Abstract
OBJECTIVE
To examine the relation between problem drinking and medication adherence among persons with HIV infection.
DESIGN
Cross-sectional survey.
SETTING/PARTICIPANTS
Two hundred twelve persons with HIV infection who visited 2 outpatient clinics between December 1997 and February 1998.
MEASUREMENTS AND MAIN RESULTS
Nineteen percent of subjects reported problem drinking during the previous month, 14% missed at least 1 dose of medication within the previous 24 hours, and 30% did not take their medications as scheduled during the previous week. Problem drinkers were slightly more likely to report a missed dose (17% vs 12 %, P = .38) and significantly more likely to report taking medicines off schedule (45% vs 26%, P = .02). Among drinking subtypes, taking medications off schedule was significantly associated with both heavy drinking (high quantity/frequency) (adjusted odds ratio [OR], 4.70; 95% confidence interval [95% CI], 1.49 to 14.84; P < .05) and hazardous drinking (adjusted OR, 2.64; 95% CI, 1.07 to 6.53; P < .05). Problem drinkers were more likely to report missing medications because of forgetting (48% vs 35%, P = .10), running out of medications (15% vs 8%, P = .16), and consuming alcohol or drugs (26 % vs 3 %, P < .001).
CONCLUSION
Problem drinking is associated with decreased medication adherence, particularly with taking medications off schedule during the previous week. Clinicians should assess for alcohol problems, link alcohol use severity to potential adherence problems, and monitor outcomes in both alcohol consumption and medication adherence.
Keywords: adherence, alcohol, HIV infection
Highly active antiretroviral therapy has significantly improved the prognosis of persons with HIV infection.1 However, the complex antiviral drug regimen can be difficult to take as scheduled because medications may need to be taken at work, in strict relationship to meals, or may interfere with normal sleeping times. Unfortunately, missing even a few doses or taking medications off schedule may result in the development of viral resistance and may adversely impact survival.2 Therefore, adherence to HIV therapy is a very important concern of both patients and their physicians. Furthermore, the development of drug-resistant HIV may be a public health concern if persons spread resistant viruses into the community.3
Several factors appear to be associated with adherence to HIV medications, including demographic characteristics, medication dosing schedules, psychiatric illness, attitudes about medications, side effects, lack of primary care physician involvement, and illicit drug use.4–11 Little information is available on the relationship of alcohol use to medication adherence, and the data reported to date are contradictory.8–11 Previous studies used different measures of alcohol consumption, which further confuses the ability to make conclusions about alcohol consumption and adherence to HIV therapy.
The relationship of alcohol use to adherence is important because alcohol consumption is common among persons with HIV. One quarter to one half of persons in some HIV clinics consume at least moderate amounts of alcohol and many of these have problem drinking.12,13 Problem drinking is defined as alcohol consumption sufficiently large enough to lead to problems of health and social functioning, but does not necessarily meet Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria for alcohol abuse or dependence.14 Several specific patterns of problem drinking, including hazardous,5 heavy,6 and binge7,8 drinking have been linked to adverse social and health consequences in primary care settings. Yet, it is not clear which, if any, of these drinking patterns interferes with medication adherence among persons with HIV. If specific patterns of drinking are associated with greater risks for nonadherence, clinicians may be able to identify persons with HIV who are most likely to benefit from interventions which improve adherence and/or reduce alcohol consumption.
The objectives of this study were to estimate the prevalence of problem drinking and medication nonadherence among a diverse group of outpatients with HIV infection, to determine whether specific drinking patterns are associated with medication adherence, and to identify reasons for missing medications that are more common among persons with problem drinking.
METHODS
Design
We surveyed consecutive outpatients at two HIV clinics between December 1997 and February 1998. One site was an urban, university-associated clinic in western Pennsylvania that provides outpatient care to approximately 620 persons with HIV. The other was a community-based clinic in a small city with a population of about 100,000 in eastern Pennsylvania providing care to approximately 325 persons with HIV. The study protocol was approved by the University of Pittsburgh Institutional Review Board.
Surveys were administered to a convenience sample of outpatients for 12 weeks at the urban clinic and 6 weeks at the community clinic. All persons with HIV who attended the clinic during the study enrollment period were eligible. Subjects were offered a private area to complete the anonymous survey, which took approximately 10 minutes to complete. Clinic staff attempted to distribute the survey to consecutive persons attending the clinic, but this occasionally did not occur when patients were late for appointments, during busy clinic times, or when the private area to complete the survey was occupied.
Measures
The survey instrument was available in English and Spanish and included items on alcohol use, adherence to therapy, subject demographics, and attitudes and beliefs about taking medication. Clinic staff and persons with HIV infection reviewed early versions of the survey and suggested changes. The final survey included the 10-item Alcohol Use Disorders Identification Test (AUDIT) which has been validated in both English and Spanish and can identify a current alcohol-related problem with a sensitivity of 96% and specificity of 96%.15,19 Two additional items assessed quantity and frequency of alcohol consumption during the previous month. For these items, a drink of alcohol was defined as 1 beer, 1 glass of wine, or 1 shot of liquor. Collectively, these items were used to define 3 patterns of drinking: binge drinking, if persons reported drinking at least 5 drinks (women) or 6 drinks (men) in one sitting at least monthly17; heavy drinking, if persons consumed more than 12 (women) or 16 (men) drinks per week during the previous month16; and hazardous drinking, if persons scored at least 8 of 40 possible points on the AUDIT.19 The broader term problem drinking was used to describe persons who had at least 1 of the 3 drinking types. All remaining subjects were categorized as either persons who consumed no alcohol during the previous month or those with mild-to-moderate alcohol consumption.
We measured medication adherence using self-report. No validated self-adherence measure was in widespread use at the time of survey development; therefore, we used two different measures. Persons were classified as having a missed dose if they reported missing at least one dose of medication in the previous 24 hours, and classified as taking medications off schedule unless they took their medications on time as scheduled during the previous week “all of the time” or “nearly all of the time.” Those taking medications as scheduled “nearly all of the time” received credit for being on schedule because it is unclear whether a very slight alteration in scheduling adversely affects clinical outcomes.
Participants were also asked whether they used specific illicit drugs during the previous 30 days, whether they had ever been in recovery for alcohol or drug abuse, and whether they had received any treatment for depression or anxiety in the previous year. Other survey items assessed demographic characteristics; medication history including number of pills, use of protease inhibitors, and number of times per day that pills are taken; perceived benefits of therapy; and perceived harm from therapy. Finally, participants were asked whether or not they sometimes missed a dose of medication because of 8 potential reasons identified in other studies.6,11,20,21
Data Analysis
Analyses and data management were conducted using SAS for Windows Version 6.12 (SAS Institute, Inc., Cary, NC). Of 232 surveys collected, 13 (5.6 %) were excluded because the subject was not prescribed any medications (n = 9) or because of substantial missing data (n = 4). Each drinking pattern was represented as a single indicator variable, where persons without that pattern were treated as the reference group. Persons for whom the presence or absence of a particular drinking pattern could not be determined were excluded from analyses of that particular drinking pattern, but not from the entire study. Separate analyses were conducted for each of the drinking patterns and each of the adherence measures.
The bivariate relationships of each drinking pattern to medication nonadherence was examined using binary logistic regression analysis, with χ2or Fisher's exact test used to assess statistical significance. Then, the relationship of each demographic factor, behavior, and attitude to medication adherence and each drinking pattern was determined in a similar manner. Multivariate logistic regression was used to determine the relationship of each alcohol drinking pattern with the two adherence measures. For each model, individual factors were included as potential confounding variables if they demonstrated a significant relationship (P < .20) with either the particular drinking variable of interest, the adherence variable of interest, or both. Variables included in at least one of the multivariate models included age, race (African American: yes vs no), crack/cocaine use, poppers use, intravenous drug use, treatment for depression/anxiety, and the belief that it is dangerous to miss medications. Finally, χ2statistics were used to compare the proportion of persons with and without problem drinking who missed medications for various reasons.
RESULTS
Completed surveys were available from 219 persons with HIV infection; clinic staff estimated that over 90% of persons offered the survey actually completed it. Nineteen percent of the subjects were classified as current problem drinkers and 33% as mild-to-moderate drinkers; 48% did not use alcohol in the previous year. Among the problem drinking patterns, binge drinking was most common (17%), followed by hazardous drinking (15%) and heavy drinking (10%).
Characteristics of the study population are shown in Table 1). Overall, 72% were men, most (57%) were between 31 and 40 years old, and 42% were members of racial and ethnic minorities. At both clinic sites, the sampled population was nearly identical to the overall clinic population in terms of gender, age, and the proportion identifying nonwhite ethnicity, although the sampled population had slightly fewer who identified as African American and slightly more who identified as Hispanic, compared with the overall population. The majority (81%) took at least 1 protease inhibitor, with indinavir the most commonly prescribed. Nearly 40% of the sample had received treatment for alcohol or drug abuse in the past. Only two thirds of participants believed it was dangerous to miss a dose of medication, and one fourth believed their medications were not helping them. Compared with nonproblem drinkers, problem drinkers were significantly (P < .05) more likely to be in the younger age ranges, to have consumed alcohol in the previous month, and to report using crack or cocaine in the previous month.
Table 1.
Subject Characteristics
| Problem Drinking* | ||||
|---|---|---|---|---|
| n | Yes (n = 41) | No (n = 171) | Overall (n = 219) | |
| Clinic setting, % | 219 | |||
| University-based | 73 | 70 | 71 | |
| Community-based | 27 | 30 | 29 | |
| Gender, % | 217 | |||
| Men | 83 | 70 | 72 | |
| Women | 17 | 30 | 28 | |
| Age, %† | 217 | |||
| <30 years | 10 | 12 | 11 | |
| 31–40 years | 80 | 52 | 57 | |
| >40 years | 10 | 36 | 32 | |
| Race/ethnicity, % | 214 | |||
| African American | 18 | 26 | 24 | |
| Hispanic | 12 | 16 | 15 | |
| White | 65 | 56 | 58 | |
| Other | 5 | 2 | 3 | |
| Taking protease inhibitor, % | 210 | 82 | 81 | 81 |
| HIV risk, %‡ | 214 | |||
| Gay/bisexual | 58 | 46 | 48 | |
| Heterosexual | 38 | 40 | 40 | |
| Intravenous drug use | 25 | 19 | 21 | |
| Substance use in previous month, %‡ | 217 | |||
| Alcohol† | 100 | 35 | 44 | |
| Amyl nitrate | 20 | 10 | 12 | |
| Cocaine/crack† | 27 | 10 | 13 | |
| Heroin | 5 | 5 | 5 | |
| Marijuana | 32 | 25 | 26 | |
| Methadone | 5 | 8 | 8 | |
| Treatments, % | ||||
| Ever in recovery for alcohol/drugs | 213 | 34 | 40 | 39 |
| Received treatment for depression/anxiety | 211 | 44 | 39 | 40 |
| Attitudes, % | ||||
| Believes dangerous to miss medications | 209 | 62 | 65 | 67 |
| Believes medications are helpful | 210 | 80 | 79 | 81 |
Problem drinking status could not be determined for 7 participants.
P < .01.
Respondents could select more than 1 category.
Fourteen percent of study participants stated that they missed a dose of medication during the previous 24 hours, and 30% indicated that they took their medicines off schedule during the previous week. Compared with persons without problem drinking, those with problem drinking were slightly more likely to report a missed dose of medication (17% vs 12%, P = .375) and much more likely to report taking medications off schedule (46% vs 26%, P = .019). Among problem drinkers, those with hazardous drinking were most likely to miss a dose (21%), followed by those with binge drinking (17%) and heavy drinking (15%). Taking medicines off schedule was most common among those with heavy drinking (59%) and hazardous drinking (53%), and slightly less among persons with binge drinking (38%). There was no significant difference in medication adherence between those persons with mild-to-moderate drinking and those without any current drinking.
In multivariate analyses, taking medications off schedule was significantly associated with both heavy drinking (adjusted odds ratio [OR], 4.70; 95% confidence interval [95% CI], 1.49 to 14.84; P < .05) and hazardous drinking (adjusted OR, 2.64; 95% CI, 1.07 to 6.53; P < .05), but not with binge drinking (Table 2). Persons with each type of problem drinking were also more likely to report a missed dose of medication, although these results did not achieve statistical significance (Table 2).
Table 2.
Relationship of Problem Drinking to Medication Adherence: Multivariate Analysis*
| Took Medications Off Schedule During Previous Week | Missed Dose During Previous 24 Hours | |
|---|---|---|
| Drinking Type | Adjusted Odds Ratio (95% Confidence Interval) | Adjusted Odds Ratio (95% Confidence Interval) |
| Binge drinking | 1.43 (0.61 to 3.34) | 1.83 (0.52 to 6.38) |
| Hazardous drinking | 2.64 (1.07 to 6.53)† | 3.34 (0.88 to 12.75) |
| Heavy drinking | 4.70 (1.49 to 14.84)† | 1.94 (0.32 to 11.67) |
| Problem drinking (any of above 3 types) | 1.91 (0.85 to 4.22) | 1.71 (0.53 to 5.54) |
Variables were included in multivariate analyses if they demonstrated a relationship with the drinking variable of interest, the adherence variable of interest, or both.
P < .05.
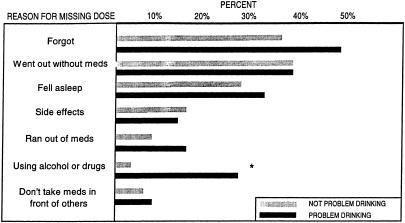
The proportion of participants who reported missing medications for various reasons are shown in Figure 1. Persons with problem drinking, compared with those without problem drinking, were significantly more likely to miss a dose because they were drinking and/or using drugs (26 % vs 3 %, P < .001), and also more likely to report missing a dose because they forgot (48% vs 35%, P = .10) or because they ran out of medicine (15% vs 8%, P = .16).
FIGURE 1.
Proportion of persons with or without problem drinking who indicated they sometimes miss a dose of medicine for each specific reason. *P < .01.
DISCUSSION
This study examined the relationship of problem drinking to medication adherence among a diverse group of persons with HIV infection. To our knowledge, it is the first study to compare the effect of several types of problem drinking on medication adherence within the same population. The results suggest that: (1) problem drinking is associated with decreased medication adherence, particularly with taking medications off schedule during the previous week; (2) heavy drinking (high quantity/frequency) and hazardous drinking (high score on AUDIT) were the drinking patterns most strongly associated with adherence problems; and (3) persons with problem drinking may be more likely to miss a dose of medicine because of actively consuming alcohol or drugs, forgetting, or running out of medication.
Problem drinking is a significant issue among persons with HIV infection, affecting at least 1 of 5 persons in our clinics. Measurement of problem drinking varies from study to study, which makes it difficult to directly compare prevalence across different populations. An even higher prevalence of alcohol problems has been reported in some other HIV-related settings, perhaps because other studies classified persons as problem drinkers with lower levels of alcohol consumption or with past drinking problems.12,13 For the present study, we assessed only current drinking and chose specific measures of problem drinking that have been associated with adverse outcomes in clinical settings.15–18
Problem drinking was one of very few potentially modifiable factors found to be a significant predictor of medication adherence in this diverse population. The specific link between alcohol and adherence is not known, and several explanations are possible. Alcohol may have a causal relationship with adherence if individuals miss their medications because they are intoxicated or because they attend social functions such as parties or bars. Alternatively, the two behaviors could be related through a common underlying factor such as individual personality, attitudes, or depression.22 Persons may believe that it is dangerous to take medications while drinking, although we are aware of no evidence that alcohol has significant interactions with HIV therapies.23 The true nature of the relationship remains unclear, and additional research is needed to further identify the specific reasons that problem drinking impacts upon medication adherence.
Clinicians have several options to assist patients with medication adherence, such as limiting the number of pill doses per day, using special packaging, providing reminders or timers, and tailoring advice for specific individuals.24,25 It is not clear whether any of these strategies is especially effective among problem drinkers. In primary care settings, interventions that identify persons with problem drinking and provide brief motivational counseling have led to reduced alcohol consumption, lower levels of health care utilization, and reduced health care costs over time.17,26 It is possible that similar interventions targeting alcohol consumption could positively impact on medication adherence among persons with HIV infection, but this has not been investigated to date.
Several study limitations warrant mention. The study population was a convenience sample, and it is possible that persons who were not approached differed from the sampled population. However, over 90% of persons who were approached completed the survey, and the sample population was similar to the overall clinic population in terms of gender, age, and ethnicity. We measured adherence by participant self-report, which has both limitations and strengths. With self-report, persons tend to overreport their medication adherence,27,28 and it is possible that persons who admit to problem drinking would be more willing to admit to nonadherence. In order to mitigate the tendency to overreport adherence, we used an anonymous survey with nonjudgmental questions. While this precluded the ability to link adherence data to objective biologic outcomes, self-reported data have been shown to correlate with biologic outcomes in other settings.6,20,28 Unfortunately, there is no gold standard for measuring adherence, and no method of adherence measurement is without problems.24,29 Even electronic monitoring systems have limitations, as persons may place their medications in alternative containers,30 use the monitoring devices improperly,27 or change their behavior if they know they are being monitored.30,31
In conclusion, the results of this study emphasize the importance of screening for alcohol problems in outpatient settings serving persons with HIV infection. It is important to note that the majority of persons with problem drinking in our study did not report difficulty with medication adherence, because some physicians may withhold important medications from substance-using patients if they believe that they are unable to adhere to the complex medical regimens.32 Rather than using the patient's substance use history to simply predict nonadherent behavior, clinicians might work with individual patients to devise individual strategies to deal with adherence.33 When alcohol problems are identified, clinicians should address them directly, link alcohol use severity to potential for adherence problems and clinical outcomes, and increase expectations that alcohol intervention will result in increased medication efficacy.34 Specific drinking situations that could result in nonadherence could be discussed. For example, our data suggest that persons with problem drinking may be more likely to miss medications when they are actively drinking or using drugs, and that they may be more likely to forget to take their medications or run out of pills early. Finally, clinicians should monitor outcomes in both alcohol consumption and HIV medication adherence in order to most effectively assist their patients in achieving their optimal long-term health.
Acknowledgments
The authors thank Dr. Jaqueline Dunbar-Jacob, Dr. Christopher Ryan, and Christine Morrison for advice on survey development. They also thank John Michael Harding, Juanita Goodwin, and the staff at the two participating clinics who helped to distribute the surveys. Dr. Cook is recipient of a Mentored Patient-Oriented Research Career Development Award from NIAAA. Dr. Conigliaro is the recipient of an Advanced Career Development Award from the Department of Veterans Affairs and is a Generalist Physician Faculty Scholar of the Robert Wood Johnson Foundation.
REFERENCES
- 1.Report of the NIH Panel To Define Principles of Therapy of HIV Infection. Ann Intern Med. 1998;128:1057–78. doi: 10.7326/0003-4819-128-12_part_2-199806151-00002. [DOI] [PubMed] [Google Scholar]
- 2.Vanhove GF, Schapiro JM, Winters MA, Merigan TC, Blaschke TF. Patient compliance and drug failure in protease inhibitor monotherapy. JAMA. 1996;276:1955–6. [PubMed] [Google Scholar]
- 3.Wainberg MA, Friedland G. Public health implications of antiretroviral therapy and HIV drug resistance. JAMA. 1998;279:1977–83. doi: 10.1001/jama.279.24.1977. [DOI] [PubMed] [Google Scholar]
- 4.Mehta S, Moore RD, Graham NM. Potential factors affecting adherence with HIV therapy. AIDS. 1997;11:1665–70. doi: 10.1097/00002030-199714000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Singh N, Squier C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8:261–9. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- 6.Samet JH, Libman H, Steger KA, et al. Compliance with zidovudine therapy in patients infected with human immunodeficiency virus, type 1: a cross-sectional study in a municipal hospital clinic. Am J Med. 1992;92:495–502. doi: 10.1016/0002-9343(92)90746-x. [DOI] [PubMed] [Google Scholar]
- 7.Smith MY, Rapkin BD, Morrison A, Kammerman S. Zidovudine adherence in persons with AIDS. The relation of patient beliefs about medications to self-termination of therapy. J Gen Intern Med. 1997;12:216–23. doi: 10.1046/j.1525-1497.1997.012004216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haubrich R, Little S, Dube M, et al. Self-reported treatment adherence and drug/alcohol use are associated with virologic outcomes in CCTG 570: a clinical strategy trial of HIV RNA antiretroviral (ARV) monitoring. Int Conf AIDS. 1998;12:597. Abstract. [Google Scholar]
- 9.Halkitis P, Remien R, Parsons JT, Stirratt MJ. Factors related to protease inhibitor (PI) adherence among sexually active men-who-have-sex-with-men. Int Conf AIDS. 1998;12:1034. Abstract. [Google Scholar]
- 10.Stone VE, Adelson-Mitty J, Duefield CA, Steger KA, Stein MD, Mayer KH. Adherence to protease inhibitor (PI) therapy in clinical practice: usefulness of demographics, attitudes and knowledge as predictors. Int Conf AIDS. 1998;12:588. Abstract. [Google Scholar]
- 11.Weidle PJ, Ganea CE, Ernst J, McGowan J, Irwin KL, Holberg SD. Multiple reasons for nonadherence to antiretroviral medications in an inner-city minority population: need for a multifaceted approach to improve adherence. Int Conf AIDS. 1998;12:593. Abstract. [Google Scholar]
- 12.Lefevre F, O'Leary B, Moran M, et al. Alcohol consumption among HIV-infected patients. J Gen Intern Med. 1995;10:458–60. doi: 10.1007/BF02599920. [DOI] [PubMed] [Google Scholar]
- 13.Page-Shafer K, Delorenze GN, Satariano WA, Winkelstein W., Jr Comorbidity and survival in HIV-infected men in the San Francisco Men's Health Survey. Ann Epidemiol. 1996;6:420–30. doi: 10.1016/s1047-2797(96)00064-6. [DOI] [PubMed] [Google Scholar]
- 14.Rinaldi RC, Steindler EM, Wilford BB, Goodwin D. Clarification and standardization of substance abuse terminology. JAMA. 1988;259:555–7. [PubMed] [Google Scholar]
- 15.Isaacson JH, Butler R, Zacharek M, Tzelepis A. Screening with the Alcohol use Disorders Identification Test (AUDIT) in an inner-city population. J Gen Intern Med. 1994;9:550–3. doi: 10.1007/BF02599279. [DOI] [PubMed] [Google Scholar]
- 16.Sanchez-Craig M, Wilkinson DA, Davila R. Empirically based guidelines for moderate drinking: 1-year results from three studies with problem drinkers. Am J Public Health. 1995;8:823–8. doi: 10.2105/ajph.85.6.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fleming MF, Barry KL, Manwell LB, Johnson K, London R. Brief physician advice for problem alcohol drinkers. A randomized controlled trial in community-based primary care practices. JAMA. 1997;277:1039–45. [PubMed] [Google Scholar]
- 18.Wechsler H, Davenport A, Dowdall G, Moeykens B, Castillo S. Health and behavioral consequences of binge drinking in college. A national survey of students at 140 campuses. JAMA. 1994;272:1672–7. [PubMed] [Google Scholar]
- 19.Babor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 20.Hecht FM, Colfax G, Swanson M, Chesney MA. Adherence and effectiveness of protease inhibitors in clinical practice. Fifth Annual Conference of Retroviral and Opportunistic Infections. 1998;107:1–5. [Google Scholar]
- 21.Condor B. The psychology of compliance. Posit Aware. 1997;8:18–20. [PubMed] [Google Scholar]
- 22.Ferrando SJ, Wall TL, Batki SL, Sonensen JL. Psychiatric morbidity, illicit drug use and adherence to zidovudine (AZT) among injection drug users with HIV disease. Am J Drug Alcohol Abuse. 1996;22:475–87. doi: 10.3109/00952999609001674. [DOI] [PubMed] [Google Scholar]
- 23.Friedland G. HIV disease in substance abusers: treatment issues. In: Sande MA, Volberding PA, editors. The Medical Management of AIDS. 6th ed. Philadelphia: WB Saunders; 1999. pp. 575–91. [Google Scholar]
- 24.Haynes RB, McKibbon KA, Kanani R. Systematic review of randomised trials of interventions to assist patients to follow prescriptions for medications. Lancet. 1996;348:383–6. doi: 10.1016/s0140-6736(96)01073-2. [DOI] [PubMed] [Google Scholar]
- 25.Melnikow J, Kiefe C. Patient compliance and medical research: issues in methodology. J Gen Intern Med. 1994;9:96–105. doi: 10.1007/BF02600211. [DOI] [PubMed] [Google Scholar]
- 26.Conigliaro J, Lofgren RP, Hanusa BH. Screening for problem drinking: impact on physician behavior and patient drinking habits. J Gen Intern Med. 1998;13:251–6. doi: 10.1046/j.1525-1497.1998.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Melbourne KM, Geletko SM, Brown SL, Willey-Lessne C, Chase S, Fisher A. Medication adherence in patients with HIV infection: a comparison of two measurement methods. AIDS Reader. 1999;9:329–38. [PubMed] [Google Scholar]
- 28.Amsten JH, Grant RW, Domas PA, et al. Adherence with antiretroviral therapy in HIV-infected drug users: how does self-report compare with electronic monitors? J Gen Intern Med. 2000;15(suppl 1):51–2. [Google Scholar]
- 29.Hecht FM. Measuring HIV treatment adherence in clinical practice. AIDS Clin Care. 1998;10:57–9. [PubMed] [Google Scholar]
- 30.Miller LG, Hays RD. Adherence to combination antiretroviral therapy: synthesis of the literature and clinical implications. AIDS Reader. 2000;10:177–85. [PubMed] [Google Scholar]
- 31.Potter L, Oakley D, de Leon-Wong E, Canamar R. Measuring compliance among oral contraceptive users. Fam Plann Perspect. 1996;28:154–8. [PubMed] [Google Scholar]
- 32.Sontag D, Richardson L. Doctors withhold H.I.V. pill regimen from some. New York Times; 1997. March 2, 1,35. [PubMed] [Google Scholar]
- 33.Lerner BH, Gulick RM, Dubler NN. Rethinking nonadherence: historical perspectives on triple-drug therapy for HIV disease. Ann Intern Med. 1998;129:573–8. doi: 10.7326/0003-4819-129-7-199810010-00012. [DOI] [PubMed] [Google Scholar]
- 34.Bryant KJ, Levine GL. Drinking and HIV: Knowledge and context. Focus. 1999;14:1–8. [PubMed] [Google Scholar]