Abstract
OBJECTIVE
To investigate whether patients are influenced by the order in which they learn the risks and benefits of a treatment and whether this effect is attenuated by a treatment's associated risk and/or benefit.
DESIGN
Subjects were randomized to review 1 of 6 medical treatment information brochures.
SETTING
Waiting rooms of primary care physicians at an academic health center.
PARTICIPANTS
Six hundred eighty-five subjects, ages 18 to 70 years.
INTERVENTION
Subjects reviewed 1 of 3 treatments for symptomatic carotid artery disease. The first (aspirin) was low-risk/low-benefit, the second (carotid endarterectomy surgery) was high-risk/high-benefit, and the third (extracranial-to-intracranial bypass surgery) was high-risk but of unknown benefit. Patients were also randomized to receive information about risk either before or after benefit. Patients were asked to rate the favorability of the treatment on a scale of 0 to 100 and whether they would consent. Finally, subjects rated how their decisions were influenced by the risk and benefit information.
MAIN RESULTS
Subjects evaluating aspirin therapy were influenced by the order of the risk/benefit information. Those learning about risks after benefits had a greater drop in their favorability ratings than subjects learning about risks before benefits (−10.9 vs −5.2 on a 100-point scale; P = .02) and were less likely to consent (odds ratio, 2.27; P = .04). In contrast, subjects evaluating carotid endarterectomy and extracranial-to-intracranial bypass were not influenced by information order. When subjects were influenced by the order of information, they also reported that the treatment's risk had less influence on their decision making (P < .01).
CONCLUSIONS
When patients evaluate low-risk medical interventions, they may form less favorable impressions of the treatment and be less likely to consent to the treatment when they learn about the risks after the benefits. Order effects were not observed with high-risk treatments regardless of potential benefits.
Keywords: decision making, informed consent, information order
Patients make many decisions when obtaining care from physicians. One critical decision is whether to consent to a treatment recommendation. Patients making informed decisions about treatment options should receive balanced presentations about both the benefit and risk. Does the order of this information matter?
Human judgment is known to be sensitive to the order in which an individual receives information.1 Order can influence everyday judgments, such as the likeability of an individual,2 as well as judgments of great consequence, such as the determination of guilt by jurors.3 Sometimes, information early in a sequence can be more influential, an effect known as primacy.4 At other times, there is greater influence from information presented late in a sequence, an effect known as recency.5 Whether a primacy or a recency information effect is observed is thought to be related to the amount and complexity of this information.1 Research shows that physicians place more weight on items of clinical data when they learn them late in a diagnostic evaluation instead of at the beginning.6,7,8
While the effect of information order on physicians' decision-making has been documented, there is little research about the impact of information order on the decision-making of patients. Clearly, patients need to be informed about both the potential benefits and risks of proposed treatments. Ideally, the order in which this information is received should not bias their decisions. In preliminary research on this question, patients were found to be less favorable about a procedure and less likely to consent to it when they read about the risks after the benefits instead of before the benefits.9
Interestingly, this information order effect was observed when patients were asked about influenza immunization and screening sigmoidoscopy but was not observed when they were asked about carotid endarterectomy. These findings raised the possibility that the variability could be due to differences in risk associated with interventions, differences in benefits, or differences in familiarity with the diseases used in the scenarios.
To assess some of these factors, in the current study, we use a single disease (symptomatic carotid stenosis) but vary the recommended treatment. We then ask whether patients' judgments about these treatments depend upon the order in which they receive information about risks and benefits. Our specific research hypotheses are as follows:
An information order effect will be observed when the order of information about risks and benefits affects judgments about medical interventions. Patients will feel less favorable about a treatment when risks are learned following benefits than when risks are learned before benefits. Additionally, patients reviewing the risks after the benefits will be less likely to agree to a recommended treatment.
The effect of information order on decision making will be attenuated when patients evaluate treatments with large risk.
The effect of information order will be attenuated when patients evaluate treatments with large benefit.
METHODS
Men and women between the ages of 18 years and 70 years were recruited in the waiting room of primary care physicians' offices at an academic medical center. The subjects were seeking medical attention for a wide variety of reasons, not necessarily related to the problems described in the scenarios. Subjects were assigned, using a random number table, to one of two experimental arms. In one arm, subjects received brochures about the recommended treatment detailing the risk before the benefit (Order RB), and in the other experimental arm they received brochures detailing the risk after the benefit (Order BR). Non–English-speaking patients were excluded. The University of Iowa human subjects review board approved this research project, and written consent was obtained from all subjects.
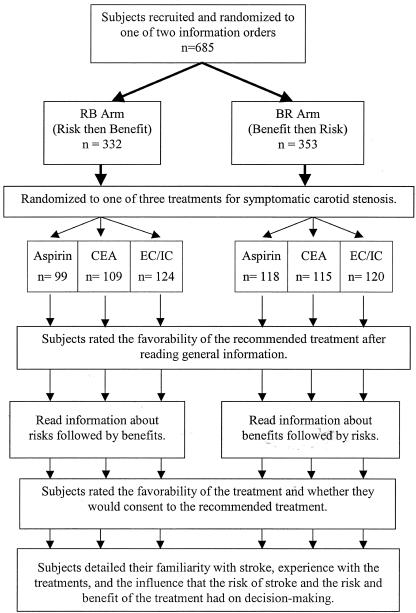
Subjects in the two experimental arms (Order RB and Order BR) were then randomized to 1 of 3 treatment scenarios. All scenarios involved a realistic but hypothetical health state involving a 20-minute episode of numbness of the face and right arm. In one scenario, subjects were asked to imagine that they had mild carotid stenosis (40% occlusion) and were advised to use life-long aspirin therapy. In the second scenario, subjects were asked to imagine that they had moderate carotid stenosis (80% occlusion) and were advised to undergo carotid endarterectomy surgery (CEA). In the third scenario, subjects were asked to imagine having near total carotid stenosis (over 99% occlusion) with stage II hemodynamic failure and were advised to undergo extracranial-intracranial bypass surgery (EC/IC).10 Thus, subjects were assigned to 1 of 6 groups determined by 3 carotid disease severity/treatment scenarios and 2 information orders. Within each disease severity/treatment scenario, subjects in both information order arms read exactly the same information although the order of this information was manipulated. A schematic of the experiment is shown in Figure 1.
FIGURE 1.
A schematic of the experiment.
After the subjects read general information about carotid stenosis and the recommended treatment, they rated the favorability of the recommended treatment on a scale extending from 0 (very negative) to 100 (very positive) with a midpoint of 50 (neutral). Subjects then reviewed the specific risks and benefits of their treatment in either BR or RB order and detailed information about what they could expect if they either agreed or did not agree to the recommended treatment.
In the aspirin scenario, the risk of stroke without intervention was described as 2% over 3 years, which could be reduced to 1% by the use of aspirin (i.e., number needed to treat [NNT] = 100).11 The risk associated with aspirin therapy was detailed as a 40% higher rate of gastrointestinal side effects, a 2-fold increase in risk of ulcers but still less than 1 in 1,000 per year, and 33% chance of bleeding problems although most would be minor. Finally, patients were told that aspirin users were twice as prone to intracerebral hemorrhage although still only 1 in 3,000 experienced this complication per year.
In the endarterectomy scenario, patients were told that they had a 12% risk of stroke but that this could be reduced to 5% through the use of CEA (NNT = 14).12 These subjects were told that they could expect a 2.5% chance of peri-operative stroke or death. In the EC/IC scenario, subjects were told that their risk of stroke without intervention was 33% and that the benefit of this procedure was undefined.10 EC/IC was presented as having a 10% risk of peri-operative stroke and death. Subjects evaluating CEA and EC/IC were told that the surgical procedure would result in at least an overnight stay in the intensive care unit, 1 week or less of hospitalization, and a 4- to 6-week recovery time.
After completing the entire informational brochure, subjects again rated the favorability of the treatment and were asked whether they would a) agree to undergo the recommended treatment, b) refuse, or c) request to delay making the decision. They also were asked to quantify, using a rating scale extending from 0 (no influence) to 100 (great influence), how the health risks associated with stroke and how the benefits and risks of the treatment each impacted their decision making. Finally, subjects assessed their familiarity with stroke on a 100-point scale (0 = “not at all familiar” to 100 = “very familiar”) and they were asked whether they had personally ever used long-term daily aspirin therapy or had undergone either CEA or EC/IC.
ANALYSIS
The subjects' perceptions of the treatment favorability, rated on the 100-point scale, were analyzed using parametric methods. For each disease severity/treatment scenario, the differences between the initial and final favorability ratings for the 2 information order arms were compared using a t test.
Additionally, the proportion of subjects who accepted each recommended treatment were compared across order condition using χ2 tests. Subjects who refused the recommended treatment or asked to delay making a decision were combined for this analysis. Acceptance of the treatment was also evaluated by logistic regression in order to adjust for personal experience with the intervention and initial favorability rating of the treatment. These factors were included as covariates because it was anticipated that personal experience with a treatment and initial feelings toward a procedure could influence judgments.
The perceived influences of the risks and benefits on judgments of each information order arm, within each disease severity/treatment scenario, were compared by t test. Analysis of variance was used to compare these influences across disease severity/treatment scenarios. Some treatment scenarios did not demonstrate an order effect, so an exploratory analysis was undertaken comparing the aggregated data on the reported influences of risks and benefits from the scenarios that did and did not demonstrate an order effect. A t test was used for this comparison. All tests were 2-sided with an α of 0.05.
RESULTS
Participants
Six hundred eighty-five patients completed the experiment. The entire group of subjects had a mean age of 37.9 (±14.4) years; 65% were women. Subjects reviewing each scenario were similar in terms of gender, age, and familiarity with stroke, as shown in Table 1. Similarly, within each treatment scenario, there was balance in terms of gender, age, and stroke familiarity between the 2 information order arms.
Table 1.
Description of the Subjects Who Evaluated 1 of 3 Treatment Scenarios for Symptomatic Carotid Stenosis*
| Subjects | Aspirin All, RB†/BR | CEA All, RB†/BR | EC/IC All, RB†/BR | P Value‡ |
|---|---|---|---|---|
| Age, y | 39.1, 38.7/39.6 | 37.8, 36.6/36.8 | 37.5, 35.6/39.3 | .22 |
| Familiarity with stroke, 0–100 | 62.4, 62.4/61.9 | 61.8, 62.5/61.2 | 58.7, 57.4/60.0 | .32 |
| Having used treatment, % | 22, 20/23 | 0, 0/0 | 0, 0/0 | <.001 |
Mean values for all subjects randomized to each treatment of stroke are shown first, followed by mean values in each of the two information order arms.
For each treatment of stroke, the characteristics of the subjects in the 2 information order arms (RB = Risk then Benefit Information, BR = Benefit then Risk Information) were not significantly different (P > .05).
P values are for comparison across treatment arms.
CEA, carotid endarterectomy surgery; EC/IC, extracranial-intracranial bypass surgery.
Aspirin Therapy
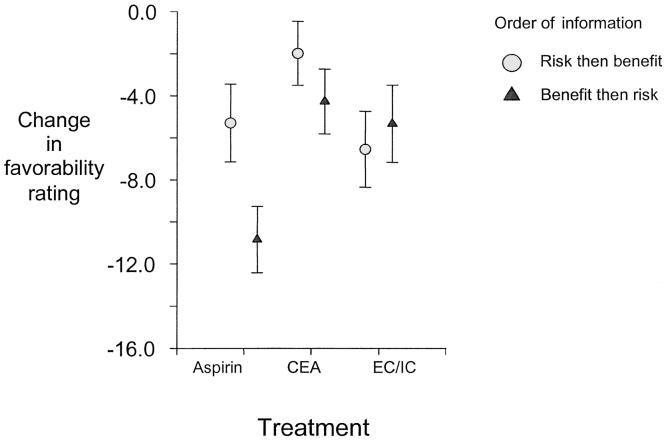
Two hundred seventeen subjects rated the favorability of using aspirin to prevent stroke in the face of a 40% internal carotid artery stenosis. After reading identical introductory information about the intervention, subjects in the 2 information order arms had similar favorability ratings (77.4 vs 76.5; P = .61). As shown in Figure 2, after reading detailed information about the treatment's risks and benefits, subjects in the BR arm showed a significantly greater drop in favorability ratings than did subjects in the RB arm (−10.9 vs −5.2; P = .02). This significant difference indicates that information about risk had more impact on subjects when learned after the benefit of the treatment than when the risk information was learned before benefit.
FIGURE 2.
Favorability rating change, in the 2 information order arms, by subjects reviewing aspirin, carotid endarterectomy (CEA), extracranial-intracranial bypass surgery (EC/IC) for stroke prevention. Change in rating represents the change in subjects' favorability ratings from first reviewing general information about their condition and the proposed treatment and then after reviewing detailed information about the risks and benefits of the treatment.
A greater percentage of subjects in the RB arm accepted aspirin than those in the BR arm. In the univariate analysis, this difference was not statistically significant (odds ratio [OR], 1.38; P = .29). However, this difference was statistically significant in the logistic model that adjusted for initial favorability ratings of this treatment and personal experience using long-term daily aspirin therapy (OR, 2.27; 95% confidence interval, 1.03 to 5.00; P = .04)
Carotid Endarterectomy Surgery
Two hundred twenty-four subjects were asked to evaluate the favorability of undergoing CEA in the face of an 80% internal carotid artery stenosis. Subjects in each order condition gave this intervention similar favorability ratings after reading the brief introductory information (74.4 for BR vs 75.1 for RB; P = .82). After reading the detailed risks and benefits, subjects in the 2 conditions had similar declines in favorability ratings (−4.2 for BR vs −1.9 for RB; P = .30) indicating that patients' judgments about the surgery were not significantly impacted by whether the risks were presented before or after the benefits.
Information order did not appear to affect whether subjects agreed to endarterectomy for their carotid artery disease. This was true in both the univariate analysis (OR, 1.31; P = .35) and in the logistic regression model (OR, 0.96; P = .92).
Extracranial-to-Intracranial Bypass Surgery
No order effect was observed for the 244 subjects asked to evaluate the favorability of EC/IC for stroke prevention in the face of near total internal carotid stenosis. Subjects in both information order arms gave this treatment similar favorability ratings after reading the brief introductory information about the health problem and intervention (67.8 for BR vs 70.4 for RB; P = .43). After reading the detailed risks and benefits, similar changes were observed in favorability ratings (−5.3 for BR vs −6.8 for RB; P = .70).
Subjects' willingness to consent to EC/IC surgery did not appear to be influenced by information presentation order. This was true for both the univariate analysis (OR, 1.1; P = .71) and the multivariate logistic regression (OR, 0.99; P = .98).
The Influence of Perceived Risks and Benefits
There were significant differences in the extent to which subjects reviewing the 3 treatment scenarios reported being influenced by the treatments' risks (P < .01) and benefits (P = .02); the perceived influence of the health risks associated with stroke did not differ significantly across scenarios (P = .12). As shown in Table 2, subjects reviewing the most risky treatment (EC/IC) reported the greatest influence from the risk of the intervention, while those in the aspirin group (the least risky treatment) reported the lowest. Subjects reviewing the CEA scenario reported the greatest influence from the benefit of the intervention and those reviewing the EC/IC scenario reported the lowest. The order of risk/benefit information did not impact these influence estimates (P > .05 within each scenario). These findings suggest that subjects ranked the riskiness and benefits of the treatments in an order consistent with the information in the brochures that they read.
Table 2.
The Perceived Influence of Risk and Benefit on Decision Making on a 100-point Scale*
| Influence on Decision | Aspirin All, RB†/BR | CEA All, RB†/BR | EC/IC All, RB†/BR | P Value‡ |
|---|---|---|---|---|
| Health risk associated with stroke | 78.1, 78.1/78.0 | 80.0, 79.3/80.7 | 75.5, 75.7/75.4 | .11 |
| Health risk associated with intervention | 55.4, 55.0/55.7 | 59.7, 57.8/61.5 | 63.1, 64.7/61.6 | <.01 |
| Health benefit associated with intervention | 76.5, 75.5/77.3 | 80.9, 79.0/82.6 | 75.3, 74.5/76.1 | <.05 |
0 = “No influence,” 100 = “great influence” as reported by subjects reviewing treatment scenarios for symptomatic carotid stenosis. Mean values for all subjects randomized to each treatment of stroke are shown first, followed by mean values in each of the 2 information order arms.
For each treatment of stroke, the influence of health risks and benefits on the decision making of subjects in the 2 information order arms (RB = Risk then Benefit Information, BR = Benefit then Risk Information) did not differ significantly (P > .05).
P values are for comparison across treatment arms. Within each treatment, there were no significant differences between the RB and BR order arms.
CEA, carotid endarterectomy surgery; EC/IC, extracranial-intracranial bypass surgery.
The reported influence of risk/benefit information was then compared between treatment scenarios that did and did not show an information order effect. Subjects evaluating the 2 surgical treatments (no order effect) reported that treatment risk had significantly greater influence on their decision making than did those subjects randomized to aspirin therapy (61.5 vs 55.4 on a 100-point scale; P < .01). However, there were no differences between the scenarios in the reported influence from treatment benefit on decision making (76.5 vs 78.0; P = .42) or from risk associated with stroke (78.1 vs 78.1; P = .83). These findings suggest that on the whole, risks had more influence on judged favorability of a treatment than did benefits, and that the order effect is more attenuated by risk information than by benefit information.
DISCUSSION
Patients generally desire to be involved in decisions concerning their medical care.13 One recurring judgment task is whether to agree to a physician's treatment recommendations. Because patients should review both the risks and the benefits of a treatment before giving consent, and because this information is necessarily processed sequentially, the order of presentation has a potential impact on their decision making.
Our research focused on 3 hypotheses. The first was that detailed risks presented after benefits would be more influential than if presented before benefits, that is, a recency information order effect. This order effect was observed with only 1 of the 3 treatment scenarios. However, there was no evidence that risk information was more influential when it was learned first, that is, there was no evidence of a primacy order effect in any treatment scenario. The second research hypothesis was that the information order effect would be attenuated by increased treatment risks; consistent with this, a significant information order effect was observed only with the low-risk treatment, aspirin therapy. The third research hypothesis was that the information order effect would be impacted by variations in treatment benefits. This hypothesis was not supported; the reported influence of treatment benefits on decision making did not differentiate those treatments that did and did not show order effects. Thus, it appears that risk but not benefit associated with treatments moderates the information order effect.
We also found that as subjects learned more about the risk and the benefit of a treatment, their favorability ratings declined, i.e., all the difference scores shown in Figure 2 are negative. Thus, our subjects tended to formulate less-favorable impressions of recommended treatments as they learned more about risks and benefits, indicating that, overall, risks affected judgments more than benefits. This overall decline in favorability in response to a balanced presentation of information is consistent with the known finding that humans tend to demonstrate “loss aversion.”14 That is, losses generally loom larger than gains in the sense that the loss of a given magnitude tends to be felt more than the same magnitude of gain. It is notable that in some cases, final impressions were more negative when subjects learned the risk of a treatment after the benefit.
The observed information order effect, one of recency, is consistent with results of over 30 previous experiments.1,6–9 It has been posited that this effect arises because people typically process sequential information by contrasting each new piece of evidence with their current opinion.1 In our decision-making task, patients are considering whether a proposed treatment, with its risks and benefits, will lead to a more favorable outcome. Information unsupportive of the intervention (information about complications) can seem very convincing when contrasted with a prior opinion based on the preceding supportive information (information about reduction in stroke).
We can think of several explanations for why increases in a treatment's risk will attenuate the information order effect. The first possibility is that when asked to consider a riskier treatment, patients are more careful or systematic in considering the information and think more deeply about both sides of the issue. Previous research shows that context effects, such as an order effect, tend to diminish when the decision maker is more involved and attentive.15 Subjects evaluating the high-risk procedures might have studied the brochure more carefully and re-read the information about the risks and benefits, thus minimizing any effect from the order of presentation. The brochures used in this experiment did not prevent this type of review. A second possibility is that the anxiety associated with considering risky treatments could block attention to the detailed information, resulting in a lesser tendency to contrast risk and benefit information.16 A third possibility is that when considering risky options, the risk becomes so salient that it just overwhelms the smaller effect of information order.17 A combination of these possibilities could also account for our results.
Although there is little prior research with patients on the effects of information order, our finding of interaction between risk and information order is consistent with research findings outside of medicine. For example, an analysis of voting patterns concluded that citizens are more likely to vote for the first-listed candidate in minor electoral races but order does not impact voting patterns in major races in which the stakes are higher.18 One might hypothesize that an explanation of the variable order effect arises from differences in familiarity that subjects report with the decision task. We observed an order effect only with the treatment that many subjects had personal experience with. However, earlier research suggests that familiarity with a decision task attenuates, rather than accentuates, the order effect.19
One may question the relevance of our findings to patients facing actual medical decisions because we did not study patients engaged in decision tasks that impacted their own health. Additionally, printed brochures were used to inform patients about the risk and benefit of recommended treatments, whereas most physicians typically deliver this type of information orally. However, the experimental task attained a high degree of realism. We recruited subjects who were actually visiting physicians' offices and thus were expecting to be involved in medical decisions. The information about risks and benefits was realistic, gathered through a search of the medical literature. Although providing risk/benefit information to patients in written form is routine only before patients are asked to consent to immunizations,20 it is possible that our use of brochures diminished the effect of information order. Because subjects could re-read the information about risks and benefits before making their decisions in our experiment, one might expect the order effect to be more evident in clinical settings in which oral presentations of this information are more typical.
In summary, because information order influences have been documented in many different settings, we thought it worthwhile to investigate if and when patients are influenced by the order of information about risks and benefits. On the basis of our findings, we anticipate that in some clinical situations, patients told about the benefits followed by the risks may form less favorable impressions because of the order effect, a clear example of biased judgment. From a clinical point of view, the good news is that the information order effect did not play a significant role in decisions about higher-risk treatments. However, information order may be influential when patients are considering low-risk treatments. Because many preventive interventions fall into this category, information order effects may have a significant health impact.
Prior work suggests a decision maker can systematically minimize errors in judgment through training.21,22 Further research is needed to assess whether it is possible to systematically de-bias patients, allowing them to make better decisions about their own health care.
REFERENCES
- 1.Hogarth RM, Einhorn HJ. Order effects in belief updating: the belief-adjustment model. Cognit Psychol. 1992;24:1–55. [Google Scholar]
- 2.Strang KR, Schwei M, Geiselman RE. Effects of the structure of descriptions on group impression formation. Bull Psychosom Soc. 1978;12:224–26. [Google Scholar]
- 3.Schadewald MS, Limberg ST. Effect of information order and accountability on causal judgments in a legal context. Psychol Rep. 1992;71:619–25. [Google Scholar]
- 4.Adelman L, Bresnick T, Black PK, Marvin FF, Sak SG. Research with Patriot air defense officers—examining information order effects. Hum Factors. 1996;38:250–61. [Google Scholar]
- 5.Tubbs RM, Gaeth GJ, Levin IP, VanOsdol LA. Order effects in belief updating with consistent and inconsistent evidence. J Behav Decis Making. 1993;6:257–69. [Google Scholar]
- 6.Bergus GR, Chapman GB, Gjerde C, Elstein AS. Clinical reasoning about new symptoms despite pre-existing disease: sources of error and order effects. Fam Med. 1995;27:314–20. [PubMed] [Google Scholar]
- 7.Chapman GB, Bergus GR, Elstein AS. Order of information affects clinical judgment. J Behav Decis Making. 1996;9:201–11. [Google Scholar]
- 8.Bergus GR, Chapman GB, Levy BT, Ely JW, Oppliger RA. Clinical diagnosis and the order of information. Med Decis Making. 1998;18:412–17. doi: 10.1177/0272989X9801800409. [DOI] [PubMed] [Google Scholar]
- 9.Bergus GR, Levin IP, Johnson C. The influence of information order on patient decision making. Med Decis Making. 1998;18:460. [Google Scholar]
- 10.Grubb RL, Jr, Derdeyn CP, Fritsch SM, et al. Importance of hemodynamic factors in the prognosis of symptomatic carotid occlusion. JAMA. 1998;280:1055–60. doi: 10.1001/jama.280.12.1055. [DOI] [PubMed] [Google Scholar]
- 11.Collaborative overview of randomised trials of antiplatelet therapy–I. Prevention of death, myocardial infarction, and stroke by prolonged antiplatelet therapy in various categories of patients. Antiplatelet Trialists' Collaboration. BMJ. 1994;308:81–106. [PMC free article] [PubMed] [Google Scholar]
- 12.North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991;325:445–53. doi: 10.1056/NEJM199108153250701. [DOI] [PubMed] [Google Scholar]
- 13.Guadagnoli E, Ward P. Patient participation in decision-making. Soc Sci Med. 1998;47:329–39. doi: 10.1016/s0277-9536(98)00059-8. [DOI] [PubMed] [Google Scholar]
- 14.Kahneman D, Tversky A. Prospect Theory: an analysis of decision under risk. Econometrica. 1979;47:263–91. [Google Scholar]
- 15.Smith SM, Levin IP. Need for cognition and choice framing effects. J Behav Decis Making. 1996;9:283–90. [Google Scholar]
- 16.Sanbonmatsu DM, Kardes FR. The effects of physiologic arousal on information processing and persuasion. J Consum Res. 1988;15:379–85. [Google Scholar]
- 17.Pham MT. Cue representation and selection effects of arousal on persuasion. J Consum Res. 1996;22:373–87. [Google Scholar]
- 18.Miller JM, Krosnick JA. The impact of candidate name order on election outcomes. Public Opin Q. 1998;62:291–330. [Google Scholar]
- 19.Wang H, Zhang J, Johnson TR. Human belief revision and order effect. Hillsdale, NJ: Erlbaum; 2000. Proceedings of the 22th Annual Conference of the Cognitive Science Society. [Google Scholar]
- 20.Instructions for the Use of Vaccine Information Statements. Available at: http://www.cdc.gov/nip/publications/vis/vis-Instructions.pdf, created 10/1/01. Accessed 01/06/02.
- 21.Lopes LL. Procedural debiasing. Acta Psychol (Amst) 1987;64:167–85. [Google Scholar]
- 22.Wang H. Order Effects in Human Belief Revision. Dissertation. Columbus, Ohio: The Ohio State University; 1998. [Google Scholar]