Abstract
BACKGROUND
There are few data available on how physicians inform patients about bad news. We surveyed internists about how they convey this information.
METHODS
We surveyed internists about their activities in giving bad news to patients. One set of questions was about activities for the emotional support of the patient (11 items), and the other was about activities for creating a supportive environment for delivering bad news (9 items). The impact of demographic factors on the performance of emotionally supportive items, environmentally supportive items, and on the number of minutes reportedly spent delivering news was analyzed by analysis of variance and multiple regression analysis.
RESULTS
More than half of the internists reported that they always or frequently performed 10 of the 11 emotionally supportive items and 6 of the 9 environmentally supportive items while giving bad news to patients. The average time reportedly spent in giving bad news was 27 minutes. Although training in giving bad news had a significant impact on the number of emotionally supportive items reported (P < .05), only 25% of respondents had any previous training in this area. Being older, a woman, unmarried, and having a history of major illness were also associated with reporting a greater number of emotionally supportive activities.
CONCLUSIONS
Internists report that they inform patients of bad news appropriately. Some deficiencies exist, specifically in discussing prognosis and referral of patients to support groups. Physician educational efforts should include discussion of prognosis with patients as well as the availability of support groups.
Keywords: communication, bad news, end-of-life care
Studies have shown that physician communication skills can affect patient satisfaction,1,2 compliance with treatment,1 quality of life,3 and health outcomes.4,5 Poor communication skills have been linked with physician burnout,6,7 professional dissatisfaction, and increased litigation.8,9 Giving a patient bad news, for example, that he or she has cancer, poses a special challenge in patient–physician communication.
For patients, receiving a diagnosis of cancer or other bad news causes great stress and can lead to psychological morbidity.10–12 Studies have suggested that physician communication can affect the psychological well-being of patients being given a diagnosis of cancer.13–19 Many patients prefer a patient-centered style of communication.20 Authors stress the importance of giving information that is perceived as adequate and eliciting and responding to the emotional reaction of each patient.11,13,21 Patients may be more likely to develop psychiatric disorders when they do not receive the information that they want or do not receive sufficient attention to their emotional responses.11,21
In the last decade, several authors have published recommendations and guidelines for breaking bad news.22–34 There is little evidence about the best methods for giving bad news, so most guidelines are based on opinion.27,35 The guidelines generally recommend individualized disclosure, i.e., tailoring the interview to the individual patient.28 Nondisclosure is no longer considered ethical. However, complete disclosure without regard for the patient's readiness for the information is also inappropriate. Patients differ in their reactions to being given bad news and in their needs during this emotional time.
Buckman22 developed a 6-step protocol including the following: 1) giving the news in person, in private, with enough time and without interruptions; 2) finding out what the patient knows about the diagnosis; 3) finding out what the patient wants to know; 4) sharing the information, which includes giving a warning shot and then a small amount of information in simple language at a pace the patient can handle, with a caring and honest attitude; Buckman includes eliciting and listening to the patient's fears and concerns in this fourth step; 5) responding to the patient's feelings, which includes identifying, acknowledging, and validating his or her reaction; 6) planning and follow-through, which includes planning the next steps, summarizing what has been said, identifying sources of support, and making an early follow-up appointment.
There are relatively few data on how physicians actually give bad news. Ford et al.36 in the United Kingdom have analyzed oncologists' interactions with their patients. In Ford's analysis of audiotaped interactions, she found little psychosocial exchange compared to biomedical exchange, few empathic responses of physicians to their patients, and high physician control over the interviews. Several studies have shown that physicians do not detect or they under-rate distress in their patients. For example, Fallowfield et al.13 found that surgeons did not detect emotional distress in women with breast cancer in 70% of cases. Ford et al.36 found that oncologists under-rated distress in their cancer patients. Other authors37–41 also have found that oncologists do not detect or assist patients well with their psychosocial issues.
There are even fewer data on how physicians in the United States give bad news. Eggly et al.42 analyzed videotapes of general internal medicine residents giving the diagnosis of lung cancer to simulated patients. They found a mean rating of 3.42 on informative items out of a possible 5 and a mean rating of 3.45 on affective items out of a possible 5. They found that the residents had the most difficulty in eliciting the patients' perceptions of the problem before giving bad news, exploring whether the patient wanted to receive the news, and eliciting the patient's emotional reaction to the news.
The purpose of the current study was to survey practicing internal medicine physicians in the United States on their self-reported practices in giving bad news. We also collected data on demographic factors and prior training in communication skills or personal experience with illness that could impact how these physicians give bad news.
METHODS
We conducted a cross-sectional mail survey of 1,000 randomly selected practicing internists in the United States, identified through the American Medical Association (AMA) master file, a comprehensive list of U.S. physicians, not limited to AMA members. Students, residents, and non-practicing physicians were excluded. To test the hypothesis that there is a difference in how specialists and general internists deliver bad news, the study, which was approved by the Institutional Review Board of Christiana Care Health System, included 500 general internists and 500 medical subspecialists.
Each physician received an anonymous questionnaire along with a $5 incentive. A second questionnaire was mailed to all nonresponders. All responses received before June 1, 2000 were included in the analysis.
The survey presented a hypothetical patient with metastatic carcinoma of the liver and lungs with an unknown primary. Items in the survey were developed from a study28 that used a consensus panel consisting of 28 medical oncologists, general practitioners, surgeons, nurses, social workers, clergy, and human rights representatives, along with 100 patients diagnosed with cancer within the previous 6 to 12 months. Items recommended by the panel and indicated as essential or desirable by more than 70% of the patients were included.
Eleven questions ascertained information about how internists give bad news and the emotional support that they provide to patients and their families. These questions included providing support to the family when giving bad news, finding out how much the patient wants to know, avoiding the use of specific statistics on survival, touching the patient on the hand or arm while giving bad news, giving an indication that things are serious before giving the details about the bad news (“warning shot”), conveying some kind of hope to the patient, avoiding giving the patient a specific amount of time that he/she will live, inquiring about the patient's worries, fears and concerns, starting the process of giving the bad news by first assessing the patient's understanding of his/her condition, encouraging the patient to express his/her feelings, and avoiding telling the patient that “everything will be all right” when conveying bad news.22,28,33 These items are referred to in this paper as emotionally supportive items.
Nine questions addressed the physical and social aspects of giving bad news in the office setting. These questions included ensuring that the bad news is given in a private setting, picking a time for giving bad news that is convenient for the patient and his/her family, sitting in a chair next to the patient (rather than behind a desk) when giving bad news, avoidance of a white lab coat when giving bad news (this item was included on the basis of suggestions during pretesting), referral to a cancer support group, ensuring that a support person is present when giving bad news, asking the receptionist to hold all phone calls when giving bad news, turning off the beeper or having someone hold it when giving bad news, and the avoidance of giving bad news by telephone.22,23,28,33 These items are referred to in this paper as environmentally supportive items. Respondents were asked to indicate how often they would perform each behavior, based on a 4-point Likert-type scale (always, frequently, rarely, never).
Items were framed so that a mix of positive and negative responses were deemed optimal (Appendix A). Demographic questions about the respondents were also included. The survey was pretested for face and content validity among 25 practicing physicians at Christiana Care Health System. Respondents in the pretest completed the questionnaire, and were then questioned about their understanding of each of the items on the survey instrument.
Data were entered for analysis manually by 2 individuals. In a cross-check of 30% of the entered data, no errors were detected. The effects of the demographic data on the number of activities indicated as being performed by respondent physicians always or frequently for each of 2 broad aspects of giving bad news (emotionally supportive items and environmentally supportive items) were analyzed by analysis of variance. Demographic variables included age, gender, marital status, life-threatening illness in the respondent, life-threatening illness in a spouse, year of medical school graduation, prior training in giving bad news, location and type of practice, percent of time seeing patients, specialty/subspecialty, and percent of practice in primary care. Demographic variables demonstrating a significant association (P < .05) with the outcome in a univariable regression model were entered into multivariable models. The dependent variables in these models were the number of emotionally supportive items that the respondents reported as doing always or frequently and the number of environmentally supportive items that the respondents reported as doing always or frequently.
RESULTS
Of the 1,000 questionnaires, 26 were returned undelivered, and 13 physicians had retired from practice. Of the 961 internists who were eligible and received surveys, 461 (48%) returned questionnaires. Respondents' demographic and professional characteristics are shown in Table 1. The responding physicians had an average age of 50 years and were largely male, white, and married. While a majority of respondents (63%) had experienced a life-threatening illness in a spouse or loved one, only 17% had personally experienced such an illness. The practices of most respondents were in urban or suburban settings, and most were in private practices; general internists and subspecialists were equally represented. Physicians spent an average of 84% of their time seeing patients, with 65% of the time spent in primary care. As expected, there was a significant difference between generalists and subspecialists, with generalists spending 94%± 16% of their time in primary care, while subspecialists spent 35%± 37% of their time in primary care (P < .001). Responses by physicians in different subspecialties and general internists were not significantly different (although numbers in each subspecialty were small), and therefore the results are pooled for the entire respondent group. Only 25% of the respondents had received any type of training in how to give bad news to patients.
Table 1.
Characteristics of Responding Physicians*
| Characteristic | Value |
|---|---|
| Mean age, y ±SD | 50 ± 11 |
| Gender, n (%) | |
| Male | 365 (79) |
| Female | 94 (20) |
| Marital status, n (%) | |
| Married | 401 (87) |
| Divorced | 21 (5) |
| Single | 31 (7) |
| Widowed | 5 (1) |
| Having a spouse or loved one with a life-threatening illness, n (%) | |
| Yes | 292 (63) |
| No | 166 (36) |
| Yourself having had a life-threatening illness, n (%) | |
| Yes | 77 (17) |
| No | 382 (83) |
| Specialty, n (%) | |
| General internal medicine | 233 (51) |
| Medicine subspecialty | 227 (49) |
| Practice type, n (%)† | |
| Private practice | 326 (71) |
| Academic medicine | 75 (16) |
| HMO | 52 (11) |
| VA | 20 (4) |
| Other | 7 (2) |
| Practice locale, n (%) | |
| Urban | 214 (46) |
| Suburban | 182 (39) |
| Rural | 60 (13) |
| Percent of time seeing patients, mean ±SD | 85 ± 20 |
| Percent of practice devoted to primary care, mean ±SD | 65 ± 41 |
| Training in giving bad news to patients, n (%) | |
| Yes | 113 (25) |
| No | 347 (75) |
Not all respondents answered every question. Percent does not add up to 100 because of rounding and nonresponse.
Respondents were asked to check all categories that applied. Percent adds up to more than 100 because of multiple choices.
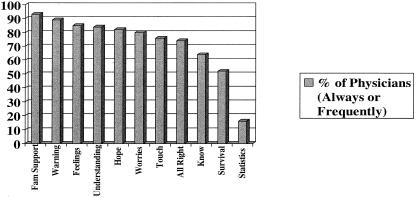
Most of the physicians who responded to the survey indicated that they always or frequently provided 10 of the 11 emotionally supportive items to the patient and the family at the time that bad news was communicated (Fig. 1). However only 16% of physicians always or frequently avoided giving specific statistics of survival to patients.
FIGURE 1.
Percent of 461 respondent physicians performing emotionally related items always or frequently.
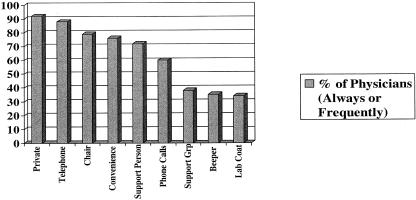
Fewer physicians attended to the environmentally supportive items involved in giving bad news to patients (Fig. 2). A minority of respondents always or frequently avoided wearing white lab coats (34%), turned off their beepers (35%), and referred the patients to support groups when giving bad news (38%). The average amount of time spent giving bad news was 27 ± 12 minutes.
FIGURE 2.
Percent of 461 respondent physicians performing structurally related items always or frequently.
Several demographic features of the respondents were associated with the number of emotionally supportive items performed always or frequently as determined by multiple linear regression analysis (Table 2). Age >50 (P = .013) and a personal experience with a life threatening illness (P = .007) were both associated with an increased number of emotionally supportive items being done always or frequently. Being married (P = .015) was negatively associated with these factors being performed. Female physicians who responded were significantly more likely than were male physicians to provide emotionally supportive items to patients and their families (P = .002) and to spend more time with patients when giving bad news (31 ± 14 minutes for female physicians, 26 ± 11 minutes for male physicians; P = .001). Training in giving bad news was associated with an increased frequency in providing emotionally supportive items (P = .026). There was no difference seen between generalists and subspecialists.
Table 2.
Demographic Factors Independently Associated With Number of Emotionally Supportive Items Performed Always or Frequently by Respondents
| Variable | Items* | P Value |
|---|---|---|
| Age | ||
| ≥50 y | 8.1 ± 1.6 | .013 |
| ≤49 y | 7.8 ± 1.7 | |
| Married | ||
| Yes | 7.9 ± 1.6 | .015 |
| No | 8.4 ± 1.4 | |
| Personal illness | ||
| Yes | 8.5 ± 1.4 | .007 |
| No | 7.8 ± 1.6 | |
| Previous training | ||
| Yes | 8.2 ± 1.6 | .026 |
| No | 7.9 ± 1.6 | |
| Gender | ||
| Female | 8.4 ± 1.4 | .002 |
| Male | 7.8 ± 1.7 | |
Mean number ±SD of emotionally supportive items out of 11 performed by respondents; R2 = .085.
The only demographic factor associated with the frequency of engaging in recommended environmentally supportive items in giving bad news as determined by multiple linear regression analysis was the type of practice of the respondents. Physicians who engaged in private practice were significantly more likely to provide environmentally supportive items for the benefit of the patient than were physicians who did not engage in private practice (P = .031). No other demographic variables were associated with these factors, and previous training in how to give bad news to patients had no effect.
DISCUSSION
A number of authors28,32,33 have suggested ways in which physicians can more empathically inform patients and their families about bad news. In this study, respondents stated that they always or frequently used most of these emotionally supportive items when informing patients of a life-threatening illness such as metastatic cancer. However, when discussing prognosis, many physicians in this study indicated that they usually give specific statistics about likelihood of survival to patients, and a large percentage of respondents stated that they informed patients of a specific predicted length of life.
Most guidelines have suggested that patients be given a range of time of survival and averages in terms of prognosis, rather than specific times of survival and statistics.28 It is impossible to know the exact time of survival of any given patient. Statistics refer to populations, whereas the individual patient may fall above or below the mean in terms of their survival. Before giving information about prognosis, it is also important to know the question that is being asked by the patient. In one study43 of 32 patients recently diagnosed with cancer, only 1 participant requested a specific life expectancy, and initially regretted having asked for the information. When information is given about prognosis, it is important to tailor that information to the needs and desires of the patient (individualized disclosure). Thus, although many of the emotionally supportive items of giving bad news are attended to by internists in this study, there is a need for changes in how prognosis is conveyed to patients.
Although a majority of respondents in this study did ensure that no phone calls would interrupt the meeting with a patient when giving bad news, only a small percentage indicated that they routinely turned off or handed off their beepers. Thus, interruptions may be occurring when these physicians give bad news to patients. A consensus panel of clinicians and patients recently diagnosed with cancer indicated that avoiding interruptions when informing patients about bad news was important,28 and some authors suggest turning off beepers or giving them to a colleague to hold.23 There is no consensus on wearing white coats while giving bad news, so it is not surprising that a majority of participants in this study did not avoid wearing them.
Perhaps most surprisingly, a majority of the responding physicians did not routinely refer patients to support groups when informing them of bad news such as a life-threatening illness. Referral to support groups has been advocated by some authors.28 Studies12,18 suggest that patients who experience supportive physician interaction cope in a more effective manner with terminal illnesses. Support from peers with a similar disease state could also increase patient adjustment and decrease anxiety. In one study44 on parents who were informed of their newborn child's cleft lip and/or palate, it was demonstrated that 67% of those surveyed strongly desired to have such support. In another study,45 supportive-expressive group therapy was found to increase the quality of life in metastatic breast cancer patients by improving mood and decreasing the perception of pain. Therefore, there is information about the benefits and availability of support groups that should be disseminated to physicians.
Several demographic features of the responding group of physicians in this study were associated with an increased attendance to the emotionally supportive and/or environmentally supportive items of informing patients about bad news. It is not surprising that respondents who had personally experienced a life-threatening illness were more attentive to the emotionally supportive needs of their patients. Several authors46–48 have written of their own personal experiences with illness and how it changed the way in which they communicated with patients. Similarly, one might expect that as physicians age they would consider such emotionally supportive items more prominently in their dealings with patients. In fact, the respondents in this study who were over the age of 50 years were more likely to have reported performing emotionally supportive items of giving bad news than were younger physicians.
Female physicians who responded to this survey spent more time than their male counterparts when informing patients about bad news, and engaged in more emotionally supportive items than did male respondents. One might question whether female physicians are inherently more nurturing, or if their training and previous experiences have allowed them to be more attentive to patients' emotional needs. Further work in this area is warranted.
Those respondents who indicated that they had received some type of previous training in communicating bad news were more likely to attend to the emotionally supportive aspects of informing patients about a life-threatening illness than were respondents without such prior training. However, only 25% of respondents had received any type of education in this area. Studies42 have demonstrated that residents generally lack the necessary competence in delivering bad news to patients. Training can make a significant difference in how bad news is communicated to patients, as demonstrated by Baile et al.49 in their study of practicing oncologists and by Fallowfield et al.50 in a study in the United Kingdom.
This study has some limitations. The data are self reports by physicians; no attempts were made to assess the actual behaviors by general internists, subspecialist internists, or other types of physicians in giving bad news to patients. Thus, respondents may have reported that they engaged in such behaviors more than they actually did, and may have not performed some of the behaviors in a competent fashion. These possibilities only serve to emphasize the need for more educational interventions for physicians in this important area of communication.
Second, the low response rate may introduce the possibility of nonrespondent bias. However, the age, gender, and specialty distribution of the respondents in this survey is similar to that of practicing physicians in the United States in 1997–1998.51 One would suspect that the nonrespondents were those physicians who again were either not engaging in the communication of bad news to patients, or who were not interested in the topic, even though they did deliver bad news to patients. If the latter was the case, it would more strongly point out the need for greater physician awareness of the importance of giving bad news in an appropriate fashion.
Third, the hypothetical case used in the survey was that of a patient diagnosed with metastatic carcinoma. The survey did not vary the type of bad news communicated to the hypothetical patient. How physicians communicate bad news may be dependent upon the clinical situation and their familiarity with the medical condition.
Finally, this study did not attempt to assess patients' opinions about how bad news is communicated or whether the specific guidelines impact on patient satisfaction or on outcomes. Areas for further study include objective assessments by patients or physician educators on how physicians give bad news; whether the published guidelines on giving bad news reflect patients' expressed needs and desires; and whether conveying bad news according to current guidelines impacts on patient satisfaction and clinical outcomes.
In summary, internal medicine physicians report that they do generally recognize and perform many items as recommended in the literature in giving bad news to patients. However, many internal medicine physicians report that they do not convey prognosis as recommended by some authors, and only a minority would refer patients to support groups. Educational efforts for physicians in giving bad news should include discussing prognosis with patients. Additionally, physicians should be made aware of the availability and possible benefit of support groups for patients. These results can help guide both undergraduate and postgraduate medical education curriculum development.
Acknowledgments
This work was supported by a grant from the Osler Fund, Department of Medicine of Christiana Care Health System.
Appendix A
Survey Instrument
| End-of-Life Communication Study Group | |||||
| We are interested in the way in which you give bad news to patients. Your completion of this survey is totally voluntary; however, should you decide to participate, we ask that you complete all questions as fully as is possible. Please be assured that your answers will remain totally confidential, and you will not be identified on this questionnaire. Although not sufficient to reimburse you for your time, please accept the $5.00 bill as a token of our appreciation. | |||||
| Neil J. Farber, MD Susan Y. Urban, MD Ronald Polite, MD | |||||
| For each of the following questions, we ask you to assume that you are telling a patient that he or she has carcinoma of an unknown primary that has metastasized to the liver and lungs, so that only palliative therapy is available. | |||||
| For a patient such as the one presented above, how often would you do each of the following (check one box for each question): | |||||
| Always | Frequently | Sometimes | Rarely | Never | |
| 1. Provide support to the family (when they are available) when giving bad news to the patient | □ | □ | □ | □ | □ |
| 2. Find out how much the patient wants to know before giving bad news | □ | □ | □ | □ | □ |
| 3. Give specific statistics to patients about survival of life-threatening illnesses | □ | □ | □ | □ | □ |
| 4. Touch a patient on the hand or arm when giving bad news | □ | □ | □ | □ | □ |
| 5. Give an indication that things are serious before giving details about bad news | □ | □ | □ | □ | □ |
| 6. Ensure there is some kind of hope conveyed to patients when giving bad news | □ | □ | □ | □ | □ |
| 7. Give a definite amount of time of survival when giving bad news if the patient asks | □ | □ | □ | □ | □ |
| 8. Inquire as to patients' worries, fears, and concerns when giving bad news | □ | □ | □ | □ | □ |
| 9. Start giving bad news by first assessing the patient's understanding of his/her condition | □ | □ | □ | □ | □ |
| 10. Encourage the patient to express his/her feelings when giving bad news | □ | □ | □ | □ | □ |
| 11. Tell the patient that everything will be all right when giving bad news | □ | □ | □ | □ | □ |
| For the following questions, we ask you to assume that you are informing the patient of his/her metastatic carcinoma in your outpatient office. If you do not have such an office, please answer as many of the following questions as apply to you, and indicate N/A next to any question that does not apply. | |||||
| How often do you (check one box for each answer): | |||||
| Always | Frequently | Sometimes | Rarely | Never | |
| 12. Ensure that the meeting with the patient to give bad news is done in private | □ | □ | □ | □ | □ |
| 13. Pick a time to give bad news that is most convenient for the patient and his/her family | □ | □ | □ | □ | □ |
| 14. Sit in a chair next to the patient rather than behind your desk when giving bad news | □ | □ | □ | □ | □ |
| 15. Wear a white lab coat when giving bad news | □ | □ | □ | □ | □ |
| 16. Refer the patient to a cancer support group after giving bad news to the patient | □ | □ | □ | □ | □ |
| 17. Ensure that the patient has a support person present when giving bad news | □ | □ | □ | □ | □ |
| 18. Ask your receptionist to hold all phone calls when giving bad news to a patient | □ | □ | □ | □ | □ |
| 19. Turn off your beeper (or ask someone to hold it) when giving bad news to a patient | □ | □ | □ | □ | □ |
| 20. Give bad news to a patient by telephone | □ | □ | □ | □ | □ |
| 21. On average, how much time do you usually spend with the patient when informing him/her of the bad news? | |||||
| _________________________minutes | |||||
| We need some information about yourself: | |||||
| 22. Age__________ | |||||
| 23. Gender (check one): □Male □Female | |||||
| 24. Marital status (check one answer): | |||||
| □Married □Divorced □Single □Widowed □Other_____________ | |||||
| 25. Has a spouse or other loved one ever experienced a life-threatening illness (check one answer)? | |||||
| □Yes □No | |||||
| 26. Have you ever experienced a life-threatening illness (check one answer)? | |||||
| □Yes □No | |||||
| 27. Year graduated from medical school _________ | |||||
| 28. Have you had any training in how to give bad news to patients, other than informally on rounds (check one answer)? | |||||
| □Yes □No | |||||
| If so, was it in (check all that apply): | |||||
| □Medical school | |||||
| □Residency | |||||
| □Fellowship | |||||
| □Continuing medical | |||||
| □Other__________ | |||||
| 29. How would you characterize the locale which you practice (check one answer)? | |||||
| □Urban □Suburban □Rural | |||||
| 30. How would you characterize your type of practice (check all that apply)? | |||||
| □Private practice | |||||
| □HMO practice | |||||
| □Academic faculty | |||||
| □VA | |||||
| □Other_____________________ | |||||
| 31. What percent of you professional time is spent seeing patients? _______________% | |||||
| 32. What is your medical specialty? ____________________________________ | |||||
| 33. What is your medical subspecialty? ____________________________________ | |||||
| 34. What percent of your practice is devoted to primary care? _________________% | |||||
| THANK YOU FOR YOUR ASSISTANCE. | |||||
REFERENCES
- 1.Ley P. Communicating with Patients: Improving Communication, Satisfaction, and Compliance. London: Croom Helm Ltd.; 1988. [Google Scholar]
- 2.Bertakis KD, Roter D, Putnam SM. The relationship of physician medical interview style to patient satisfaction. J Fam Pract. 1991;32:175–81. [PubMed] [Google Scholar]
- 3.Fallowfield LJ. The ideal consultation. Br J Hosp Med. 1992;47:364–7. [PubMed] [Google Scholar]
- 4.Kaplan SH, Greenfield S, Ware JE. Assessing the effects of physician–patient interactions on the outcome of chronic disease. Med Care. 1989;27(suppl):110–27. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 5.Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303:1385–7. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramirez A, Graham J, Richards M, et al. Burnout and psychiatric disorder among cancer clinicians. Br J Cancer. 1995;71:1263–9. doi: 10.1038/bjc.1995.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fallowfield L. Can we improve the professional and personal fulfillment of doctors in cancer medicine? Br J Cancer. 1995;71:1132–3. doi: 10.1038/bjc.1995.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levinson W, Roter D, Mullooly JP, Dull VT, Frankel RM. Physician-patient communication: the relationship with malpractice claims among primary care physicians and surgeons. JAMA. 1997;277:553–9. doi: 10.1001/jama.277.7.553. [DOI] [PubMed] [Google Scholar]
- 9.Vincent C, Young M, Phillips A. Why do people sue doctors: a study of patients and relatives taking legal action. Lancet. 1994;343:1609–13. doi: 10.1016/s0140-6736(94)93062-7. [DOI] [PubMed] [Google Scholar]
- 10.Cooper CL, Watson M. Cancer and Stress: Psychological, Biological and Coping Studies. New York: Wiley; 1991. pp. 147–69. [Google Scholar]
- 11.Maguire P. Breaking bad news. Eur J Surg Oncol. 1998;24:188–99. doi: 10.1016/s0748-7983(98)92929-8. [DOI] [PubMed] [Google Scholar]
- 12.Molleman E, Krabbendam PJ, Annyas AA, Koops HS, Sleijfer DT, Vermey A. The significance of the dotor-patient relationship in coping with cancer. Soc Sci Med. 1984;18:475–80. doi: 10.1016/0277-9536(84)90003-0. [DOI] [PubMed] [Google Scholar]
- 13.Fallowfield LJ, Hall A, Maguire GP, Baum M. Psychological outcomes of different treatment policies in women with early breast cancer outside a clinical trial. BMJ. 1990;301:575–80. doi: 10.1136/bmj.301.6752.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fogarty LA, Curbow BA, Wingard JR, Mc Donnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–9. doi: 10.1200/JCO.1999.17.1.371. [DOI] [PubMed] [Google Scholar]
- 15.Omne-Ponten M, Holmberg L, Sjoden PO. Psychosocial adjustment among women with breast cancer Stages I and II: six year follow-up of consecutive patients. J Clin Oncol. 1994;12:1778–82. doi: 10.1200/JCO.1994.12.9.1778. [DOI] [PubMed] [Google Scholar]
- 16.Paraskevaidis E, Kitchener HC, Walker LG. Doctor-patient communication and subsequent mental health in women with gynecological cancer. Psycho-Oncol. 1993;2:195–200. [Google Scholar]
- 17.Roberts CS, Cox CE, Reintgen DS, Baile WF, Gibertini M. Influence of physician communication on newly diagnosed breast patients' psychological adjustment and decision-making. Cancer. 1994;74:336–41. doi: 10.1002/cncr.2820741319. [DOI] [PubMed] [Google Scholar]
- 18.Siminoff LA. Improving communication with cancer patients. Oncology. 1992;6:83–7. [PubMed] [Google Scholar]
- 19.Sardell AN, Trierweiler SJ. Disclosing the cancer diagnosis. Procedures that influence patient hopefulness. Cancer. 1993;72:3355–65. doi: 10.1002/1097-0142(19931201)72:11<3355::aid-cncr2820721135>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 20.Dowsett SM, Saul JL, Butow PN, et al. Communication styles in the cancer consultation: preferences for a patient-centered approach. Psycho-Oncol. 2000;9:147–56. doi: 10.1002/(sici)1099-1611(200003/04)9:2<147::aid-pon443>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 21.Parle M, Jones B, Maguire P. Maladaptive coping and affective disorders in cancer patients. Psychol Med. 1996;26:735–44. doi: 10.1017/s0033291700037752. [DOI] [PubMed] [Google Scholar]
- 22.Buckman R. How to Break Bad News—A Guide for Health Care Professionals. Baltimore, Md: The Johns Hopkins University Press; 1992. [Google Scholar]
- 23.Campbell CL. Breaking bad news to patients. JAMA. 1994;271:1052. doi: 10.1001/jama.271.13.1052. [DOI] [PubMed] [Google Scholar]
- 24.Chisholm CA, Pappas DJ, Sharp MC. Communicating bad news. Obstet Gynecol. 1997;90:637–9. [PubMed] [Google Scholar]
- 25.Ellis PM, Tattersall MHN. How should doctors communicate the diagnosis of cancer to patients? Ann Med. 1999;31:336–41. doi: 10.3109/07853899908995900. [DOI] [PubMed] [Google Scholar]
- 26.Fallowfield L. Giving sad and bad news. Lancet. 1993;341:476–8. doi: 10.1016/0140-6736(93)90219-7. [DOI] [PubMed] [Google Scholar]
- 27.Faulkner A, Maguire P, Regnard C. Breaking bad news—a flow diagram. Palliat Med. 1994;8:145–51. doi: 10.1177/026921639400800208. [DOI] [PubMed] [Google Scholar]
- 28.Girgis A, Sanson-Fisher RW. Breaking bad news: consensus guidelines for medical practitioners. J Clin Oncol. 1995;13:2449–56. doi: 10.1200/JCO.1995.13.9.2449. [DOI] [PubMed] [Google Scholar]
- 29.Girgis A, Sanson-Fisher RW. Breaking bad news 1: current best advice for clinicians? Behav Med. 1998;24:53–9. doi: 10.1080/08964289809596381. [DOI] [PubMed] [Google Scholar]
- 30.Girgis A, Sanson-Fisher RW, Schofield MJ. Is there consensus between breast cancer patients and providers on guidelines for breaking bad news. Behav Med. 1999;25:69–77. doi: 10.1080/08964289909595739. [DOI] [PubMed] [Google Scholar]
- 31.Swindells S, Mohr J, Justis JC, et al. Quality of life in patients with human immunodeficiency virus infection: impact of social support, coping style and hopelessness. Int J STD AIDS. 1999;10:383–91. [PubMed] [Google Scholar]
- 32.Quill TE, Townsend P. Bad news: delivery, dialogue, and dilemmas. Arch Intern Med. 1991;151:463–8. [PubMed] [Google Scholar]
- 33.Ptacek JT, Eberhardt TL. Breaking bad news: a review of the literature. JAMA. 1996;276:496–502. [PubMed] [Google Scholar]
- 34.Shields CE. Giving patients bad news. Prim Care. 1998;25:381–90. doi: 10.1016/s0095-4543(05)70070-1. [DOI] [PubMed] [Google Scholar]
- 35.Walsh RA, Girgis A, Sanson-Fisher RW. Breaking bad news. 2: what evidence is available to guide clinicians? Behav Med. 1998;24:61–72. doi: 10.1080/08964289809596382. [DOI] [PubMed] [Google Scholar]
- 36.Ford S, Fallowfield L, Lewis S. Doctor-patient interaction in oncology. Soc Sci Med. 1996;42:1511–9. doi: 10.1016/0277-9536(95)00265-0. [DOI] [PubMed] [Google Scholar]
- 37.Cull A, Stewart M, Altman DG. Assessment of and intervention for psychosocial problems in routine oncology practice. Br J Cancer. 1995;72:229–35. doi: 10.1038/bjc.1995.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davenport S, Goldberg D, Millar T. How psychiatric disorders are missed during medical consultations. Lancet. 1987;2:439–41. doi: 10.1016/s0140-6736(87)90970-6. [DOI] [PubMed] [Google Scholar]
- 39.Ford S, Fallowfield L, Lewis S. Can oncologists detect distress in their out-patients and how satisfied are they with their performance during bad news consultations? Br J Cancer. 1994;70:767–70. doi: 10.1038/bjc.1994.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hardman A, Maguire P, Crowther D. The recognition of psychiatric morbidity on a medical oncology ward. J Psychosom Res. 1989;33:235–9. doi: 10.1016/0022-3999(89)90051-2. [DOI] [PubMed] [Google Scholar]
- 41.Maguire P. Improving the detection of psychiatric problems in cancer patients. Soc Sci Med. 1985;20:819–23. doi: 10.1016/0277-9536(85)90336-3. [DOI] [PubMed] [Google Scholar]
- 42.Eggly S, Alfonso N, Rojas G, Baker M, Cardozo L, Robertson RS. An assessment of residents' competence in the delivery of bad news to patients. Acad Med. 1997;72:397–9. doi: 10.1097/00001888-199705000-00023. [DOI] [PubMed] [Google Scholar]
- 43.Peteet JR, Abrams HE, Ross DM, Stearns NM. Presenting a diagnosis of cancer: patients' views. J Fam Pract. 1991;32:577–81. [PubMed] [Google Scholar]
- 44.Strauss RP, Sharp MC, Lorch SC, Kachalia B. Physicians and the communication of “bad news”: parent experiences of being informed of their child's cleft lip and/or palate. Pediatrics. 1995;96:82–9. [PubMed] [Google Scholar]
- 45.Goodwin PJ, Leszca M, Ennis M, et al. The effect of group psychosocial support on survival in metastatic breast cancer. N Engl J Med. 2001;345:1719–26. doi: 10.1056/NEJMoa011871. [DOI] [PubMed] [Google Scholar]
- 46.Aoun H. From the eye of the storm, with the eyes of a physician. Ann Intern Med. 1992;116:335–8. [PubMed] [Google Scholar]
- 47.Poulson J. Bitter pills to swallow. N Engl J Med. 1998;338:1844–6. doi: 10.1056/NEJM199806183382512. [DOI] [PubMed] [Google Scholar]
- 48.Waxman HS. The patient as physician. Ann Intern Med. 1997;126:656–7. doi: 10.7326/0003-4819-126-8-199704150-00013. [DOI] [PubMed] [Google Scholar]
- 49.Baile WF, Lenzi R, Kudelka AP, et al. Improving physician-patient communication in cancer care: outcome of a workshop for oncologists. J Cancer Educ. 1997;12:166–73. doi: 10.1080/08858199709528481. [DOI] [PubMed] [Google Scholar]
- 50.Fallowfield L, Lipkin M, Hall A. Teaching senior oncologists communication skills: results from phase I of a comprehensive longitudinal program in the United Kingdom. J Clin Oncol. 1998;16:1961–8. doi: 10.1200/JCO.1998.16.5.1961. [DOI] [PubMed] [Google Scholar]
- 51.Randolph L. Physician Characteristics and Distribution in the U.S. Chicago: American Medical Association; 1997. [Google Scholar]