Abstract
OBJECTIVE
Individuals with peripheral arterial disease (PAD) have a 3- to 6-fold increased risk of coronary heart disease and stroke compared to those without PAD. We documented physician-reported practice behavior, knowledge, and attitudes regarding atherosclerotic risk factor reduction in patients with PAD.
DESIGN
National physician survey.
PATIENTS/PARTICIPANTS
General internists (N = 406), family practitioners (N = 435), cardiologists (N = 473), and vascular surgeons (N = 264) randomly identified using the American Medical Association's physician database.
MEASUREMENTS AND MAIN RESULTS
Physicians were randomized to 1 of 3 questionnaires describing a) a 55- to 65-year-old patient with PAD; b) a 55- to 65-year-old patient with coronary artery disease (CAD), or c) a 55- to 65-year-old patient without clinically evident atherosclerosis (no disease). A mailed questionnaire was used to compare physician behavior, knowledge, and attitude regarding risk factor reduction for each patient. Rates of prescribed antiplatelet therapy were significantly lower for the patient with PAD than for the patient with CAD. Average low-density lipoprotein levels at which physicians “almost always” initiated lipid-lowering drugs were 121.6 ± 23.5 mg/dL, 136.3 ± 28.9 mg/dL, and 149.7 ± 24.4 mg/dL for the CAD, PAD, and no-disease patients, respectively (P < .001). Physicians stated that antiplatelet therapy (P < .001) and cholesterol-lowering therapy (P < .001) were extremely important significantly more often for the CAD than for the PAD patient. Perceived importance of risk factor interventions was highly correlated with practice behavior. Compared to other specialties, cardiologists had lowest thresholds, whereas vascular surgeons had the highest thresholds for initiating cholesterol-lowering interventions for the patient with PAD. Cardiologists were significantly more likely to report “almost always” prescribing antiplatelet therapy for the patient with PAD than were all other physicians.
CONCLUSIONS
Deficiencies in physician knowledge and attitudes contribute to lower rates of atherosclerotic risk factor reduction for patients with PAD. Reversing these deficiencies may reduce the high rates of cardiovascular morbidity and mortality associated with PAD.
Keywords: peripheral vascular disease, quality of care, cardiovascular disease
Lower extremity peripheral arterial disease (PAD) affects 20% to 30% of men and women age ≥50 years in general medicine practices,1–3 making PAD a problem commonly encountered by physicians. Persons with PAD have a 3- to 5-fold increased risk of cardiovascular disease (CVD) mortality compared to persons without PAD.4–7 The risk of CVD morbidity and mortality in PAD is comparable to that in coronary artery disease (CAD).8,9 An association between PAD and future CVD events is well-established, even among PAD persons without clinically evident CVD.7 Because of the strong, consistent association between PAD and future CVD events, the American Heart Association (AHA) and the National Cholesterol Education Program (NCEP) recommend equally intensive atherosclerotic risk factor reduction for PAD and CAD patients.6,8,10–12
Previous studies indicate that patients with PAD are undertreated for atherosclerotic risk factors.3,13–15 In the PAD Awareness, Risk, and Treatment: New Resources for Survival (PARTNERS) program, PAD was identified via anchor branchial complex screening in 29% of 6,979 older patients in 350 general medicine practices across the United States.3 Compared to participants with CVD diseases other than PAD, PAD participants in PARTNERS were treated less frequently for hypertension and hyperlipidemia and received antiplatelet therapy less often.3 Such undertreatment may contribute to high rates of CVD morbidity and mortality in PAD.
Reasons for undertreatment of atherosclerotic risk factors in patients with PAD are unknown. One possible explanation is that physicians may be unaware of the high rate of CVD morbidity and mortality or the importance of risk factor reduction in PAD. To our knowledge, no previous studies have compared physician-reported knowledge, attitudes, and practice behavior regarding the importance of atherosclerotic risk factor reduction between a patient with PAD and a patient with CAD or a patient with no clinically evident atherosclerosis. We addressed these matters in a national physician survey. We hypothesized that physicians would report less-intensive atherosclerotic risk factor reduction for a patient with PAD than for a patient with CAD and that physicians would report more-intensive atherosclerotic risk factor reduction for a patient with PAD than for a patient without clinically evident atherosclerosis. We further hypothesized that physicians' knowledge and attitudes regarding the risk of CVD events and the importance of atherosclerotic risk factor reduction would be less for a patient with PAD than for a patient with CAD. Finally, we hypothesized that physicans' knowledge and attitudes regarding the importance of atherosclerotic risk factor intervention would correlate significantly with intensity of their reported risk factor intervention behavior.
METHODS
Sampling Frame and Sample Selection
The Institutional Review Board of Northwestern University's Feinberg School of Medicine approved the study protocol. We used the American Medical Association (AMA) and American Osteopathic Association (AOA) databases to construct the sampling frame of U.S. physicians. These databases are the most comprehensive lists available and include all U.S. physicians, Medical Doctors and Doctors of Osteopathy, members and nonmembers of the AMA and AOA. We studied general internists, cardiologists, vascular surgeons, and family physicians because PAD patients most frequently identify these physicians as their primary physician.13 To achieve a sample size of 1,500 participants, we randomly selected 5,119 physicians from the database, after stratifying by physician specialty.
Inclusion and Exclusion Criteria
We included nonretired physicians engaged in 10 or more hours of direct patient care per week. We excluded physicians-in-training and physicians whose primary professional activity was in research, teaching, or administration to ensure that our results would be generalizable to attending-level clinicians who commonly care for PAD patients.
Questionnaires
The study questionnaire measured domains of the Theory of Planned Behavior, a theoretical model that is commonly used to explain behavior.16–18 The Theory of Planned Behavior proposes that the best predictor of a behavior is the behavioral intention to perform it and that behavioral intentions are driven primarily by a) knowledge and attitudes, b) the desire to conform to social norms, and c) perceived behavioral control. Perceived behavioral control represents one's degree of control over the desired behavior when behavior is not completely under volitional control.
The primary aim of this study was to compare physicians' behavior, knowledge, and attitudes regarding atherosclerotic risk factor reduction for patients with PAD, patients with CAD, and patients with no atherosclerotic disease. Just 2 domains of the theory of planned behavior address this primary study aim. For the first domain of current physician practice, we queried physicians about their reported current practice behavior for a specific hypothetical patient. The second domain was physicians' knowledge and attitudes regarding the importance and benefit of atherosclerotic risk factor reduction for the hypothetical patient. Another component of this domain was measuring physicians' knowledge of the association between PAD and future CVD risk. Because our pilot data showed suboptimal atherosclerotic risk factor reduction for antiplatelet therapy, cholesterol lowering, and exercise, we focused on these behaviors in addition to cigarette smoking.13 We also studied behavior regarding prescription of a supervised exercise program, because available data for PAD indicate that supervised exercise programs are superior to unsupervised exercise.19
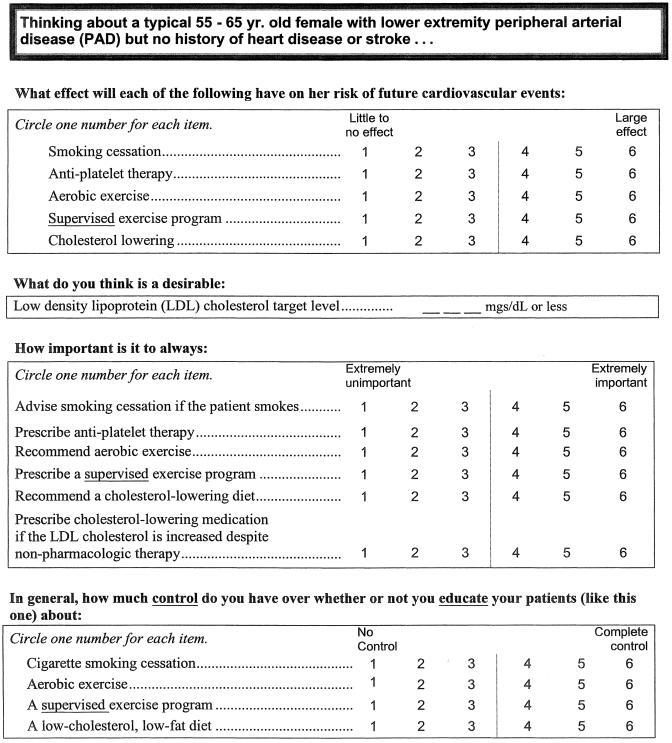
Three 7-page questionnaires, each describing 3 hypothetical patients, were developed (see sample page of questionnaire in Fig. 1). The questions in each were identical, but the hypothetical patient differed. The 3 hypothetical patients were: a) a 55- to 65-year-old patient with PAD and no other clinically evident atherosclerosis; b) a 55- to 65-year-old patient with CAD and no other clinically evident atherosclerosis; and c) a 55- to 65-year-old patient without any clinically evident atherosclerosis. For each patient, half of the questionnaires described a female and half described a male patient. We studied CVD risk factor treatments recommended by the NCEP and the AHA at the time of the data collection, between February 1, 2000 and January 31, 2001. Specifically, AHA and NCEP recommendations for patients with PAD were prescription of antiplatelet therapy, regular aerobic exercise (preferably supervised exercise), smoking cessation if the patient smokes, and lowering low-density lipoprotein (LDL) cholesterol to <100 mg/dL.6,10–12 NCEP guidelines for patients with PAD or CAD included prescription of cholesterol-lowering diet therapy for LDL cholesterol levels ≥100 mg/dL and prescription of cholesterol-lowering drug therapy for LDL cholesterol levels ≥130 mg/dL.10,11 The 2002 U.S. Preventive Services Task Force guidelines on aspirin and primary prevention of cardiovascular events were not published at the time of data collection.20
FIGURE 1.
Sample page of study questionnaire.
Physicians were asked to rank the likelihood that they would prescribe each specific therapy on a Likert scale ranging from 1 to 6. The Likert scale was structured such that a response of 1 represented “almost never” and a response of 6 represented “almost always” with remaining numerical scores representing a range of prescribing patterns between “almost never” and “almost always”. This variable was dichotomized into a score of “6” versus “less than 6.” We dichotomized the variable in this way because a response of “almost always” for frequency of risk factor treatment is most consistent with current guidelines regarding atherosclerotic risk factor treatment for patients with PAD. We dichotomized Likert scale questions on knowledge and attitudes regarding atherosclerotic risk factor treatment similarly, using a “6” to indicate that treating a particular risk factor had a “large effect” or was “extremely important” for cardiovascular risk prevention.
Mailings to Sampled Physicians
Because vascular surgeons do not typically care for CAD patients without other vascular disease or patients without evidence of atherosclerosis, all vascular surgeons were randomized to receive 1 of the 2 questionnaires (male or female) describing the patient with PAD and were mailed their questionnaire directly. Vascular surgeons were asked to return their questionnaire, indicating whether they met eligibility criteria and whether they were willing to participate, even if they did not complete the questionnaire.
Nonsurgeons were randomized to receive a questionnaire describing 1 of the 3 patients. To ensure the questionnaires were distributed equally among specialties, we sent a stamped, addressed postcard to sampled nonsurgeons on which they indicated their eligibility and willingness to participate. Upon receipt of each postcard indicating that a physician was eligible and willing to participate, he/she was randomized to receive a questionnaire describing 1 of the 3 patient types (either male or female).
Incentives
Up to 4 mailings were completed for each sampled physician. All mailings to vascular surgeons included questionnaires, whereas for nonsurgeons, the first 2 mailings were postcards and the third and fourth mailings were questionnaires as described below. Because response rates were initially lower than anticipated, we implemented 3 strategies at the time of the third mailing to increase response rates. First, for nonsurgeons, we eliminated the postcard mailing because response rates from surgeons (who did not receive a postcard) were substantially greater than from nonsurgeons (who received a postcard). In addition, our final survey response rate was necessarily limited by the postcard response rate. Physicians who had not returned their postcard when this change was made were randomized and mailed their questionnaire directly. The second strategy was inclusion of a $5 bill with the mailed questionnaires.21,22 The third strategy was provision of the opportunity to apply for Continuing Medical Education (CME) credit after questionnaire completion. Physicians who previously completed the questionnaire were mailed a $5 bill “thank you” token and were offered the opportunity to receive CME credit.
Statistical Analyses
Characteristics between the 4 specialties, comparisons between physician responses for the first 3 patient types regarding knowledge and attitudes, and comparisons of current behavior, knowledge, and attitudes across 4 specialties for the PAD questionnaire were made using standard statistical tests for continuous and categorical data. Because of the multiple outcomes tested, we chose a statistical significance level of P < .01 as the criterion for overall comparisons between the 3 patient types and 4 specialty groups. Pairwise comparisons were made between the PAD and CAD patient and between the PAD and the no-disease patient using the Bonferroni inequality to adjust for multiple comparisons (P < .01/2 = P < .005).23 Six pairwise comparisons were performed for physician specialties using Bonferroni adjustment (P < .01/6 = P < .002).
Univariate logistic regression analyses and univariate linear regression analyses were performed to determine associations between patient type (independent variable) and current behavior (dependent variable). Multivariable logistic regression analyses and multivariable linear regression analyses were performed to determine the independent associations between patient type (independent variable) and current behavior (dependent variable), adjusting for patient gender and physician specialty, age, gender, board certification status, and race (white versus nonwhite). In these analyses, odds ratios and regression coefficients were estimated for the patient with PAD and the patient with no disease, respectively, in reference to the patient with CAD. Finally, to determine whether differences in physician attitude and knowledge regarding the effects and importance of treating atherosclerotic risk factors mediated differences in current behavior between patient types, we repeated multivariable logistic regression analyses and multivariable linear regression analyses adjusting for attitudes and knowledge in addition to the aforementioned variables. In these analyses, Likert scale responses for attitudes and knowledge were collapsed into 1 of 3 categories: a) Likert scale score of 1 to 4; b) Likert scale score of 5; c) Likert scale score of 6.
Analyses were performed separately for all physicians and for all nonsurgeon physicians. Because vascular surgeon respondents represented a substantially larger proportion of all U.S. vascular surgeons than the proportion of nonsurgeon respondents among all U.S. nonsurgeons, our results for differences between patient types are presented for the nonsurgeons (i.e., excluding vascular surgeons).
Correlations between physician report of the importance of atherosclerotic risk factor reduction and current practice behavior in the PAD questionnaire were determined using Spearman's correlation coefficient. SAS statistical software, version 8.00 (SAS Institute, Inc., Cary, NC) was used for all analyses.
RESULTS
Of the 531 randomly selected vascular surgeons, 313 (58.9%) replied to the study mailing. Of these, 270 (86.3%) were eligible and 264 (97.8%) completed the questionnaire. Of the 4,688 randomly selected nonsurgeons, 2,283 (48.7%) replied to a study mailing. Of these, 1,705 (74.7%) were eligible and 1,314 (77.1%) completed the questionnaire. Thus, a total of 1,578 physicians participated.
Among the 270 eligible surgeons, the average age of physicians completing the survey was 48.0 ± 8.2 years versus 54.7 ± 9.1 years for those not completing the survey (P = .050). In addition, 84.9% of completers versus 67.7% of noncompleters were white (P = .244), and 92.8% of completers versus 83.3% of noncompleters were board certified (P = .398). Among the 1,705 eligible nonsurgeons, the average age of physicians who completed the survey was 47.1 ± 11.2 years versus 48.7 ± 10.8 years for noncompleters (P = .014). In addition, 76.2% of completers versus 56.0% of noncompleters were white (P < .001), and 82.6% of completers versus 74.7% of noncompleters were board certified (P < .001). There were no significant differences in gender between questionnaire completers and noncompleters. Table 1 shows characteristics of questionnaire completers.
Table 1.
Characteristics of Eligible Physicians Who Completed a Survey by Specialty (N = 1,578)
| General Internists (N = 406) | Family Physicians (N = 435) | Cardiologists (N = 473) | Vascular Surgeons (N = 264) | P Value | |
|---|---|---|---|---|---|
| Mean age, y ±SD | 44.3 ± 10.7 | 46.5 ± 11.5 | 50.0 ± 10.6 | 48.0 ± 8.2 | <.001 |
| Female gender, % | 30.3 | 21.6 | 7.0 | 2.7 | <.001 |
| Board-certified, % | 79.8 | 73.3 | 93.5 | 92.8 | <.001 |
| Ethnicity, % | |||||
| White | 69.7 | 82.3 | 76.1 | 84.9 | <.001* |
| African American | 3.7 | 2.3 | 1.3 | 0.76 | <.001* |
| Latino | 2.7 | 5.1 | 4.4 | 3.4 | <.001* |
| Asian | 19.7 | 6.9 | 15.0 | 6.4 | <.001* |
| Other | 4.4 | 3.5 | 3.2 | 4.6 | <.001* |
P value is for comparison of 5 ethnic groups across all four specialties.
Current Behavior
In unadjusted analyses, physicians were less likely to report “almost always” prescribing antiplatelet therapy or recommending aerobic exercise for the patient with PAD than for the patient with CAD (Table 2). PAD status was also associated with higher cholesterol thresholds for initiating diet and drug therapy compared to CAD status. Adjusting for patient gender and physician age, specialty, gender, board certification status, and race, PAD status was associated independently with lower odds ratios for “almost always” initiating antiplatelet therapy and “almost always” recommending aerobic exercise compare to CAD status (Table 2). In these multivariable analyses, LDL thresholds for initiating diet and drug therapy were significantly higher for PAD as compared to CAD status (Table 2). When multivariable analyses were repeated adjusting for aforementioned variables in addition to knowledge and attitudes, there were no substantial changes from the multivariable regression analyses results shown in Table 2 (data not shown).
Table 2.
Unadjusted and Adjusted Associations Between Atherosclerotic Disease Status and Physician-reported Current Behavior Regarding Cardiovascular Disease Risk Factor Reduction (N = 1,314)*
| Unadjusted Odds Ratio/Regression Coefficient† | 95% Confidence Interval | P Value | Adjusted Odds Ratio/Regression Coefficient† | 95% Confidence Interval | P Value | |
|---|---|---|---|---|---|---|
| Physicians reporting that they almost always prescribe antiplatelet therapy | ||||||
| No disease | 0.12‡ | (0.09 to 0.16) | <.001 | 0.11‡ | (0.08 to 0.15) | <.001 |
| PAD | 0.41‡ | (0.31 to 0.55) | <.001 | 0.40‡ | (0.30 to 0.54) | <.001 |
| Physicians reporting that they almost always recommend aerobic exercise | ||||||
| No disease | 0.67 | (0.51 to 0.88) | .004 | 0.71 | (0.54 to 0.93) | .014 |
| PAD | 0.63 | (0.48 to 0.82) | .001 | 0.64 | (0.49 to 0.84) | .002 |
| Physicians reporting that they almost always prescribe a supervised exercise program | ||||||
| No disease | 0.52 | (0.26 to 1.03) | .060 | 0.51 | (0.26 to 1.03) | .060 |
| PAD | 0.76 | (0.41 to 1.41) | .384 | 0.74 | (0.40 to 1.37) | .334 |
| Physicians reporting that they almost always advise smoking cessation (if the patient smokes) | ||||||
| No disease | 0.63 | (0.41 to 0.99) | .045 | 0.68 | (0.43 to 1.07) | .100 |
| PAD | 0.81 | (0.51 to 1.29) | .375 | 0.85 | (0.53 to 1.35) | .480 |
| Difference in average LDL cholesterol level at which cholesterol-lowering diet is initiated§ | ||||||
| No disease | 16.72 mg/dL‡ | (13.38 to 20.04) | <.001 | 15.99 mg/dL‡ | (12.74 to 19.25) | <.001 |
| PAD | 9.28 mg/dL‡ | (5.90 to 12.67) | <.001 | 8.97 mg/dL‡ | (5.66 to 12.28) | <.001 |
| Difference in average LDL cholesterol level at which cholesterol-lowering drug is initiated§ | ||||||
| No disease | 28.49 mg/dL† | (25.12 to 31.86) | <.001 | 27.06 mg/dL‡ | (23.83 to 30.29) | <.001 |
| PAD | 12.55 mg/dL† | (5.90 to 12.67) | <.001 | 12.06 mg/dL‡ | (8.81 to 15.31) | <.001 |
N = 1,314 instead of 1,578 because surgeons are excluded from analyses.
Reference group is patients with coronary artery disease. Adjusted odds ratios and regression coefficients are adjusted for physician specialty, physician age, physician race, male versus female patient, and physician board certification. Regression coefficients are provided for average LDL levels. All other values are odds ratios.
Differences between odds ratios and regression coefficients for PAD versus no-disease groups significant at P < .001.
Regression coefficient represents difference in average LDL cholesterol level at which therapy is started for each patient group, relative to the reference group. LDL cholesterol values for the reference group (patient with coronary artery disease) are 121.4 for the average LDL cholesterol level at which a cholesterol-lowering diet is initiated and 121.6 for the LDL cholesterol level at which a cholesterol-lowering drug is initiated.
PAD, peripheral arterial disease.
Physicians' Knowledge and Attitudes
Physicians were significantly more likely to report that antiplatelet therapy is extremely important to prescribe and has a large effect on risk of future CVD events for the patient with CAD than for the patient with PAD (Table 3). Physicians were also significantly more likely to report that cholesterol-lowering drugs were extremely important to prescribe for the patient with CAD than for the patient with PAD. Physicians were significantly less likely to report complete familiarity with NCEP guidelines regarding cholesterol therapy for the patient with PAD than for the patient with CAD. However, proportions of physicians who correctly reported that the desirable LDL level is <100 mg/dL were comparable for the patient with PAD versus the patient with CAD (49.3% vs 50.7%, respectively; P = .99). Physicians' estimates of the 5-year risk of CVD events were significantly higher for the patient with PAD than for the patient with CAD and the patient with no disease (Table 3). Proportions of physicians who correctly estimated future risk of cardiovascular events6 were 59.6% for the patient with PAD and 40.4% for the patient with CAD (P < .001).
Table 3.
Physician-reported Knowledge and Attitudes Regarding Cardiovascular Disease Risk Factor Reduction by Patient Disease Status (N = 1,314)*
| Physicians' Knowledge and Attitudes | CAD (n = 442) | PAD (n = 438) | No Disease (n = 434) | Overall P Value |
|---|---|---|---|---|
| Percentage of physicians reporting that the following interventions have a “large effect” on the risk of future cardiovascular events | ||||
| Antiplatelet therapy | 41.8 | 28.8†,‡ | 19.4 | <.001 |
| Aerobic exercise | 23.0 | 22.7 | 25.0 | .667 |
| Supervised exercise program | 10.1 | 11.9 | 11.4 | .681 |
| Smoking cessation | 79.7 | 80.8 | 76.9 | .330 |
| Cholesterol lowering | 57.9 | 50.9 | 48.3 | .014 |
| Percentage of physicians who report that it is “extremely important” to | ||||
| Prescribe antiplatelet therapy | 61.5 | 37.8†,‡ | 22.7 | <.001 |
| Recommend aerobic exercise | 43.7 | 34.6 | 36.7 | .014 |
| Prescribe a supervised exercise program | 8.0 | 7.4 | 5.4 | .288 |
| Advise smoking cessation if the patient smokes | 95.5 | 93.2 | 92.4 | .147 |
| Recommend a cholesterol-lowering diet | 61.4 | 58.0 | 49.0 | <.001 |
| Prescribe cholesterol-lowering medication if the LDL cholesterol is increased despite nonpharmacologic therapy | 75.5 | 62.8†,‡ | 52.4 | <.001 |
| Physician-reported | ||||
| Ideal LDL level, mg/dL ±SD | 103.4 ± 13.9 | 106.9*,†± 18.4 | 119.1 ± 20.5 | <.001 |
| Percentage of physicians “completely familiar” with the following NCEP guidelines | ||||
| Average LDL level (mg/dL) at which cholesterol-lowering diet is prescribed | 38.6 | 32.3 | 33.7 | .121 |
| Average LDL level (mg/dL) at which cholesterol-lowering drug is prescribed | 42.1 | 34.7† | 34.7 | .033 |
| Physicians' estimates of cardiovascular event risk, % | ||||
| Average 5-year risk of cardiovascular events | 39.4 | 49.0†,‡ | 27.1 | <.001 |
Physicians were randomized to receive 1 of 3 survey types describing a hypothetical 55- to 65-year-old patient with: a) coronary artery disease, b) peripheral arterial disease, c) no clinically evident atherosclerosis, respectively. Surveys were identical except for the hypothetical patient presented in each of the 3 surveys. Half of the hypothetical patients were women and half were men.
Comparisons between PAD and CAD are statistically significant (P < .005 in χ2 test or analysis of variance with Bonferroni adjustment).
Comparisons between PAD and no-disease patients are statistically significant (P < .005 in χ2 test or analysis of variance with Bonferroni adjustment).
PAD, peripheral arterial disease; CAD, coronary artery disease; no disease, no clinically evident atherosclerosis; NCEP, National Cholesterol Education Program. Surgeons were excluded from these analyses because they received only the PAD survey.
Specialty Differences
Cardiologists were significantly more likely to report “almost always” prescribing antiplatelet therapy for the patient with PAD than were all other specialties (Table 4). Thresholds for initiating cholesterol-lowering interventions were lowest for cardiologists and highest for vascular surgeons. Compared to all other specialties, vascular surgeons were significantly less likely to state that prescribing cholesterol-lowering therapy had a large effect on risk of future cardiovascular events. Cardiologists most frequently reported complete familiarity with NCEP guidelines for cholesterol treatment in PAD, and vascular surgeons least frequently reported complete familiarity with these guidelines (Table 4).
Table 4.
Physician Knowledge, Attitude, and Behavior Regarding Cardiovascular Disease Risk Factor Reductions for Peripheral Arterial Disease Patients According to Physician Specialty (N = 702)*
| Internal Medicine (N = 134) | Family Practice (N = 143) | Cardiology (N = 161) | Vascular Surgery (N = 264) | Overall P Value | |
|---|---|---|---|---|---|
| Current behavior | |||||
| Percentage of physicians reporting that they almost always | |||||
| Prescribe antiplatelet therapy | 45.5c | 41.3c | 74.8d | 52.5c | <.001 |
| Recommend aerobic exercise | 43.9c,d | 40.6e,d | 61.4c | 60.2c | <.001 |
| Prescribe a supervised exercise program | 3.8c | 2.8c | 6.3c | 4.6c | .513 |
| Advise smoking cessation | 88.6c | 87.4c | 93.7c,e | 97.0d,e | <.001 |
| Average LDL level (mg/dL) ±SD at which | |||||
| Cholesterol-lowering diet is prescribed | 132.2 ± 22.3c,d | 135.1 ± 21.5c | 124.9 ± 22.1d | 144.1 ± 40.0c | <.001 |
| Cholesterol-lowering drug is prescribed | 138.7 ± 24.0c | 141.6 ± 23.8c | 123.0 ± 21.8d | 148.1 ± 44.0c | <.001 |
| Physicians' knowledge and attitudes | |||||
| Percentage of physicians reporting that the following interventions have a “large effect” on the risk of future cardiovascular events | |||||
| Antiplatelet therapy | 28.4c | 25.2c | 32.3c | 14.4d | <.001 |
| Aerobic exercise | 29.9c | 23.1c,e | 16.3c,d | 15.6c,e | .004 |
| Supervised exercise program | 18.1c | 14.8c | 4.4d | 9.0c,d | <.001 |
| Smoking cessation | 81.3c | 81.1c | 80.1c | 75.8c | .454 |
| Lowering cholesterol | 46.3c,d | 42.7c | 62.1d | 16.8e | <.001 |
| Percentage of physicians who report they are completely familiar with NCEP guidelines regarding | |||||
| LDL cholesterol level at which cholesterol-lowering diet should be initiated | 27.3c | 22.3c | 45.6d | 3.1e | <.001 |
| LDL cholesterol level at which cholesterol-lowering drug should be initiated | 30.5c | 22.4c | 49.4d | 2.7e | <.001 |
| Physician-reported | |||||
| Percentage of similar PAD patients who will experience a cardiovascular event in the next 5 years | 51.6c | 51.3c,d | 44.8c,d | 44.5d | <.001 |
| Ideal LDL level, mg/dL ±SD | 109.9 ± 16.5c | 110.6 ± 19.2c | 102.4 ± 14.2d | 120.4 ± 39.0c | <.001 |
Only includes physicians who received the survey describing a patient with peripheral arterial disease. Values with the same lettered superscripts (i.e., c,d,e) in a given row are not statistically significantly different from each other (Bonferroni-adjusted P < .002 within each behavior, knowledge, and attitude).
LDL, low-density lipoprotein; NCEP, National Cholesterol Education Program.
Correlations Between Physician Attitudes and Reported Current Practice Behavior
For the patient with PAD, correlations between physician report of the “importance” of atherosclerotic risk factor interventions and corresponding reported current practice behavior were 0.57 (P < .001) for antiplatelet therapy and 0.45 (P < .001) for aerobic exercise. The correlation between the importance of cholesterol-lowering drug therapy and the cholesterol level at which drug therapy is implemented was −0.29 (P < .001), indicating that greater perceived importance of cholesterol-lowering drug therapy was associated with initiating drug therapy at a lower cholesterol level.
Correlations Between Familiarity With NCEP Guidelines and Reported Current Practice Behavior
Physician-reported degree of familiarity with the NCEP-recommended LDL level at which a low-fat, low-cholesterol diet should be initiated was correlated modestly and inversely with physician report of the level of LDL at which they would initiate cholesterol-lowering diet therapy for a patient with PAD (Spearman correlation coefficient = −0.172; P < .001). Degree of familiarity with the NCEP-recommended LDL level at which cholesterol-lowering drug therapy should be initiated was correlated modestly and inversely with physician report of the level of LDL at which they would initiate cholesterol-lowering drug therapy in PAD (Spearman correlation coefficient = −0.159; P < .001).
DISCUSSION
In this national survey, physicians reported significantly lower rates of prescribing antiplatelet therapy, cholesterol-lowering therapy, and aerobic exercise for a hypothetical patient with PAD than for one with CAD. Physicians were more likely to state that antiplatelet therapy and cholesterol-lowering were extremely important interventions for the patient with CAD than for the patient with PAD, and we found strong correlations between physicians' report of the importance of risk factor interventions and their reported current practice behavior. Our data suggest that deficiencies in physician knowledge and attitudes regarding atherosclerotic risk factor reduction in patients with PAD contribute to lower rates of risk factor reduction in these patients. Because previous studies demonstrated suboptimal rates of atherosclerotic risk factor reduction for patients with CAD,24–28 our finding that physicians report even lower rates of risk factor reduction for PAD than for CAD patients is striking.
In the present study, physicians ranked future risk of cardiovascular events in a patient with PAD higher than in a patient with CAD, yet physicians still perceived that risk factor treatment was less important in PAD than in CAD and were less likely to prescribe risk factor reduction for patients with PAD than for those with CAD. These discrepancies may relate to the fact that many more clinical trials have assessed the benefits of atherosclerotic risk factor reduction in CAD as compared to PAD. For patients with CAD, physicians' attitudes and practice behavior are influenced by clinical trial results.25 Furthermore, several cholesterol-lowering and antiplatelet drugs have United States Food and Drug Administration (FDA)-approved indications for use in CAD patients, whereas only 1 antiplatelet drug has FDA approval for use in PAD populations and no cholesterol-lowering drugs have been approved for use in patients with PAD. Finally, multiple competing demands for physicians' attention and time may also affect physicians' prescribing practices for patients with PAD.
Cardiologists were significantly more likely to report “almost always” prescribing antiplatelet therapy compared to the other specialties for the patient with PAD. Cardiologists also more frequently reported complete familiarity with NCEP cholesterol-lowering guidelines in PAD and had the lowest cholesterol thresholds for initiating cholesterol-lowering therapy. Vascular surgeons had least familiarity with NCEP guidelines and the highest thresholds for initiating cholesterol-lowering therapy. A previous study showed that cardiologists provide better quality of care for patients with CAD as compared to internists and family medicine specialists.24 However, to our knowledge no prior studies have evaluated specialty differences in attitudes, knowledge, and behavior regarding atherosclerotic risk factor reduction for patients with PAD. In addition, to our knowledge no prior studies have evaluated vascular surgeons' attitudes, knowledge, or behavior regarding risk factor reduction in patients with PAD.
The PARTNERS program demonstrated lower rates of atherosclerotic risk factor interventions for patients with PAD than for those with other cardiovascular disease in 350 primary care practices representing 26 cities across the United States.3 On the basis of patient report and medical record review, patients with previously established PAD were significantly less likely to be treated for hypertension and hyperlipidemia and were less likely to receive antiplatelet therapy than were patients with established CAD. In contrast to the present study, identifying reasons for undertreatment of atherosclerotic risk factors in patients with PAD was not a primary aim of the PARTNERS program. Also in contrast to PARTNERS, we specifically evaluated risk factor treatment for patients with PAD by vascular surgeons and cardiologists.
The AHA and the NCEP recommend equivalent atherosclerotic risk factor reduction intensity for patients with PAD and with CAD. Available data support these recommendations for the following reasons. First, studies consistently demonstrate that PAD is associated with a 3- to 6-fold increased risk of future cardiovascular morbidity and mortality compared to non-PAD,4,5,7,29–32 even when PAD patients have no clinically evident CAD or cerebrovascular disease. Second, atherosclerotic risk factor reduction efforts prevent atherosclerotic morbidity and mortality both in populations with CAD and in populations without clinically evident atherosclerosis.9,33–39 Therefore, these interventions should prevent atherosclerotic events among PAD patients, who have future risk of CVD morbidity and mortality comparable to that of CAD patients and markedly higher future risk than patients without clinically evident atherosclerosis.
Physicians may have reported less-intensive atherosclerotic risk factor reduction in PAD because the hypothetical patient with PAD had no other clinically evident atherosclerosis (such as CAD or cerebrovascular disease). However, this reasoning is not supported by available data.4,5,7,29–32 Furthermore, our finding that physicians ranked future CVD event rates for the patient with PAD higher than for the patient with CAD suggests that physicians were cognizant of the increased CVD event risk in the PAD patient. Another potential explanation for undertreatment of atherosclerotic risk factors in patients with PAD is that PAD has been underemphasized, compared to CAD, in national education programs such as those of the NCEP and the AHA.10,40
Our study has some limitations, including the fact that data on current physician practice behavior were collected with questionnaires and may not necessarily reflect actual practice. Physician-reported behavior is likely to be closer to recommended practice than is actual behavior, since physicians completing a questionnaire may record the “most correct” response. In addition, many demands on physicians' time in the clinical setting (such as attention to comorbid disease) might interfere with actual atherosclerotic risk factor reduction but should not have prevented reporting of risk factor reduction in a questionnaire. Nonetheless, physician behavior for the patient with PAD was still suboptimal. Second, we did not specifically quantify effect sizes for the Likert scale that defined large versus small effect sizes of atherosclerotic risk factor therapy on prevention of cardiovascular events. It is conceivable that some physicians may have considered a 10% relative risk reduction to be a “large” effect while other physicians may have considered this a “small” effect. Finally, our results were likely affected by the fact that a large proportion of physicians did not respond to our mailings.41,42 Questionnaire completers were younger and included a higher proportion of whites and board-certified physicians as compared to noncompleters.
In conclusion, physicians report less-intensive atherosclerotic risk factor reduction for a patient with PAD than for a patient with CAD, and this discrepancy appears to be related to deficiencies in knowledge and attitudes regarding the importance of atherosclerotic risk factor reduction in patients with PAD. On the basis of these data, interventions are needed to improve rates of atherosclerotic risk factor reduction for patients with PAD, thereby ultimately preventing excess morbidity and mortality in these patients.
Acknowledgments
This work was supported by Grant R01-HL63226 from the National Heart Lung and Blood Institute. Dr. McDermott is supported in part by an Established Investigator Award from the American Heart Association. Dr. McDermott was supported by a Robert Wood Johnson Generalist Physician Faculty Scholar Award during the time this study was performed.
REFERENCES
- 1.Fowkes FG, Housley E, Cawood EH, Macintyre CC, Ruckley CV, Prescott RJ. Edinburgh Artery Study: prevalence of asymptomatic and symptomatic peripheral arterial disease in the general population. Int J Epidemiol. 1991;20:384–92. doi: 10.1093/ije/20.2.384. [DOI] [PubMed] [Google Scholar]
- 2.McDermott MM, Mehta S, Greenland P. Leg symptoms other than intermittent claudication are common in peripheral arterial disease. Arch Intern Med. 1999;159:387–92. doi: 10.1001/archinte.159.4.387. [DOI] [PubMed] [Google Scholar]
- 3.Hirsch AT, Criqui MH, Treat-Jacobson D. Peripheral arterial disease detection, awareness, and treatment in primary care. JAMA. 2001;286:1317–24. doi: 10.1001/jama.286.11.1317. [DOI] [PubMed] [Google Scholar]
- 4.Vogt MT, Cauley JA, Newman AB, Kuller LH, Hulley SB. Decreased ankle/arm blood pressure index and mortality in elderly women. JAMA. 1993;270:465–9. [PubMed] [Google Scholar]
- 5.Newman AB, Sutton-Tyrrell K, Vogt MT, Kuller LH. Morbidity and mortality in hypertensive adults with a low ankle/arm blood pressure index. JAMA. 1993;270:487–9. [PubMed] [Google Scholar]
- 6.Weitz JI, Byrne J, Clagett P, et al. Diagnosis and treatment of chronic arterial insufficiency of the lower extremities: a critical review. Circulation. 1996;94:3026–49. doi: 10.1161/01.cir.94.11.3026. [DOI] [PubMed] [Google Scholar]
- 7.Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381–6. doi: 10.1056/NEJM199202063260605. [DOI] [PubMed] [Google Scholar]
- 8.Pearson TA, Criqui MH, Luepker RV, Oberman A, Winston M. Primer in Preventive Cardiology. Dallas, Tex: American Heart Association; 1994. pp. 83–92. [Google Scholar]
- 9.CAPRIE Steering Committee A randomized, blinded trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE) Lancet. 1996;348:1329–39. doi: 10.1016/s0140-6736(96)09457-3. [DOI] [PubMed] [Google Scholar]
- 10.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II) JAMA. 1993;23:3015–23. [PubMed] [Google Scholar]
- 11. Available at http://rover.nhlbi.nih.gov/guidelines/cholesterol/atp3xsum.pdf. Accessed October 14, 2002.
- 12. Available at http://circ.ahajournals.org/cgi/content/full/104/13/1577. Accessed October 14, 2002.
- 13.McDermott MM, Mehta S, Ahn H, Greenland P. Atherosclerotic risk factors are less intensively modified in peripheral arterial disease than in coronary artery disease. J Gen Intern Med. 1997;12:209–15. doi: 10.1046/j.1525-1497.1997.012004209.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anand SS, Kundi A, Eikelboom J, Yusuf S. Low rates of preventive practices in patients with peripheral vascular disease. Can J Cardiol. 1999;15:1259–63. [PubMed] [Google Scholar]
- 15.Clark AL, Byrne JC, Nasser A, McGroarty E, Kennedy JA. Cholesterol in peripheral vascular disease—a suitable case for treatment? QJM. 1999;92:219–22. doi: 10.1093/qjmed/92.4.219. [DOI] [PubMed] [Google Scholar]
- 16.Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 17.Millstein SG. Utility of the theories of reasoned action and planned behavior for predicting physician behavior: a prospective analysis. Health Psychol. 1996;15:398–402. doi: 10.1037//0278-6133.15.5.398. [DOI] [PubMed] [Google Scholar]
- 18.Ajzen I. From intentions to actions. In: Kuhl J, Beckman J, editors. Action Control from Cognition to Behavior. New York: Springer-Verlag; 1985. pp. 11–39. In: eds. [Google Scholar]
- 19.Gardner AW, Poehlman ET. Exercise rehabilitation programs for the treatment of claudication pain. JAMA. 1995;274:975–80. [PubMed] [Google Scholar]
- 20.U.S. Preventive Services Task Force Aspirin for the primary prevention of cardiovascular events. Ann Intern Med. 2002;136:157–60. doi: 10.7326/0003-4819-136-2-200201150-00015. [DOI] [PubMed] [Google Scholar]
- 21.Donaldson GW, Moinpour CM, Bush NE. Physician participation in research surveys. A randomized study of inducements to return mailed research questionnaires. Eval Health Prof. 1999;22:427–41. doi: 10.1177/01632789922034392. [DOI] [PubMed] [Google Scholar]
- 22.Asch DA, Christakis NA, Ubel PA. Conducting physician mail surveys on a limited budget. A randomized trial comparing $2 bill versus $5 bill incentives. Med Care. 1998;36:95–9. doi: 10.1097/00005650-199801000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Miller RG. Simultaneous Statistical Inference. New York: Springer-Verlag; 1981. [Google Scholar]
- 24.Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 25.Lamas GA, Pfeffer MA, Hamm P, Werthelmer J, Rouleau JL, Braunwald E. Do the results of randomized clinical trials of cardiovascular drugs influence medical practice? N Engl J Med. 1992;327:241–7. doi: 10.1056/NEJM199207233270405. [DOI] [PubMed] [Google Scholar]
- 26.Thiru K, Gray J, Majeed A. Management of ischaemic heart disease in primary care: towards better practice. J Public Health Med. 1999;21:179–84. doi: 10.1093/pubmed/21.2.179. [DOI] [PubMed] [Google Scholar]
- 27.Harnick DJ, Cohen JL, Schechter CB, Fuster V, Smith DA. Effects of practice setting on quality of lipid-lowering management in patients with coronary artery disease. Am J Cardiol. 1998;81:1416–20. doi: 10.1016/s0002-9149(98)00209-4. [DOI] [PubMed] [Google Scholar]
- 28.Schucker B, Wittes JT, Santanello NC, et al. Change in cholesterol awareness and action. Arch Intern Med. 1991;151:666–73. [PubMed] [Google Scholar]
- 29.Howell MA, Colgan MP, Seeger RW, Ramsey DE, Sumner DS. Relationship of severity of lower limb peripheral vascular disease to mortality and morbidity: a six-year follow-up study. J Vasc Surg. 1989;9:691–7. doi: 10.1067/mva.1989.vs0090691. [DOI] [PubMed] [Google Scholar]
- 30.Dormandy J, Mahir M, Ascady G, et al. Fate of the patient with chronic leg ischaemia: a review article. J Cardiovasc Surg. 1989;30:50–7. [PubMed] [Google Scholar]
- 31.Paris BEC, Libow LS, Halperin JL, Mulvihill MN. The prevalence and one-year outcome of limb arterial obstructive disease in a nursing home population. J Am Geriatr Soc. 1988;36:607–12. doi: 10.1111/j.1532-5415.1988.tb06154.x. [DOI] [PubMed] [Google Scholar]
- 32.McKenna M, Wolfson S, Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis. 1991;87:119–28. doi: 10.1016/0021-9150(91)90014-t. [DOI] [PubMed] [Google Scholar]
- 33.Shepard J, Cobbe SM, Ford I. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 34.The Post Coronary Artery Bypass Graft Trial Investigators The effect of aggressive lowering of low-density lipoprotein levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. The Post Coronary Artery Bypass Graft Trial Investigators. N Engl J Med. 1997;336:153–62. doi: 10.1056/NEJM199701163360301. [DOI] [PubMed] [Google Scholar]
- 35.Pitt B, Waters D, Brown WV, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. Atorvastatin versus Revascularization Treatment Investigators. N Engl J Med. 1999;341:70–6. doi: 10.1056/NEJM199907083410202. [DOI] [PubMed] [Google Scholar]
- 36.Sacks FM, Pfeffer MA, Moye LA, et al. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial Investigators. N Engl J Med. 1996;335:1001–9. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 37.Downs JR, Clearfield M, Weis S. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–22. doi: 10.1001/jama.279.20.1615. [DOI] [PubMed] [Google Scholar]
- 38.Randomized trial of cholesterol-lowering in 4,444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 39.Ridker PM, Cushman M, Stampfer MJ, Tracy RP, Hennekens CH. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med. 1997;336:973–9. doi: 10.1056/NEJM199704033361401. [DOI] [PubMed] [Google Scholar]
- 40.American Heart Association and American College of Cardiology Scientific statement on assessment of cardiovascular risk by use of multiple-risk factor assessment equations. Circulation. 1999;100:1481–92. doi: 10.1161/01.cir.100.13.1481. [DOI] [PubMed] [Google Scholar]
- 41.Sheikh K. Predicting risk among non-respondents in prospective studies. Eur J Epidemiol. 1986;2:39–43. doi: 10.1007/BF00152716. [DOI] [PubMed] [Google Scholar]
- 42.Larroque B, Kaminski M, Bouvier-Colle MH, Hollebecque V. Participation in a mail survey: role of repeated mailings and characteristics of nonrespondents among recent mothers. Paediatr Perinat Epidemiol. 1999;2:218–33. doi: 10.1046/j.1365-3016.1999.00176.x. [DOI] [PubMed] [Google Scholar]