Abstract
BACKGROUND
Lower extremity mobility difficulties often result from common medical conditions and can disrupt both physical and emotional well-being.
OBJECTIVES
To assess the national prevalence of mobility difficulties among noninstitutionalized adults and to examine associations with demographic characteristics and other physical and mental health problems.
DESIGN
Cross-sectional survey using the 1994–1995 National Health Interview Survey-Disability Supplement (NHIS-D). We constructed measures of minor, moderate, and major lower extremity mobility difficulties using questions about ability to walk, climb stairs, and stand, and use of mobility aids (e.g., canes, wheelchairs). Age and gender adjustment used direct standardization methods in Software for the Statistical Analysis of Correlated Data (SUDAAN).
PARTICIPANTS
Noninstitutionalized, civilian U.S. residents aged 18 years and older. National Health Interview Survey sampling weights with SUDAAN provided nationally representative population estimates.
RESULTS
An estimated 19 million people (10.1%) reported some mobility difficulty. The mean age of those with minor, moderate, or major difficulty ranged from 59 to 67 years. Of those reporting major difficulties, 32% said their problems began at aged 50 years or younger. Adjusted problem rates were higher among women (11.8%) than men (8.8%), and higher among African American (15.0%) than whites (10.0%). Persons with mobility difficulties were more likely to be poorly educated, living alone, impoverished, obese, and having problems conducting daily activities. Among persons with major mobility difficulties, 30.6% reported being frequently depressed or anxious, compared to 3.8% for persons without mobility difficulties.
CONCLUSIONS
Reports of mobility difficulties are common, including among middle-aged adults. Associations with poor performance of daily activities, depression, anxiety, and poverty highlight the need for comprehensive care for persons with mobility problems.
For most people, walking barely requires conscious thought. For others, difficulty walking compromises not only physical safety but also emotional well-being. Moving physically around the home and community is central to daily life—going to work or school, doing errands, visiting family and friends. Without assistance or mobility aids, difficulty walking can lead to increasing isolation, anxiety, and depression. Often people seek care from primary care physicians for their underlying medical conditions, but physicians frequently fail to fully recognize patients' functional problems.11–6
Although these observations are well recognized among elderly persons, little is known about the national population prevalence of difficulties with lower extremity mobility among all adults. Other studies of mobility problem rates have targeted older people7–11 or special populations.11–14 Motivated by the 1990 passage of the Americans with Disabilities Act, the 1994–1995 National Health Interview Survey (NHIS) added a disability supplement (NHIS-D) to generate estimates of national rates of disabling conditions for people of all ages living outside institutions. Using the NHIS-D, we examined the national prevalence and various characteristics of adults reporting difficulty with lower extremity mobility.
METHODS
Database
We used responses from 145,007 persons aged 18 years and older from the 1994–1995 NHIS-D conducted by the National Center for Health Statistics (NCHS). The NHIS involves face-to-face household interviews of a nationally representative sample of civilian, noninstitutionalized U.S. residents. The disability supplement added queries about functional limitations, behavioral health, performance of daily activities, use of assistive devices, and health conditions.15,16 Interviewers obtained proxy responses for adults who were not home or were unable to answer for themselves.
Measuring Mobility
Our aim was to identify people who would have difficulty moving within their communities without personal or mechanical assistance because of problems involving lower extremity mobility. Moving unassisted throughout communities to conduct daily activities requires such physical capabilities as walking, climbing stairs, and standing. For example, persons must navigate shops then wait at cashier counters; entering many buildings, especially private homes, requires climbing stairs. Musculoskeletal factors, cardiorespiratory fitness, balance, vision and other senses, and neurological and cognitive abilities all affect these capacities.17,18 Instruments exist for clinical assessments of gait and mobility primarily for older people18–23; the NHIS-D does not contain the information required by these instruments.
The NHIS-D has 8 questions about physical actions involving the upper and lower body, including reaching, bending, and lifting heavy objects. We used the 3 questions pertinent to moving unassisted around communities: (1) whether the person has “any difficulty walking a quarter of a mile—about 3 city blocks”; (2) whether the person has “any difficulty walking up 10 steps without resting”; and (3) whether the person has “any difficulty standing for about 20 minutes.”
Persons reporting difficulty on each question were asked about its level: “some,” “a lot,” or “completely unable.” The NHIS-D asked only persons reporting being “completely unable” whether this limitation would persist at least 12 months (87.6% said it would).
We considered whether the 3 actions (walking, stair climbing, standing) deserved equal weighting in our mobility measure. Reports of any difficulty were highly, but not perfectly, correlated between pairs of questions: Pearson correlation coefficients were 0.70 for walking and stair climbing, 0.63 for walking and standing, and 0.61 for stair climbing and standing (P = .0001). On a separate activities of daily living (ADL) question, only 1.2% of respondents reported “any difficulty getting around inside of the home.” We therefore viewed this ADL as representing the most impaired end of the mobility continuum. Pearson correlation coefficients for reporting this ADL difficulty and the 3 mobility questions were similar: .35 for walking, 0.38 for stairs, and 0.37 for standing (all P = .0001). Since the variance in the “level of difficulty” ascribed to each of the 3 actions was roughly comparable (walking, 0.28; stair climbing, 0.18; and standing, 0.18), we weighted each question equally. This approach gave walking (with its somewhat higher variance) more influence than stair climbing and standing, which seemed clinically appropriate.
The 3 mobility questions did not ask about use of assistive devices. Because these questions appeared elsewhere, it was unclear whether people considered reliance on devices when reporting mobility limitations; 3.9% reported “no difficulty” with walking, stairs, or standing but said they used mobility aids. Other researchers have classified persons reporting no difficulty walking but who used mobility aids as having difficulty walking.7 We therefore included long-term (i.e., anticipated at more than 12 months) use of mobility aids in our mobility measure. Again, no existing measure fit our data source. Clinically, mobility aids are generally considered hierarchically and used sequentially as problems with weight-bearing, balance, or endurance increase, starting with “low tech” canes and progressing to electric scooters and powered wheelchairs.24–29 Given the potential stigmatization and inconvenience of mobility aids in our society,30–32 we conjectured that most people would use them only if truly needed.
Table 1 shows our 4-level mobility measure. We assigned respondents to the highest level for which they qualified, eliminating 2,435 (1.7%) persons without responses to the 3 mobility, level of difficulty, and assistive device questions.
Table 1.
Estimated Number* (%) of Adults Reporting Mobility Difficulties by Age
| Age group, y | ||||
|---|---|---|---|---|
| Definition of mobility levels† | All | 18–49 | 50–69 | ≥70 |
| None: persons reporting no difficulty with walking and climbing stairs and standing and not using any mobility aid | 168.32 (89.9) | 118.84 (96.0) | 36.29 (84.6) | 13.18 (63.8) |
| Minor: persons reporting some difficulty with walking or climbing stairs or standing or uses a cane or crutches | 7.93 (4.2) | 2.45 (2.0) | 2.72 (6.4) | 2.76 (13.4) |
| Moderate: persons reporting a lot of difficulty with walking or climbing stairs or standing or uses a walker | 5.23 (2.8) | 1.48 (1.2) | 1.91 (4.4) | 1.84 (8.9) |
| Major: persons reporting being unable to perform walking or climbing stairs or standing or uses a manual or powered wheelchair or scooter | 5.82 (3.1) | 0.98 (0.8) | 1.96 (4.6) | 2.88 (13.9) |
| Total | 18.98 (10.1) | 4.91 (4.0) | 6.59 (15.4) | 7.48 (36.2) |
Estimated number of persons in millions. Reweighted population estimates for noninstitutionalized, civilian U.S. residents.
Of the persons with minor difficulties, 10.1% were assigned only because of using a cane or crutches; of the persons with moderate difficulties, 3.4% were assigned only because of using a walker; and of the persons with major difficulties, 4.3% were assigned only because of using a manual or powered wheelchair or scooter.
Demographic and Clinical Characteristics
Basic demographic characteristics (age, gender, self-reported race and ethnicity, education, employment status, living arrangements) came from the NHIS core questionnaire. Determining the cause was complicated. Persons indicating any difficulty across the 8 physical action questions, including our 3 mobility questions, were asked an open-ended question about the “main problem or condition” causing the difficulty. To minimize respondent burden, persons were not asked separately about causes for specific difficulties or about multiple causes. We assumed that difficulty with walking, stairs, and standing would dominate reporting decisions if respondents had multiple problems. Because of the survey's design, we cannot test this assumption or identify multiple, coexisting causes. In addition, for persons not reporting any difficulties, including the 3.9% who said they used mobility aids but had no difficulties, we cannot determine whether they had similar conditions (e.g., arthritis, diabetes). The NHIS-D did not confirm the validity of respondents' self-reported conditions.
The NCHS survey staff assigned diagnosis codes similar to International Classification of Diseases, Ninth Revision, Clinical Modification codes to the self-reported conditions. Then they grouped these codes into condition categories. We aggregated clinically related categories to examine frequencies of conditions.
To characterize further physical and mental health attributes of people with mobility difficulties, we examined other selected responses. The NHIS-D asked specifically about visual impairments, dizziness, balance, and the need for support or to “touch walls” while walking. Using self-reported height and weight, we calculated body mass index, using at least 30 kg/m2 to indicate obesity. Additional questions targeted mental health concerns.
The NHIS-D asked about 6 instrumental ADLs (IADLs): preparing meals, shopping, light and heavy housework, using the telephone, and managing money. We examined the first 4. Although the NHIS-D asked reasons for not performing IADLs, the frequencies of specific reasons were too low for individual analyses. We dichotomized responses (either performed the IADL or did not).
Analyses
All results presented here considered 1994 and 1995 NHIS sampling weights and therefore provide nationally representative population estimates. Analyses used SAS-callable SUDAAN software (Version 7.5, Research Triangle Institute, Research Triangle Park, NC). We first produced population estimates for mobility difficulties. We then examined associations of our mobility categories with respondent characteristics, specified clinical attributes, and IADLs. For examining rates by various demographic and clinical characteristics, we used direct standardization to adjust for either age alone or age and gender. Age adjustment employed 5-year categories between aged 25 and 85 years, and additional categories for 18 to 24 years and 85 more or years. Because of the large sample size, even small differences were highly statistically significant (P ≤ .0001). Adjusted rates used only known responses about presence of relevant characteristics in the numerators, with the entire sample (including those with unknown responses) as the denominators. We used multivariable, logistic regression to predict IADL performance adjusting for age, gender, race, ethnicity, income category, education, living alone, depression, being confused or anxious, and our mobility categories.
RESULTS
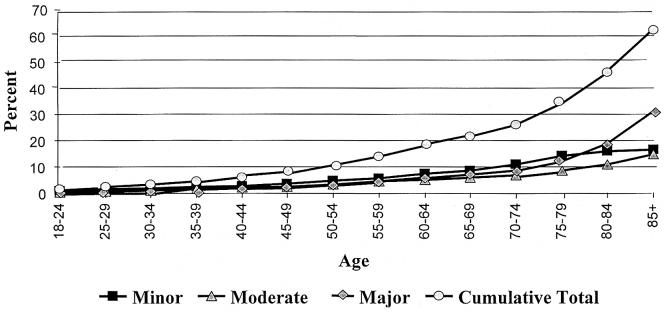
About 10.1% of noninstitutionalized U.S. residents, representing an estimated 19 million people, reported at least some mobility difficulty, with 3.1% (estimated 5.82 million) noting major problems (Table 1). Mobility difficulties increased with increasing age (Fig. 1), although 4.0% and 15.4% of persons aged 18 to 49 and 50 to 69 years, respectively, reported at least some difficulty (Table 1). The mean age for persons reporting minor, moderate, or major mobility difficulties ranged from 59 to 67 years (Table 2). Of those reporting minor and moderate difficulties, about 46% said their problems began at aged 50 years or younger, as did 31.7% of those reporting major difficulties.
FIGURE 1.
Percent of population reporting mobility problems by age category determined from reweighted population estimates for noninstitutionalized, civilian U.S. residents.
Table 2.
Characteristics of Population by Level of Mobility Difficulty
| Level of Mobility Difficulty | ||||
|---|---|---|---|---|
| Characteristic | None | Minor | Moderate | Major |
| Mean age y, (SD) | 42.1 (19.3) | 59.4 (11.8) | 60.5 (12.3) | 66.6 (9.7) |
| Median age, y | 38.9 | 61.6 | 62.0 | 68.8 |
| Age at onset*, % | ||||
| ≤60 y | — | 63.0 | 63.9 | 48.9 |
| ≤50 y | — | 46.4 | 46.3 | 31.7 |
| ≤40 y | — | 31.8 | 29.4 | 18.7 |
| ≤30 y | — | 17.9 | 15.6 | 10.2 |
| Women with given extent of problem†, % | 88.2 | 4.9 | 3.3 | 3.6 |
| Men with given extent of problem†, % | 91.2 | 3.8 | 2.3 | 2.7 |
| Whites with given extent of problem‡, % | 90.0 | 4.2 | 2.7 | 3.1 |
| Blacks with given extent of problem‡, % | 85.0 | 6.1 | 4.4 | 4.5 |
| Hispanics with given extent of problem,‡, % | 89.1 | 4.3 | 3.2 | 3.4 |
| With high school education or less‡, % | 17.2 | 29.6 | 36.5 | 34.1 |
| Living alone‡, % | 13.8 | 19.4 | 19.0 | 17.0 |
| With household income below poverty level‡, % | 8.7 | 21.2 | 26.0 | 26.5 |
| Unable to work due to health problems (persons <65 years of age)‡, % | 3.0 | 31.6 | 56.2 | 70.5 |
| Currently employed or attending school (persons <65 years of age)‡, % | 78.3 | 52.9 | 38.0 | 27.5 |
| Uses cane, crutches, or walker§, % | NA | 20.0 | 26.5 | 48.0 |
| Uses manual or powered wheelchair or scooter§, % | NA | NA | NA | 26.0 |
Asked only of respondents reporting mobility difficulties; users of mobility aids were not asked when they started using it. Percentages are cumulative not mutually exclusive. NA indicates not appplicable.
Adjusted for age category: 18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, and 85+.
Adjusted for age category and gender.
Of the persons with minor difficulties, 10.1% were assigned only because of using a cane or crutches; of the persons with moderate difficulties, 3.4% were assigned only because of using a walker; and of the persons with major difficulties, 4.3% were assigned only because of using a manual or powered wheelchair or scooter.
After age adjustment, 3.0% more women reported mobility difficulties than men (Table 2). After age and gender adjustment, about 10% of whites and persons of Hispanic origin reported difficulties, compared to 15.0% of African Americans. Adjusting for age and gender, persons reporting mobility difficulties were much more likely than others to have a high school education or less, to live alone, and to be poor and unemployed. About one quarter of persons with mobility difficulties had household incomes below the poverty level, compared to 8.7% of others.
Table 3 shows self-reported causes occurring in at least 1% of all adults, arrayed in descending order of frequency; 13.7% of respondents gave no cause when asked. By far the most common causes were arthritis and back problems, with patterns varying by age: arthritis was cited most by persons who were at least 70 years old, while back problems were reported most among those aged 18 to 49 years. Other common causes fell broadly into chronic conditions associated with aging and accidental injuries. As expected, chronic conditions were more important among older persons. Generally, accidental causes, including motor vehicle traffic accidents and injuries caused by overexertion and strain, were most important in the youngest age group. Three causes (not included in Table 3) reached the 1% cutoff but only in one age group: among persons aged 18 to 49 years, multiple sclerosis caused 1.5% and cerebral palsy and partial paralysis caused 1.1% of difficulties; and 1.0% of persons at least 70 years of age listed “poor circulation.”
Table 3.
Causes Reported (%) for at Least 1% of All Persons by Extent of Mobility Difficulties and Age Range* (in Years)
| Extent of Mobility Difficulties and Age Range (Estimated N in Millions) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Minor | Moderate | Major | |||||||
| Causes | 18–49 (2.45) | 50–69 (2.72) | ≥70 (2.76) | 18–49 (1.48) | 50–69 (1.91) | ≥70 (1.84) | 18–49 (0.98) | 50–69 (1.96) | ≥70 (2.88) |
| Arthritis and musculoskeletal problems | 18.1 | 26.0 | 30.1 | 18.6 | 26.4 | 32.5 | 15.0 | 21.7 | 29.6 |
| Intervertebral disk and other back problems and sciatica | 23.2 | 14.3 | 5.3 | 27.6 | 17.4 | 4.9 | 16.6 | 10.4 | 3.1 |
| Accidental falls | 6.7 | 5.4 | 5.3 | 8.3 | 7.3 | 5.2 | 7.3 | 5.7 | 6.2 |
| Ischemic heart disease and other heart conditions | 1.5 | 6.2 | 6.1 | 1.5 | 7.3 | 6.6 | 2.4 | 5.4 | 7.0 |
| Motor vehicle traffic accidents | 8.9 | 3.6 | 1.3 | 11.7 | 4.2 | 1.5 | 11.0 | 5.0 | 1.1 |
| Chronic bronchitis, emphysema, asthma, and other lung conditions | 3.6 | 4.7 | 3.2 | 3.5 | 4.2 | 4.2 | 2.1 | 5.4 | 4.1 |
| Cerebrovascular disease | 0.6 | 1.2 | 1.6 | 0.4 | 1.9 | 3.0 | 2.0 | 4.7 | 6.9 |
| Overexertion and strenuous movements | 4.8 | 2.1 | 0.6 | 6.0 | 3.5 | 0.4 | 4.2 | 1.5 | 0.4 |
| Unspecified accidents | 2.8 | 2.3 | 0.9 | 3.5 | 2.3 | 1.1 | 2.7 | 1.3 | 0.5 |
| Machinery, firearm, and other specified accidents | 2.7 | 1.4 | 0.3 | 3.2 | 1.6 | 0.6 | 4.2 | 1.7 | 0.6 |
| Osteoporosis and bone or cartilage disorders | 0.5 | 1.1 | 1.4 | 0.6 | 1.6 | 1.6 | 0.3 | 1.6 | 2.5 |
| Diabetes | 1.3 | 1.5 | 0.9 | 0.9 | 1.4 | 1.4 | 0.8 | 2.1 | 1.2 |
Age range in years. Percentages reweighted to population estimates for noninstitutionalized, civilian U.S. residents. Conditions listed in descending order of frequency across all persons.
After age and gender adjustment, people reporting mobility difficulties were much more likely than others to report serious vision difficulties, dizziness, balance problems, and needing to touch walls (Table 4). Among persons with major mobility difficulties, rates of problems relating to balance and dizziness were similar across age groups (Table 4). Those reporting mobility difficulties were more likely to be obese: roughly 30% for persons with mobility difficulties, compared to 15.2% for other people. Adjusting for age and gender, more persons with mobility difficulties, especially younger people, reported mental health concerns than did others. Among persons reporting major mobility difficulties, 30.6% noted being frequently depressed or anxious, compared to 3.8% of people without mobility difficulties. Mobility was strongly associated with overall health status; 38.4% of persons reporting major mobility difficulties perceived themselves in poor health, compared to 1.2% of those without any mobility difficulties.
Table 4.
Other Findings Reported by Level of Mobility Difficulty and by Age for Persons Reporting Major Mobility Difficulties
| All Persons*, % | Persons with Major Difficulties Only†, % | ||||||
|---|---|---|---|---|---|---|---|
| Findings Reported | None | Minor | Moderate | Major | 18–49 y | 50–69 y | ≥70 y |
| Serious difficulty seeing, even when using glasses or contact lenses | 2.0 | 8.3 | 11.5 | 15.1 | 12.3 | 19.0 | 23.5 |
| Problem with dizziness lasting for at least three months | 1.0 | 6.8 | 12.7 | 13.4 | 13.1 | 14.2 | 13.4 |
| Problem with balance lasting for at least three months | 1.0 | 9.6 | 16.2 | 26.3 | 26.9 | 25.2 | 25.6 |
| Needs support or touches walls when walking due to balance problems | 0.3 | 5.2 | 10.3 | 19.7 | 20.3 | 18.1 | 19.4 |
| Obese (body mass index ≥30) | 15.2 | 30.9 | 32.7 | 29.4 | 28.4 | 35.2 | 23.5 |
| Underweight (body mass index <18.5) | 5.1 | 6.0 | 5.2 | 11.5 | 12.9 | 7.9 | 10.6 |
| Frequently depressed or anxious | 3.8 | 20.1 | 29.5 | 30.6 | 34.8 | 31.8 | 22.5 |
| Frequently confused, disoriented, or forgetful | 1.4 | 10.0 | 17.3 | 19.9 | 20.5 | 18.2 | 20.0 |
| Unreasonably strong fear where most people would not be afraid | 2.7 | 12.4 | 16.0 | 17.8 | 22.5 | 10.7 | 6.2 |
| Self-perceived health status | |||||||
| Excellent | 34.3 | 9.1 | 4.0 | 6.8 | 9.1 | 2.3 | 3.1 |
| Very good | 31.4 | 16.2 | 9.8 | 8.0 | 9.2 | 5.2 | 6.9 |
| Good | 25.8 | 32.1 | 26.1 | 20.5 | 23.2 | 13.7 | 18.7 |
| Fair | 6.8 | 29.0 | 31.2 | 25.3 | 24.0 | 26.1 | 30.4 |
| Poor | 1.2 | 12.7 | 28.5 | 38.4 | 33.5 | 51.4 | 39.9 |
Adjusted for age category (18–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84, and 85+) and gender.
Adjusted for relevant age groupings within age category and gender.
As expected, the fraction of people reporting IADL limitations rose with increasing mobility difficulties (Table 5). After adjusting for demographic characteristics and mental health factors, mobility difficulties remained overwhelmingly associated with reported IADL limitations (Table 5). Mobility was the strongest predictor of IADL problems, with age a distant second. The percent of variation (R2 × 100) in shopping performance explained by respondents' characteristics was 10.3%, with mobility contributing 4.2% and age contributing .3%. Similarly, respondent characteristics explained 19.4% of variation in performance of heavy housework, with mobility contributing 8.6% while age contributed .5%.
Table 5.
Daily Activities by Extent of Mobility Difficulties
| Extent of Mobility Difficulties | ||||
|---|---|---|---|---|
| Instrumental Activities of Daily Living | None | Minor | Moderate | Major |
| % with problems performing activity* | ||||
| Meals† | 0.3 | 3.2 | 9.6 | 33.0 |
| Shopping‡ | 0.6 | 5.4 | 14.8 | 42.4 |
| Heavy housework§ | 2.4 | 27.5 | 52.4 | 73.5 |
| Light housework∥ | 0.3 | 5.4 | 16.1 | 42.9 |
| Adjusted odds ratio (95% confidence interval) of reporting problems performing activity¶ | ||||
| Meals | 1.0 | 7.5 (6.0 to 9.5)# | 18.8 (15.0 to 23.5)# | 92.4 (76.0 to 112.4)# |
| Shopping | 1.0 | 7.2 (6.0 to 8.6)# | 20.0 (17.0 to 23.8)# | 83.6 (71.9 to 97.1)# |
| Heavy housework | 1.0 | 10.8 (9.9 to 11.9)# | 30.0 (27.5 to 32.9)# | 65.6 (59.2 to 72.6)# |
| Light housework | 1.0 | 15.3 (12.5 to 18.7)# | 46.3 (37.4 to 57.3)# | 192.8 (159.4 to 233.0)# |
Rates are adjusted for age category and gender.
Meals indicates preparing their own meals.
Shopping indicates shopping for personal items, such as toilet items or medicine.
Heavy housework indicates doing heavy work around the house like scrubbing floors, washing windows, and doing heavy yard work.
Light housework indicates doing light work around the house like doing dishes, straightening up, light cleaning, or taking out the trash.
Adjusted for age; gender; race (white, African American, other); ethnicity (Hispanic); high school education or less; household income (< $15,000, $15,000 to <$30,000, $30,000 to <$50,000, ($50,000); living alone; reporting being frequently depressed or anxious; reporting being frequently confused, disoriented, or forgetful.
P < .0001.
DISCUSSION
Over 10% of noninstitutionalized adults residing in the U.S. reported at least some problem with lower extremity mobility. Other studies of mobility difficulties have examined older adults7–11 or special populations.11–14 The NHIS-D offered a unique opportunity to examine prevalence among persons of all ages nationwide. It suggests that self-perceived mobility difficulties are common, including among nonelderly persons. Many people with mobility difficulties reported developing the problem in middle age.
The absolute numbers of people with mobility difficulties will grow over the next decades. Today, only 12.8% of U.S. residents are older than 65 years, but this will surpass 20% by 2030 with aging “baby boomers.”33 New treatments for chronic conditions will presumably reduce mobility impairments. Changing personal behaviors, such as increasing exercise and decreasing smoking, will help, although overexertion injuries and persistent obesity could attenuate beneficial effects. In the meantime, our findings highlight the importance of identifying and addressing mobility difficulties, including among younger patients.
Obviously, specific clinical interventions will vary for different causes of mobility difficulties, but there are several common implications. Mobility difficulties were associated with higher rates of depression, fear, anxiety, confusion, obesity, poor vision, dizziness, imbalance, and other worrisome findings. Some of these findings, most notably poor vision, dizziness, imbalance, and needing support, are significantly associated with risk of falls.34–37 Reduced physical activity and limited weight bearing exercise make people with impaired mobility especially susceptible to osteoporosis and compromised cardiovascular and respiratory fitness.38–43 Obesity complicates the picture, especially for encouraging exercise.44 From the NHIS-D, we cannot tell whether people have impaired mobility because of obesity, or whether the obesity results from decreased physical activity caused by mobility problems. Care for people with mobility difficulties therefore must address several issues, including maximizing and maintaining physical function or compensating for its loss (e.g., with wheelchairs, scooters); treating underlying medical diseases, comorbid conditions, and mental health needs45,46; minimizing risk factors for injury; and considering routine screening and preventive services recommended for most adults.47–51
Socioeconomic factors may affect plans for comprehensive interventions. As expected,9,52 people reporting mobility difficulties were more likely than others to be impoverished, poorly educated, and unable to work. They were also more likely to live alone, even though they reported lesser ability to perform routine daily activities, such as preparing meals. The combined effects of poverty and inability to perform daily tasks raise fundamental questions about quality of life.53 However, health insurers, including Medicare,54 strictly limit coverage of services to meet basic daily needs (e.g., personal assistance). Medicare and other insurers typically do not pay for physical therapy to maintain physical function or prevent its decline55 or for ongoing occupational therapy to monitor safety in the home. Similarly, health insurers often resist paying for mobility aids,56–58 despite little evidence that wheelchairs, in particular, are overprescribed.59
To advocate effectively for patients, primary care physicians may need additional education about performing mobility assessments, working with physical and occupational therapists, and the range of options for improving or restoring mobility. While physiatrists and many geriatricians emphasize patients' daily functioning, primary care physicians often do not.6 Primary care physicians typically receive little formal training in addressing concerns such as ambulation; some believe that such activities lie beyond their purview; and many are unsure when to refer patients to physical or occupational therapists.6 Several studies suggest that primary care physicians frequently fail to accurately assess patients' functional limitations.1–6 About two thirds of people with various disabilities have not received rehabilitation because their physicians did not recommend it.60 Although many mobility aids now exist,24–29 primary care physicians are typically unaware of these options, the process for prescribing them, and approaches for evaluating patients' needs. Guidelines for these activities do exist.40
More thought is needed about how to integrate assessments of patients' mobility into primary care encounters. While systematically assessing patients' functional status should identify areas of need, the research evidence is mixed about its value in improving patients' outcomes.5,61,62 Adding questions about functioning to the standard review of systems could help, but brief questioning, intermingled with queries about acute signs and symptoms, may not elicit patients' true concerns about mobility. Several tools capture different dimensions of functional abilities, including walking.63–65 Some physicians ask patients to complete functional status questionnaires in waiting rooms prior to their visits; patients' acceptance of such questionnaires is generally high.64–66
More thought is also needed about how best to deal with barriers raised by the current health care environment. Progressively shortening appointment times, virtually by definition, limit the scope and depth of discussions between physicians and patients. Ironically, addressing the full range of health-related concerns may require multiple visits for the people least able to get around. Physicians often need extra time to position people with mobility problems safely on examining tables or to watch them walk.67 In addition, despite the Americans with Disabilities Act and other laws mandating access to public spaces and services, physically inaccessible care sites and inadequate equipment (e.g., examining tables without automated height adjustment) continue to compromise care for people with mobility problems.46,49,68,69 Another challenge involves developing collaborative relationships with clinicians expert in functional assessments and rehabilitation, including physiatrists and physical and occupational therapists. While research about the outcomes of rehabilitation and physical and occupational therapy has increased in the last decade, more studies are needed.70
Our study has important limitations related to its data source. The NHIS-D did not address several crucial physical functions, such as surmounting curbs, essential to full mobility around communities. The self-reported causes (Table 3) often did not represent specific clinical diagnoses and were not validated. While self-reports provide the only authentic information about persons' perceptions of their functioning, the clinical accuracy of these assessments is unknown. Other studies have raised questions about the objectivity of such self-reports.14,71
Proxies provided about one third of the responses, complicating interpretation of the findings.72–74 The mean age of self-respondents was 46.4 years, compared to 41.2 for persons with proxies; men were less likely to respond themselves (45.2%) than women (66.6%). Self-respondents were more likely to report mobility difficulties (13.0%) than those with proxy respondents (6.7%).72 This makes sense: self-respondents could have been at home explicitly because of mobility problems, while those without difficulties were out and unable to respond in person. Studies comparing self-reports to proxy reports generate varied conclusions, but most suggest that proxies rate both physical functional status and emotional and social well-being as more impaired than do patients.73–81 Determining the true effect of proxy responses on mobility problem rates requires further study.
Finally, the NHIS-D gives only cross-sectional views of noninstitutionalized persons. Including people in nursing homes and other residential facilities would raise population estimates for mobility difficulties. Among roughly 2.1 million Medicare beneficiaries living in long-term care facilities, 85.2% have mobility difficulties, ranging from 50.7% for persons under age 65 to 94.9% for persons 85 and older.82 Longitudinal analyses of older persons suggest that serious functional limitations have declined importantly over recent years.7,10,83 Despite its limitations, the NHIS-D is likely to provide the best information on population prevalence of disabling conditions for the foreseeable future. Conducting such nationally representative surveys is expensive and methodologically difficult.
One positive perspective is that concerned primary care doctors are uniquely placed to help.84 Recognizing and listening to patients who have difficulty walking will become a public health priority with our aging population. These discussions must balance physical realities with recognition of the options for assisting people to move freely and independently about their communities and beyond. In many instances, addressing mobility difficulties could truly improve patients' quality of life.84–89
Acknowledgments
Dr. Iezzoni was supported by The Robert Wood Johnson Foundation Investigator Award in Health Policy Research.
REFERENCES
- 1.Stewart MA, Buck CW. Physicians' knowledge of and response to patients' problems. Med Care. 1977;15:578–85. doi: 10.1097/00005650-197707000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Wartman SA, Morlock LL, Malitz FE, Palm E. Impact of divergent evaluations by physicians and patients of patients' complaints. Public Health Rep. 1983;98:141–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson E, Conger B, Douglass R, et al. Functional health status levels of primary care patients. JAMA. 1983;249:3331–8. [PubMed] [Google Scholar]
- 4.Calkins DR, Rubenstein LV, Cleary PD, et al. Failure of physicians to recognize functional disability in ambulatory patients. Ann Intern Med. 1991;114:451–4. doi: 10.7326/0003-4819-114-6-451. [DOI] [PubMed] [Google Scholar]
- 5.Calkins DR, Rubenstein LV, Cleary PD, et al. Functional disability screening of ambulatory patients: a randomized controlled trial in a hospital-based group practice. J Gen Intern Med. 1994;9:590–2. doi: 10.1007/BF02599291. [DOI] [PubMed] [Google Scholar]
- 6.Hoenig H. Educating primary care physicians in geriatric rehabilitation. Clin Ger Med. 1993;9:883–93. [PubMed] [Google Scholar]
- 7.Freedman VA, Martin LG. Understanding trends in functional limitations among older Americans. Am J Public Health. 1998;88:1457–62. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harris T, Kovar MG, Suzman R, Kleinman JC, Feldman JJ. Longitudinal study of physical ability in the oldest old. Am J Public Health. 1989;79:698–702. doi: 10.2105/ajph.79.6.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kovar MG, Weeks JD, Forbes WF. Disability among older people: United States and Canada. Vital Health Stat. 1995;5(8):1–82. [PubMed] [Google Scholar]
- 10.Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proc Nat Acad Sci. 1997;94:2593–8. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guralnik JM, Fried LP, Simonsick EM, editors. Bethesda, Md: National Institute on Aging; 1995. The Women's Health and Aging Survey: Health and Social Characteristics of Older Women with Disability. NIH publication 95-4009. eds. [Google Scholar]
- 12.Branch LG, Jette AM. The Framingham disability study: I. Social disability among the aging. Am J Public Health. 1981;71:1202–10. doi: 10.2105/ajph.71.11.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jette AM, Branch LG. The Framingham disability study: II. Physical disability among the aging. Am J Public Health. 1981;71:1211–6. doi: 10.2105/ajph.71.11.1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly-Hayes M, Jette AM, Wolf PA, D'Agostino RB, Odell PM. Functional limitations and disability among elders in the Framingham study. Am J Public Health. 1992;82:841–5. doi: 10.2105/ajph.82.6.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Adams PF, Marano MA. Current estimates from the National Health Interview Survey, 1994. National Center for Health Statistics. Vital Health Stat. 1995;10(193) [PubMed] [Google Scholar]
- 16.National Health Interview Survey on Disability Web site Data collection survey instruments questionnaires for 1994 National Health Interview Survey Supplement Booklet: Disability Phase I and 1995 National Health Interview Survey Supplement Booklet: Disability Phase I. Available at: http://www.cdc.gov/nchs/about/major/nhis_dis/nhis_dis.htm Accessed July 28, 1998.
- 17.Kerrigan DC, Schaufele M, Wen MN. Gait analysis. In: DeLisa JA, Gans BM, editors. Rehabilitation Medicine: Principles and Practice. 3rd ed. Philadelphia: Lippincott-Raven Publishers; 1998. pp. 167–87. In: [Google Scholar]
- 18.Alexander NB. Gait disorders in older adults. J Am Ger Soc. 1996;44:434–51. doi: 10.1111/j.1532-5415.1996.tb06417.x. [DOI] [PubMed] [Google Scholar]
- 19.Tinetti ME. Performance-oriented assessment of mobility problems in elderly patients. J Am Geriar Soc. 1986;34:119–26. doi: 10.1111/j.1532-5415.1986.tb05480.x. [DOI] [PubMed] [Google Scholar]
- 20.Tinetti ME, Ginter SF. Identifying mobility dysfunctions in elderly patients. JAMA. 1988;259:1190–3. [PubMed] [Google Scholar]
- 21.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get up & go” test. Arch Phys Med Rehabil. 1986;67:387–9. [PubMed] [Google Scholar]
- 22.Podsiadlo D, Richardson S. The timed “up & go”: a test of basic functional mobility for frail elderly persons. J Am Geriar Soc. 1991;39:142–8. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 23.Nutt JG, Marsden CD, Thompson PD. Human walking and higher-level gait disorders, particularly in the elderly. Neurology. 1993;43:268–79. doi: 10.1212/wnl.43.2.268. [DOI] [PubMed] [Google Scholar]
- 24.Joyce BM, Kirby RL. Canes, crutches and walkers. Am Fam Physician. 1991;43:535–42. [PubMed] [Google Scholar]
- 25.Ragnarsson KT. Lower extremity orthotics, shoes, and gait aids. In: DeLisa JA, Gans BM, editors. Rehabilitation Medicine: Principles and Practice. 3rd ed. Philadelphia: Lippincott-Raven Publishers; 1998. pp. 651–67. In: [Google Scholar]
- 26.Karp G. Sebastpol, Calif: O'Reilley & Associates; 1998. Choosing a Wheelchair. A Guide for Optimal Independence. [Google Scholar]
- 27.Karp G. Sebastpol, Calif: O'Reilley & Associates; 1999. Life on Wheels. For the Active Wheelchair User. [Google Scholar]
- 28.Palmer ML, Toms JE. 3rd ed. Philadelphia: F.A. Davis Company; 1992. Manual for Functional Training; pp. 119–26. [Google Scholar]
- 29.Warren CG. Powered mobility and its implications. J Rehabil Res Dev Clin Suppl. 1990;(2):74–85. [PubMed] [Google Scholar]
- 30.Oliver M. New York: St. Martin's Press; 1996. Understanding Disability: From Theory to Practice. [Google Scholar]
- 31.Thomson RG. New York: Columbia University Press; 1997. Extraordinary Bodies. Figuring Physical Disability in American Culture and Literature. [Google Scholar]
- 32.Charlton JI. Berkeley, Calif: University of California Press; 1998. Nothing About Us Without Us: Disability Oppression and Empowerment. [Google Scholar]
- 33.Feasley JC, editor. Washington, DC: National Academy Press; 1996. Health Outcomes for Older People: Questions for the Coming Decade. [PubMed] [Google Scholar]
- 34.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–7. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 35.Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315:1049–53. doi: 10.1136/bmj.315.7115.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337:1279–84. doi: 10.1056/NEJM199710303371806. [DOI] [PubMed] [Google Scholar]
- 37.Rizzo JA, Friedkin R, Williams CS, Nabors J, Acampora D, Tinetti ME. Health care utilization and costs in a Medicare population by fall status. Med Care. 1998;36:1174–88. doi: 10.1097/00005650-199808000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Wagner EH, LaCroix AZ, Buchnes DM, Larson EB. Effects of physical activity on health status in older adults I: observational studies. Annu Rev Public Health. 1992;13:451–68. doi: 10.1146/annurev.pu.13.050192.002315. [DOI] [PubMed] [Google Scholar]
- 39.Santiago MC, Coyle CP, Kinney WB. Aerobic exercise effect on individuals with physical difficulties. Arch Phys Med Rehabil. 1993;74:1192–8. [PubMed] [Google Scholar]
- 40.Davis G, Plyley MJ, Shephard RJ. Gains of cardiorespiratory fitness with arm crank training in spinally disabled men. Can J Sport Sci. 1991;16:64–72. [PubMed] [Google Scholar]
- 41.Compton DM, Eisenman PA, Henderson HL. Exercise and fitness for persons with disabilities. Sports Med. 1989;7:150–62. doi: 10.2165/00007256-198907030-00002. [DOI] [PubMed] [Google Scholar]
- 42.Fentem PH. Exercise in prevention of disease. Br Med Bull. 1992;48:630–50. doi: 10.1093/oxfordjournals.bmb.a072568. [DOI] [PubMed] [Google Scholar]
- 43.Ensrud KE, Nevitt MC, Yunis C. Correlates of impaired function in older women. J Am Geriatr Soc. 1994;42:481–9. doi: 10.1111/j.1532-5415.1994.tb04968.x. [DOI] [PubMed] [Google Scholar]
- 44.Wee CC, McCarthy EP, Davis RB, Phillips RS. Physician counseling about exercise. JAMA. 1999;282:1583–8. doi: 10.1001/jama.282.16.1583. [DOI] [PubMed] [Google Scholar]
- 45.Verbrugge LM, Lepkowski JM, Imanaka Y. Comorbidity and its impact on disability. Milbank Q. 1989;67:450–84. [PubMed] [Google Scholar]
- 46.Burns TJ, Batavia AI, Smith QW, DeJong G. Primary health care needs of persons with physical disabilities: what are the research and service priorities? Arch Phys Med Rehabil. 1990;71:138–43. [PubMed] [Google Scholar]
- 47.Stuifbergen AK, Becker H, Sands D. Barriers to health promotion for individuals with disabilities. Fam Community Health. 1990;13:11–22. [Google Scholar]
- 48.Stuifbergen AK, Becker HA, Ingalsbe K, Sands D. Perceptions of health among adults with disabilities. Health Values. 1990;14:18–26. [Google Scholar]
- 49.Gans BM, Mann NR, Becker BE. Delivery of primary care to the physically challenged. Arch Phys Med Rehabil. 1993;74:S15–9. [PubMed] [Google Scholar]
- 50.Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility impairments and use of screening and preventive services. Am J Pub Health. 2000;90:955–61. doi: 10.2105/ajph.90.6.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.U.S. Preventive Services Task Force . 2nd ed. Baltimore, Md: Williams & Wilkins; 1996. Guide to Clinical Preventive Services. [Google Scholar]
- 52.DeJong G, Batavia AI, Griss R. America's neglected health minority: working-age persons with disabilities. Milbank Q. 1989;67(Suppl 2 Pt 2):311–51. [PubMed] [Google Scholar]
- 53.Bassuk SS, Glass TA, Berkman LF. Social disengagement and incident cognitive decline in community-dwelling elderly patients. Ann Intern Med. 1999;131:165–73. doi: 10.7326/0003-4819-131-3-199908030-00002. [DOI] [PubMed] [Google Scholar]
- 54.Helbing C, Sangl JA, Silverman HA. Home health agency benefits. Health Care Financ Rev Annu Suppl. 1992;14:125–48. [PubMed] [Google Scholar]
- 55.Cassel CK, Besdine RW, Siegel LC. Restructuring Medicare for the next century: what will beneficiaries really need? Health Aff (Millwood) 1999;18:118–31. doi: 10.1377/hlthaff.18.1.118. [DOI] [PubMed] [Google Scholar]
- 56.LaPlante MP, Hendershot GE, Moss AJ. Assistive technology devices and home accessibility features: prevalence, payment, need, and trends. Adv Data. 1992;217:1–11. [PubMed] [Google Scholar]
- 57.Batavia AI. Of wheelchairs and managed care. Health Aff (Millwood) 1999;18:177–82. doi: 10.1377/hlthaff.18.6.177. [DOI] [PubMed] [Google Scholar]
- 58.Iezzoni LI. Boundaries. Health Aff (Millwood) 1999;18:171–6. doi: 10.1377/hlthaff.18.6.171. [DOI] [PubMed] [Google Scholar]
- 59.Wickizer TM. Controlling outpatient medical equipment costs through utilization management. Med Care. 1995;33:383–91. doi: 10.1097/00005650-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 60.American Medical Association, Department of Geriatric Health . 2nd ed. Chicago: American Medical Association; 1996. Guidelines for the Use of Assistive Technology: Evaluation, Referral, Prescription. [Google Scholar]
- 61.Rubenstein LV, McCoy JM, Cope DW, et al. Improving patient quality of life with feedback to physicians about functional status. J Gen Intern Med. 1995;10:607–14. doi: 10.1007/BF02602744. [DOI] [PubMed] [Google Scholar]
- 62.Espallargues M, Valderas JM, Alonso J. Provision of feedback on perceived health status to health care professionals. A systematic review of its impact. Med Care. 2000;38:175–86. doi: 10.1097/00005650-200002000-00007. [DOI] [PubMed] [Google Scholar]
- 63.Stewart AL, Greenfield S, Hays RD, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262:907–13. [PubMed] [Google Scholar]
- 64.Nelson E, Wasson J, Kirk J, et al. Assessment of function in routine clinical practice: description of the COOP Chart method and preliminary findings. J Chronic Dis. 1987;40(Suppl 1):55S–69S. doi: 10.1016/s0021-9681(87)80033-4. [DOI] [PubMed] [Google Scholar]
- 65.Wasson J, Keller A, Rubenstein L, Hays R, Nelson E, Johnson D. Benefits and obstacles of health status assessment in ambulatory settings. The clinician's point of view. The Dartmouth Primary Care COOP Project. Med Care. 1992;30(5 Suppl):MS42–9. doi: 10.1097/00005650-199205001-00004. [DOI] [PubMed] [Google Scholar]
- 66.Wald JS, Rind D, Safran C, Kowaloff H, Barker R, Slack WV. Patient entries in the electronic medical record: an interactive interview used in primary care. Proc Annu Symp Comput Appl Med Care. 1995:147–51. [PMC free article] [PubMed] [Google Scholar]
- 67.Iezzoni LI. What should I say? Communication around disability. Ann Intern Med. 1998;129:661–5. doi: 10.7326/0003-4819-129-8-199810150-00018. [DOI] [PubMed] [Google Scholar]
- 68.Peters L. Women's health care. Approaches in delivery to physically disabled women. Nurse Pract. 1982;7:34–48. [PubMed] [Google Scholar]
- 69.President's Advisory Commission on Consumer Protection and Quality in the Health Care Industry. Consumer Bill of Rights and Responsibilities. 1997. Washington, DC:
- 70.Hoenig H, Nusbaum N, Brummel-Smith K. Geriatric rehabilitation: state of the art. J Am Geriatr Soc. 1997;45:1371–81. doi: 10.1111/j.1532-5415.1997.tb02939.x. [DOI] [PubMed] [Google Scholar]
- 71.Mathiowetz NA, Lair TJ. Getting better? Change or error in the measurement of functional limitations. J Econ Soc Measure. 1994;20:237–62. [Google Scholar]
- 72.Iezzoni LI, McCarthy EP, Davis RB, Siebens H. Mobility problems and perceptions of disability in self- and proxy-respondents. Med Care. 2000;38:1051–7. doi: 10.1097/00005650-200010000-00009. [DOI] [PubMed] [Google Scholar]
- 73.Andresen EM, Fitch CA, McLendon M, Meyers AR. Reliability and validity of disability questions for US census 2000. Am J Pub Health. 2000;90:1297–9. doi: 10.2105/ajph.90.8.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Todorov A, Kirchner C. Bias in proxies' report of disability: data from the National Health Interview Survey on disability. Am J Pub Health. 2000;90:1248–53. doi: 10.2105/ajph.90.8.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Epstein AM, Hall JA, Tognetti J, Son LH, Conant L., Jr Using proxies to evaluate quality of life. Can they provide valid information about patients' health status and satisfaction with medical care? Med Care. 1989;27(3 Suppl):S91–8. [PubMed] [Google Scholar]
- 76.Branch LG, Meyers AR. Assessing physical function in the elderly. Clin Geriatr Med. 1987;3:29–51. [PubMed] [Google Scholar]
- 77.Magaziner J, Simonsick EM, Kashner TM, Hebel JR. Patient-proxy response comparability on measures of patient health and functional status. J Clin Epidemiol. 1988;41:1065–74. doi: 10.1016/0895-4356(88)90076-5. [DOI] [PubMed] [Google Scholar]
- 78.Rothman ML, Hedrick SC, Bulcroft KA, Hickam DH, Rubenstein LZ. The validity of proxy-generated scores as measures of patient health status. Med Care. 1991;29:115–24. doi: 10.1097/00005650-199102000-00004. [DOI] [PubMed] [Google Scholar]
- 79.Dorevitch MI, Cossar RM, Bailey FJ, et al. The accuracy of self and informant rating of physical functional capacity in the elderly. J Clin Epidemiol. 1992;45:791–8. doi: 10.1016/0895-4356(92)90057-t. [DOI] [PubMed] [Google Scholar]
- 80.Spragers MA, Aaronson NK. The role of health care providers and significant others in evaluating the quality of life of patients with chronic disease: a review. J Clin Epidemiol. 1992;45:743–60. doi: 10.1016/0895-4356(92)90052-o. [DOI] [PubMed] [Google Scholar]
- 81.Sneeuw KC, Aaronson NK, Osoba D, et al. The use of significant others as proxy raters of the quality of life of patients with brain cancer. Med Care. 1997;35:490–506. doi: 10.1097/00005650-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 82.Olin GL, Hongji L, Merriman B. Rockville, Md: Westat; 1999. Health & Health Care of the Medicare Population: Data from the 1995 Medicare Current Beneficiary Survey; p. 77. [Google Scholar]
- 83.Allaire SH, LaValley MP, Evans SR, et al. Evidence for decline in disability and improved health among persons aged 55 to 70 years: the Framingham Heart Study. Am J Public Health. 1999;89:1678–83. doi: 10.2105/ajph.89.11.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Iezzoni LI. When walking fails. JAMA. 1996;276:1609–13. doi: 10.1001/jama.276.19.1609. [DOI] [PubMed] [Google Scholar]
- 85.Miles-Tapping C, MacDonald LJ. Lifestyle implications of power mobility. Phys Occup Therapy Ger. 1994;12:31–49. [Google Scholar]
- 86.Abresch RT, Seyden NK, Wineinger MA. Quality of life: issues for persons with neuromuscular disease. Phys Med Rehabil Clin N Am. 1998:233–48. [PubMed] [Google Scholar]
- 87.Mairs N. Boston: Beacon Press; 1996. Waist-high in the World; pp. 38–9. [Google Scholar]
- 88.Cleland M. Atlanta: Cherokee Publishing Company; 1989. Strong at the Broken Places. [Google Scholar]
- 89.Scherer MJ. Cambridge, Mass: Brookline Books; 1996. Living in the State of Stuck. How Technology Impacts the Lives of People with Disabilities. [Google Scholar]