Abstract
CONTEXT
There is agreement that warfarin decreases stroke risk in patients with atrial fibrillation (AF), but prior studies suggest that warfarin is markedly underused, for unclear reasons.
OBJECTIVE
To determine if warfarin is underused in the treatment of patients with atrial fibrillation.
DESIGN
Cross-sectional.
SETTING
Tertiary care VA hospital.
PATIENTS
All patients with a hospital or outpatient diagnosis of AF between 10/1/95 and 5/31/98.
DATA COLLECTION
One or more physician investigators reviewed pertinent records for each patient. When any of the 3 investigators thought warfarin might be indicated, the patient's primary care provider completed a survey regarding why warfarin was not used.
RESULTS
Of 1,289 AF patients, 844 (65%) had filled at least 1 warfarin prescription. Of the 445 remaining, 19 had died, 5 had inadequate medical records, and 54 received warfarin elsewhere, leaving 367 patients. Of these, 160 had no documented AF, 53 had only a history of AF, and 49 had only transient AF. Of the remaining 105 patients, 17 refused warfarin therapy and 72 had documented contraindications to warfarin use including bleeding risk or history, fall risk, alcohol abuse, or other compliance problems. The reasons for not using warfarin among the 16 patients remaining included provider oversight (n = 4) and various reasons suggesting provider knowledge deficits.
CONCLUSION
In contrast to prior studies that suggested that warfarin is markedly underused, we found that few patients with AF and no contraindication to anticoagulation were not receiving warfarin. We believe that differing study methodologies, including the use of physician review and provider survey, may explain our markedly different rate of warfarin underutilization, although local institutional factors cannot be excluded. The findings suggest that primary providers may be far more compliant with the standard of care for patients with atrial fibrillation than previously believed.
Keywords: warfarin, atrial fibrillation, quality of care, physician practice
Atrial fibrillation (AF) is a common arrhythmia estimated to affect as many as 2.2 million Americans.1 It is particularly common in the elderly, affecting 5% of persons 65 years of age or older.1,2 The annual stroke risk for patients with AF not receiving anticoagulants is approximately 5%.3 Up to 15% of ischemic strokes are associated with atrial fibrillation.4
A combined analysis of 5 separate randomized controlled trials published since 1989 demonstrated that warfarin reduces ischemic stroke risk in patients with AF by approximately two thirds.5 Aspirin has also been shown to reduce the risk of ischemic stroke in these patients, but clearly to a lesser extent than warfarin.5 National consensus groups have concluded that in the absence of contraindications, all patients with atrial fibrillation should receive warfarin with the exception of those at low risk for stroke.6
Despite the strong evidence of benefit, a number of studies have indicated that 21% to 67% of patients with AF who appear to be appropriate candidates for warfarin do not receive it.7–25 Most estimates are in excess of 40%, including a recently published study of a national sample of inpatients conducted as part of the Medicare peer review program.26 This pattern is seen in inpatients,7–14 outpatients,15–24 and patients in long-term care settings.25 It is also seen in patients with prior stroke, a particularly high-risk group.14 Although warfarin therapy carries a risk of bleeding complications, these high rates of warfarin underutilization persist after excluding persons with contraindications to anticoagulation. In several studies of hospitalized patients with AF, over half of patients without apparent contraindications to anticoagulants were not receiving warfarin.8–10,13 Among studies examining practice patterns in the outpatient setting, rates of nonuse are similarly high.15–24 These findings have caused the Health Care Financing Administration (HCFA) to include AF as 1 of only 6 clinical conditions targeted for quality improvement in its current contracts with the Peer Review Organizations that are charged with overseeing the quality of care received by Medicare beneficiaries.
The reasons for these low rates of warfarin use are not clearly understood.27 Unfortunately, the studies that have identified this underuse have not conducted detailed investigations into the reasons warfarin is underutilized. Surveys of physicians' attitudes toward warfarin use in AF have suggested that the most important factors predicting warfarin use in theoretical scenarios are physicians' estimates of embolization risk and bleeding risk.28,29 Additionally, physicians are less likely to say they would anticoagulate a theoretical patient when the patient is older. Unfortunately, responses on surveys may not correspond to actual practice patterns, and the physician's intent to anticoagulate is only one part of the decision to use warfarin. Therefore, we carried out this study to determine the rate of warfarin underutilization at our institution and to comprehensively examine why warfarin is not being used.
METHODS
We identified our study population using the computerized records of the Pittsburgh Veterans Administration Healthcare System (PVAHCS), a tertiary referral VA hospital. We included all patients with a hospital or clinic visit International Classification of Diseases, Ninth Revision (ICD-9) diagnosis code for atrial fibrillation between October 1, 1995 and May 31, 1998. To ensure that our study population had updated medical records, we required that patients had been seen at least once for medical care at the PVAHCS after July 1st, 1997 and that they be alive as of July 1st, 1999. Patients were excluded from chart review if they had ever received warfarin after September 1995, according to computerized pharmacy records maintained by the PVAHCS.
One physician investigator (SDW) reviewed the electronic medical records of each subject not known to have received warfarin, focusing on 3 data elements. First, information was collected about the timing and duration of the episodes of atrial fibrillation. Patients were classified as having no clear evidence of atrial fibrillation, a history of atrial fibrillation only (diagnosed in the past with no episodes while receiving care at the PVAHCS), transient nonrecurrent atrial fibrillation (1 or a few brief episodes of AF since beginning care at the PVAHCS), chronic paroxysmal (multiple episodes of AF that either continued to occur or were sufficiently prolonged that we believed anticoagulation was indicated) or continuous atrial fibrillation. Second, the reviewer identified current warfarin use not captured by the computerized VA pharmacy system. Although most patients received their medications from the PVAHCS pharmacy, a small number of study patients used other VA pharmacies or received their warfarin from a provider outside the VA system.
Finally, the investigator recorded contraindications to warfarin use and other reasons for not treating with warfarin, such as patient refusal to use warfarin or terminal illness. The contraindications included a history of prior bleeding episodes or high risk of bleeding, previous falls or high fall risk, active alcohol abuse, patient noncompliance with medical therapy, end-stage liver disease, dialysis-dependent renal disease, and persistent uncontrolled blood pressure (BP) (defined as systolic BP over 180mm/hg or diastolic BP over 100mm/hg).
If the initial reviewer identified chronic paroxysmal or persistent atrial fibrillation with no clearly documented contraindication or reason for warfarin nonuse and could not find evidence warfarin was being used, a second investigator independently reviewed that patient's complete medical record (electronic and paper chart). This second reviewer once again assessed the diagnosis and time course of the atrial fibrillation, any use of warfarin, and any contraindications to warfarin therapy. This assessment was reviewed with the primary reviewer. If both agreed that warfarin was clearly contraindicated, the reason was recorded. For each remaining patient, all 3 investigators collectively reviewed key elements of the medical record in order to come to a consensus on the patient's candidacy for warfarin. If all agreed that a patient was not a candidate for anticoagulation, the reason for that determination was recorded. When at least 1 investigator believed that the patient was a potential candidate for warfarin, the patient's primary provider was asked to complete a confidential 1-page survey to determine his/her reasons for withholding warfarin. All providers signed a consent form prior to completing this survey. We followed up all nonresponders in person or by telephone.
We reviewed the completed provider surveys to classify the reasons provided for warfarin nonuse. Electronic and paper medical records were re-evaluated concurrently to search for documentation supporting these reasons. The 3 physician-investigators then made a global assessment of the patient's candidacy for warfarin using both the medical record and the provider surveys. Differences among the investigators were resolved by consensus.
Because many of the commonly cited contraindications to warfarin use are relative contraindications, we reviewed definitions used in the current HCFA-sponsored national quality improvement project directed at this issue. We noted that the HCFA definitions were formulated to give the provider the benefit of the doubt in cases of warfarin nonuse by using a very liberal definition of each contraindication. For example, a documented history of bright red blood per rectum or guaiac-positive stools would be considered a contraindication even if subsequent evaluation had demonstrated hemorrhoids. Since we utilized a physician review process, we intentionally left room for subjective judgement about contraindications to ensure that we did not exclude patients from further review who had “soft” contraindications to warfarin use (e.g., GI bleeding evidenced only by a guaiac-positive stool). Similarly, if a nursing note documented a fall risk, the primary reviewer sought confirmation of multiple previous falls and/or gait abnormalities prior to determining that warfarin was contraindicated. However, if the treating provider specifically documented that a contraindication on our list was the reason for withholding warfarin, we accepted that contraindication as long as the condition persisted and could be confirmed by chart review to be clinically significant.
The primary chart review data collection instrument was used in parallel by 2 reviewers for the first 50 cases, with clarification of the definition of each data element when necessary. As a check of the abstraction process, the second investigator performed a complete electronic record review of a random 10% of cases (based on the last digit of the social security number) to determine if there were any cases for which he would have asked for a second review when the primary reviewer had not. In 2 cases, the second reviewer would have classified warfarin as contraindicated without the need for further review, while the primary reviewer had requested dual review. In no cases did the second reviewer request the review of a case that the primary reviewer had not. Thus, we believe the primary reviewer was successful in identifying all cases that needed dual review in which a contraindication to warfarin was not clearly present or the duration and frequency of the atrial fibrillation was not apparent.
RESULTS
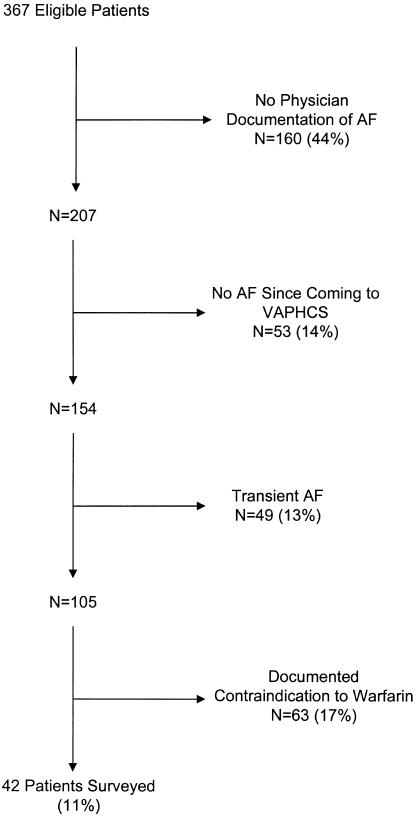
We identified 1,289 patients with an ICD-9 diagnosis code for atrial fibrillation for an inpatient stay or outpatient visit between October 1, 1995 and May 31, 1998 who had received medical care at the PVAHCS after July 1, 1997. Of these, 844 (65%) had received at least 1 warfarin prescription according to VA pharmacy records and were excluded from further analysis. We excluded 24 patients because they were deceased as of June 1st, 1998 (n = 19) or because we could not identify adequate medical records to classify them (n = 5). This left 421 patients. They were primarily male (98%), white (91%) and older (mean age 72.6 years). Chart review revealed that 54 (12.8%) of these patients were receiving warfarin from other sources. The reasons for not using warfarin for the remaining 367 patients are categorized in Figure 1. One hundred sixty subjects (44%) had no documented episodes of atrial fibrillation. Many of these had provider notes indicating the presence of an irregular rhythm or supraventricular tachycardia, but evaluation of electrocardiograms and other data confirmed that atrial fibrillation had not been present. In 53 cases (14%), atrial fibrillation had been documented prior to coming to the PVAHCS, but there was no evidence of this arrythmia while the patients were being cared for at our institution. Finally, 49 subjects (13%) had transient and nonrecurring atrial fibrillation during their care at the VA.
FIGURE 1.
Reasons for warfarin nonuse among 367 living veterans with adequate records, an ICD-9 diagnosis of AF, and no evidence of warfarin use in the preceding 5 years.
Of the remaining 105 patients, 63 had reasons documented in the medical record for why warfarin was not used. The most common reasons were patient refusal to use warfarin (24%), high fall risk (24%), and bleeding (32%). Several patients had more than 1 contraindication to warfarin. A summary of these results is found in Table 1. This left 42 patients with atrial fibrillation who appeared to be reasonable candidates for anticoagulation with warfarin. Primary provider surveys of these patients were completed in 41 cases. The justifications provided for not using warfarin are summarized in Table 2. Extensive review of the medical record of the 1 patient whose provider did not complete a survey chart by the 3 investigators and subsequent telephone discussions with the provider indicated that deferral to an outside physician was the reason warfarin was not used.
Table 1.
Documented Contraindications to Warfarin (N = 63)
| Contraindication | n(%) |
|---|---|
| Prior bleeding episodes/bleeding risk | 20 (32) |
| Fall risk/frequent fall | 15 (24) |
| Patient refusal | 15 (24) |
| Patient noncompliance | 5 (8) |
| Alcohol abuse | 6 (10) |
| Terminal illness | 2 (3) |
Table 2.
Provider Rationale for Warfarin Nonuse (N = 42)
| Reviewer Consensus on Rationale | ||
|---|---|---|
| Provider's Stated Rationale | Valid (n = 26) | Invalid (n = 16) |
| Bleeding risk or history | 6 | 1 |
| Fall risk | 4 | 3 |
| Alcohol abuse | 3 | 0 |
| Transient nature of AF | 8 | 1 |
| Noncompliance | 4 | 0 |
| History of AF only | 2 | 0 |
| Patient refusal | 2 | 0 |
| No survey completed | 0 | 1 |
| Provider oversight* | 0 | 4 |
| Other† | 0 | 6 |
Investigators unanimously assigned provider oversight as reason for nonanticoagulation after review of provider survey and chart.
These include: asymptomatic; no stroke in 18 years on aspirin; not anticoagulated by outside provider (n = 2); rate controlled on digoxin; age, he will be 81 soon.
Valid reasons for warfarin nonuse total more than 26 because some patients had more than one reason for nonuse. AF, atrial fibrillation.
In 26 of 42 patients, the reviewers unanimously agreed with the provider's decision to withhold anticoagulation. For the 16 remaining patients (including the one without a written survey), at least 1 investigator disagreed with the reason the provider gave for warfarin nonuse. These reasons included asymptomatic atrial fibrillation, old age in an 80-year-old patient, and fall risk in a person without documented evidence of falls or significant gait instability. An additional reason offered by providers was resolution of the arrhythmia when our review of the medical record suggested that atrial fibrillation was probably still present. We categorized this as “provider oversight” (Table 2).
Thus, of 445 patients receiving care at the PVAHCS with an ICD-9 diagnosis of atrial fibrillation and no pharmacy record of warfarin use, only 16 (3.6%) were not being treated with warfarin and were judged to be reasonable candidates for anticoagulation. Moreover, among 207 patients who had adequate medical records, medical record documentation of atrial fibrillation, and no warfarin use, 191 (92.3%) appeared to have good reason for not being treated with warfarin.
DISCUSSION
In contrast to multiple previous studies conducted in diverse settings, we found that only a very small fraction of patients with AF without contraindication to anticoagulant therapy were not treated with warfarin. One previous study, performed in an outpatient setting, found a substantially lower rate of inappropriate warfarin nonuse than most other studies.18 In that study, performed in an academically affiliated staff model HMO, Gottlieb et al. found that 21.2% of eligible patients were not receiving warfarin, although 28% of those had been offered it. However, other authors have reported higher rates of warfarin nonuse in outpatient populations. A study of more than 11,000 persons enrolled in a California HMO demonstrated that only 55% of persons without known contraindications were receiving warfarin.22 Similarly, multiple studies of hospitalized patients have found fewer than 60% of eligible patients receive warfarin.26
Why do our findings differ so markedly from those of previous studies examining the question of warfarin use among patients with atrial fibrillation? There are several plausible explanations, which can be divided into 2 broad categories. First, the difference in the prevalence of warfarin underuse between our study and prior studies may be due to differences in anticoagulation practices between the PVAHCS and the sites previously studied. Alternately, it may be that anticoagulation practices are similar in the PVAHCS and elsewhere, but our methods were sufficiently different to give rise to these markedly different results. We explore both sets of reasons below.
It is plausible that the PVAHCS is unusually successful at achieving high levels of warfarin use. Overall, 65% of patients with an ICD-9 diagnosis of atrial fibrillation had been treated at least briefly with warfarin as an outpatient. This percentage is higher than many prior studies have estimated, even though those studies excluded persons with contraindications to warfarin and those in whom a diagnosis of AF could not be confirmed. There are several reasons why the PVAHCS might be unusually successful at achieving high rates of warfarin use. First, a highly effective anticoagulation clinic is present in the PVAHCS. Once a provider at our institution decides to use warfarin, this anticoagulation clinic takes full responsibility for patient education, warfarin dose adjustment, and follow-up of the International Normalized Ratio. The provider no longer needs to be concerned about the management of warfarin dosing and follow-up. Other investigators have hypothesized that such clinics might be effective methods to increase warfarin use.29,30 Second, it may be easier for patients at our institution to comply with warfarin therapy. Most patients pay little or nothing for their medications. Although warfarin is an inexpensive drug, there are likely fewer financial barriers to care for patients at VA medical centers. Additionally, providers at our institution may be particularly up to date about atrial fibrillation and its treatment. The academic environment at the PVAHCS provides ample opportunity for providers to learn how to effectively treat patients with atrial fibrillation. Furthermore, because of the demographics of the patient population, a large percentage of patients have atrial fibrillation, which gives providers greater experience with this arrhythmia. Finally, because we analyzed data from a recent period, the differences in warfarin use may reflect temporal trends toward increasing use of warfarin, although a recent analysis of data from the National Ambulatory Medical Care Surveys suggests that rates stopped rising after 1996.23
Although these factors may explain some of the observed difference, we believe it is more likely that the difference in prevalence of warfarin underutilization between our study and previous studies reflects the unique strengths of our methods. Whereas most prior studies examining this question have used trained nurses or medical records personnel to conduct the chart review, we used physician review. We postulate that use of physician reviewers decreases the apparent rate of warfarin underuse by identifying important reasons for withholding warfarin that require physician judgment. For example, the use of physician reviewers allowed us to supplement and broaden the standard explicit chart review process, with subjective, yet medically educated, judgment about whether relative contraindications were sufficiently important to justify not using warfarin for individual patients. Similarly, we could judge whether episodes of AF that were transient and infrequent warranted the use of warfarin, and whether AF that was raised as a diagnostic possibility was eventually confirmed, even if no explicit statement was made. It is notable that the previously cited study by Gottlieb et al. also relied on physician chart review, as did the study of inpatients that had the lowest rate (36%) of inappropriate warfarin nonuse.7 In this latter study, physician review found that warfarin nonuse was justified in 54 of 96 cases (56%) that were classified as inappropriate after explicit standard chart review. Although other studies mention physician review, this sometimes reflects review of an abstract of data from the record, rather than the record itself.17
Prior studies evaluating the use of warfarin among patients with atrial fibrillation have been carried out on a cohort of either inpatients or outpatients. These studies were performed by examining the records either from a single hospitalization or from a limited time period of outpatient care. For most of these studies, treatment with warfarin was implicitly defined as “treatment at one point in time” and relied on a limited set of medical records typically not including ambulatory pharmacy records. In contrast, we reviewed electronic records that included multiple outpatient visits and ambulatory pharmacy records, as well as inpatient discharge summaries. For those patients whose electronic records did not provide a reason for warfarin nonuse, we conducted a detailed review of the paper chart before surveying the primary care provider (PCP). This extensive review process, which in many cases involved a review of several years of medical records, allowed us to identify all contraindications that the PCP or other providers had documented. It also allowed us to confirm that warfarin use was ongoing in those patients who appeared to be receiving this therapy. Moreover, since many of the PCPs in the PVAHCS are either trainees or supervisors of trainees, the level of detail of the medical record documentation is probably greater than is seen in most medical records maintained by private sector physicians.
Finally, we gave primary providers an opportunity to provide information about contraindications to warfarin that were not apparent from our initial review of the medical record. Although only a small percentage of providers were surveyed, this process may have been enough to explain some of the difference between our results and those of Gottlieb et al. We found that in most cases where chart review did not reveal a clear contraindication to warfarin use, the PCP could provide a compelling rationale for nonuse.
We should acknowledge the limitations of the present study. First, this is a single-center study. As noted above, it is possible that practice patterns at the PVAHCS are very atypical. It is a tertiary care, university-affiliated facility caring for a seriously ill population. A healthier population would be less likely to have contraindications to using warfarin. However, aside from the anticoagulation clinic, there is little reason to think that practice patterns at the PVAHCS differ from those in other tertiary care academic settings.
Second, the internal validity of the study could be limited by several factors. A physician who was aware of the senior investigator's prior finding that physician review often uncovered reasons for inappropriate warfarin nonuse carried out the initial data collection.7 The potential for bias is exaggerated by the subjective nature of data collection, specifically the judgments made regarding the appropriateness of warfarin. However, a certain degree of physician judgement is unavoidable in assessing the presence of contraindications. Since we were aware of the potential for bias, the primary reviewer referred cases for secondary review whenever there was any question that warfarin might be appropriate. This led to our performing dual review of 20% of charts. Re-review of a random 10% sample of cases by a second investigator did not uncover any cases that the second reviewer would have referred for further discussion, when the primary reviewer had not. We note that in the majority of cases where a PCP was surveyed, the reason for nonuse of warfarin provided by the PCP was one that had been noted during physician chart review, but at least 1 investigator was unconvinced that it was justification for withholding warfarin. This suggests that our attempts to bias the study toward including people with relative contraindications successfully kept marginal cases from being prematurely classified as poor warfarin candidates and ensured that few patients were misclassified as appropriate nonusers of warfarin.
We also acknowledge that we only studied some of the patients with atrial fibrillation treated at the PVAHCS. First, we only reviewed patients with an ICD-9 diagnosis of atrial fibrillation. Although it is possible that this method missed some patients with AF, all prior studies of warfarin use utilized a similar mechanism to identify patients with this arrythmia. Additionally, we did not review the medical records of any of the 844 patients with an ICD-9 code for AF whose pharmacy records showed they had received warfarin, even if warfarin therapy had been discontinued. We believe that these patients were less likely to be inappropriately not treated with warfarin than the patients we included in our study. Had we examined the records for these 844 patients, the rates we found of inappropriate nonuse of warfarin could have been different, perhaps even lower.
Finally, we should note that we only reviewed warfarin underuse. We did not examine the adequacy or appropriateness of treatment with warfarin in those patients receiving this therapy. Treatment with warfarin clearly is not the same as adequate treatment with warfarin. The question of how adequately warfarin is used by patients with atrial fibrillation is an important one and a matter of ongoing study. Moreover, we did not review the prevalence of inappropriate treatment with warfarin. An analysis of inappropriate treatment among study patients receiving warfarin might well have suggested that providers at our institution are too aggressive in their warfarin use.
Because of the very low rates of inappropriate nonuse we found, we had limited ability to address one of the questions that motivated the study—why providers don't anticoagulate patients with clearly documented atrial fibrillation who are good candidates for this effective drug. Nonetheless, we can provide some guidance based on the 16 patients who appear to have been missed at our institution. In these patients, the reasons for nonuse commonly reflected knowledge deficits on the part of providers (adequate rate control, lack of symptoms, and old age in an 80-year-old were each cited at least once). Additionally, in a few cases, the presence of a regular rhythm based either on complete heart block with electronic ventricular pacing or a native slow ventricular response caused the provider to believe that atrial fibrillation was not present. These causes suggest that both physician education and systematic interventions, such as routine communication of the presence of AF to primary providers, may be of some benefit in improving utilization of this therapy.
In conclusion, the findings of this study suggest that primary care providers may be far more compliant with the standard of care for patients with atrial fibrillation than previously believed. We believe that this most likely reflects important methodological limitations of prior studies. Although some individual untreated patients may reap considerable benefit if warfarin therapy is instituted, the magnitude of the quality improvement effort focused on increasing warfarin use may be disproportionate to the need. Nonetheless, although fewer than 8% of individuals with definite atrial fibrillation had never received warfarin and had no apparent reason for the omission, the high prevalence of AF and the magnitude of the benefit of anticoagulation still warrant attention to this problem. Our results provide guidance to those who are seeking to develop mechanisms to determine if warfarin is used when appropriate.
REFERENCES
- 1.Feinberg WM, Blackshear JL, Laupacis A, Kronmal R, Hart RG. Prevalence, age distribution, and gender of patients with atrial fibrillation. Analysis and implications. Arch Intern Med. 1995;155:469–73. [PubMed] [Google Scholar]
- 2.Furberg CD, Psaty BM, Manolio TA, Gardin JM, Smith VE, Rautaharju PM. Prevalence of atrial fibrillation in elderly subjects (the Cardiovascular Health Study). Am J Cardiol. 1994;74:236–41. doi: 10.1016/0002-9149(94)90363-8. [DOI] [PubMed] [Google Scholar]
- 3.Wheeldon NM. Atrial fibrillation and anticoagulant therapy. Eur Heart J. 1995;16:302–12. doi: 10.1093/oxfordjournals.eurheartj.a060911. [DOI] [PubMed] [Google Scholar]
- 4.Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch Intern Med. 1987;147:1561–4. [PubMed] [Google Scholar]
- 5.Atrial Fibrillation Investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Analysis of pooled data from five randomized controlled trials. Arch Intern Med. 1994;154:1449–57. [PubMed] [Google Scholar]
- 6.Laupacis A, Albers G, Dalen J, Dunn MI, Jacobson AK, Singer DE. Antithrombotic therapy in atrial fibrillation. Chest. 1998;114:579S–89S. doi: 10.1378/chest.114.5_supplement.579s. [DOI] [PubMed] [Google Scholar]
- 7.Whittle J, Wickenheiser L, Venditti LN. Is warfarin underused in the treatment of elderly persons with atrial fibrillation? Arch Intern Med. 1997;157:441–5. [PubMed] [Google Scholar]
- 8.Albers GW, Yim JM, Belew KM, et al. Status of antithrombotic therapy for patients with atrial fibrillation in university hospitals. Arch Intern Med. 1996;156:2311–6. [PubMed] [Google Scholar]
- 9.Brass LM, Krumholz HM, Scinto JM, Radford M. Warfarin use among patients with atrial fibrillation. Stroke. 1997;28:2382–9. doi: 10.1161/01.str.28.12.2382. [DOI] [PubMed] [Google Scholar]
- 10.Lip GY, Tean KN, Dunn FG. Treatment of atrial fibrillation in a district general hospital. Br Heart J. 1994;71:92–5. doi: 10.1136/hrt.71.1.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bath PM, Prasad A, Brown MM, MacGregor GA. Survey of use of anticoagulation in patients with atrial fibrillation. BMJ. 1993;307:1045. doi: 10.1136/bmj.307.6911.1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lok NS, Lau CP. Presentation and management of patients admitted with atrial fibrillation: a review of 291 cases in a regional hospital. Internat J Cardiol. 1995;48:271–8. doi: 10.1016/0167-5273(94)02259-l. [DOI] [PubMed] [Google Scholar]
- 13.Munschauer FE, Priore RL, Hens M, Castilone A. Thromboembolism prophylaxis in chronic atrial fibrillation. Practice patterns in community and tertiary-care hospitals. Stroke. 1997;28:72–6. doi: 10.1161/01.str.28.1.72. [DOI] [PubMed] [Google Scholar]
- 14.Brass LM, Krumholz HM, Scinto JD, Mathur D, Radford M. Warfarin use following ischemic stroke among Medicare patients with atrial fibrillation. Arch Intern Med. 1998;158:2093–100. doi: 10.1001/archinte.158.19.2093. [DOI] [PubMed] [Google Scholar]
- 15.Sudlow M, Thomson R, Thwaites B, Rodgers H, Kenny RA. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet. 1998;352:1167–71. doi: 10.1016/S0140-6736(98)01401-9. [DOI] [PubMed] [Google Scholar]
- 16.Mendelson G, Aronow WS. Underutilization of warfarin in older persons with chronic nonvalvular atrial fibrillation at high risk for developing stroke. J Am Geriatr Soc. 1998;46:1423–4. doi: 10.1111/j.1532-5415.1998.tb06011.x. [DOI] [PubMed] [Google Scholar]
- 17.Antani MR, Beyth RJ, Covinsky KE, et al. Failure to prescribe warfarin to patients with nonrheumatic atrial fibrillation. J Gen Intern Med. 1996;11:713–20. doi: 10.1007/BF02598984. [DOI] [PubMed] [Google Scholar]
- 18.Gottlieb LK, Salem-Schatz S. Anticoagulation in atrial fibrillation. Does efficacy in clinical trials translate into effectiveness in practice? Arch Intern Med. 1994;154:1945–53. doi: 10.1001/archinte.154.17.1945. [DOI] [PubMed] [Google Scholar]
- 19.Samsa GP, Matchar DB, Goldstein LB, et al. Quality of anticoagulation management among patients with atrial fibrillation: results of a review of medical records from 2 communities. Arch Intern Med. 2000;160:967–73. doi: 10.1001/archinte.160.7.967. [DOI] [PubMed] [Google Scholar]
- 20.White RH, McBurnie MA, Manolio T, et al. Oral anticoagulation in patients with atrial fibrillation: adherence with guidelines in an elderly cohort. Am J Med. 1999;106:165–71. doi: 10.1016/s0002-9343(98)00389-1. [DOI] [PubMed] [Google Scholar]
- 21.Smith NL, Psaty BM, Furberg CD, et al. Temporal trends in the use of anticoagulants among older adults with atrial fibrillation. Arch Intern Med. 1999;159:1574–8. doi: 10.1001/archinte.159.14.1574. [DOI] [PubMed] [Google Scholar]
- 22.Go AS, Hylek EM, Borowsky LH, Phillips KA, Selby JV, Singer DE. Warfarin use among ambulatory patients with nonvalvular atrial fibrillation: the anticoagulation and risk factors in atrial fibrillation (ATRIA) study. Ann Intern Med. 1999;131:927–34. doi: 10.7326/0003-4819-131-12-199912210-00004. [DOI] [PubMed] [Google Scholar]
- 23.Stafford RS, Singer DE. Recent national patterns of warfarin use in atrial fibrillation. Circulation. 1998;97:1231–3. doi: 10.1161/01.cir.97.13.1231. [DOI] [PubMed] [Google Scholar]
- 24.Stafford RS, Singer DE. National patterns of warfarin use in atrial fibrillation. Arch Intern Med. 1996;156:2537–41. [PubMed] [Google Scholar]
- 25.Gurwitz JH, Monette J, Rochon PA, Eckler MA, Avorn J. Atrial fibrillation and stroke prevention with warfarin in the long-term care setting. Arch Intern Med. 1997;157:978–84. [PubMed] [Google Scholar]
- 26.Jencks SF, Cuerdon T, Burwen DR, et al. Quality of medical care delivered to Medicare beneficiaries: A profile at state and national levels. JAMA. 2000;284:1670–6. doi: 10.1001/jama.284.13.1670. [DOI] [PubMed] [Google Scholar]
- 27.Bungard TJ, Ghali WA, Teo KK, McAlister FA, Tsuyuki RT. Why do patients with atrial fibrillation not receive warfarin? Arch Intern Med. 2000;160:41–6. doi: 10.1001/archinte.160.1.41. [DOI] [PubMed] [Google Scholar]
- 28.McCrory DC, Matchar DB, Samsa G, Sanders LL, Pritchett EL. Physician attitudes about anticoagulation for nonvalvular atrial fibrillation in the elderly. Arch Intern Med. 1995;155:277–81. [PubMed] [Google Scholar]
- 29.Monette J, Gurwitz JH, Rochon PA, Avorn J. Physician attitudes concerning warfarin for stroke prevention in atrial fibrillation: results of a survey of long-term care practitioners. J Am Geriatr Soc. 1997;45:1060–5. doi: 10.1111/j.1532-5415.1997.tb05967.x. [DOI] [PubMed] [Google Scholar]
- 30.Kutner M, Nixon G, Silverstone F. Physicians' attitudes toward oral anticoagulants and antiplatelet agents for stroke prevention in elderly patients with atrial fibrillation. Arch Intern Med. 1991;151:1950–3. [PubMed] [Google Scholar]