs at a similarly high rate. In fact, MD referrals had a lower program enrollment rate than did personal referrals and were similar in enrollment rate to media referrals. There are several likely explanations for these findings. First, at the initial consultation, MD referrals described themselves as less motivated to lose weight and less tolerant of the effort required to lose weight, relative to other needs assessment attendees. Second, staff reports suggest that financial considerations are often more of an issue for the physician referrals than for others, perhaps reflecting the fact that the referrals were initiated by people other than the prospective patient, often without regard for program fees. Third, it is possible that some MD referrals attend needs assessments primarily to appease their physician and consider themselves to have met their obligation simply by attending. A final consideration is the higher enrollment rate among callers from the personal category. Often, prior patients or employees have referred these individuals, and one could speculate that they have been exposed to information regarding both program quality and fees. As a result, many of these callers may be predisposed to joining programs even before attending the initial consultation.
After treatment began, effects of referral source were only seen for rate of treatment completion. In the VLCD program, MD-referred patients were much more likely to complete programs than were those individuals who were self-referred. This distinction was not apparent in the LCD program. Further, among completers, weight loss outcomes of physician referrals did not differ from those of patients who were self-referred in either LCD or VLCD programs. This contrasts with the only other examination of treatment outcome as a function of referral source, which found that physician referrals had less successful outcomes in a 12-week VLCD program.18
Some psychological theories (e.g., self-determination20 and stages of change21) may predict that lasting behavior change requires that individuals should arrive at their own decision to decrease weight, because external directions to do so may not engage the same level of commitment to make the changes necessary for weight management. The present results suggest that this may be true for embarking on treatment but not necessarily for outcome once treatment has begun. While physician referrals are less likely than some others to join programs, they are no less likely to complete or profit from them.
Anecdotal reports indicate that many of the initial calls to the program for the physician referral subjects were made directly by the physician or the physician's staff. It may therefore be assumed that many of the people thus referred made contact with the treatment program at a time when otherwise they would not have, primarily as a result of physician intervention. Although only a small percentage of physician referrals actually enter weight loss treatment, it appears worthwhile for physicians to refer patients, given the minimal time and effort required of the physician and/or staff. This is especially true for patients entering a VLCD program, since once these patients do enter treatment, they are more likely to complete.
Motivation was measured in the present study prior to initial contact with the clinician and was found to be lower among physician referrals as compared to those otherwise referred. While the current design does not allow for determination of the influence the initial consultation may have on motivation, the influence of this initial contact with weight management programs on patient motivation is a worthwhile consideration for future research. Perhaps by focusing these initial contacts on helping patients to progress to an “action stage” of motivation,21 the decision to enter treatment will be facilitated. Also, providing a wider range of treatment options to suit varying levels of motivational readiness may encourage more of these less-motivated individuals to enter treatment.
Further, the physician referrals who attended needs assessments were more likely to report having comorbid health conditions such as diabetes mellitus and hypertension. Our data do not permit determination of the extent to which these physician referrals differ on their comorbidities from other obese patients of the referring physician. However, it is possible that physicians are targeting those obese patients who are at greatest risk from their obesity. Other possible explanations include increased probability of physician contact for patients who have comorbid diagnoses and/or an increased likelihood that patients with comorbid conditions will heed their physician's advice to seek weight loss treatment. Unfortunately, once in contact with our program, those referrals with greatest health risk were not more likely to join programs, but the referral from physicians did succeed in exposing these heavier, less-healthy patients to a treatment facility. This is particularly important because some research22 suggests that while gender, age, and BMI may predict weight loss treatment seeking, comorbidities such as hypertension and diabetes do not, making it particularly important that physicians direct these patients who most need weight loss to treatment.
The present study has some notable strengths. First, although physicians are increasingly seen as having an important role to play in the management of obesity, research examining the outcomes of their efforts is limited. This study addressed one aspect of physician management, referral, with a large sample of patients that included physician referrals and patients from other sources. Second, physician referrals were compared to other patients at each step of participation in the program, from initial contact to program completion. The vast majority of clinical studies in obesity examine patients only after they have joined a program and ignore the (often larger) group of people who make initial contact with a weight loss program but do not enroll. Finally, the fee-for-service setting allows for a somewhat more naturalistic approach than is often possible in research settings with necessarily restrictive subject selection criteria, thus improving generalizability to the experiences of the typical weight management consumer.
Some limitations are also apparent. First, some comorbid conditions were not assessed, for example, obstructive sleep apnea, which may have led to an underestimation of comorbidity. Second, while it is possible to speculate about the role that financial limitations may have had on enrollment rates, we could not obtain data concerning socioeconomic status from patients, thus limiting our ability to investigate issues of access to treatment (i.e., financial barriers). Third, information about referral source and comorbidities was all based on self-report. Finally, and obviously, only those physician-referred persons who actually contacted the Center were available for inclusion in this study, so information about the characteristics of patients who do not follow their physicians' referrals is not available.
Overall, physicians appear to be encouraging patients to at least seek initial consultation. Therefore, elucidating the factors that may influence patient follow-through with physician instructions subsequent to initial referral may be of primary importance in developing effective strategies to improve patient compliance. It has previously been demonstrated that by providing physicians with a brief counseling framework for intervening with patients, readiness to adopt increased physical activity is improved in the short term.23 By providing referring physicians with the tools to begin the process of motivational enhancement prior to the referral to a weight loss treatment facility, and with better methods to follow up after the referral is made, the number of patients entering weight loss treatment may be increased.
Another important implication of this study is that the results highlight some rarely discussed limitations of clinical trials of both pharmacological and nonpharmacological treatments. Those people who actually begin fee-for-service treatment represent a small minority of those who may inquire about treatment. This minority differs in important ways from the more numerous group of nonenrollees (i.e., referral source, self-reported motivation, race). The representativeness of clinical trial participants should be similarly examined, and these factors should be considered when the generalizability of clinical trial findings is appraised. Finally, since many who inquire about treatment do not enroll, it is possible that the treatments that are most studied (i.e., long-term behavioral programs, individual behavior therapy, and pharmacological interventions) may not be those that are most attractive to consumers.
Acknowledgments
The authors wish to acknowledge the contributions of Ted Blevins and Stacey Harris for their assistance with data management for this project.
REFERENCES
- 1.World Health Organization. Report of a WHO Consultation on Obesity. Geneva: World Health Organization; 1998. Obesity: Preventing and Managing the Global Epidemic. [PubMed] [Google Scholar]
- 2.National Institute of Health and National Heart, Lung, and Blood Institute. Clinical guidelines in the identification, evaluation, and treatment of overweight and obesity in adults—the evidence report. Obes Res. 1998;6(Suppl 2):51S–210S. [PubMed] [Google Scholar]
- 3.Must A, Spadano J, Coakley EH, Field AE, Colditz G, Dietz WH. The disease burden associated with obesity. JAMA. 1999;282:1523–9. doi: 10.1001/jama.282.16.1523. [DOI] [PubMed] [Google Scholar]
- 4.Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530–8. doi: 10.1001/jama.282.16.1530. [DOI] [PubMed] [Google Scholar]
- 5.Hill JO. Dealing with obesity as a chronic disease. Obes Res. 1998;6(S1):34–8. doi: 10.1002/j.1550-8528.1998.tb00686.x. [DOI] [PubMed] [Google Scholar]
- 6.Anderson DA, Wadden TA. Treating the obese patient. Arch Fam Med. 1999;8:156–67. doi: 10.1001/archfami.8.2.156. [DOI] [PubMed] [Google Scholar]
- 7.Rippe JM. The case for the medical management of obesity: a call for increased physician involvement. Obes Res. 1998;6(S1):23–33. doi: 10.1002/j.1550-8528.1998.tb00685.x. [DOI] [PubMed] [Google Scholar]
- 8.Simkin-Silverman LR, Wing RR. Management of obesity in primary care. Obes Res. 1997;5:603–12. doi: 10.1002/j.1550-8528.1997.tb00582.x. [DOI] [PubMed] [Google Scholar]
- 9.Nawaz H, Adams ML, Katz DL. Weight loss counseling by health care providers. Am J Public Health. 1999;89:764–7. doi: 10.2105/ajph.89.5.764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wadden TA, Berkowitz RI, Vogt RA, Steen SN, Stunkard AJ, Foster GD. Lifestyle modification in the pharmacologic treatment of obesity: a pilot investigation of a potential primary care approach. Obes Res. 1997;5:218–26. doi: 10.1002/j.1550-8528.1997.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 11.O'Neil PM, Rogers R. Health care providers' unhealthy attitudes towards obese people. Weight Control Digest. 1998;8:762, 765–7. [Google Scholar]
- 12.Price JH, Desmond SM, Krol RA, Snyder FF, O'Connell JK. Family practice physicians' beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45. [PubMed] [Google Scholar]
- 13.Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight. JAMA. 1999;282:1576–8. doi: 10.1001/jama.282.16.1576. [DOI] [PubMed] [Google Scholar]
- 14.Kristellar JL, Hoerr RA. Physician attitudes toward managing obesity: differences among six specialty groups. Prev Med. 1997;26:542–9. doi: 10.1006/pmed.1997.0171. [DOI] [PubMed] [Google Scholar]
- 15.Wadden TA, Anderson DA, Foster GD, Bennett A, Steinberg C, Sarwer DB. Obese women's perceptions of their physicians' weight management attitudes and practices. Arch Fam Med. 2000;9:854–60. doi: 10.1001/archfami.9.9.854. [DOI] [PubMed] [Google Scholar]
- 16.O'Neil PM, Dansky BS, Kilpatrick DG, Brewerton TD. Effects of patient's degree overweight and race on physician behaviors to encourage weight loss. Obes Res. 1993;1:84S. [Google Scholar]
- 17.Yanovski SZ. A practical approach to treatment of the obese patient. Arch Fam Med. 1993;2:309–16. doi: 10.1001/archfami.2.3.309. [DOI] [PubMed] [Google Scholar]
- 18.Baran L, Alain M. Desir de controle et perte de poids./desire for control and weight loss. Science et Comportement. 1993;23:131–43. [Google Scholar]
- 19.Brownell KD. Dieting readiness. Weight Control Digest. 1990;1:5–9. [Google Scholar]
- 20.Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight loss maintenance. J Pers Soc Psychol. 1996;70:115–26. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- 21.Prochaska JO, DiClemente CC. Toward a comprehensive model of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors: Processes of Change. New York, NY: Plenum Press; 1986. pp. 3–27. [Google Scholar]
- 22.Fontaine KR. Predicting treatment seeking for overweight. J Nerv Ment Dis. 1999;187:248–50. doi: 10.1097/00005053-199904000-00010. [DOI] [PubMed] [Google Scholar]
- 23.Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001;23:2–10. doi: 10.1207/S15324796ABM2301_2. [DOI] [PubMed] [Google Scholar]