Abstract
OBJECTIVE
To determine if patient gender and race affect decisions about pain management.
DESIGN, SETTING, AND PARTICIPANTS
Experimental design using medical vignettes to evaluate treatment decisions. A convenience sample of 111 primary care physicians (61 men, 50 women) in the Northeast was asked to treat 3 hypothetical patients with pain (kidney stone, back pain) or a control condition (sinusitis). Symptom presentation and severity were held constant, but patient gender and race were varied.
MEASUREMENTS AND MAIN RESULTS
The maximum permitted doses of narcotic analgesics (hydrocodone) prescribed at initial and return visits were calculated by multiplying mg per pill × number of pills per day × number of days × number of refills. No overall differences with respect to patient gender or race were found in decisions to treat or in the maximum permitted doses. However, for renal colic, male physicians prescribed higher doses of hydrocodone to white patients versus black patients (426 mg vs 238 mg), while female physicians prescribed higher doses to blacks (335 mg vs 161 mg, F1,85 = 9.65 , P = .003). This pattern was repeated for persistent kidney stone pain. For persistent back pain, male physicians prescribed higher doses of hydrocodone to males than to females (406 mg vs 201 mg), but female physicians prescribed higher doses to females (327 mg v. 163 mg, F1,28 = 5.50 , P = .03).
CONCLUSION
When treating pain, gender and racial differences were evident only when the role of physician gender was examined, suggesting that male and female physicians may react differently to gender and/or racial cues.
Keywords: gender, race, pain treatment
Patient gender and race predict the amount of analgesic given to patients in a variety of clinical settings. In general, women1–3 and minorities3–6 receive less analgesic than men and nonminority patients undergoing similar medical procedures. These findings suggest that, for pain as well as for other medical conditions,7–11 women and minority patients are treated less aggressively. Such findings raise concerns that decisions about pain management may be influenced by patient characteristics unrelated to clinical condition and point to possible treatment biases. Because these studies involved retrospective reviews of medical records, however, it is unclear whether treatment differences reflected patient behavior, the behavior of the medical staff, or both.6 Gender or ethnic differences in style of communication,3,5,12 language spoken, insurance coverage, disease manifestations, or body weight may have resulted in the treatment differences found in these studies.
The aim of this study was to determine whether patient gender and race would influence decisions about pain management. An experimental design using medical vignettes was employed to hold disease characteristics and body weight constant and to vary patient gender and race systematically. Decisions about pain management were assessed by asking physicians to select a course of treatment (i.e., a dose of analgesic) and report on follow-up care in cases where the patient's pain persisted. It was predicted that patients presented as female and as black would receive lower doses of narcotic analgesics than patients described as male and as white.
METHODS
Subjects
Primary care physicians (family practitioners and general internists) were recruited from regions in the Northeast (i.e., Albany and New York City, NY; Worcester and Boston, Mass). They were contacted through listings in local telephone directories and insurance company directories, and through physician referrals. In addition, permission was obtained from department chairs to distribute questionnaires at staff and resident meetings. The protocol was approved by the Human Subjects' Review Committee (Union College, Schenectady, NY), and all subjects provided informed consent.
Approximately 220 surveys were distributed, and 111 (50%) were returned. Table 1 summarizes the characteristics of the 111 participants. Sixty-one (55%) were male, and 50 were (45%) female. Eighty-eight (79%) were white, and 15 (13.5%) were of Asian ancestry; only 3 (2.7%) of the physicians were black. Forty-seven (42%) were family practitioners, and 61 (55%) were internists. All had completed at least 2 years of residency; 98 (88%) were attendings.
Table 1.
Physician Characteristics
| Physicians, n | 111 | |
| Mean age, y (range) | 41.31 (26–72) | |
| Mean number of years in practice (range) | 12 (0–40) | |
| Gender, n (%) | ||
| Male | 61 (55) | |
| Female | 50 (45) | |
| Race or ethnic group, n (%) | ||
| White | 88 (79.3) | |
| Black | 3 (2.7) | |
| Hispanic | 3 (2.7) | |
| Asian/Pacific Islander | 15 (13.5) | |
| No response | 2 (1.8) | |
| Specialty, n (%) | ||
| Family practice | 47 (42.3) | |
| Internal medicine | 61 (55) | |
| No response | 3 (2.7) | |
| Doctor status, n (%) | ||
| Resident | 12 (10.8) | |
| Attending | 98 (88.3) | |
| No response | 1 (0.9) | |
| Board certified, n (%) | ||
| Yes | 95 (85.6) | |
| No | 14 (12.6) | |
| No response | 2 (1.8) |
Materials
Three medical vignettes were created depicting patients suffering from common medical complaints (see Appendix). Two vignettes (kidney stone, back injury) had pain as the primary complaint. The pain was described as acute, severe or intense, and unresponsive to nonprescription analgesics. The 2 painful conditions were chosen because of their very different implications. Kidney stone pain presents a relatively uncomplicated problem; it is infrequent, but not rare, and severe, but not chronic. In contrast, lower back pain is much more common, varies greatly in its intensity, is apt to become chronic, and can lead to continued use of narcotics. The third vignette presented symptoms of sinusitis. The purpose of the sinus scenario was to disguise the study's focus on treatment of pain and to test whether biases in analgesic prescription might mirror those observed in the treatment of other medical conditions.
Each vignette presented a fictitious patient whose race and gender varied. Cues about the patient's race and gender were enhanced by providing fictitious names generated from previous research on ethnic stereotyping.13 White male and female names were Mark/Mary McKenzie, Donald/Donna Stern, and John/Joan Reilly; black male and female names were Malik/Moesha Washington, Darnell/Desiree Tyson, and Jamal/Jamesha Jackson.
Questions following each vignette assessed the aggressiveness with which physicians would treat the symptoms of the presenting patient (see Appendix). For back pain and kidney stone patients, the physicians were given the option of prescribing a combination of hydrocodone and acetaminophen (generic Lortab) or of making other suggestions for easing the patient's pain. If they chose to prescribe hydrocodone, they were asked to choose a strength (2.5, 5.0, 7.5, or 10.0 mg with 500 mg of acetaminophen), a maximum number of pills per day (1 to 12), a maximum number of days (1 to 6), and a number of refills (0 to 3). If they chose to prescribe hydrocodone, they were asked whether they would modify their original prescription if the patient returned to the office complaining of insufficient pain relief, and they were given the same dosing options. Furthermore, physicians were asked if they would prescribe a refill if the patient completed the prescription but complained that the pain returned. Hydrocodone was selected for several reasons: the brand name medication (Lortab) is well known to physicians and is commonly prescribed for moderately severe pain; it comes in a series of strengths; and it is a narcotic and, therefore, has a potential for addiction.
In the sinusitis scenario, physicians were asked if they would treat the patient with antibiotics or recommend other treatments. If they would prescribe antibiotics, they were asked for the type of antibiotic, the duration of treatment in days, and the number of refills, and were asked what they would do if the patient returned in 4 days to report that his or her condition was not improved.
Procedures
A 2 (patient race) × 2 (patient gender) × 2 (physician gender) between-subjects experimental design was used, in which each physician read one version of each vignette. This design was chosen, as in other studies of bias,11,14 because it would have been impossible to mask the true nature of the study if the physicians were given multiple vignettes that were identical on all parameters except for patient gender and race. All physicians read the same 3 scenarios, and the patient characteristics of gender and race were always presented in an alternating fashion (e.g., male-female-male; black-white-black) across the 3 vignettes. Vignettes were distributed using a modified block-randomization design without replacement. The 4 experimental combinations (white male, black male, white female, black female) were randomly ordered and presented in that sequence to male physicians and to female physicians throughout the study.11,14 This procedure ensured that male and female physicians were equally distributed across the 4 conditions and guarded against any effects due to selection bias. Upon completion, physicians were asked to recall the patient characteristics (i.e., gender, age, and ethnicity) from each vignette to assess whether patient cues were salient. Physicians receiving surveys by mail were instructed to seal their responses to the vignettes in the envelope provided before completing the final questionnaire that asked them to recall patient characteristics. All completed surveys were returned on site or mailed back to the investigator. In exchange for their participation, physicians were offered refreshments, or they were given the option of receiving $5.00 in cash or having the money donated to Hospice in their name.
Analysis
SPSS for Windows Version 9.0 (SPSS Inc., Chicago, Ill, 1999) was used for analyses. Frequency analyses were conducted to summarize physician characteristics (Table 1) and to determine the extent to which physicians accurately recalled the patients' race and gender. Pearson χ2 statistics were used for categorical data reflecting physicians' decisions to treat patients with prescription medication and their willingness to revise prescriptions for patients reporting unsatisfactory relief. Chi-square analyses were also used to establish comparability of male and female physicians regarding board certification and specialty, while t tests determined comparability with regard to age and years in practice. The impact of patient gender and patient race on treatment decisions was assessed using a univariate analysis of variance (ANOVA) of hydrocodone doses prescribed for both initial and recurrent kidney stone and back pain. Physician age and years in practice were included as covariates in each ANOVA because male physicians were slightly older and had been in practice longer than female physicians. For both pain scenarios, the total dose of hydrocodone was entered as the dependent variable while patient gender, patient race, and physician gender were entered as fixed factors in the ANOVA. The analysis tested for main effects for patient gender, patient race, and physician gender as well as for interactions between these 3 factors. Total dose of hydrocodone was calculated using the following formula: hydrocodone strength per pill × number pills per day × number of days × number of refills. Exploratory box plot analyses were used to identify outliers that may have contributed to significant effects.
RESULTS
Manipulation Check
Most physicians accurately recalled the gender (98.2%) and race (91.5%) of the patients depicted in the vignettes.
Group Comparability
Male and female physicians did not differ with regard to specialty (family practice vs internal medicine) or board certification. However, male physicians were older (44 vs 38 years; P = .001) and had been in practice more years than female physicians (15 vs 9 years; P = .002).
Kidney Stone Pain
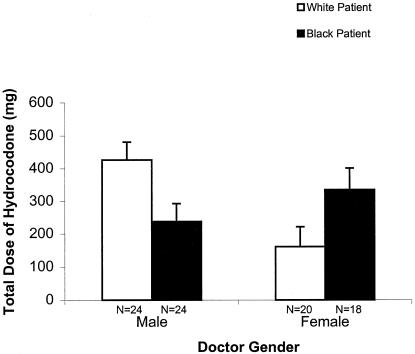
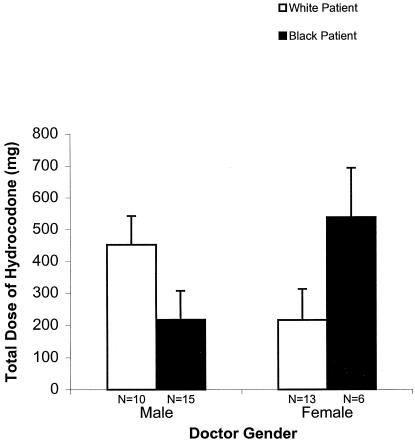
One hundred seven (96.4%) of the physicians opted to treat kidney stone pain with a prescription analgesic. Chi-square analyses revealed that this decision did not vary by physician gender, patient race, or patient gender. Descriptive statistics for doses of hydrocodone prescribed for initial and follow-up treatment of kidney stone pain by patient gender and patient race are presented in Table 2. The ANOVA of hydrocodone prescribed for initial kidney stone pain demonstrated no main effects, and neither covariate was significant (doctor age, P = .83; years in practice, P = .48). Dose of hydrocodone selected did not differ by patient race (white = 308 mg; black = 271 mg), patient gender (male = 251 mg; female = 340 mg), or physician gender (male = 332 mg; female = 248 mg). However, the ANOVA did reveal a significant interaction between physician gender and patient race(F1,85 = 9.65, P = .003). While male physicians prescribed higher doses of hydrocodone to white patients than to black patients (426 mg vs 238 mg), female physicians did the reverse (161 mg vs 335 mg; see Fig. 1). All other interactions tested for by the ANOVA of initial hydrocodone doses selected for kidney stone pain were not significant (i.e., physician gender and patient gender, P = .70; patient gender and patient race, P = .37). The ANOVA of follow-up doses prescribed for persistent kidney stone pain demonstrated similar findings. There were no main effects for patient race (white = 381 mg; black = 319 mg), patient gender (male = 258 mg; female = 366), or physician gender (male = 335 mg; female = 378 mg), and neither covariate was significant (physician age, P = .83, years in practice, P = .54). However, a similar interaction between physician gender and patient race occurred for hydrocodone prescribed to patients complaining of inadequate analgesia (F1,43 = 6.90, P = .01). Male physicians' revised doses of hydrocodone were higher for white patients than for black patients (452 mg vs 218 mg), while female physicians' revised doses were higher for black patients (539 mg vs 217 mg; seeFig. 2. No significant interactions were demonstrated between physician gender and patient gender (P = .61) or patient gender and patient race (P = .93) for follow-up care. Chi-square analysis revealed that male physicians were more likely than female physicians to prescribe refills of hydrocodone to kidney stone patients of either race (χ12 = 5.16, P = .03). We ran exploratory box plot analyses to identify any outliers with regard to kidney stone treatment. No changes in the results occurred when these were excluded.
Table 2.
Initial and Follow-up Hydrocodone Doses (mg) Prescribed for Kidney Stone Pain by Patient Race and Patient Gender
| Patient Gender | Patient Race | Initial Treatment | Follow-up Treatment | ||||
|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | ||
| Male | White | 24 | 286 | 328 | 14 | 227 | 255 |
| Black | 23 | 214 | 166 | 13 | 290 | 234 | |
| Total | 47 | 251 | 261 | 27 | 258 | 243 | |
| Female | White | 20 | 335 | 344 | 9 | 365 | 413 |
| Black | 19 | 345 | 268 | 8 | 366 | 264 | |
| Total | 39 | 340 | 305 | 17 | 366 | 341 | |
| Total | White | 44 | 308 | 332 | 23 | 281 | 325 |
| Black | 42 | 271 | 225 | 21 | 319 | 242 | |
| Total | 86 | 291 | 284 | 44 | 299 | 286 | |
FIGURE 1.
Mean initial doses of hydrocodone (mg) prescribed by physician gender and patient race for kidney stone pain. Error bars indicate standard errors.
FIGURE 2.
Mean follow-up doses of hydrocodone (mg) prescribed by physician gender and patient race for kidney stone pain. Error bars indicate standard errors.
Back Pain
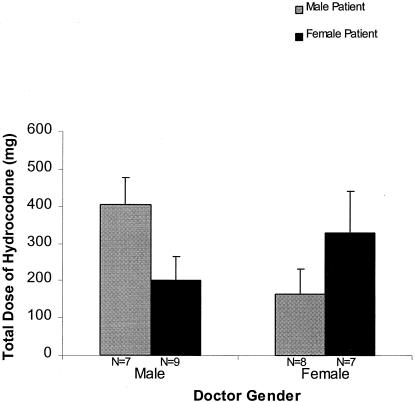
Ninety physicians (81.1%) opted to treat back pain with a prescription analgesic. Descriptive statistics for doses of hydrocodone prescribed for initial and follow-up treatment of back pain by patient gender and patient race are presented in Table 3. As with kidney stone pain, χ2 analyses demonstrated that the decision to treat back pain did not vary by patient race, patient gender, or physician gender. Furthermore, ANOVA analyses of total initial hydrocodone doses prescribed for back pain demonstrated no main effects for patient race (white = 188 mg; black = 233 mg), patient gender (male = 192 mg; female = 233 mg), or physician gender (male = 212 mg; female = 215 mg); neither covariate was significant (physician age, P = .68; years in practice, P = .56). No interactions between physician gender and patient race (P = .37), physician gender and patient gender (P = .90), or patient gender and patient race (P = .80) were demonstrated. Similarly, the ANOVA of follow-up hydrocodone doses prescribed for back pain demonstrated no main effects for patient race (white = 245 mg; black = 290 mg), patient gender (male = 268 mg; female = 272 mg), or physician gender (male = 304 mg; female = 246 mg); neither covariate was significant (physician age, P = .68; years in practice, P = .56). However, analyses of revised prescriptions for follow-up care revealed an interaction between physician gender and patient gender (F1,28 = 5.50, P = .03). As shown in Figure 3, male physicians who revised their prescriptions gave higher follow-up doses of hydrocodone to male patients than to female patients (406 mg vs 201 mg), and female physicians prescribed higher doses to female patients than to male patients (327 mg vs 163 mg). No interactions between physician gender and patient race (P = .56) or patient gender and patient race (P = .22) were demonstrated. Male physicians were, however, more likely than female physicians to prescribe refills of hydrocodone to patients suffering recurrent back pain, regardless of the patient's gender (χ12 = 108 = 4.38, P = .03). Exploratory box plot analyses revealed that there were no outliers with regard to back pain treatment.
Table 3.
Initial and Follow-up Hydrocodone Doses (mg) Prescribed for Back Pain by Patient Race and Patient Gender
| Patient Gender | Patient Race | Initial Treatment | Follow-up Treatment | ||||
|---|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | ||
| Male | White | 19 | 177 | 157 | 8 | 291 | 282 |
| Black | 18 | 207 | 143 | 7 | 241 | 208 | |
| Total | 37 | 192 | 149 | 15 | 268 | 242 | |
| Female | White | 15 | 202 | 91 | 5 | 171 | 111 |
| Black | 19 | 258 | 212 | 9 | 328 | 146 | |
| Total | 34 | 233 | 170 | 14 | 272 | 151 | |
| Total | White | 34 | 188 | 131 | 13 | 245 | 233 |
| Black | 47 | 233 | 181 | 16 | 290 | 175 | |
| Total | 71 | 211 | 160 | 29 | 270 | 200 | |
FIGURE 3.
Mean follow-up doses of hydrocodone (mg) prescribed by physician gender and patient gender for back pain. Error bars indicate standard errors.
Sinus Infection
Ninety-one physicians (82%) reported that they would treat a probable sinus infection by prescribing an antibiotic. Male and female physicians' initial decision to treat sinusitis did not differ by patient gender or race. However, white patients were prescribed a longer course of antibiotics (mean, 13.7 vs 9.2 days; F1,87 = 4.90, P = .03) and were prescribed refills for their antibiotic more often than were black patients (χ12 = 107 = 4.05, P = .04). In addition, male patients were prescribed a more expensive, broader coverage antibiotic more often than were female patients (χ12 = 106 = 6.41, P < .04). Male physicians were more likely than female physicians to allow their patients with sinusitis to refill their antibiotic (χ12 = 107 = 4.35, P = .04).
DISCUSSION
We expected on the basis of previous studies1–6 that physicians presented with medical vignettes would treat the pain of women and minority patients less aggressively, but we found no overall differences in decisions to prescribe analgesic or in doses of analgesic selected. In fact, physicians' initial decisions to treat patients' medical complaints were unaffected by patient gender or race across all 3 medical conditions. The lack of overall treatment bias revealed in this study is an important finding, especially given recent concerns about the media's overstatement of research findings implying that discrimination pervades medical decision making.15
We did find, however, a more complicated set of treatment patterns that suggest possible differences in the treatment approaches of male and female physicians. When treating hypothetical kidney stone pain, male physicians prescribed twice as much hydrocodone to white patients than to black patients, whereas female physicians did the reverse. In addition, male physicians treating hypothetical patients presenting with unresponsive lower back pain prescribed twice as much hydrocodone to male patients than to female patients; female physicians did the reverse and prescribed more hydrocodone to female patients than to male patients. Therefore, gender and racial differences were evident only when the role of physician gender was examined, suggesting that male and female physicians may react differently to gender and/or racial cues.
The decision to treat sinusitis, like the decision to prescribe narcotics at all for pain, was not related to patient gender or race. Only the types of antibiotics selected and their duration reflected differences by gender or race. While these results are in accordance with other studies reporting gender and racial differences in the treatment of medical conditions where pain is not the primary complaint,7,9,10 they illustrate that treatment differences observed in one clinical condition do not always mirror the type or direction of differences in another. The finding that treatment bias did not occur in all scenarios and that the differences observed occurred only with regard to the aggressiveness of the regimen selected and not decisions to treat is reassuring.
It is unclear why treatment approaches varied according to the gender of the physician in this study. The reasons for these differences can only be speculative. Physicians may sympathize or identify with patients of the same gender7 or race (in the case of male physicians), or with patients of disadvantaged groups (in the case of female physicians). It is also unclear why physician gender interacted with patient race when treating acute kidney stone pain but with patient gender when treating persistent lower back pain. The differences noted between the prescribing patterns of male and female physicians were unexpected and may be spurious. They warrant further investigation; if confirmed, they could help explain previous reports of less aggressive pain management in women and minorities, at least in studies where male physicians did4 or may have predominated.
In testing whether patient gender and race would influence decisions about pain management, we tried to overcome some of the problems found in previous studies. All physicians in the study read identical vignettes that held symptom presentation, body weight, and disease severity constant in a systematic fashion to minimize the influence of factors that may have accounted for differences in treatment reported in previous studies of gender and race.1–6 Therefore, the findings raise the possibility that treatment disparities may not necessarily be a function of the way patients present their illnesses or interact with physicians.4,12
The limitations of the study are that the sample was one of convenience, moderate in size, and restricted to physicians primarily in the Northeast. In addition, only half of the physicians solicited chose to participate. Therefore, these findings may not be representative of all primary care providers. In addition, we were unable to control for physicians' overall prescribing habits. However, given the manner with which physicians were assigned patient vignettes, and the balance of male and female physicians across the 4 experimental conditions that varied patient gender and race, it is unlikely that patients of a particular gender or race were consistently assigned to physicians with particular prescribing habits.
Future projects would be to study a larger sample of physicians and to include physicians of different ethnic backgrounds. The majority of physicians in the sample were white, so that the impact of physician race could not be ascertained. Future studies could involve an expanded set of different pain scenarios, and they could allow systematic variation of other patient factors such as socioeconomic status or age. The extent to which gender and race influence physician-patient communication also calls for further study, especially given evidence that health care messages are more effective when the educator's race matches that of the audience.16
Although male and female physicians exhibited different treatment patterns in this study, the meaning of these different treatment approaches is difficult to ascertain. More treatment, whether with narcotics for back pain or kidney stone pain or with antibiotics for presumed sinusitis, does not necessarily indicate better care and may, indeed, reflect worse care. Therefore, the clinical significance of the findings is unclear. In addition, whether the results accurately reflect treatment patterns occurring in clinical practice is unknown because this study used vignettes and did not assess physician responses to actual patients. Still, the results of this study raise the possibility that physicians' decisions about pain management are impacted differently by gender and racial cues, a finding that warrants further research, particularly in light of the fact that physician gender has been largely ignored in studies of treatment bias.
Acknowledgments
This project was funded by a Union College Faculty Research Grant. We thank Alan Markus, MD, Rita Rienzo, PA, and Elizabeth Roessler, PA for their assistance in creating the medical vignettes; Matthew Modderno for his help in designing the study; Raquel Mintah for her help in collecting data; and Dan Burns for his useful comments and assistance with the preparation of this article.
APPENDIX
Vignettes and Sample Questions
Kidney Stone
(Name), a 33-year-old 145 lb (race) (gender), presents with a severe right flank pain. The pain started suddenly, is colicky, radiates into her/his right groin, and is unaffected by 3 Advil every 6 hours. (Name) does not have a fever, and her/his bowels are functioning normally. (Name)'s past medical history is unremarkable. On exam, (Name)'s temperature is 98.6°F. She/he is in considerable discomfort, bending forward and slightly to the right side. The exam is otherwise normal. Her/his urine dipstick is highly positive for blood and negative for leukocytes and nitrites. Under the microscope, the spun urine shows TNTC RBCs, 0 to 2 WBCs, and no bacteria. An IVP shows a stone in (name)'s right ureter with no evidence of obstruction. The urologist you consult suggests watchful waiting. During her/his appointment, (Name) makes it clear that she/he does not want to be hospitalized.
Back Pain
(Name), a 38-year-old 157 lb (race) (gender), comes to your office complaining of lower back pain. While working in the yard yesterday, (Name) had lifted a bag of topsoil and had felt sudden severe pain in the lower back. The pain has persisted in spite of taking 3 Advil every 6 hours. (Name) is uncomfortable in all positions and has had trouble sleeping. The pain radiates into the left buttock and posterior left thigh, and s/he has occasional numbness as well in the posterior thigh. (Name)'s bowels and bladder are functioning normally. She/he is otherwise healthy and has no allergies to medications. On exam, (Name) is in obvious pain, is tender to palpation over the left lower lumbar area, and has severe pain in the left back, buttock, and posterior thigh with straight leg raising to 45 degrees. Her/his sensation to touch and pinprick, muscle strength, and reflexes are normal. During her/his appointment, (Name) makes it clear that she/he does not want to be hospitalized.
Sample Pain Treatment Questions
Would you prescribe additional pain medication to (Name)? YES NO
-
If YES:
A) You find that (Name)'s HMO covers only generic Lortab (hydrocodone/acetaminophen). How would your prescription read?
Lortab strength: 2.5/500 5.0/500 7.5/500 10.0/500 (Circle one) Maximum number of pills per day: 1 2 3 4 5 6 7 8 9 10 11 12 Maximum number of days: 1 2 3 4 5 6 Number of refills: 0 1 2 3 B) If (Name) returns to your office prior to completing the original prescription and complains that s/he is not obtaining as much pain relief as s/he had hoped, would you modify your original prescription? YES NO
If YES, how would your revised prescription read? (same options presented as in 2A)
If NO, what course of action would you take:________________________________
Sinus Infection
(Name), a 42-year-old 168 lb (race) (gender), comes to your office because of a bad cold. (Name) has had cold symptoms for the past 4 days. Now, (Name) has developed a thick yellow nasal discharge and pressure over the left cheek. (Name) reports having trouble sleeping because of the congestion, and s/he has not felt relief from Advil or any other pain relievers. (Name) has no other medical problems and is not allergic to medications. On exam, (Name)'s temperature is 100°F, she/he is mildly tender over her/his left cheek, and her/his nostril is full of purulent mucous. The rest of the exam is noncontributory. During her/his appointment, (Name) makes it clear that she/he does not want to be hospitalized.
Sample Sinusitis Treatment Questions
Would you treat (Name) with antibiotics? YES NO
-
If YES:
A) What would you prescribe?
Type of antibiotic: Duration (in days): Number of refills: 0 1 2 3 (Circle one) B) If (Name) returns to your office in 4 days to report that his/her condition is not improved, would you modify your original course of action? Yes No
If NO, what course of action would you take:________________________________
REFERENCES
- 1.Calderone JL. The influence of gender on the frequency of pain and sedative medication administered to postoperative patients. Sex Roles. 1990;23:713–25. [Google Scholar]
- 2.Cleeland CS, Gronin R, Hatfield AK, et al. Pain and its treatment in outpatients with metastatic cancer. N Engl J Med. 1994;330:592–6. doi: 10.1056/NEJM199403033300902. [DOI] [PubMed] [Google Scholar]
- 3.McDonald DD. Gender and ethnic stereotyping and analgesic administration. Res Nurs Health. 1994;17:5–49. doi: 10.1002/nur.4770170107. [DOI] [PubMed] [Google Scholar]
- 4.Knox H, Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;296:1537–9. [PubMed] [Google Scholar]
- 5.Ng B, Dimsdale JE, Rollnik JD, Shapiro H. The effect of ethnicity on prescriptions for patient-controlled analgesia for post-operative pain. Pain. 1996;66:9–12. doi: 10.1016/0304-3959(96)02955-7. [DOI] [PubMed] [Google Scholar]
- 6.Ng B, Dimsdale JE, Shragg GP, Deutsch R. Ethnic differences in analgesic consumption for postoperative pain. Psychosom Med. 1996;58:125–9. doi: 10.1097/00006842-199603000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Lurie N, Slater J, McGovern P, Ekstrum J, Quam L, Margolis K. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993;329:478–82. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]
- 8.Poses RM, Smith WR, Schmitt BP, Alexander-Forti D, Cebul RD, Wigton RS. Do women and men receive different care for sore throats? Motiv Res. 1995;19:193–203. [Google Scholar]
- 9.Burns RB, McCarthy EP, Freund KM, et al. Black women receive less mammography even with similar use of primary care. Ann Intern Med. 1996;125:173–82. doi: 10.7326/0003-4819-125-3-199608010-00002. [DOI] [PubMed] [Google Scholar]
- 10.Sleath B, Svarstad B, Roter D. Patient race and psychotropic prescribing during medical encounters. Patient Educ Couns. 1998;34:227–38. doi: 10.1016/s0738-3991(98)00030-5. [DOI] [PubMed] [Google Scholar]
- 11.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–26. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 12.Elderkin-Thompson V, Waitzkin H. Differences in clinical communication by gender. J Gen Intern Med. 1999;14:112–21. doi: 10.1046/j.1525-1497.1999.00296.x. [DOI] [PubMed] [Google Scholar]
- 13.Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the implicit association test. J Pers Soc Psychol. 1998;74:1464–80. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 14.McDonald DD, Bridge GR. Gender stereotyping and nursing care. Res Nurs Health. 1991;14:373–8. doi: 10.1002/nur.4770140508. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz LM, Woloshin S, Welch HG. Misunderstandings about the effects of race and sex on physicians' referrals for cardiac catheterization. N Engl J Med. 1999;341:279–82. doi: 10.1056/NEJM199907223410411. [DOI] [PubMed] [Google Scholar]
- 16.Kalichman SC, Kelly JA, Hunter TL, Murphy DA, Tyler R. Culturally tailored HIV-AIDS risk-reduction messages targeted to African-American urban women: impact on risk sensitization and risk reduction. J Consulting Clin Psychol. 1993;61:291–5. doi: 10.1037//0022-006x.61.2.291. [DOI] [PubMed] [Google Scholar]