Abstract
Because widely held stereotypes characterize obese people as less intelligent, unhappy, lacking in self control and more prone to psychological problems, we tested whether obese appearance alone would affect medical students' decisions about the diagnosis and management of simulated patients. We videotaped 4 patient simulators presenting each of 4 cases in 2 states: normal and obese (by using padding and bulky clothing). Seventy-two clinical students at 2 medical schools viewed the cases and answered questions about diagnostic tests and management. We found the expected biases toward patients when in their obese form as well as pessimism about patient compliance and success of therapy, but there were no significant differences in tests or treatments ordered except where appropriate for an obese patient (e.g., weight reduction diet). Thus, the appearance of obesity alone biased the students' impressions of the patients, but did not affect diagnostic test ordering.
Widely held stereotypes characterize obese people as less intelligent, lacking in self control, unhappy, lazy, and poorly motivated. These stereotypes can be found among health professionals,1 including physicians and medical students.2 In addition, one study found that health care workers considered psychological causes of illness more likely in obese patients.3 There is little evidence, however, that these characterizations are true. If they were widely accepted, they could affect diagnosis and management.
To investigate whether obesity alone would affect diagnosis and management decisions, we asked third- and fourth- year students to view 4 videotaped encounters of patients presenting with abdominal pain and make recommendations regarding diagnosis, management, and prognosis based on the patient's history. Four patient simulators were videotaped in 2 forms: normal and made up to appear obese. Based on the previous studies, we hypothesized that when the students saw the patients in their obese form, they would form a different impression about them, would see them as less compliant, less motivated, and less likable, and would be more likely to ascribe their illness to psychological factors. These impressions, in turn, would affect the tests they ordered.
METHODS
Design of the Cases
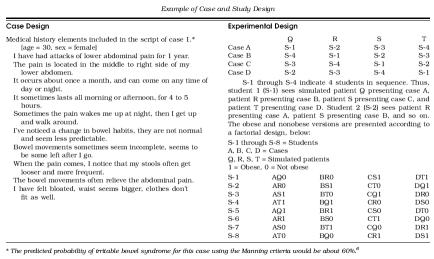
We constructed 4 unique cases: all were patients complaining of abdominal pain and disturbance in bowel motility. The cases differed in which complaint was dominant and the location and severity of the pain. To test whether students would be biased toward a psychological cause in the obese cases, we constructed each case to have an equal likelihood of organic versus functional (psychological) cause. To do this, we constructed the histories using research studies that had calculated the impact of various symptoms in predicting organic versus functional disease.4–6 Because these studies had used standardized questionnaires, we were able to specify the symptoms precisely. A sample case and details of the study design are shown in the Appendix.
Simulated Patients
Four drama students from the University of Nebraska at Omaha presented the cases, simulating patients who are visiting a physician for the first time for these complaints. Each simulator first videotaped each of the 4 cases in their normal appearance, then again using padding and bulky clothing to appear morbidly obese (Fig. 1). This produced 32 different recordings: 4 sets of the 4 cases in 2 two modes (obese and nonobese).
FIGURE 1.
Patient “S” as she appeared on the videotape showing nonobese and obese formats.
Students
We recruited 32 third-year and 16 fourth-year students over a 6-month period from students rotating on general internal medicine at the University of Nebraska College of Medicine and 24 third-year students from Northwestern University Medical School. The students were a convenience sample based on the location and month of their scheduled clinical service. All those approached participated. None were obese.
Experimental Design
Each student saw 4 different cases, each presented by a different simulated patient according to the scheme in the Appendix. Cases were arranged according to a fractional factorial design7 such that each student saw 2 obese and 2 nonobese presenters, but no student saw the same presenter in both obese and nonobese form. This design controlled for the effects of the case, the patient, and obese appearance. The sequence repeated for every 8 participants.
Measurements
After each presentation, we asked students to select the tests and treatments they would order from a list of possible choices. For each case, they estimated the success of the treatment, the likelihood that the patient would comply with it, the prognosis, and their working diagnoses. Using the semantic differential technique,8 we asked students to characterize the patient by marking where this patient fit on a line between 2 adjective pairs (e.g., attractive/unattractive, compliant/noncompliant). The distance along the line of the mark from the left end in millimeters was entered as the response. Finally, they answered a validated 15-question form that identifies problem patients.9
Statistical Analysis
We used multivariate analysis of variance to analyze the students' decisions. Because of the balanced design, if there were no effect, the marginal means would be equal for the obese and nonobese state. This was also true for effects due to the case or to the presenter. We used χ2 analysis for frequency data and corrected for multiple comparisons. Analysis of statistical power indicated we would be able to detect differences of 25% in test ordering.
RESULTS
Students' choices of tests and consultations are shown in Table 1. Seeing the obese form of a presentation did not affect the number of tests students ordered, except in the case of blood glucose, gastric pH studies, and dietary counseling. A greater proportion of students thought the obese-appearing patients would be unable to make lifestyle changes if needed for treatment of the gastrointestinal disorder, would not be as responsive to counseling, and would be less likely to comply with diet recommendations. A greater percentage of students (72.7% vs 63.9%) thought the cause of the illness was functional in the obese patients. This difference did not reach statistical significance.
Table 1.
Student Responses
| Normal | Obese | P Value | |
|---|---|---|---|
| % Who said they would order the following in the initial visits | |||
| CBC | 79.2 | 76.4 | NS |
| UA | 43.8 | 43.1 | NS |
| SGOT, LDH, SGPT | 21.5 | 27.8 | NS |
| Amylase, lipase | 25.0 | 29.9 | NS |
| BUN, creatinine | 22.2 | 25.0 | NS |
| Dietary counseling | 43.8 | 58.3 | .005 |
| Blood glucose | 18.8 | 33.3 | .013 |
| Erythrocyte sedimentation rate | 16.0 | 12.5 | NS |
| Gastric pH studies | 15.3 | 27.1 | .014 |
| Hematest of stools | 34.0 | 37.5 | NS |
| T4f | 15.3 | 19.4 | NS |
| Esophageal manometry | 4.9 | 3.5 | NS |
| Psychological testing | 3.6 | 2.8 | NS |
| Upper GI x-ray | 18.8 | 20.1 | NS |
| Barium enema | 14.6 | 16.7 | NS |
| Flexible sigmoidoscopy | 13.9 | 14.4 | NS |
| Colonoscopy | 7.6 | 8.3 | NS |
| Upper GI endoscopy | 18.8 | 20.1 | NS |
| Mammography | 2.0 | 0.0 | NS |
| Nitrogen breath test | 9.0 | 4.9 | NS |
| Abdominal ultrasound | 13.2 | 14.6 | NS |
| % Who said they would order the following assuming all initial studies were negative | |||
| GI consultation | 56.3 | 61.1 | NS |
| Psychiatry consultation | 2.8 | 2.8 | NS |
| Consult with dietitian | 25.0 | 36.8 | .03 |
| % Predicting the following outcomes would occur | |||
| Will not change overall lifestyle | 18.1 | 41.0 | .0001 |
| Will comply fully with dietary regimen | 31.8 | 19.4 | .0001 |
| Will fail to return for follow-up appointment | 0.7 | 4.2 | .06 |
| Counseling will be highly effective | 28.5 | 10.4 | .0001 |
| Will not comply with medication | 2.1 | 4.9 | NS |
| Tests will find organic cause of the problem | 54.9 | 56.3 | NS |
| Functional (vs organic) cause of illness | 63.9 | 72.7 | NS |
CBC indicates complete blood cell; UA, urinalysis, SGOT, aspartate aminotransferase; LDH, lactate dehydrogenase; SGPT, alanine aminotransferase; BUN, blood urea nitrogen; T4, thyroxine; GI, gastrointestinal.
With regard to personal characteristics, students rated the obese-appearing patients as less attractive, less compliant, and more depressed. The total score on the problem patient scale was similar for obese and nonobese patients (40.3 and 39.2, respectively). Answers to individual questions on the problem scale were consistent with the answers to questions on personal characteristics. Students viewing the obese form thought the patient would be less compliant (P < .001) and that they would be less likely to want the patient in their continuity-of-care practice (P < .015).
DISCUSSION
We found that obese appearance alone influenced medical students' impressions about the simulated patients but did not inappropriately affect test and treatment ordering. Students' answers showed the usual biases about obesity, and also showed a greater pessimism about patient compliance and the success of medical therapy, an effect not previously described in the context of medical illness. It is reassuring that the biases did not lead to changes in management.
Stigmatization of obesity is pervasive and has been shown in numerous studies among the general public and among health care workers.1,2 The effect is stronger for individuals who are morbidly obese rather than just overweight. Obese people are characterized as less intelligent, unhappy, physically unattractive, and lacking in self control. In addition, a survey of mental health professionals found they were more likely to assign negative psychological symptoms to obese patients,3 and first-year students at Duke rated simulated overweight patients as unattractive, less intelligent, and less likely to respond to dietary counseling.10
Do these biases affect patient care? Recently, Wee and colleagues found that obese patients were less likely to have received screening tests such as mammography and Pap smears, but could not tell if these differences resulted from differences in physician behavior or from patient factors.11 We did find a trend toward seeing the obese patients' illness as more psychological. We did not, however, find changes in ordering of laboratory tests and procedures that might correspond to a belief that a psychological cause was more likely, e.g., more students requesting psychiatric referrals or fewer students ordering liver function tests or endoscopy. The small increase in ordering 3 of the tests appeared to be related to obesity and medically appropriate. The increased frequency of ordering blood sugar logically relates to the increased incidence of diabetes in overweight individuals. Similarly, the increase in pH measurements may relate to obesity as a risk factor for esophageal reflux disease. Dietary counseling orders presumably were aimed at treating the obesity itself.
We did find that the medical students had less confidence that the obese patient would respond to counseling, be able to make prescribed changes in their lifestyle, or comply with a dietary regimen. Students might assume that the existence of obesity means that a patient has inadequate willpower to diet and, thus, by analogy, would not follow dietary advice or respond to counseling in other areas (e.g., a high fiber diet).
There are several limitations to the results. Responses to simulated patients do not necessarily generalize to actual clinical practice. The study did not have sufficient power to detect smaller differences in test ordering. Also, we do not know if these results generalize to other settings, or physicians in different stages of training.
In summary, these results, while showing the expected biases regarding obese patients, do not show adverse effects on patient management in the workup of abdominal pain.
Acknowledgments
The authors wish to thank Doug Patterson, PhD for help obtaining the simulated patients and Marie Reidelbach, MLS for her assistance administering the study.
Appendix
Table 2.
Example of Case and Study Design
REFERENCES
- 1.Price JH, Desmond SM, Krol RA, Snyder FF, O'Connell JK. Family practice physicians' beliefs, attitudes, and practices regarding obesity. Am J Prev Med. 1987;3:339–45. [PubMed] [Google Scholar]
- 2.Blumberg P, Mellis LP. Medical students' attitudes toward the obese and the morbidly obese. Int J Eat Disord. 1985;4:169–75. [Google Scholar]
- 3.Young LM, Powell B. The effects of obesity on the clinical judgments of mental health professionals. J Health Soc Behav. 1985;26:233–46. [PubMed] [Google Scholar]
- 4.Talley NJ, Phillips SF, Melton J, Wiltgen C, Zinsmeister AR. A patient questionnaire to identify bowel disease. Ann Intern Med. 1989;111:671–4. doi: 10.7326/0003-4819-111-8-671. [DOI] [PubMed] [Google Scholar]
- 5.Manning AP, Thompson WG, Heaton KW, Morris AF. Towards positive diagnosis of the irritable bowel. Br Med J. 1978:653–4. doi: 10.1136/bmj.2.6138.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starmans R, Muris JW, Fijten GH, Schouten HJ, Pop P, Knottnerus JA. The diagnostic value of scoring models for organic and non-organic gastrointestinal disease, including the irritable-bowel syndrome. Med Decis Making. 1994;14:208–16. doi: 10.1177/0272989X9401400302. [DOI] [PubMed] [Google Scholar]
- 7.Plackett RL, Burman JP. The design of optimum multifactorial experiments. Biometrika. 1946;33:305–25. [Google Scholar]
- 8.Osgood C, Suci G, Tannenbaum P. The Measurement of Meaning. Urbana, Ill: The University of Illinois Press; 1957. [Google Scholar]
- 9.McGaghie WC, Whitenack DC. A scale for measurement of the problem patient labeling process. J Nerv Mental Dis. 1982;170:598–604. doi: 10.1097/00005053-198210000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Breytspraak LM, McGee J, Conger JC, Whatley JL, Moore JT. Sensitizing medical students to impression formation processes in the patient interview. J Med Educ. 1977;52:47–54. doi: 10.1097/00001888-197701000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Wee CC, McCarthy EP, Davis RB, Phillips RS. Screening for cervical and breast cancer: is obesity an unrecognized barrier to preventive care? Ann Intern Med. 2000;132:697–704. doi: 10.7326/0003-4819-132-9-200005020-00003. [DOI] [PubMed] [Google Scholar]