Abstract
OBJECTIVES
Chronically fatiguing illness, defined as fatigue for at least 6 months, has been associated with various physical health conditions. Our objective was to determine whether there is a significant relationship between chronically fatiguing illness and 10 clinical conditions that frequently appear to be associated with fatigue, adjusting for the potentially confounding effects of psychiatric illness.
DESIGN
A co-twin control study controlling for genetic and many environmental factors by comparing chronically fatigued twins with their nonfatigued co-twins.
SETTING
A nationally distributed volunteer twin registry.
PARTICIPANTS
The study included 127 twin pairs in which one member of the pair experienced fatigue of at least 6 months' duration and the co-twin was healthy and denied chronic fatigue. Fatigued twins were classified into three levels using increasingly stringent diagnostic criteria.
MEASUREMENTS AND MAIN RESULTS
Twins reported on a history of fibromyalgia, irritable bowel syndrome, multiple chemical sensitivities, temporomandibular disorder, interstitial cystitis, postconcussion syndrome, tension headache, chronic low back pain, chronic pelvic pain (women), and chronic nonbacterial prostatitis (men). The prevalence of these comorbid clinical conditions was significantly higher in the fatigued twins compared to their nonfatigued co-twins. Most notably, compared to their nonfatigued co-twins, the chronically fatigued twins had higher rates of fibromyalgia (>70% vs <10%) and irritable bowel syndrome (>50% vs <5%). The strongest associations were observed between chronic fatigue and fibromyalgia (odds ratios >20), irritable bowel syndrome, chronic pelvic pain, multiple chemical sensitivities, and temporomandibular disorder (all with odds ratios ≥4). Regression analysis suggested that the number of comorbid clinical conditions associated with chronic fatigue could not be attributed solely to psychiatric illness.
CONCLUSIONS
Chronically fatiguing illnesses were associated with high rates of many other clinical conditions. Thus, patients with chronic fatigue may present a complex clinical picture that poses diagnostic and management challenges. Nonetheless, clinicians should assess such patients for the presence of comorbid clinical conditions. Future research should provide a better understanding of the temporal relationship of the onset of fatigue and these conditions, and develop strategies for early intervention.
Keywords: chronic fatigue syndrome, twins, genetics, comorbidity, psychiatric disorders
Prolonged fatigue is a common symptom in primary care.1 Chronic fatigue, defined as fatigue of at least 6 months' duration, is associated with diverse physical health conditions. Chronic fatigue syndrome (CFS) is a less prevalent condition of unknown etiology characterized by debilitating, persistent fatigue. Its diagnosis requires at least four specified symptoms in the absence of exclusionary medical and psychiatric disorders that could be responsible for the fatigue.2 Thus, medical and psychiatric diagnoses such as cancer, AIDS, multiple sclerosis, schizophrenia, and bipolar disorder are all exclusionary for CFS. Clinically, patients with chronic fatigue and CFS often present with comorbid medical and psychiatric illnesses that are not regarded as part of the exclusion criteria.3–7
The relationship between CFS and several poorly understood nonexclusionary conditions such as fibromyalgia, irritable bowel syndrome, and multiple chemical sensitivity increasingly has been the focus of recent research. For example, although the hallmarks of CFS and fibromyalgia are persistent fatigue and chronic musculoskeletal pain, respectively, up to 90% of patients with fibromyalgia report significant fatigue3–5 and a similar percentage of adults with CFS experience myalgia, headache, and other local or diffuse pain.8 Furthermore, it has been estimated that in referral clinics, 20% to 70% of fibromyalgia patients meet criteria for CFS4,5,7 and, conversely, 35% to 70% of those with CFS have fibromyalgia.4,9 Although the overlap between CFS and fibromyalgia has received the most attention in the literature, several studies have also described symptoms consistent with multiple chemical sensitivity,4,10 irritable bowel syndrome,11,12 and interstitial cystitis in fatigued individuals.13 However, the degree of association of these comorbid clinical conditions with fatigue and CFS is unknown. Furthermore, whether the apparent overlap results from shared underlying mechanisms or coexisting psychiatric disorders remains controversial.
Our primary objective was to determine if there is a significant relationship between chronically fatiguing illness and 10 clinical conditions that appear to be associated with fatigue, adjusting for the potentially confounding effects of psychiatric illness.
SUBJECTS AND METHODS
Study Design
We used the matched pair co-twin control method that directly compared twins with chronic fatigue or CFS to their healthy, nonfatigued co-twins with respect to differences in the number and type of comorbid clinical conditions. Unlike studies that compare CFS patients to healthy or depressed controls, this method also adjusts for the numerous characteristics shared by twin pairs such as age, race, preadult home environment, and genetic factors (100% in monozygotic twins and 50% on average in dizygotic twins).14
Registry Construction and Content
Twins were members of the CFS Twin Registry established in 1993 at the University of Washington. The twins had been identified through advertisements placed in national and international organizations and other sources. The advertisements did not state that a physician fatigue-related diagnosis was required. This was for several reasons. First, the criteria for CFS may not be strictly applied in community settings. Second, some individuals with fatigue may not have sought medical care. Lastly, we wished to classify twin pairs using increasingly stringent fatigue criteria applying an algorithm based on the 1994 Centers for Disease Control and Prevention (CDC) CFS case definition.2 For each pair, the twin making the initial inquiry was asked to provide their co-twin's name, address, and telephone number. No telephone screening was conducted. Written, informed consent was obtained from each registry member in accordance with the regulations of our Institutional Human Subjects Office.
A total of 632 twins responded to our solicitation and requested the registry intake questionnaire. Of these, 454 (72%) individuals returned the questionnaire. Of the 233 twin pairs identified in whom 1 or both members met the study inclusion criteria of persistent fatigue for at least 6 months, 55% were recruited through patient support group newsletters, 10% through clinicians/researchers familiar with CFS and fibromyalgia, 18% through notices placed on electronic bulletin boards, 6% through twin organizations and researchers, 3% through relatives and friends, 3% through other national and international contacts, and 6% through unknown sources. Complete data were available for both members of 204 (88%) twin pairs; 127 (62%) were discordant for ≥6 month fatigue and therefore eligible for this study.
The mailed questionnaires collected data on an extensive range of topics including demographic data; zygosity; habits; lifestyle; distress; physical health conditions; the nature, extent, and consequences of fatigue; and the symptoms of CFS.2 For nonfatigued subjects, a control version of questions was used that did not reference chronic fatigue. Physical health was measured by self-report using a checklist of medical disorders. As part of the intake questionnaire, all twins were presented with an extensive list of physical health problems that included the 10 comorbid clinical conditions. For each condition, the respondent was asked, “Have you ever had this problem?” If the answer was “yes,” the twin was asked if they had ever been seen by a physician for the specific condition.
Zygosity was assigned to the twin pairs using a previously validated method employing the response to the following question: “As children, were you and your twin as alike as two peas in a pod, or of only ordinary family resemblance?”15,16 Pairs whose responses were concordant for this question were classified as monozygotic or dizygotic. Pairs whose responses disagreed were assigned zygosity using an algorithm based on several questions about childhood similarity. A more complete description of the registry construction has been published elsewhere.17
Psychiatric Disorders
To ascertain psychiatric conditions, the Diagnostic Interview Schedule Version III-A (DIS)18 was administered by telephone. The DIS is a structured interview that uses a computer algorithm to assign lifetime psychiatric diagnoses based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Revised Third Edition.19 A trained research assistant administered the sections on major depression, dysthymia, generalized anxiety, panic, agoraphobia, posttraumatic stress disorder, mania, bipolar disorders, schizophrenia, eating disorders, somatization, and substance abuse and dependence. Telephone administration of the DIS has been validated in several large studies.20,21 Psychiatric conditions exclusionary for the diagnosis of CFS included lifetime mania, hypomania, bipolar disorder, schizophrenia, major depression with psychotic or melancholic features, anorexia or bulimia nervosa, and current alcohol or substance abuse/dependence.
Clinical Conditions
Based on a computerized search of the medical literature from 1975–1999, a review of extant publications, and our clinical experience, we identified 10 clinical conditions listed on the questionnaire that appeared to be commonly associated with CFS: fibromyalgia, irritable bowel syndrome, multiple chemical sensitivity, temporomandibular disorder, interstitial cystitis, postconcussion syndrome, tension headache, chronic low back pain, chronic pelvic pain (women), and chronic nonbacterial prostatitis (men). These syndromes have the following in common: (1) an unknown etiology; (2) the absence of objective findings on physical or laboratory examination; (3) disability often out of proportion to pathophysiology; and (4) exacerbations associated with “stress.” Importantly, none of the 10 conditions we identified are considered as exclusionary according to the 1994 CDC criteria for CFS.2 A comorbid clinical condition was considered to be present only when respondents endorsed having both the condition and a physician evaluation for that problem. Finally, we computed a summary measure consisting of the total number of these comorbid clinical conditions.
Eligibility Criteria and Fatigue Definition
As described above, all twin pairs in the registry reported that at least one member had chronic fatigue of at least 6 months' duration. The 127 twins pairs eligible to participate in the current study were classified into three progressively more stringent definitions of chronic fatigue.
Level 1 Chronic Fatigue.
To be eligible for inclusion in the level 1 group, twin pairs had to contain one member who responded “yes” to the question, “Have you been fatigued for at least 6 months?” The co-twin responded “no” to this question.
Level 2 Chronic Fatigue.
The level 2 group was defined using the 1994 CDC CFS criteria based on responses to the questionnaire and the DIS telephone interview. Following these criteria, twins in level 2 reported at least four of the eight CFS symptoms, a body mass index less than 45, and none of the exclusionary medical (see below) or psychiatric disorders. This group was considered to have presumptive CFS. For inclusion in the analyses, the exclusion criteria were applied both to fatigued and to nonfatigued co-twins.
The medical diagnoses considered exclusionary were developed by consensus of two internists, a psychiatrist with expertise in CFS, an infectious disease specialist, and an emergency department physician with knowledge of, but little clinical exposure to, CFS. Examples of exclusionary conditions included (but were not limited to) steroid-dependent asthma, infectious hepatitis, diabetes, cancer (other than skin), congestive heart failure, stroke, cirrhosis, multiple sclerosis, and systemic lupus erythematosus. To assess reliability, self-reported conditions were compared to physician confirmation of these diagnoses by chart review and telephone contact with treating physicians for 44 twins. Within this sample, no fatigued twin was found to have an exclusionary medical condition that was missing or inaccurately obtained by self-report. Conversely, no exclusionary conditions were observed in any twin who reported good health.
Level 3 Chronic Fatigue.
The most restrictive classification, level 3, required twins to be at least 18 years of age, monozygotic, reared together, and discordant for CFS. They also had to be willing to travel together to Seattle to undergo a comprehensive clinical and laboratory evaluation, and be willing to discontinue alcohol, caffeine, and all medications 2 weeks prior to and during the evaluation. First, fatigued and nonfatigued twins were screened as described above for level 2. Next, all medical records for the past 5 years were reviewed by an internist (D.B.) for potentially exclusionary conditions. Of the 29 twin pairs who met the stringent eligibility criteria and were invited to participate, 22 (76%) completed a 7-day evaluation in our research clinic that included laboratory and diagnostic studies, and a physical examination. Four (14%) were unable to discontinue potentially interfering medications, 2 (7%) had a scheduling conflict with work or school, and 1 (3%) refused to participate. Only monozygotic twins were included in this group in order to control completely for genetic influences. All fatigued level 3 twins met the CDC case definition for CFS.
Statistical Analyses
Descriptive analyses estimated the prevalence of the lifetime comorbid clinical conditions in fatigued and nonfatigued twins. We then calculated matched pair odds ratios (ORs) and exact 95% confidence intervals (CIs) to assess the magnitude of the association between fatigue and the 10 individual comorbid conditions.22 These analyses were performed separately for each of the three levels of chronic fatigue. It should be noted that in no case was there a differential pattern of association between fatigue level and comorbidity by zygosity or gender; therefore, results were pooled across zygosity and gender.
To assess the association of chronic fatigue and the count of comorbid conditions after adjustment for potential confounding factors, we used random-effects regression models23 for ordinal dependent variables. This approach accounts for the paired structure of the data and estimates the strength of the association between chronic fatigue and the count of comorbid conditions in terms of adjusted ORs and 95% CIs. We developed three different regression models to assess confounding. An initial regression model included only the effects of chronic fatigue on the total number of comorbid conditions. The second model included chronic fatigue as well as the sociodemographic factors of age, sex, zygosity, educational level, marital status, and number of children. A third regression model included chronic fatigue, the sociodemographic factors listed above, and the number of nonexclusionary psychiatric diagnoses. The number of psychiatric diagnoses was calculated based on a count of the diagnoses that did not exclude a diagnosis of CFS: major depressive episode, depression not otherwise specified, dysthymia, panic disorder, generalized anxiety disorder, and posttraumatic stress disorder. Analyses were conducted using SPSS for Windows, Version 6.1.4 (SPSS, Inc., Chicago, Ill); SAS for Windows, Version 6.12 (SAS Institute, Inc., Cary, NC); MIXOR, Version 2 (shareware by Donald Hedecker, PhD and Robert D. Gibbons, PhD, UIC, Chicago, Ill); and PEPI Pairs, Version 3 (shareware by JH Abramson and PM Gahlinger, USD, Inc., Stone Mountain, Ga).
RESULTS
Subject Characteristics and Prevalence of Comorbid Conditions
Table 1 presents the distribution of eligible twins according to zygosity, sex, and chronic fatigue level along with basic demographic information on age, education, and marital status. A more detailed account of subject characteristics has been previously published.17 On a 10-point scale that rated their fatigue during the last week (1 = least and 10 = most fatigue), fatigued twins had a mean score of 7.7 and nonfatigued twins a mean of 3.1. The prevalence data for the 10 comorbid clinical conditions in fatigued and nonfatigued twins are shown in Table 2. With the exception of chronic nonbacterial prostatitis, the fatigued twins more frequently endorsed receiving a lifetime diagnosis for each of the comorbid conditions examined. The most commonly reported conditions affecting fatigued twins at some time in their lives were fibromyalgia (range, 72% 77%), irritable bowel syndrome (range, 52% 59%), chronic low back pain (range, 43% 48%), and tension headache (range, 39% 46%). Temporomandibular disorder and chronic pelvic pain occurred in one quarter to one third of fatigued twins; considerably less frequent were multiple chemical sensitivity (range, 11% 24%), interstitial cystitis (range, 9% 17%), and postconcussion syndrome (range, 5% 8%). The distribution of the count of comorbid conditions was dramatically different between fatigued and nonfatigued twins at all levels of diagnostic stringency. Over 60% of fatigued twins experienced three or more comorbid conditions; in contrast, more than 75% of the nonfatigued co-twins reported no or only one condition.
Table 1.
Zygosity and Demographic Characteristics of Twins by Fatigue Classification*
| Level 1 Fatigue ≥6 Months (n = 127 pairs) | Level 2 Presumptive CFS (n = 80 pairs) | Level 3 Clinical CFS Diagnosis (n = 22 pairs) | |
|---|---|---|---|
| Gender and zygosity, % | |||
| Male-male monozygotic | 4 | 6 | 9 |
| Female-female monozygotic | 54 | 54 | 91 |
| Male-male dizygotic | 2 | 3 | 0 |
| Female-female dizygotic | 24 | 23 | 0 |
| Male-female dizygotic | 15 | 15 | 0 |
| Demographics | |||
| White, % | 99 | 100 | 100 |
| Year of birth, % ± SE | 1953 ± 0.9 | 1953 ± 1.6 | 1957 ± 2.1 |
| Education, mean years ± SE | 14.6 ± 0.2 | 14.8 ± 0.2 | 14.3 ± 1.4 |
| Children, mean number ± SE | 1.4 ± 0.1 | 1.5 ± 0.1 | 1.4 ± 0.2 |
| Married, % | 61 | 63 | 59 |
CFS indicates chronic fatigue syndrome.
Table 2.
Frequency of Comorbid Clinical Conditions Among Fatigued and Nonfatigued Twins by Fatigue Classification*
| Level 1 Fatigue ≥6 Months | Level 2 Presumptive CFS | Level 3 Clinical CFS Diagnosis | ||||
|---|---|---|---|---|---|---|
| Fatigued | Nonfatigued | Fatigued | Nonfatigued | Fatigued | Nonfatigued | |
| Individual diagnoses, %† | ||||||
| Fibromyalgia | 72 | 7 | 75 | 4 | 77 | 0 |
| Irritable bowel syndrome | 52 | 14 | 54 | 14 | 59 | 9 |
| Multiple chemical sensitivities | 13 | 2 | 11 | 3 | 24 | 0 |
| Temporomandibular disorder | 29 | 11 | 33 | 11 | 27 | 14 |
| Interstitial cystitis | 17 | 2 | 16 | 1 | 9 | 5 |
| Postconcussion syndrome | 6 | 2 | 8 | 0 | 5 | 0 |
| Tension headache | 42 | 22 | 39 | 22 | 46 | 23 |
| Chronic low back pain | 48 | 25 | 48 | 23 | 43 | 24 |
| Chronic pelvic pain‡ | 26 | 7 | 25 | 8 | 30 | 5 |
| Chronic nonbacterial prostatitis§ | 0 | 0 | 0 | 0 | 0 | 0 |
| Comorbid clinical conditions‖ | ||||||
| None | 8 | 56 | 7 | 55 | 5 | 48 |
| 1 | 15 | 19 | 12 | 23 | 14 | 33 |
| 2 | 13 | 11 | 12 | 13 | 5 | 14 |
| ≥3 | 63 | 14 | 69 | 9 | 76 | 5 |
Percentages may not add up to one hundred due to missing data from some twin pairs for certain conditions.
For level 1, n = 127 pairs; for level 2, n = 80 pairs; and for level 3, n = 22 pairs.
Percentages based on female-female twin pairs only: for level 1, n = 99 pairs; for level 2, n = 62 pairs; and for level 3, n = 20 pairs.
Percentages based on male-male twin pairs only: for level 1, n = 8 pairs; for level 2, n = 7 pairs; and for level 3, n = 2 pairs.
For level 1, n = 120 pairs; for level 2, n = 75 pairs; and for level 3, n = 21 pairs.
CFS indicates chronic fatigue syndrome
Odds Ratio Analysis
The ORs for the association of fatigue with each of the 10 clinical conditions are displayed in Table 3 for the three progressively more stringent levels of fatigue. Fatigued twins were more than 20 times more likely to report a lifetime diagnosis of fibromyalgia, and 4 to 10 times more likely to be diagnosed with irritable bowel syndrome, temporomandibular disorder, multiple chemical sensitivity, and chronic pelvic pain compared to their unaffected co-twin regardless of the definition of chronic fatigue. Similarly, fatigued twins experienced more than a 2-fold increase in the prevalence of chronic tension headache and chronic low back pain compared to the nonfatigued twins. Despite higher rates of lifetime clinical conditions among the fatigued twins in the level 3 group, the small number of pairs, and consequent decrease in statistical power, precluded achieving statistically significant findings for individual comorbid conditions aside from irritable bowel syndrome. A striking association between chronic fatigue and the total number of comorbid clinical conditions was observed. The ORs progressively increased with the level of diagnostic stringency (from 14.1 to 29.4 to 92.6), although the CIs were broad.
Table 3.
Odds Ratio Analysis of Comorbid Clinical Conditions Among Fatigued and Nonfatigued Twins by Fatigue Classification
| Level 1 Fatigue ≥6 Months (n = 127 pairs) | Level 2 Presumptive CFS (n = 80 pairs) | Level 3 Clinical CFS Diagnosis (n = 22 pairs) | |
|---|---|---|---|
| Lifetime Diagnosis | OR (95% CI) | OR (95% CI) | OR (95% CI) |
| Fibromyalgia | 21.5 (8.1 to 80.7) | 29.5 (7.8 to 249.3) | ‡ |
| Irritable bowel syndrome | 9.0 (3.9 to 25.6) | 7.4 (2.9 to 24.1) | 6.5 (1.5 to 59.3) |
| Multiple chemical sensitivities | 7.5 (1.7 to 67.6) | 8.0 (1.1 to 355.0) | ‡ |
| Temporomandibular disorder | 4.1 (1.8 to 11.2) | 4.4 (1.6 to 15.0) | 4.0 (0.4 to 197.0) |
| Interstitial cystitis | 20.0 (3.2 to 829.0) | 13.0 (2.0 to 552.5) | 2.0 (0.1 to 118.0) |
| Postconcussion syndrome | 6.0 (0.7 to 276.0) | ‡ | ‡ |
| Tension headache | 2.7 (1.4 to 5.2) | 2.4 (1.1 to 6.0) | ‡ |
| Chronic low back pain | 3.3 (1.7 to 6.7) | 3.2 (1.5 to 7.7) | 3.0 (0.5 to 30.4) |
| Chronic pelvic pain* | 5.8 (2.0 to 22.9) | 3.5 (1.1 to 14.6) | 6.0 (0.7 to 276.0) |
| Chronic nonbacterial prostatitis†‡ | ‡ | ‡ | |
| No. of comorbid conditions | 14.1 (7.6 to 26.1) | 29.4 (12.1 to 71.3) | 92.6 (7.6 to 1135.2) |
Female-female twin pairs only.
Male-male twin pairs only.
Undefined.
CFS indicates chronic fatigue syndrome; 95% CI, 95% confidence interval.
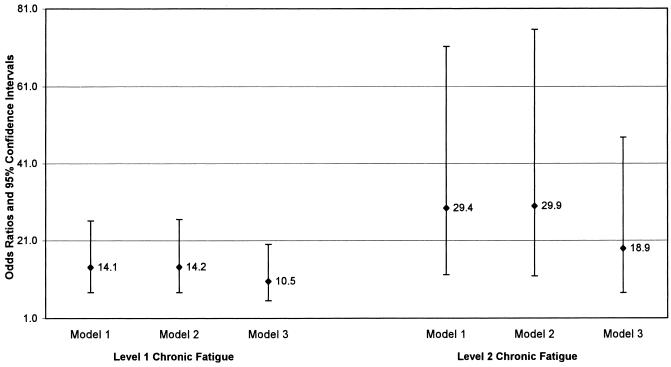
Regression Analysis of the Count of Comorbid Conditions
Figure 1 presents the regression-derived ORs (and their 95% CIs) between chronic fatigue and the number of lifetime comorbid clinical conditions for the level 1 and 2 definitions of chronic fatigue. Regression models could not be generated for the level 3 definition because of sample size limitations. The initial regression analysis (model 1) is equivalent to the unadjusted ORs found in Table 3 for the number of comorbid conditions and chronic fatigue. There is little evidence of confounding due to sociodemographic factors (model 2) because the ORs are nearly identical to the unadjusted estimates. However, when adjusted for the number of nonexclusionary psychiatric conditions (model 3), the ORs, while still large, are substantially reduced (from 14 to 11 for level 1 and from 29 to 19 for level 2).
FIGURE 1.
Odds ratios and 95% confidence intervals for chronic fatigue and the number of comorbid clinical conditions. Model 1 is unadjusted. Model 2 is adjusted for age, sex, zygosity, educational level, marital status, and number of children. Model 3 is adjusted for the sociodemographic factors used in model 2 and the number of nonexclusionary psychiatric disorders.
DISCUSSION
The 1994 publication that summarized the CDC criteria for CFS urged investigators to better define the co-occurrence of fatigue with the many other health conditions frequently observed in patients with chronic fatigue, regardless of their apparent relatedness to CFS.2 In the present study, fibromyalgia, irritable bowel syndrome, temporomandibular disorder, tension headache, and chronic low back pain were the conditions most commonly comorbid with chronic fatigue. Over a 70% lifetime prevalence of fibromyalgia was reported by fatigued twins, and fatigued twins were 20 times more likely than their nonfatigued co-twins to suffer from this disorder. These results are consistent with previous studies documenting that among adults with CFS, as many as 90% experience myalgias and other local or diffuse pain,8 and 35% to 70% meet criteria for fibromyalgia.4,9 Similarly, in patients diagnosed with fibromyalgia, up to 90% are fatigued, and 42% actually have CFS.3–5,7,8
While the overlap between fibromyalgia, chronic fatigue, and CFS has been relatively well characterized, the relationship of fatigue to many of the other clinical conditions under study is considerably less clear. The only publication to systematically examine the relationship of chronic fatigue to irritable bowel syndrome24 found that 73% of chronically fatigued adults met the Manning symptom-based irritable bowel syndrome criteria25 over a 1-year retrospective time period. This somewhat higher than the physician-diagnosed lifetime estimates of irritable bowel syndrome reported by our fatigued twins (52% 59%). We previously observed that when the Manning case definition was applied to CFS clinic patients, up to 92% met lifetime criteria for irritable bowel syndrome.26 Although definitions differ across studies, these rates all greatly exceed the estimated prevalence of irritable bowel syndrome in the general population which ranges from 9% to 21%,27 suggesting that chronically fatigued individuals are disproportionately affected with this condition.
Although temporomandibular disorder, tension headache, and low back pain commonly occur in syndromes of chronic painlike fibromyalgia,28,29 and are reported anecdotally among CFS patients, to our knowledge, these relationships have not been investigated in fatigued populations. This is surprising because we noted relatively high lifetime rates and a two- to four-fold increase in the likelihood of having these three conditions among the fatigued twins compared to their nonfatigued co-twins. Similarly, there has been no information published on the frequency of interstitial cystitis or chronic pelvic pain among chronically fatigued individuals. While interstitial cystitis was not one of the more prevalent disorders in the level 3 group, it was associated with an OR of 20 in the level 1 sample. In support of an overlap with chronic fatigue, a recent, large survey found that 9% of interstitial cystitis patients had CFS.13 Finally, with regard to multiple chemical sensitivity, our earlier study noted that 53% to 67% of CFS patients reported a worsening of their multisystem symptoms with exposure to various chemicals.4 The lower prevalence of multiple chemical sensitivity (11% 24%) reported by fatigued twins probably reflects the difference between the frequency of a symptom (hypersensitivity) and a more well-defined syndrome (multiple chemical sensitivity). Alternately, as some have argued, multiple chemical sensitivity may often be unrecognized by affected individuals or treating physicians leading to an underestimation of this disorder among fatigued individuals.30
Given the common perception that manifestations of CFS and related disorders such as fibromyalgia may be explained, at least in part, by underlying psychiatric disorders,31 investigating this association was of great interest. Thus, we examined whether the consistently higher frequency of comorbid conditions among the fatigued twins would be observed when adjusted for the number of lifetime affective and anxiety psychiatric disorders. The OR comparing the frequency of comorbid conditions between fatigued and nonfatigued twins was greater than 10, even after adjusting for psychiatric status, suggesting that the association was not solely the consequence of psychiatric illness.
If the relationship between chronic fatigue and the associated clinical conditions assessed here is not primarily attributable to psychiatric factors, what are possible alternative explanations? It seems highly probable that the manifestation of chronic fatigue and a spectrum of comorbid conditions is due to the complex interplay between genes and environmental influences.7,14 Moreover, the “hardwiring” of perception almost certainly has a heritable basis,32 and symptom perception has cognitive and psychological components that depend on information processing by the central nervous system. In this regard, studies have shown that pain perception is related to activation of cortical and subcortical brain structures in patients with fibromyalgia.33 Furthermore, objective similarities among some clinical conditions such as increased pain sensitivity in patients with fibromyalgia and interstitial cystitis suggest a possible common alteration in central processing mechanisms.34 Finally, the high rates of health care utilization among patients with chronic fatigue, CFS, and fibromyalgia35,36 suggest that one consequence of excessively seeking health care may be the receipt of multiple diagnoses.
Clinically, patients with multiple syndromes may be more difficult to treat than those with a single condition. One clinical study observed that temporomandibular disorder patients with poor outcomes had significantly more general health complaints.37 Other investigators have noted that patients with temporomandibular disorder who also have nonmasticatory musculoskeletal complaints were more refractory to treatment than those without auxiliary pain.38 The degree of comorbidity also may have a substantial negative impact on health care utilization and costs. For example, the number of concurrent health conditions among fibromyalgia patients was the most powerful predictor of total health care costs in a recent 7-year, multicenter prospective study.35 In chronically fatigued patients, comorbid clinical conditions may further compound the social cost of an illness already associated with substantial economic consequences in terms of health care, excessive unemployment, and functional disability.36,39 Thus, our findings, in conjunction with others cited here, should alert providers to the potentially devastating cumulative effects of these conditions and argue for early and aggressive intervention.
This co-twin control study had several notable limitations. First, the study relied on self-reported health conditions rather than on a clinical examination and review of medical records for all subjects. This may be particularly problematic for the 10 comorbid clinical conditions under investigation. This methodology could have resulted in either an over- or underestimation of the fatigue-associated conditions we evaluated, depending on the accuracy of the twins' reporting. However, at least for the medical diagnoses exclusionary for CFS, we presented evidence based on written and verbal communication with physicians that self-report appeared to be valid. Second, the method used to identify the sample was not ideal. Solicitation by advertisement resulted in a volunteer sample of twin pairs with the potential for ascertainment problems. However, the more desirable strategy of systematically identifying twins from a well-defined population-based twin registry is not readily accomplished in the United States. Although we emphasized in all recruitment efforts that twins were desired regardless of either the health of their co-twin or a definitive CFS diagnosis, subjects likely screened themselves as eligible or ineligible. This could likely limit the generalizability of our findings to more severely fatigued individuals, such as those found in tertiary care clinics.
A third limitation is related to sample size. Because the clinically diagnosed group consisted of only 22 pairs, we had insufficient power to make definitive statements about the relationship of CFS to specific conditions under study. However, we were able to demonstrate a greater than 90-fold OR between the number of comorbid conditions associated with CFS in the level 3 sample. Other potential problems arise from difficulties in defining and identifying these conditions. Several of the illnesses under study are controversial and do not have a universally agreed upon case definition. Furthermore, the criteria applied by diverse physicians representing many disciplines may have influenced our findings because certain specialties may be more (or less) likely to recognize and diagnose comorbid clinical conditions. Lastly, results from this study cannot ascertain whether their onset came before or after the development of CFS.
In conclusion, this co-twin control study is the first to demonstrate that individuals with a range of fatiguing illnesses have a consistently increased likelihood of experiencing selected comorbid clinical conditions compared to exceedingly well-matched, healthy controls who denied chronic fatigue. These results were independent of the stringency of the case definition for fatigue and the degree of psychiatric morbidity. We relied upon the strengths of a twin design because this method is especially well suited to the study of disorders of unknown etiology and those for which the appropriate comparison groups are not clearly defined.14 Because they control, to a substantial extent, for genetic and environmental factors, twin studies offer a unique approach to the examination of CFS and comorbid conditions—illnesses that represent complex interactions of biological, psychological, and environmental factors. Investigators with access to unselected, population-based twin registries should attempt to replicate our findings to better determine the relative influences of genetic and noninherited factors underlying the relationships between fatigue and related illnesses. Future research should also investigate the temporal relationship of fatigue onset to the appearance of other clinical conditions, and assess the usefulness of early interventions.
Acknowledgments
This work was funded by grant U19 AI38429 from the NIAID (Dr. Buchwald). The authors would like to thank the participants in the University of Washington Twin Registry for their cooperation, patience, and goodwill, and Dr. Leigh Sawyer, Program Officer, NIAID for her encouragement and support. We also wish to acknowledge our Advisory Panel, who with sage advice and ongoing encouragement, improved our scientific efforts.
REFERENCES
- 1.Bates DW, Schmitt W, Buchwald D, et al. Prevalence of fatigue and chronic fatigue syndrome in a primary care practice. Arch Intern Med. 1993;153:2759–65. [PubMed] [Google Scholar]
- 2.Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A International Chronic Fatigue Syndrome Study Group. The chronic fatigue syndrome: a comprehensive approach to its definition and study. Ann Intern Med. 1994;121:953–9. doi: 10.7326/0003-4819-121-12-199412150-00009. [DOI] [PubMed] [Google Scholar]
- 3.Buchwald D, Goldenberg DL, Sullivan JL, Komaroff AL. The “chronic, active Epstein-Barr virus infection” syndrome and fibromyalgia. Arthritis Rheum. 1987;30:1132–6. doi: 10.1002/art.1780301007. [DOI] [PubMed] [Google Scholar]
- 4.Buchwald D, Garrity D. Comparison of patients with chronic fatigue syndrome, fibromyalgia, and chemical sensitivities. Arch Intern Med. 1994;154:2049–53. [PubMed] [Google Scholar]
- 5.Wysenbeek AJ, Shapira Y, Leibovici L. Primary fibromyalgia and the chronic fatigue syndrome. Rheumatol Int. 1991;10:227–9. doi: 10.1007/BF02274883. [DOI] [PubMed] [Google Scholar]
- 6.Manu P, Matthews DA, Lane TJ. The mental health of patients with a chief complaint of chronic fatigue. Arch Intern Med. 1988;148:2213–7. [PubMed] [Google Scholar]
- 7.Hudson JI, Goldenberg DL, Pope HG, Keck PE, Schlesinger L. Comorbidity of fibromyalgia with medical and psychiatric disorders. Am J Med. 1992;92:363–7. doi: 10.1016/0002-9343(92)90265-d. [DOI] [PubMed] [Google Scholar]
- 8.Komaroff AL, Buchwald D. Symptoms and signs in chronic fatigue syndrome. Rev Infect Dis. 1991;13:S8–S11. doi: 10.1093/clinids/13.supplement_1.s8. [DOI] [PubMed] [Google Scholar]
- 9.Goldenberg DL, Simms RW, Geiger A, Komaroff AK. High frequency of fibromyalgia in patients with chronic fatigue seen in a primary care practice. Arthritis Rheum. 1990;33:381–7. doi: 10.1002/art.1780330311. [DOI] [PubMed] [Google Scholar]
- 10.Ziem G, McTamney J. Profile of patients with chemical injury and sensitivity. Environ Health Perspect. 1997;105:417–36. doi: 10.1289/ehp.97105s2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sivri A, Cindas A, Dincer F, et al. Bowel dysfunction and irritable bowel syndrome in fibromyalgia patients. Clin Rheumatol. 1997;15:233–5. doi: 10.1007/BF02229708. [DOI] [PubMed] [Google Scholar]
- 12.Veale D, Kavanagh G, Fielding JF, et al. Primary fibromyalgia and the irritable bowel syndrome: different expressions of a common pathogenetic process. Br J Rheumatol. 1991;30:220–2. doi: 10.1093/rheumatology/30.3.220. [DOI] [PubMed] [Google Scholar]
- 13.Alagiri M, Chottiner S, Ratner V, Slade D, Hanno PM. Interstitial cystitis: unexplained associations with other chronic disease and pain syndromes. Urology. 1997;49(Suppl 5A):52–7. doi: 10.1016/s0090-4295(99)80332-x. [DOI] [PubMed] [Google Scholar]
- 14.Hubric Z, Robinette CD. The study of human twins in medical research. N Engl J Med. 1984;310:435–41. doi: 10.1056/NEJM198402163100706. [DOI] [PubMed] [Google Scholar]
- 15.Torgersen S. The determination of twin zygosity by means of a mailed questionnaire. Acta Genet Med Gemellol (Roma) 1979;28:225–36. doi: 10.1017/s0001566000009077. [DOI] [PubMed] [Google Scholar]
- 16.Eisen SA, Neuman R, Goldberg J, Rice J, True W. Determining zygosity in the Vietnam Era Twin Registry: an approach using questionnaires. Clin Genet. 1989;35:423–32. doi: 10.1111/j.1399-0004.1989.tb02967.x. [DOI] [PubMed] [Google Scholar]
- 17.Buchwald DS, Herrell R, Ashton S, Belcourt M, Schmaling K, Goldberg J. The chronic fatigue twin registry: method of construction, composition and zygosity assignment. Twin Res. 1999;2:203–11. doi: 10.1375/136905299320565870. [DOI] [PubMed] [Google Scholar]
- 18.Robins LN, Helzer JE. Diagnostic Interview Schedule (DIS): Version III-A. St. Louis: Department of Psychiatry, Washington University School of Medicine; 1985. [Google Scholar]
- 19.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. Revised Third Edition. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- 20.Wells KB, Burnan MA, Leake B, Robins LN. Agreement between face-to-face and telephone administered versions of the depression section of the NIMH Diagnostic Interview Schedule. J Psychiatr Res. 1988;22:207–20. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- 21.Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews in assessing axis I and axis II disorders. Am J Psychiatry. 1997;154:1593–8. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- 22.Breslow NE, Day NE. The Analysis of Case-Control Studies. Vol. 1. New York, NY: Oxford University Press; 1980. Statistical Methods in Cancer Research. [PubMed] [Google Scholar]
- 23.Hu FB, Goldberg J, Hedecker D, Henderson WG. Modelling ordinal responses from co-twin control studies. Stat Med. 1998;17:957–70. doi: 10.1002/(sici)1097-0258(19980515)17:9<957::aid-sim791>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 24.Gomborone JE, Gorard DA, Dewsnap PA, Libby GW, Farthing MJ. Prevalence of irritable bowel syndrome in chronic fatigue. J R Coll Physicians Lond. 1996;30:512–3. [PMC free article] [PubMed] [Google Scholar]
- 25.Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. BMJ. 1978;2:653–4. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aaron LA, Burke MM, Buchwald D. Overlapping conditions among patients with chronic fatigue syndrome, fibromyalgia, and temporomandibular disorder. Arch Intern Med. 2000;160:221–7. doi: 10.1001/archinte.160.2.221. [DOI] [PubMed] [Google Scholar]
- 27.Talley NJ, Boyce PM, Jones M. Predictors of health care seeking for irritable bowel syndrome: a population based study. Gut. 1997;41:394–8. doi: 10.1136/gut.41.3.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Plesh O, Wolfe F, Lane N. The relationship between fibromyalgia and temporomandibular disorders: prevalence and symptom severity. J Rheumatol. 1996;23:1948–52. [PubMed] [Google Scholar]
- 29.Yunus MB. Fibromyalgia syndrome: clinical features and spectrum. J Musculoskeletal Pain. 1994;2:5–19. [Google Scholar]
- 30.Ziem G, Donnay A. Chronic fatigue, fibromyalgia and chemical sensitivity: overlapping disorders. Arch Intern Med. 1995;155:1913. [PubMed] [Google Scholar]
- 31.Hudson JI, Harrison Hg., Jr Fibromyalgia and psychopathology: is fibromyalgia a form of “affective spectrum disorder?”. J Rheumatol. 1989;16(suppl 19):15–22. [PubMed] [Google Scholar]
- 32.Watson D, Pennebaker JW. Situational, dispositional, and genetic bases of symptom reporting. In: Skelton JA, Croyle RE, editors. Mental Representation in Health and Illness. New York: Springer Verlag; 1991. pp. 61–84. [Google Scholar]
- 33.Mountz JM, Bradley LA, Modell JG, et al. Fibromyalgia in women: abnormalities of regional blood flow in the thalamus and caudate nucleus are associated with low pain threshold levels. Arthritis Rheum. 1995;38:926–38. doi: 10.1002/art.1780380708. [DOI] [PubMed] [Google Scholar]
- 34.Clauw DJ, Schmidt M, Radulovic D, Singer A, Katz P, Bresette J. The relationship between fibromyalgia and interstitial cystitis. J Psychiatr Res. 1997;31:125–31. doi: 10.1016/s0022-3956(96)00051-9. [DOI] [PubMed] [Google Scholar]
- 35.Wolfe F, Anderson J, Harkness D, et al. A prospective, longitudinal, multicenter study of service utilization and costs in fibromyalgia. Arthritis Rheum. 1997;40:1560–70. doi: 10.1002/art.1780400904. [DOI] [PubMed] [Google Scholar]
- 36.Bombardier CH, Buchwald D. Disability and health care utilization in chronic fatigue, chronic fatigue syndrome, and fibromyalgia. Med Care. 1996;34:924–30. doi: 10.1097/00005650-199609000-00005. [DOI] [PubMed] [Google Scholar]
- 37.De Leeuw JR, Ros WJ, Steenks MH, Lobbezoo-Scholte AM, Bosman F, Winnubst JA. Craniomandibular dysfunction: patient characteristics related to treatment outcome. J Oral Rehabil. 1994;21:67–78. doi: 10.1111/j.1365-2842.1994.tb01182.x. [DOI] [PubMed] [Google Scholar]
- 38.Krogstad BS, Jokstad A, Dahl BL, Vassend O. Relationships between risk factors and treatment outcome in a group of patients with temporomandibular disorders. J Orofac Pain. 1996;10:48–53. [PubMed] [Google Scholar]
- 39.Lloyd AR, Pender H. The economic impact of chronic fatigue syndrome. Med J Aust. 1992;157:599–601. [PubMed] [Google Scholar]