Abstract
Teaching medical students to integrate patient-centered skills into the medical interview is challenging. Longitudinal training requires significant curricular and faculty time. Unsupervised students risk harm if they uncover and inappropriately manage psychosocial issues in actual patients. They fear saying the wrong thing in emotionally charged situations. Two half-day workshops for pre-clinical students integrate patient- and physician-centered interviewing. The first occurs early in the first year. The second, late in the second year, presents interview challenges (e.g., breaking bad news). Ten professional actors portray standardized patients (SPs). Groups of 10 to 15 students interview an SP, each eliciting a part of the patient's story. Qualitative evaluation revealed that, for many students, SPs afford the opportunity to experiment without harming real patients. Students view the workshops as effective (mean score for first-year students, 6.6 [standard deviation (SD), 1.0], second-year students, 7.1 [SD, 0.7] on a Likert-type scale: 1 = not at all effective to 8 = very effective).
Keywords: physician-patient relations; communication; curriculum; teaching methods; interview methods; patient-centered care; education, medical
Patient-centered interviewing is associated with improved diagnostic accuracy,1,2 patient satisfaction,3 treatment adherence,4 and health outcomes,5 while poor interviewing skills are associated with patient dissatisfaction6 and malpractice suits.7–9 Patient-centered interviewing may also lead to improved efficiency10 and cost savings.11 Integrating patient-centered and more traditional physician-centered interviewing skills best elicits the patient's biopsychosocial story.12
Organizations such as the American Academy on Physician and Patient (AAPP) (http://www.physicianpatient.org) and the Bayer Institute for Health Care Communication (BIHCC) (http://www.bayerinstitute.org) teach practicing physicians to employ patient-centered skills. Residency training programs have successfully taught these skills to housestaff,13–18 but fewer than half of medical schools surveyed in 1991 taught aspects of patient-centered interviewing (e.g., doctor-patient relationship, biopsychosocial model, empathy).19 Indeed, teaching these skills in medical school presents unique challenges. Longitudinal training in patient-centered interviewing requires significant curricular and faculty time20—both in short supply at many medical schools.19 Unsupervised beginning students risk harm if they uncover and inappropriately manage psychosocial issues.21,22 They fear saying the wrong thing in emotionally charged situations.22,23 Actual patients may not be optimal for small-group teaching of patient-centered interview skills.24 Subjecting patients suffering psychological distress (e.g., terminal illness, sexual abuse) to novice interviewers raises ethical considerations. Without such training, however, students' psychosocial interviewing skills may actually worsen as they progress through medical school.25,26
We sought to address some of the challenges of teaching medical students integrated patient- and physician-centered interviewing by designing, implementing, and evaluating efficient half-day workshops using a small number of faculty, and professional actors as standardized patients (SPs). We chose the pre-clinical years to capitalize on students' early desire to communicate with patients. We designed the workshops so that students could learn in a safe, supportive atmosphere, free of concern about causing pain or making mistakes. We asked if students would view these workshops as effective and if they would accept and value the SP experience.
PROGRAM DESCRIPTION
At our institution, medical interview and physical examination skills are primarily taught by 60 faculty, who each meet with 4 students weekly for the first 2 years of medical school. Interview teaching is enhanced by 8 hour-long lecture/demonstrations for the first-year class.
Six general internist clinician-educators in the Department of Medicine with interest in doctor-patient communication founded the Interview Skills Working Group in early 1996. Our training included courses offered by AAPP and BIHCC. Because of limited classroom time in the pre-clinical years, our workshops, additions to the curriculum, were limited to one-half day each for the first- and second-year students.
We built our workshops with the following rationale:
The medical interview has 3 major functions: establishing rapport, obtaining information, and informing and educating the patient.27
A successful interview integrates doctor-centered and patient-centered approaches.28–34
Patient-centered interviewing skills (eg., listening, negotiating, responding to emotion empathically, and focusing the patient's story) can be taught.29
An interview with an SP allows students to work in small groups, reflect, share ideas, practice skills, give and receive feedback, and learn without causing harm, discomfort, or embarrassment to a real patient.21,22
As students advance through medical school, they learn skills in a developmentally appropriate, step-wise manner. Interview skills should also be approached this way, building on basic skills by offering more complex problems as students progress.
Our workshops use multidimensional SPs who can participate in a broad-ranging and in-depth interview. Each SP is represented by a 6-component scenario:
Presenting problems or concerns
Biomedical history
Family, personal, and social histories
A set of beliefs, attitudes, and preferences
Personality
Programmed responses to specified cues (e.g., cue: empathy; response: acknowledgment of a drinking problem)
Ideas for the 30 standardized patient scripts came from a variety of sources: patients known to one of us (FDH) (e.g., a young woman with a lingering cough leading to a new diagnosis of Hodgkin's disease); a disease, topic, or issue (e.g., somatization disorder, domestic violence, interviewing through an interpreter); a literary character (a salesman with multiple medical and psychosocial problems, modeled after Willy Loman in “Death of a Salesman”); and a character developed by one of the actors (a businesswoman whose routines are disrupted by the recent onset of asthma). The dialog is spontaneous. Scenarios are written in narrative form and are available from one of the authors (FDH).
Ten professional actors known as the Patient Players portray SPs. Each plays 2 to 4 characters of varying levels of complexity. As actors, our SPs can convincingly display a range of emotions and faithfully repeat a particularly difficult or moving scene, allowing for comparison of different approaches by students. Compared with lay people, SP actors may take less time to train.35 Finally, the SP actors can present more-or-less challenging problems, depending on the level of training of the students.
The Office of Education funds the workshops at a cost of approximately $3,000 per year. This covers program materials, snacks, and SP stipends.
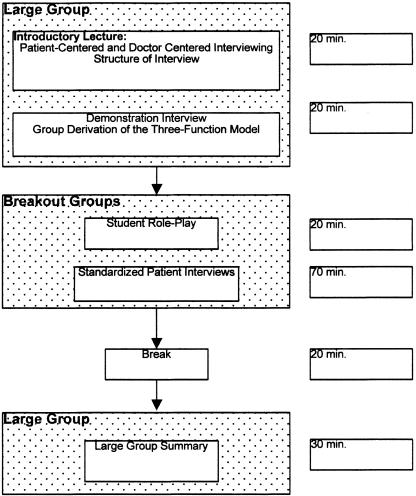
The first of two 3-hour workshops is offered in the first month of the first year of medical school when students are eager to start relating to patients and before they have been socialized into the culture and language of Medicine. The second workshop, in the last half of the second year presents a more sophisticated interview challenge. For each workshop, the entire class (about 100) is accommodated. Both workshops begin and end in a large-group setting (Fig. 1), but most of the time is devoted to the small breakout groups in which students take turns interviewing the SP.
FIGURE 1.
Format of workshop for first-year students.
In the workshop for first-year students (Fig. 1), a mini-lecture introduces patient-centered and doctor-centered interviewing and the importance of integrating the two styles.29 We review the structure of the medical interview (chief concern, history of present illness, past medical history, etc.); the students then derive the 3 functions of the interview27 by viewing a doctor-patient encounter role-played by faculty. The students watch as the doctor uses both patient-centered and physician-centered techniques to elicit the patient's story and concerns, respond to the emotional content of the interview with empathy, educate and reassure the patient, and negotiate an appropriate plan. The interview takes 5 to 10 minutes and reasonably reflects a “real-life” office encounter. The students' observations about what took place are used to help them actively discover the 3 functions of the medical interview. Having students observe faculty engaging in a role-play also seems to make them more at ease in participating in their own subsequent role-play.
The students then form breakout groups of 10 to 15, each led by a faculty facilitator (Fig. 1). They begin with a brief role-play, done in triads consisting of a patient, a physician, and an observer. The “physician” is privately instructed to conduct two 5-minute interviews, one in a strictly doctor-centered style using only closed-ended questions, and the second in a patient-centered, open-ended style. The “patient” and observer are unaware of the intent. The triads then regroup to discuss the differences noted in the two interviews from each participant's perspective. The group is able to discover the strengths and weaknesses of each technique and the usefulness of an integrated approach, which is encouraged for the SP interview that follows.
In the SP interview, students take turns as the “physician.” We allow about 60 minutes for the interview and another 10 minutes for discussion with the SP. Each student has 7 to 10 minutes to elicit a part of the patient's story, allowing for about half the students in the group to interview. The SP can “rewind” so that an interviewer can try a new technique. The students can see which techniques are more successful and learn from their classmates. At the end of the interview, the SP offers nonjudgmental reactions to what was said and done,30 for example, “My character is a very scared and lonely person who responds well to your soothing tone of voice.”
For second-year students, the mini-lecture focuses on interview challenges. There is no demonstration interview or student role-play. The SP presents a more sophisticated interview problem, e.g., the interviewer must break the news that a recent chest x-ray, done for a persistent cough, shows a tumor, or deal with an angry patient.
In both years, after the SP interview, each breakout group reports to the large group on the nature of their physician-patient encounter and on the specific skills they learned. The students give a frank presentation of which techniques worked and which did not. They hear about interview skills that may not have been used in their own breakout group. They are also able to share emotional reactions they may have had to the interview process.
PROGRAM EVALUATION
The major outcome we examined was students' perceptions of the workshop's effectiveness. They completed an evaluation form at the end of each workshop, assessing the effectiveness of each workshop component (Fig. 1) (i.e., introductory lecture, demonstration interview, student role-play, SP interview, large-group summary) and the workshop overall, with a Likert-type rating scale (1 = not at all effective to 8 = very effective). We analyzed data using SPSS-PC Base 10.0 for Windows (SPSS, Inc., Chicago, Ill). Means and standard deviations were calculated on the individual program evaluation items.
Students were also asked to write about what they learned from the workshop, how the standardized patients contributed to their learning, strengths of the workshop, and suggestions for further improvement. We qualitatively analyzed their comments and derived mutually exclusive categories of responses for each question. Percent frequency of these response categories for the 1999–2000 academic year is reported.
As Table 1 illustrates, the overall workshop was rated highly. The most effective aspects of the workshop were the SP interview, with a mean rating of 7.5 from first-year students and 7.8 from second-year students. Students perceived the introductory lectures as less effective (mean rating of 5.5 from first-year students and 5.7 from second-year students).
Table 1.
Mean Ratings of Workshop Components for 1999–2000 Academic Year
| Mean Effectiveness (SD) (Rating Scale: 1 = Not at All Effective to 8 = Very Effective) | ||
|---|---|---|
| Interview Skills Workshop Components | First-year Students (N = 91) | Second-year Students (N = 36) |
| Introductory lecture | 5.5 (1.5) | 5.7 (1.6) |
| Demonstration interview | 6.1 (1.3) | NA |
| Student role play | 6.4 (1.3) | NA |
| Standardized patient interview | 7.5 (1.0) | 7.8 (0.6) |
| Large group summary | 5.4 (2.0) | 6.1 (1.8) |
| Overall workshop evaluation | 6.6 (1.0) | 7.1 (0.7) |
NA, not applicable.
Table 2 reports the percent frequency of the response categories derived from the students' written comments. Students most frequently cited interview skills and techniques as the area that they learned most about. Approximately a third of students in each year said they learned the most about the psychosocial/relational aspects of the encounter. Both first- and second-year students indicated that the SPs contributed to their learning by giving them the opportunity to experiment, critique, and analyze their interviewing skills without harming real patients. First-year students tended more to feel that the SPs provided a real-life context. Second-year students felt more that the SPs were important in providing them feedback and allowing them to address psychosocial issues. The workshop strengths noted by both first- and second-year students were the SPs and the opportunity to practice interviewing skills. First-year students cited the role-play. Second-year students noted learning how to address psychosocial issues. Areas for workshop improvement included having smaller groups, more SPs and more time with them, and having the workshops more often. The least effective workshop component cited was the introductory lecture.
Table 2.
Percent Frequency of Response Categories Derived from Written Comments for 1999–2000 Academic Year
| Frequency of Responses by Category, % | ||
|---|---|---|
| Response Categories | First-year Students | Second-year Students |
| What did you learn from the workshop? | ||
| Interviewing skills and techniques | 50 | 41 |
| Relationship building/psychosocial perspectives | 30 | 36 |
| Fund of knowledge | 20 | 23 |
| How did SP contribute to teaching? | ||
| Provided place for experimentation, analysis, and critique of interviewing skills | 44 | 37 |
| Provided “real life” context | 30 | 16 |
| Provided opportunity to give feedback | 15 | 26 |
| Allowed opportunity to address psychosocial/relationship issues | 11 | 21 |
| Strengths of workshop | ||
| Standardized patients | 29 | 44 |
| Role play | 20 | NA |
| Small-group discussion | 18 | 11 |
| Ability to practice interviewing skills | 15 | 28 |
| Large-group discussion | 9 | — |
| Faculty involvement/commitment | 9 | — |
| Address psychosocial issues | — | 17 |
| How can workshop be improved? | ||
| Have smaller groups | 27 | 25 |
| Have workshops more often | 23 | 31 |
| Have more standardized patients | 17 | 19 |
| Reduce/improve lecture components | 17 | 12 |
| No need for improvement | 9 | — |
| More time to participate with SPs | 7 | 13 |
NA, not applicable.
DISCUSSION
These brief, multi-modal hands-on workshops in the pre-clinical years are well-received and viewed as effective by students. They accept the use of standardized patients and find working with them in small groups with a faculty facilitator to be the high point of the workshops. Strengths of teaching this material in a workshop format include efficiency of both time and faculty effort; the opportunity for students to learn skills from one another; realistic, experiential learning without having to worry about harming patients (a universal concern of beginning students), and immediate feedback from the SPs. Teaching this material starting early in the first year allows us to capture student interest, emphasize the importance of patient-centeredness and draw on students' natural relational and conversational ability unencumbered by medical jargon and socialization.
Weaknesses of the workshops, as indicated by students' evaluations, include too much time spent in the large group (an introductory lecture that was initially too long and a summary session that was not as valuable to learners as more time with SPs would have been). Students desire smaller groups, and more SPs in each session. Presenting this important material in only one afternoon must also be seen as a weakness; indeed students often requested more such workshops.
The evaluation instrument allowed us to assess students' perceptions of the effectiveness of individual workshop components, allowing us to fine-tune the experience. Qualitative data also provided insights into perceived strengths and weaknesses of the workshops. Weaknesses of our evaluation include no measurement of the workshop's impact on interviewing skills or students' attitudes toward patient-centered interviewing.
Because of the popularity of these workshops and students' expressed desire for more, we have secured support to recruit and train more faculty and SPs in order to present one more workshop in each pre-clinical year, with smaller groups and more time with the SPs. We also are expanding this program into the clinical years of medical training. Workshops in the third- and fourth-year will allow us to present these clinically advanced students with even more sophisticated interview challenges (e.g., developing awareness of negative attitudes,22,36 end-of-life communication skills37) to reinforce and enhance their skills, hopefully preventing atrophy.25,26 By directly observing their interactions with SPs we can assess improvement in students' ability to apply these skills and their attitude toward integrated interviewing. We plan to observe fourth-year students in actual patient encounters in order to assess retention and use of these skills in a clinical setting.18 Finally, we are providing training to the 60 faculty who teach the longitudinal component of the physical diagnosis course to reinforce integrated interviewing skills throughout the course.
We were challenged to highlight the important area of integrated patient- and doctor-centered interviewing in one half day of curricular time per pre-clinical year. Because of the use of a developmental model, multiple teaching methods, a small core of skilled faculty, and hands-on experience, students view these popular workshops as effective and they want more of them.
Our greatest challenge, faced by many medical schools, has been to integrate the psychosocial aspects of medicine into the larger curriculum.38 By extending this program into the clinical years, we are taking steps to assimilate patient- and physician-centered interviewing throughout the 4-year curriculum, emphasizing the importance of these skills in becoming a mature physician.
Acknowledgments
The authors thank Patrick O'Connor, MD and Anna Reisman, MD for reviewing earlier drafts of this manuscript, the Students of Yale University School of Medicine, and The Patient Players.
REFERENCES
- 1.Beckman HB, Frankel RM. The effect of physician behavior on the collection of data. Ann Intern Med. 1984;101:692–6. doi: 10.7326/0003-4819-101-5-692. [DOI] [PubMed] [Google Scholar]
- 2.Marvel MK, Epstein RM, Flowers K, Beckman HB. Soliciting the patient's agenda: have we improved. JAMA. 1999;281:283–7. doi: 10.1001/jama.281.3.283. [DOI] [PubMed] [Google Scholar]
- 3.Korsch BM, Gozzi EK, Francis V. Gaps in doctor-patient communication. 1. Doctor-patient interaction and patient satisfaction. Pediatrics. 1968;42:855–71. [PubMed] [Google Scholar]
- 4.DiMatteo MR, DiNicola DD. Achieving Patient Compliance: The Psychology of the Medical Practitioner's Role. New York: Pergamon Press; 1982. [Google Scholar]
- 5.Kaplan SH, Greenfield S, Ware J. Impact of the doctor-patient relationship on the outcomes of chronic disease. In: Stewart M, Roter D, editors. Communicating with Medical Patients. Newbury Park: Sage; 1989. [Google Scholar]
- 6.Roter DL, Hall JA, Katz NR. Relations between physicians' behaviors and analogue patients' satisfaction, recall, and impressions. Med Care. 1987;25:437–51. doi: 10.1097/00005650-198705000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Vaccarino JM. Malpractice. The problem in perspective. JAMA. 1977;238:861–3. doi: 10.1001/jama.238.8.861. [DOI] [PubMed] [Google Scholar]
- 8.Sommers PA. Malpractice risk and patient relations. J Fam Pract. 1985;20:299–301. [PubMed] [Google Scholar]
- 9.Beckman HB, Markakis KM, Suchman AL, Frankel RM. The doctor-patient relationship and malpractice. Lessons from plaintiff depositions. Arch Intern Med. 1994;154:1365–70. [PubMed] [Google Scholar]
- 10.Bergh KD. Time use and physicians' exploration of the reason for the office visit. Fam Med. 1996;28:264–70. [PubMed] [Google Scholar]
- 11.Friedman R, Sobel D, Myers P, Caudill M, Benson H. Behavioral medicine, clinical health psychology, and cost offset. Health Psychol. 1995;14:509–18. doi: 10.1037//0278-6133.14.6.509. [DOI] [PubMed] [Google Scholar]
- 12.Smith RC, Hoppe RB. The patient's story: integrating the patient- and physician-centered approaches to interviewing. Ann Intern Med. 1991;115:470–7. doi: 10.7326/0003-4819-115-6-470. [DOI] [PubMed] [Google Scholar]
- 13.Lipkin M, Quill TE, Napodano RJ. The medical interview: a core curriculum for residencies in internal medicine. Ann Intern Med. 1984;100:277–84. doi: 10.7326/0003-4819-100-2-277. [DOI] [PubMed] [Google Scholar]
- 14.Langewitz WA, Eich P, Kiss A, Wossmer B. Improving communication skills—a randomized controlled behaviorally oriented intervention study for residents in internal medicine. Psychosom Med. 1998;60:268–76. doi: 10.1097/00006842-199805000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Davies M. The way ahead: teaching with simulated patients. Med Teach. 1989;11:315–20. doi: 10.3109/01421598909146419. [DOI] [PubMed] [Google Scholar]
- 16.Smith RC, Lyles JS, Mettler J, et al. The effectiveness of intensive training for residents in interviewing. A randomized, controlled study. Ann Intern Med. 1998;128:118–26. doi: 10.7326/0003-4819-128-2-199801150-00008. [DOI] [PubMed] [Google Scholar]
- 17.Yeheskel A, Biderman A, Borkan JM, Herman J. A course for teaching patient-centered medicine to family medicine residents. Acad Med. 2000;75:494–7. doi: 10.1097/00001888-200005000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Oh J, Segal R, Gordon J, Boal J, Jotkowitz A. Retention of patient-centered interviewing skills after intensive training. Acad Med. 2001;76:647–50. doi: 10.1097/00001888-200106000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Novack DH, Volk G, Drossman DA, Lipkin M., Jr Medical interviewing and interpersonal skills teaching in US medical schools. Progress, problems, and promise. JAMA. 1993;269:2101–5. [PubMed] [Google Scholar]
- 20.Werner A, Schneider JM. Teaching medical students interactional skills. A research-based course in the doctor-patient relationship. N Engl J Med. 1974;290:1232–7. doi: 10.1056/NEJM197405302902206. [DOI] [PubMed] [Google Scholar]
- 21.Barrows HS. An overview of the uses of standardized patients for teaching and evaluating clinical skills. AAMC. Acad Med. 1993;68:443–53. doi: 10.1097/00001888-199306000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Smith RC. Teaching interviewing skills to medical students: the issue of ‘countertransference’. J Med Educ. 1984;59:582–8. doi: 10.1097/00001888-198407000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Batenburg V, Gerritsma JG. Medical interviewing: initial student problems. Med Educ. 1983;17:235–9. doi: 10.1111/j.1365-2923.1983.tb01456.x. [DOI] [PubMed] [Google Scholar]
- 24.Simek-Downing L, Quirk ME, Letendre AJ. Simulated versus actual patients in teaching medical interviewing. Fam Med. 1986;18:358–60. [PubMed] [Google Scholar]
- 25.Helfer RE. An objective comparison of the pediatric interviewing skills of freshman and senior medical students. Pediatrics. 1970;45:623–7. [PubMed] [Google Scholar]
- 26.Helfer RE, Ealy KF. Observations of pediatric interviewing skills. A longitudinal and cross-sectional study. Am J Dis Child. 1972;123:556–60. doi: 10.1001/archpedi.1972.02110120080006. [DOI] [PubMed] [Google Scholar]
- 27.Bird J, Cohen-Cole SA. The three-function model of the medical interview. An educational device. Adv Psychosom Med. 1990;20:65–88. [PubMed] [Google Scholar]
- 28.Smith RC, Lyles JS, Mettler JA, et al. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70:729–32. doi: 10.1097/00001888-199508000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Smith RC. Patient Centered Interviewing. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2002. [Google Scholar]
- 30.Lipkin M, Putnam SM, Lazare A. The Medical Interview: Clinical Care, Education, and Research. New York: Springer-Verlag; 1995. [Google Scholar]
- 31.Suchman AL, Markakis K, Beckman HB, Frankel R. A model of empathic communication in the medical interview. JAMA. 1997;277:678–82. [PubMed] [Google Scholar]
- 32.Engel GL. From biomedical to biopsychosocial. Being scientific in the human domain. Psychosomatics. 1997;38:521–8. doi: 10.1016/S0033-3182(97)71396-3. [DOI] [PubMed] [Google Scholar]
- 33.Roter DL, Hall JA, Kern DE, Barker LR, Cole KA, Roca RP. Improving physicians' interviewing skills and reducing patients' emotional distress. A randomized clinical trial. Arch Intern Med. 1995;155:1877–84. [PubMed] [Google Scholar]
- 34.Matthews DA, Suchman AL, Branch WT., Jr Making “connexions": enhancing the therapeutic potential of patient-clinician relationships. Ann Intern Med. 1993;118:973–7. doi: 10.7326/0003-4819-118-12-199306150-00010. [DOI] [PubMed] [Google Scholar]
- 35.Meier RS, Perkowski LC, Wynne CS. A method for training simulated patients. J Med Educ. 1982;57:535–40. doi: 10.1097/00001888-198207000-00005. [DOI] [PubMed] [Google Scholar]
- 36.Smith RC, Marshall Dorsey A, Lyles JS, Frankel RM. Teaching self-awareness enhances learning about patient-centered interviewing. Acad Med. 1999;74:1242–8. doi: 10.1097/00001888-199911000-00020. [DOI] [PubMed] [Google Scholar]
- 37.von Gunten CF, Ferris FD, Emanuel LL. Ensuring competency in end-of -life care: communication and relational skills. JAMA. 2000;284:3051–7. doi: 10.1001/jama.284.23.3051. [DOI] [PubMed] [Google Scholar]
- 38.Brody H. Relationship-centered care: beyond the finishing school. J Am Board Fam Pract. 1995;8:416–8. [PubMed] [Google Scholar]