Abstract
OBJECTIVE
To measure the persistence of impaired health-related quality of life (HRQL) and psychological distress associated with co-occurring psychiatric and substance use disorders in a longitudinal sample of medically hospitalized male veterans.
DESIGN
A random sample followed observationally for 1 year after study enrollment.
SETTING
Inpatient medical and surgical wards at three university-affiliated Department of Veterans Affairs Medical Centers.
PATIENTS/PARTICIPANTS
A random sample of 1,007 admissions to medical and surgical inpatient services, excluding women and admissions for psychiatric reasons. A subset of participants (n = 736) was designated for longitudinal follow-up assessments at 3 and 12 months after study enrollment. This subset was selected to include all possible participants with study-administered psychiatric diagnoses (52%) frequency-matched by date of study enrollment to approximately equivalent numbers of participants without psychiatric diagnoses (48%).
MEASUREMENTS AND MAIN RESULTS
All participants were administered a computerized structured psychiatric diagnostic interview for 13 psychiatric (include substance use) disorders and received longitudinal assessments at 3 and 12 months on a multidimensional measure of HRQL, the SF-36, and a measure of psychological distress, the Symptom Checklist, 90-item version. On average, HRQL declined and psychological distress increased over time (P < .05). Psychiatric disorders were associated with significantly greater impairments in functioning and increased distress on all measures (P < .001) except physical functioning (P < .05). These results were replicated in the patients (n = 130) who received inpatient or outpatient mental health or substance abuse services.
CONCLUSIONS
General medical physicians need to evaluate the mental health status of their hospitalized and seriously ill patients. Effective mental health interventions can be initiated posthospitalization, either immediately in primary care or through referral to appropriate specialty care, and should improve health functioning over time.
Keywords: comorbidity, psychiatric disorders, substance use disorders health status, psychological distress, functioning
Individuals with medical illnesses, especially those using inpatient or outpatient medical services, experience high levels of psychological distress and functional impairment at the time of service use.1–5 These reports document that up to 50% of medically ill patients report substantial depression, anxiety, or general distress. Furthermore, psychiatric comorbidity is associated with substantially higher health care costs for medical illness during hospitalization3,6 and in primary care.7
Psychiatric comorbidity, whether measured as symptomatology or by psychiatric diagnostic interview, is also associated with substantial functional impairment in individuals with medical illnesses.5,8,9 In individuals with comorbid serious medical illnesses, these decrements in functioning have been observed only cross sectionally or longitudinally for depression alone.8 But we have little information about the impact of the range of co-occurring psychiatric disorders on longitudinal functioning for the broad spectrum of medical illness. This question is particularly important as health practitioners and health care organizations are being increasingly asked to provide information on patient outcomes to employers and other health care purchasers.
Generally, it is not clear whether the high levels of distress and reduced functioning associated with a medical hospitalization and co-occurring psychiatric disorders are transient circumstances surrounding an acute medical crisis. Questions remain as to whether the observed distress is a consequence of the medical illness (or its treatment) that will subside once the crisis is resolved2,3,10,11 and that disentangling the effects of the medical illness from those of many psychiatric disorders is difficult at best.12 If psychological distress is associated only with the immediate medical crisis, it should subside over time and functioning might improve. Prospective assessment of psychological and functional outcomes over time should help disentangle the effects of comorbid psychiatric problems from those of the medical illness.
Assessment of longitudinal outcomes associated with comorbid psychiatric and medical disorders is complicated on an observational basis by potential receipt of mental health treatment in the intervening time interval. We know that treatment of most psychiatric disorders is effective when appropriately given.13–17 Therefore, observational assessment of long-term outcomes must measure receipt of mental health services and assess the impact of these services on the course of psychological symptoms and health-related quality of life (HRQL) in individuals treated for medical disorders.
We report on the 1-year functional and psychological outcomes for medically hospitalized men at three Department of Veterans Affairs Medical Centers (VAMCs). In a prior report,5, we found that almost half (46.6%) met lifetime criteria for at least one American Psychiatric Association disorder according to the Diagnostic and Statistical Manual, Revised Third Edition (DSM-III-R),18 and almost one fifth of the sample reported recent symptoms of their psychiatric disorder. This current report represents a prospective cohort study with psychiatric status as the exposure of interest for longitudinal outcomes in 734 men who were assigned to be interviewed at 3 and 12 months following their initial baseline assessment. The purpose of this report is to determine whether the functional impairment associated with psychiatric disorders and the psychological distress observed during a medical hospitalization persists over 1 year.
METHODS
Subjects and Procedures
A random sample of patients admitted to acute medical and surgical wards between November 1992 and August 1994 to the three participating VAMCs was requested to participate in the study. Details of recruitment, study eligibility, and sample identification are published elsewhere.5 Briefly, all male patients admitted to acute medical and surgical wards and transfers from intensive care units were eligible for the study if they had been admitted for medical, not psychiatric, purposes. We did not enroll women in the study by design because of the low frequencies of women hospitalized at the three medical centers (∼1%) and differing population distributions of psychiatric disorders in women compared with men.19,20 All patients received a written and oral description of the study and signed informed consent to participate. This project was approved by the respective Institutional Review Boards for the three participating VAMCs.
Consenting patients were administered a battery of assessments upon study enrollment (see Measures). In all, we conducted interviews with 1,007 men at the three participating VAMCs during the initial hospitalization. A designated subset of these patients was assigned to participate in longitudinal interviews at 3 and 12 months after the initial assessment. All patients who met diagnostic criteria for one or more psychiatric disorders and completed the full battery of interviews were designated into the longitudinal sample. A “comparison” sample of patients with no psychiatric diagnosis were frequency-matched into the longitudinal study on a weekly basis in equivalent numbers to that week's number of longitudinal study participants with psychiatric disorders. The longitudinal study subjects were contacted by letter to remind them of their study participation 1 month before each follow-up interview. Where possible, follow-up instruments were self-administered and returned by mail. Otherwise, they were conducted by telephone interview.
Measures
The instruments chosen measured comorbid psychiatric disorders and psychological distress, HRQL, and severity of illness. All instruments were administered during the index hospitalization and measures of HRQL and psychological distress were readministered at the follow-up interviews.
Co-occurring psychiatric disorders were identified by the computerized Quick Diagnostic Interview Schedule Interview (Q-DIS) for the American Psychiatric Association's diagnoses according to the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition (DSM-III-R).18 The Q-DIS identifies lifetime and recent (past 12 months) psychiatric disorders.21 For this study, we used the Q-DIS for 13 diagnoses: posttraumatic stress disorder, panic disorder, generalized anxiety disorder, agoraphobia, social phobia, simple phobia, obsessive-compulsive disorder, depression or dysthymia, mania, schizophrenia or schizophreniform disorder, alcohol abuse or dependence, drug abuse or dependence, and antisocial personality disorder. (The Q-DIS does not make distinctions between alcohol or drug dependence versus abuse, or between major depression and dysthymia.) Recent data have shown the Q-DIS to have good to excellent sensitivity and specificity compared to more structured and detailed paper-and-pencil diagnostic interviews.21 The Q-DIS was administered to patients by the study's research assistants using portable computers.
The distribution of these diagnoses among the 1,007 participants is available in a previous report.5 Briefly, the most frequent lifetime diagnoses were alcohol abuse or dependence (32.5%), posttraumatic stress disorder (10.0%), and major depression or dysthymia (9.0%). The most frequent recent (past 12 months) diagnosis was major depression or dysthymia (7.0%). We have commented previously that these prevalence rates are not surprising for a hospitalized male sample and confirm previous studies of high psychological distress in medical inpatients.5 At the close of the Q-DIS interview, the data obtained were used to classify patients into three groups: those with no Q-DIS diagnosis, those with a lifetime diagnosis and no recent symptoms, and those with a recent diagnosis (e.g., a diagnosis with symptoms during the past 12 months). This classification was used to designate participants into the longitudinal sample and also for analysis of the longitudinal data.
We measured current mental health symptomatology and distress using the Symptom Checklist, 90-item version (SCL-90).22 This measure has shown consistent factor structure23 and concurrent validity.24 The SCL-90 subscales include current (past 2 weeks) depression and anxiety and can be used to calculate an overall summary score, the Global Severity Index (GSI). The SLC-90 was administered during the index hospitalization as a baseline measurement and at each follow-up contact.
For measurement of HRQL, we used the Medical Outcomes Study Short Form, 36-Item General Health Survey (SF-36). The SF-36 assesses health concepts relevant to functional status and well-being and measures physical functioning; physical role functioning; bodily pain; general health; vitality; social health; emotional role functioning; and mental health.25,26 The SF-36 was administered during the initial hospitalization at the same time as the Q-DIS and at the follow-up assessments. In analysis of the first measurement of HRQL obtained during hospitalization, we found substantial decrements in HRQL associated with co-occurring psychiatric disorders, with the lowest functioning observed for those with recent Q-DIS disorders.5 The greatest decrements associated with psychiatric comorbidity were in physical and emotional role functioning.
We measured illness severity to avoid confounding the decreased functioning for seriously medically ill patients with any impairment associated with the co-occurring psychiatric disorder. We used several measures of illness severity. First, we used an independent assessment of medical illness severity, the Computerized Severity Index (CSI).27 Using clinical data abstracted from medical records, the CSI provides an overall maximum severity score for each patient that is based upon the severity of all existing diseases states. Information in the medical record, including multiple International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) codes,28 disease complications, and objective clinical findings such as laboratory values and symptoms are used to generate a severity score from 1 to 4.27 Photocopies of medical records from the index hospitalization were sent to the developers of the CSI for abstraction and scoring.
Our second measure of illness severity was the Charlson comorbidity index, which is based on age and medical diagnoses.29,30 The Charlson is a weighted index that takes into account age and the number/seriousness of comorbid disorders. It was initially designed and validated in the prediction of overall survival, but it also has been used in predictive studies of service use and costs.31,32 The advantage of the Charlson index was that it could be computed directly from VA administrative data and did not require the availability of the medical record. Our third measure of illness severity, again calculated from VA administrative data, was the number of VA medical/surgical hospitalizations in the year after discharge from the index hospitalization.
Mental Health Services After Initial Hospitalization
The course of psychological distress and HRQL may be influenced by intervening mental health services. Therefore, we identified VA inpatient and outpatient use of psychiatric or substance abuse care after the initial hospitalization from the VA national utilization databases. Inpatient psychiatric or substance abuse care was identified by relevant diagnosis-related groups (DRGs) and outpatient use was identified by clinic visits to a range of clinics providing mental health and substance abuse care.
Statistical Methods
We grouped subjects into three mutually exclusive categories according to their Q-DIS diagnostic data: (1) no lifetime DSM-III-R psychiatric diagnosis; (2) a past disorder, defined as any lifetime diagnosis but no recent (past 12 months) disorder; or (3) any recent (past 12 months) disorder. The first purpose of the analysis of the 3- and 12-month data was to identify whether observed differences in HRQL associated with a past or recent psychiatric disorder during the initial hospitalization5 persisted or changed qualitatively. The second purpose was to measure the persistence of psychological distress following the index hospitalization.
Our analysis approach took advantage of the multiple time points and used random regression models for longitudinal data.33–35 These models provide solutions to commonly observed problems in longitudinal data of missing data and serial correlation among multiple observations. Models are fit with all available data and the random subject effects and fixed effects are calculated from nonmissing observations. Therefore, individuals who have died are also included in analysis up to the point of their missing interview(s). We tested a basic mixed model with random and fixed effects with the dependent variables related to patient functioning, measured by HRQL (SF-36 subscales), and psychological distress (SCL-90 measures) from the three time points (i.e., the initial hospitalization, 3 and 12 months later). Independent variables were age, race, marital status, discharge diagnosis, severity of illness (separately, the CSI, Charlson comorbidity index, and number of medical/surgical hospitalizations), and co-occurring psychiatric disorders measured by Q-DIS diagnoses. Critical tests included the effect of time to identify whether functioning changed over time, and the interaction between time and co-occurring psychiatric disorders to identify whether change over time differed for patients with and without psychiatric disorders. If this interaction term was not significant, then we tested the main “between subjects” effect to determine whether co-occurring psychiatric disorders were associated with differences in functioning averaged over time.
Because of concerns with selectivity bias and associated biased regression coefficients for the effect of services,36 we analyzed the relationship between psychiatric comorbidity and HRQL separately for mental health service users (inpatient and outpatient combined) and nonusers. Selection effects occur when a measured independent variable (e.g., presence of a co-occurring psychiatric disorder) as well as unmeasured characteristics are associated with both another independent variable (e.g., mental health service use) and with the dependent variable.
RESULTS
Of the 1,007 subjects recruited into the initial study, 736 participated in the longitudinal portion. As intended by the study design, most of the participants with psychiatric disorders in the initial study were entered into the longitudinal study. Three quarters (75%) of all participants with a recent psychiatric disorder and 87% of those with a past disorder and no recent symptoms were included in the longitudinal assessments. In general, patients with a Q-DIS diagnosis did not participate in the longitudinal study because they either refused to participate in longitudinal follow-ups, were unable to participate in longitudinal follow-ups because of homelessness or lack of stable address, or were discharged from the hospital before completing additional assessments. Of the longitudinal study patients, 18% had a recent psychiatric disorder and 34% had a past disorder only. The longitudinal study participants did not differ from nonparticipants in age, education, race, medical diagnosis, CSI severity of illness, Charlson comorbidity index, or number of medical/surgical hospitalizations in the year after the index hospitalization.
Two thirds of the longitudinal study subjects were at least 65 years of age, 15% were nonwhite, two thirds had the lowest maximum CSI score, 37% had Charlson comorbidity index scores of 0 to 1 and 14% had scores of 3 to 6. Ten percent had initial hospitalizations for cancer diagnoses, 26% for heart disease, 7% for digestive diseases, 6% for muscle/bone diagnoses, 7% for injuries, 8% for circulatory disorders, and 36% had other less common diagnoses. The longitudinal sample was equally divided between medical (50%) and surgical (50%) discharges. All but 13 medical discharges were from general acute medicine whereas the surgical discharges were distributed relatively evenly among general surgery and subspecialties such as ophthalmology, orthopedics, otolaryngology, thoracic surgery, and peripheral vascular surgery. Over half (57%) were readmitted for medical or surgical diagnoses in the year after the index hospitalization (range, 1 to 13 hospitalizations). There were no associations between comorbid psychiatric diagnosis and our 3 severity of illness measures.
At the 3-month interview, 89% or 657 of the 736 longitudinal study subjects completed assessments. Subjects who were not interviewed were either deceased (4%), refused (3%), were too ill (1%), or could not be located (3%). At the 12-month interview, 11% (n = 87) of the original 736 were deceased over the year and 90% of the surviving subjects (583/649) completed the assessments, or 79% of all longitudinal study participants. Of the surviving subjects at 12 months, 4% refused, 4% were not located, and 2% were too ill to participate. There were no differences in age, race, education, or co-occurring psychiatric disorders between 12-month completers and noncompleters. However, noncompleters had a greater severity of illness as demonstrated by the CSI (P < .001), but not by the Charlson comorbidity index or number of medical/surgical hospitalizations. Noncompleters were also more likely to have cancer diagnoses and less likely to have muscle/bone or injury diagnoses during the initial hospitalization (P < .01). These differences were largely due to the increased mortality for patients who had the highest severity of illness on the CSI at the index hospitalization and those with cancer. There were also no differences in initial hospital HRQL or SCL-90 scores between completers and noncompleters, with the exception of the SF-36 Social Health Index (66 vs 60, P = .03).
Health-Related Quality of Life
Overall, based on paired t tests, we found significant declines over the 12-month follow-up interval in all measures of HRQL except the social health index, physical role functioning, and vitality. No measure of HRQL improved over the year. The greatest decline was observed for emotional role functioning (21 ± 46 points), but we also found modest declines in the physical functioning index (8 ± 29 points) and the general health ratings index (6 ± 21 points).
Early analyses of the SF-36 scores examined the impact of co-occurring psychiatric disorders on HRQL, controlling for age, race, marital status, medical diagnosis, and severity of illness (the maximum CSI [max-CSI], Charlson comorbidity index, and number of medical/surgical hospitalizations). However, inclusion of the max-CSI necessitated a loss of 100 subjects from analysis because their medical records were unavailable for review. Furthermore, we found that the max-CSI was unrelated to HRQL in multivariate models and the main effects of psychiatric comorbidity were essentially unchanged with the inclusion of the max-CSI. Therefore, we took advantage of the larger available sample size for analysis with the Charlson comorbidity index and the number of medical/surgical hospitalizations, for which we had complete data from administrative data files, as our measures of illness severity. In fact, we found that the number of medical/surgical hospitalizations was generally a strong predictor of HRQL in most analyses whereas the Charlson index was not. Both are included in subsequent analyses as controls for illness severity.
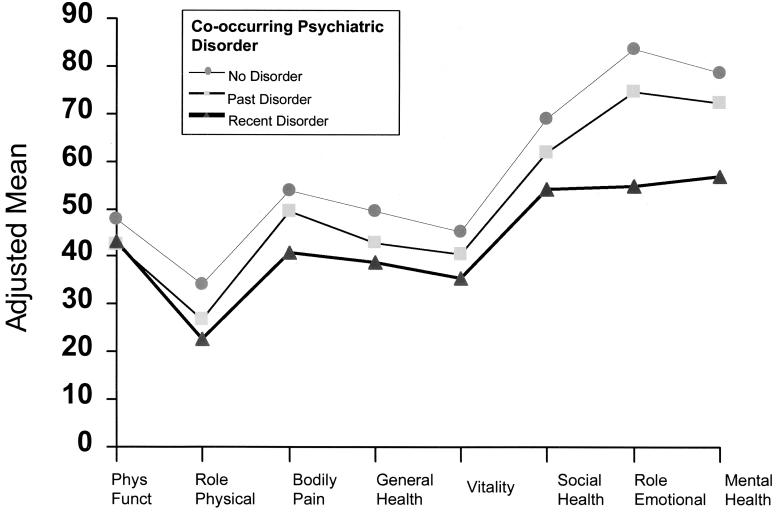
In the random regression models, we found a significant longitudinal effect of time representing declines in HRQL on the general health ratings index, physical functioning index, pain, emotional role functioning, and mental health index (all P < 0.0001, except P = .0043 for pain). We did not find any significant statistical interactions between time and co-occurring psychiatric disorders on any of the HRQL measures, indicating that the differences associated with psychiatric disorders observed during the index hospitalization5 remained relatively constant over the year. Overall psychiatric comorbidity, measured as a “between subjects” effect, was significantly associated with all measures of HRQL scales of the SF-36 after controlling for other factors including illness severity (all P < .001, except physical functioning index, P = .03). Because the interaction terms of comorbidity with time were non-significant, we calculated adjusted means for the individual SF-36 measures averaged over the three time points for each subject. These mean SF-36 scores, adjusted for age, race, marital status, medical diagnosis, and severity of illness, are presented in Figure 1 by level of co-occurring psychiatric disorders.
FIGURE 1.
Adjusted average means for health-related quality of life between initial hospitalization and 1 year later, for levels of co-occurring psychiatric disorders. Means are averaged over 3 assessments (initial hospitalization, and 3 and 12 months later) and are adjusted for age, race, marital status, medical diagnosis, and severity of medical illness. All contrasts are strongly statistically significant (P < .001) except for the physical functioning index (P = .03).
Psychological Distress
The SCL-90 measures of psychological distress and symptom of depression and anxiety all significantly increased over the year (paired t test, P < .001), with increased severity of symptoms noted for all subjects, not just for those with lifetime or recent psychiatric disorders. In the longitudinal random regression analyses of the all three SCL-90 scales analyzed, we found a significant interaction effect for the combination of time and psychiatric comorbidity (depression, P = .02; anxiety, P = .03; GSI, P = .002). This finding indicated that the effect of Q-DIS psychiatric disorders varied over the three assessments. In order to examine adjusted means for all three time points for the GSI (Table 1), we had to calculate the more traditional fixed effects repeated measures analysis because our random regression software (SAS PROC MIXED; SAS Institute, Cary, NC)cannot calculate adjusted means for interaction terms. These data show that the difference in GSI between participants with no psychiatric disorder, a past disorder only, and a recent disorder gradually widened over time, even though the levels of psychological distress at least doubled in all three groups over the year of study.
Table 1.
Longitudinal Adjusted Means* for SCL-90 Global Severity Index by Psychiatric Disorder Status at Index Hospitalization
| Psychiatric Disorder Status | |||
|---|---|---|---|
| No Diagnosis Mean (SE) | Past Disorder Mean (SE) | Recent Disorder Mean (SE) | |
| Baseline | 0.19 (0.05) | 0.30 (0.06) | 0.67 (0.06) |
| 3 months | 0.36 (0.08) | 0.45 (0.08) | 0.80 (0.09) |
| 12 months | 0.47 (0.09) | 0.61 (0.09) | 1.08 (0.10) |
Adjusted for age, race, marital status, medical diagnosis, and severity of medical illness. Analysis conducted using fixed effects repeated measures. The time*comorbidity interaction was significant (Roy's greatest root, P = .009). All pairwise contrasts at each time interval were significant (P < .01) except for no diagnosis versus past disorder at 3 months (P = .054). SCL-90 indicates Symptom Checklist, 90-item version.
Use of Mental Health Services over Follow-up
During the 1-year follow-up period, only 15 of the 734 longitudinal study participants (2%) were hospitalized in the VA health care system for a psychiatric or substance abuse disorder and 127 (17%) attended at least one mental health or substance abuse clinic visit (range, 1–206 visits). Not surprisingly, there were significant relationships between a Q-DIS diagnosis of psychiatric disorders and service use. Nine percent of those with a recent disorder were hospitalized for a psychiatric diagnosis over the year compared with less than 1% of those with no psychiatric disorder during the index hospitalization (P < .001). One third (34%) of individuals with a recent psychiatric disorder attended at least one mental health clinic visit compared with only 13% of those with no diagnosis (P < .001). The number of outpatient clinics differed significantly between Q-DIS groups (P < .001), with five visits on average for those with a recent disorder and less than one visit on average for those with a lifetime only diagnosis or no diagnosis.
There were 130 users and 612 nonusers of inpatient or outpatient mental health services in the longitudinal sample. We found no significant association between medical or surgical discharge and subsequent use of mental health or substance abuse services (20% vs 15%, P = .07). In bivariate analysis (data not shown), we found that HRQL and psychological distress were strong predictors of service use, in that service users had generally substantially lower HRQL and more symptoms of distress during the index hospitalization. Because of associated concerns regarding unmeasured characteristics differing between service users and nonusers, we proceeded to evaluate long-term functioning separately for these two groups. Table 2 presents separate adjusted means for service users and nonusers by levels of psychiatric comorbidity from the random regression analyses. Again, we adjusted for demographics, medical diagnosis, and severity of medical illness measured by the Charlson index and number of subsequent medical/surgical hospitalizations.
Table 2.
Average Adjusted Means for Psychological Distress and HRQL*
| Mental Health and Substance Abuse Service Users | Mental Health and Substance Abuse Service Nonusers | |||||
|---|---|---|---|---|---|---|
| No Disorder (n = 46) | Past Disorder (n = 38) | Recent Disorder (n = 46) | No Disorder (n = 309) | Past Disorder (n = 215) | Recent Disorder (n = 89) | |
| Psychological distress | ||||||
| Anxiety | 0.45† | 0.61 | 1.22 | 0.25† | 0.35 | 0.60 |
| Depression | 0.57† | 0.88 | 1.49 | 0.42† | 0.54 | 0.88 |
| Global Severity Index | 0.43† | 0.68 | 1.09 | 0.32† | 0.41 | 0.65 |
| HRQL | ||||||
| Physical functioning index | 55.8§ | 40.8 | 45.7 | 47.3 | 43.7 | 42.1 |
| Physical role functioning | 31.8† | 15.5 | 17.7 | 34.2‡ | 28.8 | 25.3 |
| Bodily pain | 53.7† | 49.4 | 40.9 | 54.1‡ | 49.9 | 43.7 |
| General health ratings index | 44.6‡ | 34.5 | 31.5 | 50.1‡ | 44.2 | 42.7 |
| Vitality | 47.1† | 36.9 | 30.3 | 44.9 | 41.7 | 38.8 |
| Social health index | 63.8§ | 53.4 | 47.6 | 69.5† | 63.0 | 57.4 |
| Emotional role functioning | 88.8† | 61.6 | 35.5 | 83.0† | 76.9 | 66.3 |
| Mental health index | 76.2† | 67.8 | 44.9 | 78.7† | 73.1 | 63.2 |
Averaged over 1 year of follow-up, adjusted for age, race, marital status, medical diagnosis, and severity of medical illness. Mental health and substance abuse service use measured over 1 year after discharge from index hospitalization. HRQL indicates health-related quality of life.
P < .001.
P < .01.
P < .05.
Among the 130 mental health and substance abuse service users, we found that there was a significant effect of time for four measures of HRQL (physical functioning, general health ratings index, emotional role functioning, and mental health index) that declined over the 1-year follow-up. On average, psychiatric comorbidity was significantly associated with reduced HRQL (all P < .05) and increased psychological distress in these individuals who received at least some mental health or substance abuse care. As shown in Table 2, psychological distress was generally two to three times greater for individuals with a recent psychiatric disorder compared with those with no diagnosed psychiatric disorder in the index hospitalization. Furthermore, decrements in HRQL associated with a recent psychiatric disorder in these patients who did receive some mental health care were as low as 55% for physical role functioning and 40% for emotional role functioning compared with patients with no psychiatric disorders. These measures represent the loss in general functioning or abilities to perform usual activities attributed to either physical or emotional problems.
Among the nonservice nonusers, there were significant time effects for psychological distress and the physical functioning index, pain index, general health ratings index, emotional role functioning, mental health index, and the three scales from the SCL-90. Comorbid psychiatric disorders were again associated with lower HRQL (except physical functioning and vitality) and all three SCL-90 measures of psychological distress. The significant HRQL impairments associated with a recent psychiatric disorder were still substantial among these nonusers but in all cases were less (74% to 85%) compared with no psychiatric disorders than for the service users. although psychological distress for recent psychiatric disorders was generally about double that of individuals with no psychiatric disorders, the levels of distress were substantially lower compared with those who received some mental health or substance abuse services.
DISCUSSION
This was a large multisite longitudinal study of over 700 men with medical hospitalizations. Of this sample, over half had at least one psychiatric diagnoses, including mood, anxiety, and substance use disorders, and almost one fifth (18%) experienced recent symptoms of a psychiatric disorder in the year before their index hospitalization. Over time, psychological distress increased for all surviving subjects, even in those without psychiatric diagnoses, both in individuals who had received mental health or substance abuse services and in those who did not. Health-related quality of life or health-related functioning did not improve and even worsened over time in many measures. On average, decrements in functioning associated with psychiatric disorders persisted over the year after the initial hospitalization and persisted even for those receiving minimal or extended mental health services. This long-term impairment in functioning associated with psychiatric disorders also remained after statistical control of medical diagnosis and severity of medical illness including number of medical/surgical hospitalizations over the year, as well as age and other demographic factors.
The negative impact of psychiatric illness on functioning is well known, and we have been able to examine the added impact of psychiatric illness in patients with medical illnesses severe enough to require hospitalization. In fact, just over half the longitudinal sample were sick enough to require additional medical or surgical hospitalization in the year after the index episode of care. We were able to examine the impact of a range of psychiatric disorders in the same study, including mood, anxiety and substance abuse disorders; previous studies have generally only examined a single disorder in medically ill patients, most commonly depression. This study extends the findings of recently published research examining mortality and health services use by medically hospitalized patients with depression. These studies found that co-occurring depression was significantly associated with earlier mortality37,38 and with greater use of health services after hospitalization.39 In fact, our study's documentation of substantially lower HRQL over time for patients with recent psychiatric and substance use disorders provides insight into the health processes that lead toward increased mortality and service use.
In an earlier report describing the associations between co-occurring psychiatric disorders and HRQL during the initial hospitalization,5 we questioned whether the negative associations of psychiatric comorbidity and psychological distress on self-reported functioning/HRQL could be separated from the immediate circumstances of a medical hospitalization. Many researchers have identified the difficulties of disentangling the stress surrounding medical illness and treatment, particularly the challenge of separating out the effect of the psychiatric disorder from the more short-term symptoms of depression and/or anxiety associated with acute medical conditions and hospitalization. Our data indicate that the substantial impairments in functioning associated with psychiatric disorders during medical hospitalization are not short-term and do not subside, but continue over the space of 1 year, despite of statistical control for two measures of severity of the medical illness.
We used a global measure of mental health services that did not determine their content, adequacy, or appropriateness. Some services may have been minimal or not consistent with current guidelines, but our measure of service use did provide an indication of contact with mental health providers with potential opportunities for appropriate interventions. Our intent was not to measure the effect of services on outcome but rather to examine whether we could account for the lower functioning associated with psychiatric disorders by the absence of mental health services. This was not the case because the impairments in functioning were strongest in those who received some mental health services. Such a finding is not surprising because of the selection effects—patients who received mental health services had lower HRQL and greater psychological distress at the index hospitalization, indicating the likelihood of poorer outcome over time.
One third of those with a recent psychiatric disorder in this longitudinal sample received at least one outpatient mental health or substance abuse visit or were hospitalized for similar reasons, indicating that a substantial proportion of needy patients were referred to mental health care after their medical or surgical hospitalization. Although we found no significant differences in referral rates between medicine and surgical discharges, the referral rates from surgical discharges were lower. This finding suggests that, when possible, general medical providers should review the mental health status of their postsurgery patients as well as after medical hospitalizations where they may have been in attendance.
Our finding that patients who received mental health or substance abuse services had worse functioning and distress compared with those who did not should not be interpreted as a discouragement to referrals. The HRQL and SCL-90 data show that patients who received these services had substantially lower functioning and greater distress in the index hospitalization, perhaps indicating that providers were indeed recognizing patients in need of specialty services. Without these interventions, impairments in these very sick individuals may well have been worse. Conversely, the persistence of impairment in the mental health service users may be a function of inadequate mental health care, including only minimal outpatient care, which we did not measure in this report. For example, depression treatment by mental health specialists may not conform to standard practice guidelines.40
Nonetheless, the findings in this study indicate the continued need for general medical physicians to evaluate the mental health status of their hospitalized or more seriously ill patients, recognizing that physician–patient contact time is often short in most current reimbursement systems. Evaluation can be performed formally using such brief assessments as the SF-36 5-item Mental Health Index scale and the CAGE screening for alcohol abuse41 that can be completed by patients before meeting with their physician. A structured program designed to include a combination of initial screening, primary care physician interventions, consultations with psychiatric or mental health specialists, and coordinated care over time should also be considered in general medicine practices.
One clinical option is to evaluate for signs and symptoms of distress during a medical crisis, continue to observe during follow-up care, and to intervene later if distress persists longer than a few weeks. Many psychiatric disorders, such as major depression, are treatable illnesses in primary care with a high likelihood of remission with appropriate treatment.42,43 Alcohol disorders are highly amenable to brief interventions delivered by physicians or other health care providers in medical settings.44,45 Patients with psychiatric disorders such as posttraumatic stress disorder may require more extensive care from a mental health practitioner. Patients with a history of mood and anxiety disorders may experience a relapse associated with the stress of acute or chronic medical illnesses and may require earlier interventions with medications or referrals for interventions by mental health providers.
There were several limitations to this study sample. First, the study did not include women because of the nature of the hospitalized veteran population, and we need to know whether these findings would replicate in female inpatients. There are gender differences in the prevalence of certain psychiatric disorders such as depression (higher in women) and substance abuse (higher in men),19,20 which might affect longitudinal changes in functioning for women. Second, we do not know how the findings for male veterans might generalize to other inpatient male samples, although there appears to be no difference between veterans' and nonveterans' use of health services.46 Veterans in the general population do not appear to have more psychiatric disorders than nonveterans, especially in the age groups and service cohorts most frequently represented in our study.47
Third, we did not measure non-VA services, which may have revealed additional mental health or substance abuse care. Nor did we review pharmacy records to determine new or renewed prescriptions for antidepressants, antianxiety medications, and other pharmacological interventions for mental disorders. However, it is important to also note that these medications are also used to treat many medical conditions as well as psychiatric disorders so that use of pharmacy records might have lead us to overcount mental health care.
In conclusion, we found that the lower HRQL and high psychological distress associated with co-occurring psychiatric disorders in hospitalized medical patients persisted over a year after the initial evaluation. In this era of accountability, report cards, and negotiations with health care payers, it is critical that mental health problems be addressed, accounted for, and treated effectively when examining health-related outcomes after medical care.
Acknowledgments
Supported by grants IIR 90-077 from the Health Services Research and Development Service, Department of Veterans Affairs to all the authors, P50-MH48197 from the National Institute of Mental Health, a Research Scientist Award from the National Institute on Drug Abuse (K02-DA00346) to Dr. Booth, and P50-AA07378 from the National Institute on Alcohol Abuse and Alcoholism to Dr. Blow.
REFERENCES
- 1.Derogatis LR, Morrow GR, Fetting J, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–7. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 2.Fulop G, Strain JJ, Vita J, Lyons JS, Hammer JS. Impact of psychiatric comorbidity on length of hospital stay for medical/surgical patients: a preliminary report. Am J Psychiatry. 1987;144:878–82. doi: 10.1176/ajp.144.7.878. [DOI] [PubMed] [Google Scholar]
- 3.Levenson JL, Hamer RM, Rossiter LF. Relation of psychopathology in general medical inpatients to use and cost of services. Am J Psychiatry. 1990;147:1498–503. doi: 10.1176/ajp.147.11.1498. [DOI] [PubMed] [Google Scholar]
- 4.Wells KB. Depression in general medical settings: Implications of three health policy studies for consultation-liaison psychiatry. Psychosomatics. 1994;35:279–96. doi: 10.1016/S0033-3182(94)71776-X. [DOI] [PubMed] [Google Scholar]
- 5.Booth BM, Blow FC, Cook C. Functional impairment and co-occurring psychiatric disorders in medically hospitalized men. Arch Intern Med. 1998;158:1551–9. doi: 10.1001/archinte.158.14.1551. [DOI] [PubMed] [Google Scholar]
- 6.Fulop G, Strain JJ, Fahs MC, Hammer JS, Lyons JS. Medical disorders associated with psychiatric comorbidity and prolonged hospital stay. Hosp Community Psychiatry. 1989;40:80–2. doi: 10.1176/ps.40.1.80. [DOI] [PubMed] [Google Scholar]
- 7.Henk HJ, Katzelnick DJ, Kobak KA, Greist JH, Jefferson JW. Medical costs attributed to depression among patients with a history of high medical expenses in a health maintenance organization. Arch Gen Psychiatry. 1996;53:899–904. doi: 10.1001/archpsyc.1996.01830100045006. [DOI] [PubMed] [Google Scholar]
- 8.Wells KB, Rogers W, Burnam MA, Camp P. Course of depression in patients with hypertension, myocardial infarction, or insulin-dependent diabetes. Am J Psychiatry. 1993;150:632–8. doi: 10.1176/ajp.150.4.632. [DOI] [PubMed] [Google Scholar]
- 9.McHorney CA, Ware Je, Jr, Raczek AE. The MOS 36-item short-form health survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care. 1993;31:247–63. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16:267–76. doi: 10.1016/0163-8343(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 11.Katon W, Schulberg H. Epidemiology of depression in primary care. Gen Hosp Psychiatry. 1992;14:237–47. doi: 10.1016/0163-8343(92)90094-q. [DOI] [PubMed] [Google Scholar]
- 12.Booth BM, Kirchner JE, Hamilton G, Harrell R, Smith GR. Diagnosing depression in the medically ill: validity of a lay-administered structured diagnostic interview. J Psychiatr Res. 1998;32:353–60. doi: 10.1016/s0022-3956(98)00031-4. [DOI] [PubMed] [Google Scholar]
- 13.McLellan AT, Grissom GR, Brill P, Durell J, Metzger DS, O'Brien CP. Private substance abuse treatments: are some programs more effective than others? J Subst Abuse Treat. 1993;10:243–54. doi: 10.1016/0740-5472(93)90071-9. [DOI] [PubMed] [Google Scholar]
- 14.McLellan AT, Luborsky L, O'Brien CP, Woody GE, Druley KA. Is treatment for substance abuse effective? JAMA. 1982;247:1423–8. [PubMed] [Google Scholar]
- 15.Hays RD, Wells KB, Sherbourne CD, Rogers W, Spritzer K. Functioning and well-being outcomes of patients with depression compared with chronic general medical illnesses. Arch Gen Psychiatry. 1995;52:11–9. doi: 10.1001/archpsyc.1995.03950130011002. [DOI] [PubMed] [Google Scholar]
- 16.Sherbourne CD, Hays RD, Wells KB. Personal and psychosocial risk factors for physical and mental health outcomes and course of depression among depressed patients. J Consult Clin Psychol. 1995;63:345–55. doi: 10.1037//0022-006x.63.3.345. [DOI] [PubMed] [Google Scholar]
- 17.Wells KB, Katon W, Rogers B, Camp P. Use of minor tranquilizers and antidepressant medications by depressed outpatients: results from the Medical Outcomes Study. Am J Psychiatry. 1994;151:694–700. doi: 10.1176/ajp.151.5.694. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd (revised) ed. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 19.Robins LN, Helzer JE, Weissman MM, et al. Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry. 1984;41:949–58. doi: 10.1001/archpsyc.1984.01790210031005. [DOI] [PubMed] [Google Scholar]
- 20.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 21.Bucholz KK, Marion SL, Shayka JJ, Marcus SC, Robins LN. A short computer interview for obtaining psychiatric diagnoses. Psychiatr Serv. 1996;47:293–7. doi: 10.1176/ps.47.3.293. [DOI] [PubMed] [Google Scholar]
- 22.Derogatis LR, Lipman RS, Covi L. SCL-90: an outpatient psychiatric rating scale-preliminary report. Psychopharmacol Bull. 1973;9:13–7. [PubMed] [Google Scholar]
- 23.Hoffmann NG, Overall PB. Factor structure of the SCL-90 in a psychiatric population. J Consult Clin Psychol. 1978;46:1187–91. [PubMed] [Google Scholar]
- 24.Derogatis LR, Rickels K, Rock AF. SCL-90 and the MMPI: a step in the validation of a new self-report scale. Br J Psychiatry. 1976;128:280–9. doi: 10.1192/bjp.128.3.280. [DOI] [PubMed] [Google Scholar]
- 25.Ware Je, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30:473–83. [PubMed] [Google Scholar]
- 26.Ware Je, Jr, Snow KK, Kosinski M, et al. SF-36 Health Survey Manual and Interpretation Guide. Boston: Health Institute, New England Medical Center; 1993. [Google Scholar]
- 27.Horn SD, Sharkey PD, Buckle JM, Backofen JE, Averill RF, Horn RA. The relationship between severity of illness and hospital length of stay and mortality. Med Care. 1991;29:305–17. doi: 10.1097/00005650-199104000-00001. [DOI] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Services. Volume 1: Diseases Tabular List. 2nd ed. Washington, DC: US Government Printing Office; 1980. International classification of Diseases: 9th Revision: Clinical Modification (ICD-9-CM) [Google Scholar]
- 29.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47:1245–51. doi: 10.1016/0895-4356(94)90129-5. [DOI] [PubMed] [Google Scholar]
- 30.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 31.Librero J, Peiro S, Ordinana R. Chronic comorbidity and outcomes of hospital care: length of stay, mortality, and readmission at 30 and 365 days. J Clin Epidemiol. 1999;52:171–9. doi: 10.1016/s0895-4356(98)00160-7. [DOI] [PubMed] [Google Scholar]
- 32.Krop JS, Powe NR, Weller WE, Shaffer TJ, Saudek CD, Anderson GE. Patterns of expenditures and use of services among older adults with diabetes. Diabetes Care. 1998;21:747–52. doi: 10.2337/diacare.21.5.747. [DOI] [PubMed] [Google Scholar]
- 33.Gibbons RD, Hedeker D. Application of random-effects probit regression models. J Consult Clin Psychol. 1994;62:285–96. doi: 10.1037//0022-006x.62.2.285. [DOI] [PubMed] [Google Scholar]
- 34.Gibbons RD, Hedeker D, Waternaux C, Davis JM. Random regression models: a comprehensive approach to the analysis of longitudinal psychiatric data. Psychopharmacol Bull. 1988;24:438–43. [PubMed] [Google Scholar]
- 35.Gibbons RD, Hedeker D, Elkin I, et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data: application to the NIMH treatment of depression collaborative research program dataset. Arch Gen Psychiatry. 1993;50:739–50. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 36.Fortney J, Booth B, Zhang M, Humphrey J, Wiseman E. Controlling for selection bias in the evaluation of Alcoholics Anonymous as aftercare treatment. J Stud Alcohol. 1998;59:690–97. doi: 10.15288/jsa.1998.59.690. [DOI] [PubMed] [Google Scholar]
- 37.Koenig HG, George LK, Larson DB, McCullough ME, Branch PS, Kuchibhatla M. Depressive symptoms and nine-year survival of 1,001 male veterans hospitalized with medical illness. Am J Psychiatry. 1999;7:124–31. [PubMed] [Google Scholar]
- 38.Covinsky KE, Kahana E, Chin MH, Palmer RM, Fortinsky RH, Landefeld CS. Depressive symptoms and 3-year mortality in older hospitalized medical patients. Ann Intern Med. 1999;130:563–69. doi: 10.7326/0003-4819-130-7-199904060-00004. [DOI] [PubMed] [Google Scholar]
- 39.Koenig HG, Kuchibhatla M. Use of health services by medically ill depressed elderly patients after hospital discharge. Am J Geriatr Psychiatry. 1999;7:48–56. [PubMed] [Google Scholar]
- 40.Fortney J, Rost K, Zhang M, Warren J. The impact of geographic accessibility on the intensity and quality of depression treatment. Med Care. 1999;37:884–93. doi: 10.1097/00005650-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 41.Ewing JA. Detecting alcoholism: the CAGE questionnaire. JAMA. 1984;252:1905–7. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- 42.Clinical Practice Guideline Number 5: Depression in Primary Care, 2. US Department of Health and Human Services. Rockville, Md: AHCPR publication 93-0551; 1993. Treatment of Major Depression. [Google Scholar]
- 43.Barlow DH, Lehman CL. Advances in the psychosocial treatment of anxiety disorders: implications for national health care. Arch Gen Psychiatry. 1996;53:727–35. doi: 10.1001/archpsyc.1996.01830080079013. [DOI] [PubMed] [Google Scholar]
- 44.Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems: a review. Addiction. 1993;88:315–35. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- 45.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers: a randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 46.Wolinsky FD, Coe RM, Mosely RR, II, Homan SM. Veterans' and nonveterans' use of health services: a comparative analysis. Med Care. 1985;23:1358–71. doi: 10.1097/00005650-198512000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Norquist GS, Hough RL, Golding JM, Escobar JI. Psychiatric disorder in male veterans and nonveterans. J Nerv Ment Dis. 1990;178:328–35. doi: 10.1097/00005053-199005000-00009. [DOI] [PubMed] [Google Scholar]