Abstract
BACKGROUND
Controversy exists regarding who should provide care for those with HIV/AIDS. While previous studies have found an association between physician HIV experience and patient outcomes, less is known about the relationship of physician specialty to HIV/AIDS outcomes or quality of care.
OBJECTIVE
To examine the relationship between choice of appropriate antiretroviral therapy (ART) to physician specialty and HIV/AIDS experience.
DESIGN
Self-administered physician survey.
PARTICIPANTS
Random sample of 2,478 internal medicine (IM) and infectious disease (ID) physicians.
MEASUREMENTS
Choice of guideline-recommended ART.
RESULTS
Two patients with HIV disease, differing only by CD4+ count and HIV RNA load, were presented. Respondents were asked whether ART was indicated, and if so, what ART regimen they would choose. Respondents' ART choices were categorized as “recommended” or not by Department of Health and Human Services guidelines. Respondents' HIV/AIDS experience was categorized as moderate to high (MOD/HI) or none to low (NO/LO). For Case 1, 72.9% of responding physicians chose recommended ART. Recommended ART was more likely (P < .01) to be chosen by ID physicians (88.2%) than by IM physicians (57.1%). Physicians with MOD/HI experience were also more likely (P < .01) to choose recommended ART than those with NO/LO experience. Finally, choice of ART was examined using logistic regression: specialty and HIV experience were found to be independent predictors of choosing recommended ART (for ID physicians, odds ratio [OR], 4.66; 95% confidence interval [95% CI], 3.15 to 6.90; and for MOD/HI experience, OR, 2.05; 95% CI, 1.33 to 3.16). Results for Case 2 were similar. When the analysis was repeated excluding physicians who indicated they would refer the HIV “patient,” specialty and HIV experience were not significant predictors of choosing recommended ART.
CONCLUSIONS
Guideline-recommended ART appears to be less likely to be chosen by generalists and physicians with less HIV/AIDS experience, although many of these physicians report they would refer these patients in clinical practice. These results lend support to current recommendations for routine expert consultant input in the management of those with HIV/AIDS.
Keywords: HIV/AIDS, physician specialty, antiretroviral therapy
Over the past 4 years, the standard of care and outcomes of care for HIV/AIDS have changed dramatically.1–3 Potent 3- or 4-drug combination antiretroviral regimens have resulted in substantial increases in CD4+ cell counts and suppression of HIV plasma viral load in treated individuals. There is also growing evidence from randomized clinical trials that use of these combination antiretroviral regimens results in improved clinical outcomes for those living with HIV/AIDS.4–6 Use of these regimens also appears to have been the major factor contributing to recent reductions in morbidity and mortality due to HIV/AIDS in the United States.1,7
Evidence from both clinical trials and observational studies have demonstrated the clear benefit of this therapy, and recent guidelines have outlined its appropriate indications and use.2,3,8,9 Given the complexity of these regimens and the rapid pace at which antiretroviral management is evolving, current guidelines suggest that these medications should “generally be prescribed only by physicians with extensive experience in the management of HIV/AIDS, and when this is not possible, such expertise should be accessed through consultation.”3 This recommendation reflects a long-standing, but growing, debate regarding the role of generalists and physicians with little experience in the care of HIV/AIDS patients.
Previous research in this area found that hospitals and physicians with more HIV experience provide better HIV/AIDS care, evidenced by lower inpatient mortality and increased survival.10–15 While physicians with more HIV experience probably provide better HIV care, little is known about the specific processes of care that result in these better outcomes.16 Controversy also exists about the relative competence of generalists compared with specialists in infectious diseases to provide HIV/AIDS care; yet, there is little data to inform this debate.17 Since the advent of highly active antiretroviral therapy (HAART) for HIV/AIDS, appropriate treatment with these medications is felt to be among the most important factors affecting patients' outcomes. Appropriate prescribing of these medications, therefore, is a key indicator of HIV quality of care.
In the present study, our goal was to examine antiretroviral therapy (ART) choices of general internal medicine (IM) physicians and infectious disease (ID) subspecialists, and to examine whether these choices conform to current guideline recommendations.2,3,8,9 Physicians in this study were presented standardized cases of asymptomatic HIV/AIDS patients in a self-administered survey. Our objective was to examine whether physician respondents were aware that ART therapy was indicated for 2 of these hypothetical patients, and to examine their ability to choose an appropriate antiretroviral regimen, consistent with the current guideline recommendations. Using physicians' antiretroviral medication choices for these hypothetical patients, we also sought to examine whether choice of appropriate ART is associated with specialty, HIV experience, or both.
METHODS
Study Population
The study population consisted of ID physicians and IM physicians without subspecialty in 4 states: California, Florida, Massachusetts and New York. We chose these 2 groups of physicians because our primary study question was whether ID subspecialty was as important as HIV experience in antiretroviral prescribing and how the ART choices of generalists compared with ID subspecialists. We chose these 4 states because of their high prevalence of HIV/AIDS and their geographic diversity.7
Physicians were identified from a list of names, addresses, and self-reported specialties obtained from the American Medical Association's (AMA) Master File, which includes members and nonmembers of the AMA. We selected a random sample of 2,478 physicians, stratified according to state and specialty. The sample was comprised of 1,000 ID physicians and 1,478 IM physicians from California, Florida, Massachusetts, and New York. The ID sample size within each state was proportional to the total number of ID physicians in the state, and the number of IM physicians chosen was 1.5 times the number of ID physicians in each state's sample.
Survey Instrument
A study survey instrument was developed which presented 3 standardized cases of patients with asymptomatic HIV disease, who differed only by CD4 count and HIV RNA load. For each case, respondents were asked what level of care they would provide were they to see this patient in their clinical practice. Possible responses were to assume all the patient's care; provide primary care, but refer for HIV-specific care; provide HIV-specific care, but refer for primary care; and refer for all care. Respondents were then asked to indicate whether ART was indicated, and if so, what specific ART regimen they would prescribe. Respondents could check whichever medications they would use from a list comprised of all Food and Drug Administration-approved antiretroviral medications.
In the current report, we present results only for Cases 1 and 2, those for which ART is indicated based on the Department of Health and Human Services (DHHS) and International AIDS Society (IAS)-USA guidelines released in 1997.2,3,8,9 These 2 cases are shown in the Appendix. They are identical, except Case 1 is more advanced, with a CD4 count of 330 and HIV RNA of 250,000 copies/mL; Case 2 has a CD4 count of 460 and HIV RNA of 50,000 copies/mL. Respondents were also asked to rate the likelihood of various clinical outcomes for each case if the patient were to receive treatment with 1 of 2 ART regimens or no treatment. The results of this analysis and Case 3 are presented elsewhere.18 The survey also asked respondents for their professional and demographic characteristics.
Data Collection and Response Rate
The study sample consisted of 2,478 physicians: 1,000 ID physicians and 1,478 IM physicians. The self-administered survey was mailed to all physicians in the sample in May 1998. Follow-up mailings were sent to all nonrespondents in June and July 1998, and telephone calls were made to the offices of nonrespondents to further optimize response rate during the 2 weeks prior to and following the third mailing.
A total of 1,233 physicians responded and returned the survey; the overall response rate was 51.8%, with adjustments as listed below. A subset of 96 physicians were removed from the denominator because of an incorrect address. A number of physicians responded but did not complete their survey; therefore, their responses could not be used in the analysis. One hundred six returned the survey, but stated that they never see HIV patients, and 65 did not complete the survey because of serious illness or retirement. Thus, a total of 1,062 surveys were complete and available for analysis; the data from these responses are presented here.
Nonrespondents were compared to respondents by state and specialty, the only characteristics available for nonrespondents. There was no difference in response rate by state (P = .08). However, there was a difference in response rate by specialty (P < .05). Of the 1,417 IM physicians sampled whose addresses were correct, 569 (40.1%) returned a completed survey; compared with to 493 (51.1%) of 965 ID physicians. Of note, these numbers refer only to those respondents who returned a completed survey; those who returned the survey partially completed saying they did not see HIV patients, were too sick, or were retired are not included in these response rates. It had been anticipated that ID physicians might have more interest in this subject and respond at a higher rate. Therefore, more generalists were sampled. Thus, the respondent group consists of more IM physicians (569, 54%) than ID physicians (493, 46%).
Choice of Antiretroviral Therapy
Antiretroviral regimens chosen by responding physicians were categorized according to whether they were “recommended” or not, based on the DHHS and IAS-USA guidelines released in 1997.8,9 Both guidelines, at that time, recommended 2 nucleoside reverse transcriptase inhibitors (nRTIs) and a protease inhibitor (PI) for all HIV/AIDS patients for whom ART is indicated. According to these guidelines, ART therapy was indicated for asymptomatic patients with HIV/AIDS whose CD4 cell count is less than 500 or whose HIV RNA load is greater than 10,000 to 20,000 copies/mL.
STATISTICAL ANALYSIS
Respondents' HIV/AIDS experience was categorized as high, moderate, low, or none, based on the number of HIV patients they reported seeing in their practices currently, and over the course of their career to date. High experience was defined as more than 50 patients now and over career; low experience was defined as 0 to 5 patients now and 1 to 10 over career; moderate experience was defined as levels below high but above low experience. For the bivariate and multiple logistic regression analyses, HIV experience was dichotomized into moderate to high or none to low. Physician practice type was categorized as either hospital-based (which included academic medical centers, municipal, Veteran's Affairs and all other hospital types), private practice, or other (which consisted primarily of HMOs and community health centers). Physicians were categorized as an HIV expert or not based on their response to the question: “Do you or others consider you to be an HIV expert?”
Choice of recommended ART was examined for each case overall by calculating frequencies. Univariate analyses were performed for each case, examining the outcome of choice of recommended ART by the physician characteristics of specialty, HIV experience, gender, race/ethnicity, age, practice type, and state. These analyses utilized χ2or Fisher's exact test for categorical variables and the t test for continuous variables. To examine the relative importance of specialty compared to HIV experience in relation to choice of recommended therapy, stratified analyses of ART choice by HIV experience level and physician specialty were performed. Multiple logistic regression was performed examining the outcome of choice of recommended ART, while simultaneously controlling for physician specialty, HIV experience, gender, race/ethnicity, age, and practice type. State was not included in the logistic regression models because the rates of choice of recommended ART for Cases 1 and 2 were nearly identical across the 4 states. All analyses were conducted using SAS statistical software.19
RESULTS
Characteristics of Physician Respondents
The characteristics of responding physicians, stratified by specialty are presented in Table 1. Their gender, age and racial/ethnic distributions are generally consistent with those of U.S. physicians overall.20 The majority of respondents were IM physicians (53.6%); 46.4% were ID physicians. There were no statistical differences in respondent demographic characteristics by specialty. However, there were differences in professional characteristics by specialty; ID physicians had more HIV experience, and were more likely to be an HIV expert and hospital-based.
Table 1.
Physician Respondents N = 1,062
| Characteristic | Internal Medicine n (%) | Infectious Disease n(%) |
|---|---|---|
| Overall | 569 (53.6) | 493 (46.4) |
| Gender | ||
| Male | 410 (75.4) | 349 (73.2) |
| Female | 134 (24.6) | 128 (26.8) |
| Race/ethnicity | ||
| White | 370 (68.8) | 378 (80.1) |
| African American | 24 (4.5) | 11 (2.3) |
| Latino | 24 (4.5) | 24 (5.1) |
| Other | 120 (22.3) | 59 (12.5) |
| Practice type | ||
| Private practice | 233 (43.4) | 145 (30.3) |
| Hospital-based | 165 (30.7) | 258 (53.9) |
| Other | 139 (25.9) | 76 (15.9) |
| Location | ||
| New York | 207 (36.4) | 172 (34.9) |
| California | 178 (31.3) | 160 (32.5) |
| Massachusetts | 114 (20.0) | 90 (18.3) |
| Florida | 70 (12.3) | 71 (14.4) |
| HIV experience level | ||
| None | 31 (5.6) | 4 (0.8) |
| Low | 183 (32.9) | 11 (2.9) |
| Moderate | 308 (55.3) | 193 (40.0) |
| High | 35 (6.3) | 275 (56.9) |
| HIV expert | ||
| No | 520 (93.2) | 84 (17.5) |
| Yes | 38 (6.8) | 395 (82.5) |
| Age if | ||
| <45 | 319 (56.1) | 278 (56.4) |
| ≥45 | 250 (43.9) | 215 (43.6) |
Choice of Recommended Antiretroviral Therapy
In response to Case 1, which was the hypothetical patient who had more advanced HIV disease, 52.5% of responding physicians stated that they would manage this patient's HIV disease by themselves, while 47.5% stated they would refer the patient to another physician for management of the HIV disease. Of all responding physicians, 72.9% chose ART which conformed to the recommendations of the guidelines. Physicians who would assume care of the patient's HIV disease in clinical practice were significantly more likely to choose recommended ART (87.6%), compared with those who stated they would refer the patient for HIV care (52.5%). Table 2 summarizes choice of recommended ART. Both physician specialty and physician HIV experience were found to be significantly related to choice of recommended ART; ID physicians were more likely to choose recommended ART, and the percentage of physicians choosing recommended ART increased with increasing level of HIV experience. When the analysis was restricted to physicians who indicated that they would assume care of the patient's HIV disease (and those who would refer were excluded), neither of these physician characteristics was significantly associated with choice of recommended ART.
Table 2.
Case 1: Physician Characteristics
| All Respondents n(%) | P Value | Would Not Refer*n(%) | P Value | |
|---|---|---|---|---|
| Overall | 671 (72.9) | 468 (87.6) | ||
| Gender | .12 | .55 | ||
| Male | 481 (71.7) | 330 (86.8) | ||
| Female | 177 (77.0) | 126 (89.4) | ||
| Race/ethnicity | .19 | .62 | ||
| White | 484 (74.5) | 339 (88.3) | ||
| African American | 21 (61.8) | 17 (85.0) | ||
| Latino | 34 (77.3) | 27 (90.0) | ||
| Other | 112 (68.7) | 67 (83.4) | ||
| Specialty | .001 | .08 | ||
| Internal medicine | 261 (57.1) | 96 (82.8) | ||
| Infectious disease | 410 (88.2) | 372 (89.0) | ||
| HIV experience | .001 | .12 | ||
| None | 2 (18.2) | 0 (0) | ||
| Low | 62 (46.3) | 4 (66.7) | ||
| Moderate | 331 (72.1) | 193 (86.2) | ||
| High | 270 (87.7) | 267 (89.3) | ||
| Practice type | .14 | .94 | ||
| Hospital-based | 307 (76.4) | 221 (88.1) | ||
| Private practice | 223 (70.1) | 155 (88.1) | ||
| Other | 130 (71.4) | 85 (86.7) | ||
| Location | .72 | .59 | ||
| New York | 248 (73.6) | 171 (89.1) | ||
| California | 211 (70.6) | 153 (85.5) | ||
| Massachusetts | 121 (75.2) | 76 (90.5) | ||
| Florida | 91 (73.4) | 68 (86.1) | ||
| Age,y | .20 | .13 | ||
| <45 | 399 (74.4) | 285 (89.1) | ||
| ≥45 | 272 (70.6) | 183 (85.5) |
Excludes physicians who stated that they would refer the patient to another physician for management of HIV/AIDS.
In response to Case 2, 52.2% of responding physicians stated that they would manage this patient's HIV disease by themselves; 47.8% stated they would refer the patient to another physician for management of the HIV disease. Of all responding physicians, 63.6% chose recommended ART for Case 2. Physicians who would assume care of the patient's HIV disease in clinical practice were significantly more likely to choose recommended ART (80.4%), compared with those who stated they would refer the patient for HIV care (40.8%). Choice of recommended ART is presented in Table 3. Again, ID physicians and those with more HIV experience were found to be significantly more likely to choose recommended ART (P = .001). When the analysis was restricted to physicians who would assume HIV care (and those who would refer were excluded), the magnitude of the differences by HIV experience and specialty decreased. However, ID physicians remained significantly more likely (P = .007) to choose recommended ART than generalists. In addition, physicians whose practices were hospital-based were also more likely to choose recommended therapy than physicians in other types of practices.
Table 3.
Case 2: Physician Characteristics
| n(%) | P Value | Would Not Refer*n(%) | P Value | |
|---|---|---|---|---|
| Overall | 605 (63.6) | 440 (80.4) | ||
| Gender | .35 | .46 | ||
| Male | 435 (63.1) | 309 (79.4) | ||
| Female | 157 (66.5) | 119 (82.6) | ||
| Race/ethnicity | .22 | .14 | ||
| White | 439 (65.7) | 322 (81.7) | ||
| African American | 22 (64.7) | 18 (90.0) | ||
| Latino | 30 (66.7) | 26 (83.8) | ||
| Other | 96 (57.1) | 58 (71.6) | ||
| Specialty | .001 | .007 | ||
| Internal medicine | 216 (45.1) | 90 (72.0) | ||
| Infectious diseases | 389 (82.4) | 350 (82.9) | ||
| HIV experience | .0001 | .06 | ||
| None | 2 (15.4) | 0 (0) | ||
| Low | 49 (32.7) | 4 (57.1) | ||
| Moderate | 295 (63.3) | 185 (79.4) | ||
| High | 253 (81.9) | 246 (82.3) | ||
| Practice type | .001 | .07 | ||
| Hospital-based | 284 (70.3) | 216 (84.7) | ||
| Private practice | 190 (56.9) | 143 (77.7) | ||
| Other | 118 (63.4) | 75 (75.8) | ||
| Location | .42 | .84 | ||
| New York | 214 (61.5) | 156 (79.6) | ||
| California | 190 (62.3) | 142 (80.7) | ||
| Massachusetts | 114 (67.9) | 76 (83.5) | ||
| Florida | 87 (66.9) | 66 (78.6) | ||
| Age if | .49 | .06 | ||
| <45 | 356 (64.6) | 271 (83.1) | ||
| ≥45 | 249 (62.3) | 169 (76.5) |
Excludes physicians who stated that they would refer the patient to another physician for management of HIV/AIDS.
Stratified and Multivariate Analyses of Choice of Recommended Antiretroviral Therapy
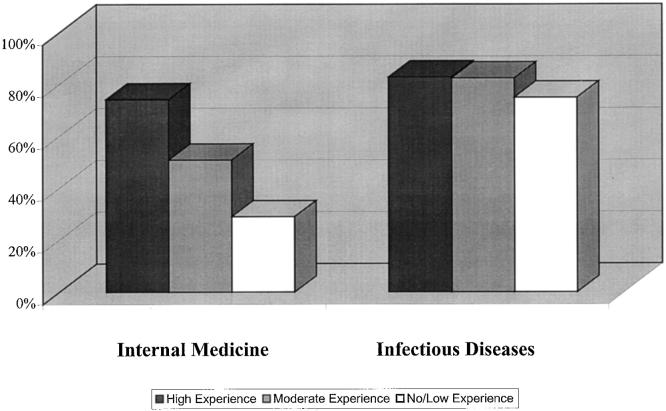
To examine the importance of physician specialty compared with HIV experience in relation to choice of recommended therapy, ART choice was examined by HIV experience level, stratified by specialty. These results are displayed for Case 1 in Figure 1 and for Case 2 in Figure 2. These analyses demonstrated that ID physicians were likely to choose recommended therapy than IM physicians at each HIV experience level for both cases (P < .05). Of note, the data for physicians with no or low experience are grouped because of the small number of ID physicians with no HIV experience.
FIGURE 1.
Recommended antiretroviral regimen chosen, stratified by specialty and HIV experience (Case 1).
FIGURE 2.
Recommended antiretroviral regimen chosen, stratified by specialty and HIV experience (Case 2).
To further examine the relative importance of physician specialty compared with HIV experience, a multiple logistic regression model examining the outcome of choice of recommended ART for Case 1 was performed which adjusted for gender, race/ethnicity, age, and type of practice, in addition to specialty and HIV experience. This model found that, of the variables examined, only physician specialty and HIV experience were significantly related to choice of recommended ART. Infectious disease physicians were significantly more likely to choose recommended ART than IM physicians, with an odds ratio (OR) of 4.66 (95% confidence interval [CI], 3.15 to 6.90); and physicians with moderate or high HIV experience were also significantly more likely to choose recommended ART than were those with no or low HIV experience, with an OR of 2.05 (95% CI, 1.33 to 3.16). A multiple logistic regression model was also performed examining the outcome of choice of recommended ART for Case 2 as well, using the same variables; the results were quite similar in direction and magnitude. The results of the regression models for both cases are presented in Table 4. Finally, the same logistic regression was repeated for both of the cases, restricting the analysis to those who would assume the “patient's” HIV care (excluding those who would refer). Physician specialty, experience, and all other physician characteristic were not significantly related to choice of recommended ART in these final models.
Table 4.
Results of Multiple Logistic Regression*
| Odds Ratio | 95% Confidence Interval | |
|---|---|---|
| Case 1 | ||
| Specialty (ID vs IM) | 4.66 | 3.15 to 6.90 |
| HIV experience (mod/high vs no/low) | 2.05 | 1.33 to 3.16 |
| Case 2 | ||
| Specialty (ID vs IM) | 4.43 | 3.12 to 6.31 |
| HIV experience (mod/high vs no/low) | 2.29 | 1.49 to 3.53 |
Recommended antiretroviral therapy chosen. Adjusted for race, gender, age, and type of practice.
DISCUSSION
This study examined choice of ART for HIV/AIDS patients among physicians in 4 states and found that general IM physicians were significantly less likely than ID physicians to choose ART that is consistent with recommendations in current guidelines.2,3,8,9 In addition, physicians with little or no previous HIV experience were also significantly less likely to choose ART consistent with current guidelines. Importantly, however, many generalists and those with less HIV experience indicated that they would have referred the patients to another physician for management of HIV. In fact, when the analysis was restricted to only those who would have managed patients with HIV themselves, smaller differences were seen in choices of appropriate medications by physician specialty and experience. These findings regarding knowledge of appropriate ART for HIV are important because it is widely acknowledged that use of this standard of care has led to substantial decreases in HIV-related morbidity and mortality due to HIV/AIDS in the United States.1,7 In addition, our findings with regard to planned referral of HIV patients by many generalists are also important, because they may serve to decrease concern about the consequences of their lower knowledge of current HIV care on the quality of care they provide.
Given how recently these guidelines have been released, it may be premature to characterize these apparent prescribing differentials by specialty and HIV experience as quality of care differences. It may be that the antiretroviral choices of general IM physicians and those with less HIV experience reflect slower adoption of antiretroviral guidelines by these physicians, not ongoing quality of care differentials. This phenomenon has been described by others regarding provision of HIV/AIDS care.21,22 One might also hypothesize that some of these physicians who did not choose recommended regimens may have chosen regimens categorized as “alternative” by the 1997 guidelines, which were 3 drug regimens containing nevirapine or saquinavir hard gel caps.8,9 Actually, choice of these “alternatives” by respondents was uncommon (6.0% for Case 1 and 4.7% for Case 2), and was significantly higher among ID physicians and those with more HIV/AIDS experience. It should be noted that the 1997 guidelines were the first to recommend triple regimens using 2 nRTIs and 1 PI for initial ART for all patients who meet criteria for treatment. While the specifics of the triple regimens have changed in subsequent guidelines,2 the changes have been subtle. Thus, physicians' ability to choose ART consistent with these recommendations remains relevant to current antiretroviral prescribing and HIV care.
The question of whether generalists are as knowledgeable and provide comparable care to specialists has generated a considerable amount of interest and research in recent years. The results of studies examining this question in several other important diseases seem to suggest that the situation is actually quite complex, regardless of whether knowledge, use of efficacious treatments, or outcomes are being examined. While several previous studies of medical treatments have found that specialists are more knowledgeable about the use of effective medical treatments,23–25 others have found that generalists' knowledge and use of these treatments is equal to or better than that of relevant specialists.25–27 The results of studies that have examined outcomes of care have been similarly mixed. The Medical Outcomes Study followed a large cohort of patients with hypertension and diabetes and found no differences in survival or quality of life among those cared for by specialists compared with those cared for by generalists.28 However, studies of the inpatient care of those with acute myocardial infarction29 and stroke30 found they had lower mortality when the admitting physicians were specialists (cardiologists and neurologists, respectively). In summary, these data examining the care provided for other important diseases suggest that specialists at times use optimal management options more than generalists, and sometimes they do not.
Few previous studies have examined the knowledge, outcomes of care, or use of indicated treatments by generalist physicians in the care of HIV/AIDS patients.10,16,31–33 More than a decade ago Northfelt and colleagues argued that HIV disease was becoming a “primary care disease.”34 Their view was that HIV was a common chronic disease like hypertension and diabetes, and would be seen in primary care settings. They further stated that primary care physicians should, therefore, be prepared to manage HIV and required certain basic HIV-related clinical skills. Briefly, these included skills in HIV testing and counseling, skills in HIV treatment and prophylaxis to prevent opportunistic infections, and skills in recognizing and managing key HIV-related clinical problems. Recently, Hecht et al. reviewed and summarized the available evidence regarding generalists' HIV-related knowledge, processes of care, and outcomes of care.17 They assert that there is growing evidence that many primary care physicians have weaknesses in each of the areas of importance delineated by Northfelt. Specifically, there is evidence that primary care physicians do not routinely screen their patients for HIV35 and may not have skills to adequately assess HIV risk and decide when screening is indicated.36 Also, there is evidence that many primary care physicians cannot recognize and diagnose Pneumocystis carinii pneumonia33 or recognize and provide care for other HIV-related problems.31 Importantly, however, the vast majority of previous studies comparing HIV/AIDS care or knowledge of generalists to specialists have focused on physician HIV experience as the key indicator of HIV expertise, not specialty. This may be in part because there is controversy about the relevant subspecialty for AIDS care, i.e., whether ID specialists have a unique role as the relevant specialists in the care of HIV/AIDS patients.17 However, based on the results presented here, it appears that the effect of specialty on HIV prescribing may be greater than the effect of HIV experience. These results provide further evidence that primary care physicians have weaknesses in the key areas of importance delineated by Northfelt, specifically, prescribing current ART.
Several recent reviews and editorials have tackled the controversy regarding whether HIV/AIDS is still a disease that can be cared for effectively by primary care physicians.17,37,38 In fact, based on the data presented here, generalists in several high HIV prevalence states may not be prepared to provide state-of-the art care for those with HIV/AIDS. However, this study provides important new insights regarding generalists and HIV care. First, it should be emphasized that the generalists with moderate to high HIV experience in this study had high levels of knowledge and apparent “prescribing practices” which were in line with current standards, and essentially equivalent to those of the ID physicians in the study. Additionally, based on these results, it appears that physicians, including generalists and those with less HIV experience, who would choose to prescribe antiretrovirals are prepared to do so. Similarly, at least in this study, those who need to seek consultative input about HIV care also appear to be aware of their need to seek such input. The recommendation that primary care physicians obtain consultative input from an HIV expert when caring for HIV/AIDS patients is articulated quite clearly in the current DHHS guidelines3 and has been echoed by others.17,37 This study provides new evidence that this recommendation is indeed appropriate.
This study has several important limitations. The results reported here are based on physicians' responses to hypothetical cases only and, thus, may not be reflective of actual antiretroviral prescribing in clinical practice. This study is also somewhat limited by response rate; only slightly more than 50% of eligible physicians responded, and there was a differential response rate by specialty, with ID physicians significantly more likely to respond than IM physicians. Therefore, it is possible that our results may be influenced by response bias. We hypothesize, however, that respondents in both specialties generally tend to be more interested in the survey subject than nonrespondents and, therefore, are probably more knowledgeable. Thus, any difference detected in knowledge by specialty and other key characteristics may have been more pronounced if the response rate had been higher.
In summary, this study reconfirms the importance of HIV/AIDS experience in physicians' effectiveness in the management of patients with HIV/AIDS. The results reported here suggest that appropriate antiretroviral prescribing is strongly related to physician HIV/AIDS experience. These data build on prior research showing that survival, utilization, and use of key preventive services are related to physician HIV/AIDS experience.10,15,32 In addition, these data demonstrate that as of mid-1998, ID physicians appear to be more likely than general IM physicians to provide ART which meets the current standard of care, based on recent guidelines. However, it appears that many physicians who are less knowledgeable about HIV/AIDS are aware of their lack of knowledge and would seek help from colleagues with expertise in HIV/AIDS when caring for these patients. These results lend support to the recommendation that primary care physicians obtain expert consultative input when caring for HIV/AIDS patients, but suggest that these physicians are able to gauge their own HIV competency and determine when there is a need for consultation.
Acknowledgments
This work was supported by a Generalist Physician Faculty Scholar Award from the Robert Wood Johnson Foundation and a grant from Agouron Pharmaceuticals, Inc.
The authors wish to acknowledge the data management and statistical analysis assistance provided by Corey Duefield, M.P.H. and Lucy Hanna, MS, MAT. They also would like to express appreciation to the numerous physicians who took the time to complete the study survey.
Appendix
Case 1
The patient a is 34-year-old white man who was recently found to be HIV infected. The patient is feeling well and offers no complaints. His past medical history is unremarkable. Family history is not significant for any major morbidity. In terms of social history, the patient denies any history of injection drug use; believes he acquired HIV through previous sexual contact. The patient denies smoking or excessive alcohol drinking; he was born and grew up in the U.S. The patient's vital signs and physical exam are essentially normal. A CBC and chemistry profile including liver enzymes were done and all the values are within normal limits. Initial CD4 count and HIV RNA viral load were done one week ago.
Initial CD4 count was 330 cells/ml
Initial HIV RNA viral load was 250,000 copies/ml (Amplicor assay)
The patient is concerned about the potential worsening of the disease, and deferring the management plan to you.
Case 2
The patient is a 34-year-old white man who was recently found to be HIV infected. The patient is feeling well and offers no complaints. His past medical history is unremarkable. Family history is not significant for any major morbidity. In terms of social history, the patient denies any history of injection drug use; believes he acquired HIV through previous sexual contact. The patient denies smoking or excessive alcohol drinking; he was born and grew up in the U.S. The patient's vital signs and physical exam are essentially normal. A CBC and chemistry profile including liver enzymes were done and all the values are within normal limits. Initial CD4 count and HIV RNA viral load were done one week ago.
Initial CD4 count was 460 cells/ml
Initial HIV RNA viral load was 50,000 copies/ml (Amplicor assay)
The patient is concerned about the potential worsening of the disease, and deferring the management plan to you.
REFERENCES
- 1.Palella FJ, Delaney, Moorman AC, et al. Declining morbidity and mortality among patients with advanced HIV infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–60. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 2.Carpenter CC, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1998: Updated recommendations of the International AIDS Society-USA Panel. JAMA. 1998;280:78–86. doi: 10.1001/jama.280.1.78. [DOI] [PubMed] [Google Scholar]
- 3.Guidelines for the use of antiretroviral agents in HIV-infected adults and adolescents. Department of Health and Human Services and Henry J. Kaiser Family Foundation. MMWR Morb Mortal Wkly Rep. 1998;47:43–82. [PubMed] [Google Scholar]
- 4.Hammer SM, Squires KE, Hughes MD, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337:725–33. doi: 10.1056/NEJM199709113371101. [DOI] [PubMed] [Google Scholar]
- 5.Cameron B, Heath-Chiozzi M, Kravcik S, Mills R, Potoff A, Henry D. Program and Abstracts of the 3rd Conference on Retroviruses and Opportunistic Infections. Washington, DC: Foundation for Retrovirology and Human Health; 1996. Prolongation of life and prevention of AIDS in advanced HIV immunodeficiency with ritonavir. [Google Scholar]
- 6.Montaner JS, Riess P, Cooper D, et al. A randomized, double-blind trial comparing combinations of nevirapine, didanosine, and zidovudine for HIV-infected patients: the INCAS trial. Italy, The Netherlands, Canada and Australia Study. JAMA. 1998;279:930–7. doi: 10.1001/jama.279.12.930. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report 1998: U.S. HIV and AIDS Cases Reported through December 1999. Vol. 9. 2000. pp. 5–44. [Google Scholar]
- 8.Fauci AS, Bartlett JG and the Panel on Clinical Practices for Treatment of HIV Infection. Panel on Clinical Practices for Treatment of HIV Infection. Guidelines for the Use of Antiretroviral Agents in HIV-infected Adults and Adolescents. Department of Health and Human Services. Office of Public Health and Science 1997. Federal Register Doc 97-16228. [Google Scholar]
- 9.Carpenter CCJ, Fischl MA, Hammer SM, et al. Antiretroviral therapy for HIV infection in 1997. Updated Recommendations of the International AIDS Society-USA Panel. JAMA 1997. 277:1962–9. [PubMed] [Google Scholar]
- 10.Kitahata MM, Koepsell TD, Deyo RA, Maxwell CL, Dodge WT, Wagner EH. Physicians' experience with the acquired immunodeficiency syndrome as a factor in patients' survival. N Engl J Med. 1996;334:701–6. doi: 10.1056/NEJM199603143341106. [DOI] [PubMed] [Google Scholar]
- 11.Stone VE, Seage GR, Hertz T, Epstein AM. The relation between hospital experience and mortality for patients with AIDS. JAMA. 1992;268:2655–61. [PubMed] [Google Scholar]
- 12.Shapiro MF, Greenfield S. Experience and outcomes in AIDS. JAMA. 1992;268:2698–9. [PubMed] [Google Scholar]
- 13.Cotton DJ. Improving survival in acquired immunodeficiency syndrome: is experience everything? JAMA. 1989;261:3016–7. [PubMed] [Google Scholar]
- 14.Markson LE, Houchens R, Fanning TR, Turner BJ. Repeated emergency department use by HIV-infected persons: effect of clinic accessibility and expertise in HIV care. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;17:3541. doi: 10.1097/00042560-199801010-00005. [DOI] [PubMed] [Google Scholar]
- 15.Brosgart CL, Mitchell TF, Coleman RL, Dyner T, Stephenson KE, Abrams DI. Clinical experience and choice of drug therapy for human immunodeficiency viral disease. Clin Infect Dis. 1999;28:14–22. doi: 10.1086/515081. [DOI] [PubMed] [Google Scholar]
- 16.Bach PB, Calhoun EA, Bennett CL. The relation between physician experience and patterns of care for patients with AIDS-related Pneumocystis carinii pneumonia: results from a survey of 1,500 physicians in the United States. Chest. 1999;115:1563–9. doi: 10.1378/chest.115.6.1563. [DOI] [PubMed] [Google Scholar]
- 17.Hecht FM, Wilson IB, Wu AW, Cook RL, Turner BJ. Optimizing care for persons with HIV infection. Society of General Internal Medicine AIDS Task Force. Ann Intern Med. 1999;131:136–43. doi: 10.7326/0003-4819-131-2-199907200-00011. [DOI] [PubMed] [Google Scholar]
- 18.Mansourati FF, Stone VE, Mayer KH, Duefield CA, Poses RM. The relation of HIV/AIDS practice variations to physicians' judgements regarding antiretroviral therapy. J Gen Intern Med. 1999;14(suppl 2):108. [Google Scholar]
- 19.SAS/STAT User's Guide: Version 7. Fifth Edition. Cary, NC: SAS Institute; 1997. [Google Scholar]
- 20.Bureau of Health Professions. Seventh Report to the President and Congress on the Status of Health Personnel in the United States. Washington, DC: National Academy Press; 1996. [Google Scholar]
- 21.Kitahata MM, Van Rompaey SE, Shields AW. Physician experience in the care of HIV-infected persons is associated with earlier adoption of new antiretroviral therapy. J Acquir Immune Defic Syndr. 2000;24:106–14. doi: 10.1097/00126334-200006010-00004. [DOI] [PubMed] [Google Scholar]
- 22.Markson LE, Cosler LE, Turner BJ. Implications of generalists' slow adoption of zidovudine in clinical practice. Arch Intern Med. 1994;154:1497–504. [PubMed] [Google Scholar]
- 23.Ayanian JZ, Hauptman PJ, Guadagnoli E, Antman EM, Pashos CL, McNeil BJ. Knowledge and practices of generalist and specialist physicians regarding drug therapy for acute myocardial infarction. N Engl J Med. 1994;331:1136–42. doi: 10.1056/NEJM199410273311707. [DOI] [PubMed] [Google Scholar]
- 24.Chin MH, Friedmann PD, Cassel CK, Lang RM. Differences in generalist and specialist physicians' knowledge and use of angiotensin-converting enzyme inhibitors for congestive heart failure. J Gen Intern Med. 1997;12:523–30. doi: 10.1046/j.1525-1497.1997.07105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ayanian JZ, Guadagnoli E, McNeil BJ, Cleary PD. Treatment and outcomes of acute myocardial infarction among patients of cardiologists and generalist physicians. Arch Intern Med. 1997;157:2570–6. [PubMed] [Google Scholar]
- 26.Chin MH, Wang JC, Zhang JX, Lang RM. Differences among geriatricians, general internists, and cardiologists in the care of patients with heart failure: a cautionary tale of quality assessment. J Am Geriatr Soc. 1998;46:1349–54. doi: 10.1111/j.1532-5415.1998.tb06000.x. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein LB, Bonito AJ, Matchar DB, Duncan PW, Samsa GP. US National Survey of Physician Practices for the Secondary and Tertiary Prevention of Ischemic Stroke. Medical therapy in patients with carotid artery stenosis. Stroke. 1996;27:1473–8. doi: 10.1161/01.str.27.9.1473. [DOI] [PubMed] [Google Scholar]
- 28.Greenfield S, Rogers W, Mangotich M, Carney MF, Tarlov AR. Outcomes of patients with hypertension and non-insulin dependent diabetes mellitus treated by different systems and different specialities. Results from the Medical Outcomes Study. JAMA. 1995;274:1436–44. [PubMed] [Google Scholar]
- 29.Jollis JG, DeLong ER, Peterson ED, et al. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N Engl J Med. 1996;335:1880–7. doi: 10.1056/NEJM199612193352505. [DOI] [PubMed] [Google Scholar]
- 30.Mitchell JB, Ballard DJ, Whisnant JP, Ammering CJ, Samsa GP, Matchar DB. What role do neurologists play in determining the costs and outcomes of stroke patients? Stroke. 1996;27:1937–43. doi: 10.1161/01.str.27.11.1937. [DOI] [PubMed] [Google Scholar]
- 31.Paauw DS, Wenrich MD, Curtis JR, Carline JD, Ramsey PG. Ability of primary care physicians to recognize physical findings associated with HIV infection. JAMA. 1995;274:1380–2. [PubMed] [Google Scholar]
- 32.Turner BJ, McKee L, Fanning T, Markson LE. AIDS specialist versus generalist ambulatory care for advanced HIV infection and impact on hospital use. Med Care. 1994;32:902–16. doi: 10.1097/00005650-199409000-00002. [DOI] [PubMed] [Google Scholar]
- 33.Curtis JR, Paauw DS, Wenrich MD, Carline JD, Ramsey PG. Ability of primary care physicians to diagnose and manage Pneumocystis carinii pneumonia. J Gen Intern Med. 1995;10:395–9. doi: 10.1007/BF02599841. [DOI] [PubMed] [Google Scholar]
- 34.Northfelt DW, Hayward RA, Shapiro MF. The acquired immunodeficiency syndrome is a primary care disease. Ann Intern Med. 1988;109:7735. doi: 10.7326/0003-4819-109-10-773. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. HIV prevention practices of primary-care physicians-United States, 1992. JAMA. 1994;271:261–2. [PubMed] [Google Scholar]
- 36.Wenrich MD, Curtis JR, Carline JD, Paauw DS, Ramsey PG. HIV risk screening in the primary care setting: Assessment of physician skills. J Gen Intern Med. 1997;12:107–13. doi: 10.1046/j.1525-1497.1997.00015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robbins GK. Time for a new paradigm-optimal management of patients with human immunodeficiency virus infection and AIDS. Clin Infect Dis. 1999;28:23–5. doi: 10.1086/515082. [DOI] [PubMed] [Google Scholar]
- 38.Stone VE. Generalists providing antiretroviral therapy for patients with HIV/AIDS: Have the rules changed? SGIM Forum. 1998 21,6–8. [Google Scholar]