Abstract
To examine the requirements of the human respiratory syncytial virus (HRSV) SH (small hydrophobic), G (attachment), and F (fusion) proteins for virus infectivity and morphology, we used the prototype A2 strain of HRSV to generate a series of cDNAs from which (i) the SH open reading frame (ORF), (ii) the SH and G ORFs, or (iii) the SH, G, and F ORFs were deleted. Each deleted ORF was replaced as follows: the SH ORF was replaced with that of green fluorescent protein; the G ORF was replaced with that of Gvsv, a chimeric glycoprotein consisting of the vesicular stomatitis Indiana virus (VSIV) G protein ecto- and transmembrane domains coupled to the HRSV F cytoplasmic tail; and the F ORF was replaced with that of marker protein β-glucuronidase. The number of genes and the intergenic junctions in the constructs were kept as found in A2 virus in order to maintain authentic levels of transcription. Infectious viruses were recovered from all three engineered cDNAs and designated RSΔsh, RSΔsh,g/Gvsv, and RSΔsh,g,f/Gvsv, respectively. Low-pH-induced syncytium formation was observed in cells infected with viruses RSΔSH,G/Gvsv and RSΔSH,G,F/Gvsv, indicating that Gvsv was expressed and functional. Neutralization of infectivity by anti-VSIV G antibodies and inhibition of entry by ammonium chloride showed that RSΔSH,G,F/Gvsv infectivity was mediated by Gvsv and that an acidification step was required for entry into the host cell, similar to VSIV virions. All three engineered viruses displayed growth kinetics and virus yields similar to a wild-type A2 virus, both in Vero and HEp-2 cells. Abundant virus-induced filaments were observed at the surface of cells infected with each of the three engineered viruses or with virus A2, indicating that neither the SH and G proteins nor the F protein ecto- and transmembrane domains were required for the formation of these structures. This is the first report of the recovery of an infectious HRSV lacking a fusion protein of the Paramyxoviridae family and of manipulation of the HRSV entry pathway via incorporation of a nonparamyxoviral transmembrane glycoprotein.
Human respiratory syncytial virus (HRSV) is a major cause of severe lower respiratory tract disease in infants and children worldwide as well as in immunosuppressed individuals and the elderly (15, 24, 50). Amidst ongoing efforts to develop HRSV-specific vaccines and therapeutic agents, prevention and treatment of HRSV disease remain a significant challenge. HRSV is the type species of the genus Pneumovirus within the family Paramyxoviridae and contains a negative-sense, single-stranded RNA genome of 15,222 nucleotides that expresses 11 known proteins from 10 genes (10, 30). Three proteins, SH (small hydrophobic), G (attachment), and F (fusion), have been characterized as transmembrane glycoproteins and are detected in purified virions (1, 29). On the surface of infected cells, the G and F proteins concentrate in cell-associated, virus-induced filamentous structures with variable lengths of up to 10 μm (3, 7, 22, 52, 57).
The SH protein is a small integral membrane protein of unknown function, with a relatively low amino acid conservation among HRSV strains (11, 12). Previous studies indicate that SH is dispensable for HRSV growth in cell culture, and its absence has little impact on the ability of the virus to replicate in the respiratory tracts of mice and chimpanzees (8, 35, 62, 72).
The G gene of HRSV expresses both a type II membrane-anchored glycoprotein and a soluble protein (28, 52, 68, 69). G protein is heavily O-glycosylated and shows significant structural similarities to mucinous proteins (68, 69). The G protein was initially characterized as providing an attachment function (37), and domains in G have since been identified that bind to sulfated glycosaminoglycans on the cell surface in vitro (20, 42). The requirement for G protein in infectivity in cell culture varies depending on the cell type. Both a cold-adapted virus in which most of the sequence encoding the SH and G proteins is absent and an engineered virus lacking the G gene replicate efficiently in Vero cells. However, replication of these G-deleted viruses is significantly impaired in HEp-2 cells as well as in mice, cotton rats, and humans (35, 64).
The fusion protein, F, is a type I transmembrane glycoprotein that mediates the formation of syncytia typically observed in HRSV-infected cells (67). The F protein is thought to direct entry of HRSV at the plasma membrane in a pH-independent manner (56). Among the transmembrane glycoproteins, F appears to be a critical component for virus transmission, as the F protein, the matrix (M) protein, and the nucleocapsid were found to be the minimal requirements for production of infectious particles, and viruses that express F as the only glycoprotein propagated efficiently in Vero cells (35, 62-64).
The G and F proteins contain the major antigenic epitopes of HRSV, and their roles in the anti-HRSV immune response have been investigated extensively (23, 45, 58, 59, 65, 66, 70). In contrast, relatively few studies have addressed the roles of SH, G, and F in viral entry, assembly, and transmission. In addition to the SH and G deletion studies described above, glycoprotein substitution studies with bovine respiratory syncytial virus (BRSV) showed that the HRSV G and F proteins could functionally replace their homologs in BRSV and that the bovine parainfluenza virus HN and F proteins could functionally replace the BRSV G and F proteins (6, 57). However, to date infectious HRSVs lacking an F gene from the Paramyxoviridae family have not been reported.
In the present work, we investigated whether an infectious HRSV could be generated that was lacking all three homologous transmembrane glycoproteins, SH, G, and F, and whether HRSV infectivity could be mediated by a membrane glycoprotein from outside the Paramyxoviridae family. The G protein of vesicular stomatitis Indiana virus (VSIV) was chosen to functionally replace the HRSV glycoproteins because it contains, in a single polypeptide, the functions for attachment and entry (via a low-pH-dependent endosomal route), and it has been used to pseudotype and mediate transmission of several distantly related viruses (9, 18, 39, 40). However, because VSIV and HRSV use different pathways of entry, successful functional replacement of SH, G, and F with the VSIV G protein depends on the ability of HRSV to adopt an alternate entry mechanism (56). Because cytoplasmic tail domains (CTDs) of viral envelope proteins can be important for incorporation of glycoproteins into virus particles, virus budding and morphology (31, 44, 46, 53, 54, 61), we modified the VSIV G protein by exchanging the nucleotides encoding its predicted CTD with those encoding the HRSV F protein CTD, and termed the resulting chimeric protein Gvsv.
From the prototype HRSV A2 strain, we generated three cDNAs from which the open reading frames (ORFs) of (i) the SH gene, (ii) the SH and G genes, or (iii) the SH, G, and F genes were deleted. The ORF of the SH gene was replaced with that of the green fluorescent protein (GFP), the ORF of the G gene was replaced with that of the chimeric glycoprotein Gvsv, and the ORF of the F gene was replaced with that of marker gene β-glucuronidase (GUS). These engineered constructs thus differed from previously reported deletion viruses in that each deleted gene was replaced, and gene start, intergenic, and gene end sequences throughout the genomes remained unaltered in order to maintain the overall sequential transcriptional control program as found in a wild-type (wt) HRSV. Infectious viruses were recovered from all three cDNAs. These engineered viruses replicated to high titers in both Vero and HEp-2 cells and were used to examine virus entry and morphology in the partial or complete absence of the homologous HRSV transmembrane glycoproteins and presence of heterologous chimeric transmembrane glycoprotein Gvsv.
MATERIALS AND METHODS
Cells, wt virus, and infections.
HEp-2 and Vero 76 (Vero) cells were acquired from the American Type Culture Collection (ATCC). The A2 strain of HRSV was used as a template for generation of cDNAs and as a comparison to the engineered viruses. Virus adsorptions were carried out in standard growth medium containing 5% fetal bovine serum for 1.5 h at 37°C.
Antibodies.
Monoclonal antibody (MAb) 19 was kindly provided by Geraldine Taylor (Institute for Animal Health, Compton, United Kingdom), and MAb L9 was provided by Ed Walsh (University of Rochester School of Medicine and Dentistry, Rochester, N.Y.). The humanized anti-F MAb Synagis was acquired from MedImmune, Inc. The anti-VSIV G and anti-vesicular stomatitis New Jersey virus G (VSNJV G) antibodies were mouse ascitic fluids acquired from the ATCC.
Construction of chimeric protein Gvsv.
A truncated VSIV G ORF (amino acids 1 to 491) flanked by a 3′ XbaI restriction site was generated using PCR. Nucleotides encoding amino acids 553 to 574 of the HRSV F protein (the CTD as predicted by hydrophobicity profiles [MacVector 7.0, Oxford Molecular]) were amplified using PCR creating an XbaI site that overlapped amino acid 553. The engineered XbaI site was used to ligate the two fragments, resulting in chimeric ORF Gvsv (Fig. 1C).
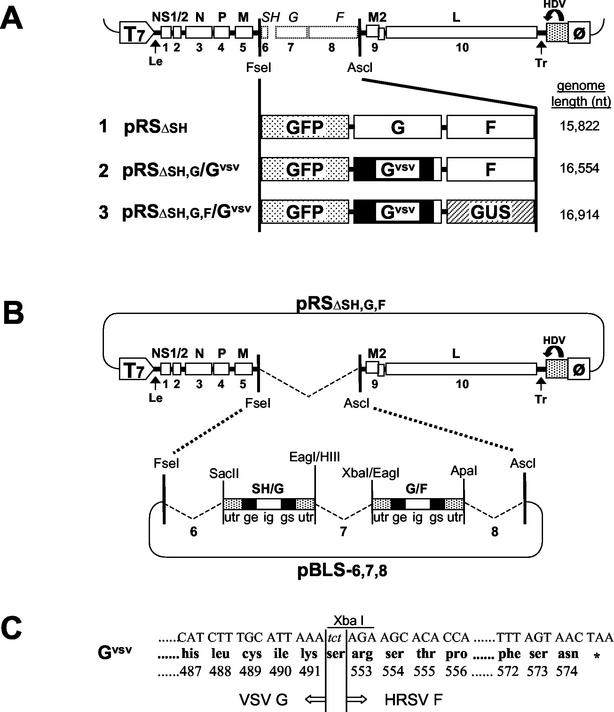
FIG. 1.
Construction and composition of HRSV cDNAs and chimeric membrane glycoprotein Gvsv. (A) Composition of HRSV cDNAs with a modified gene content in genome positions six, seven, and eight: (i) pRSΔsh lacks the SH ORF and contains instead a GFP ORF; (ii) pRSΔsh,g/Gvsv lacks the SH and G ORFs, which are replaced with those encoding GFP and Gvsv, respectively; (iii) pRSΔsh,g,f/Gvsv lacks all three transmembrane glycoprotein ORFs, SH, G, and F, and these were replaced with ORFs encoding GFP, Gvsv, and GUS, respectively. The genomic sequences in these cDNAs are flanked by a T7 promoter (T7) and an HDV self-cleaving ribozyme sequence (HDV) followed by a T7 terminator sequence (ø). In the presence of T7 polymerase, a transcript corresponding to the HRSV antigenome is produced. Numbers 1 to 10 represent the positions of each of the genes relative to the 3′ promoter of the viral genome. Sizes of the engineered viral genomes are indicated on the right in nucleotides (nt). Abbreviations: NS1/2, nonstructural proteins 1 and 2; N, nucleocapsid protein; P, phosphoprotein; M, matrix protein; M2, transcription factor; L, large (polymerase); Le, leader; Tr, trailer. (B) Strategy used for the generation of genetically modified viruses. A plasmid was generated that contained a cDNA of the prototypic HRSV A2 strain from which the SH-G-F region was deleted (pRSΔsh,g,f). A shuttle vector, pBLS-6,7,8, containing introduced restriction sites but in which the gene starts (gs), intergenic regions (ig), and gene ends (ge), as well as untranslated regions (utr) remained unaltered from the A2 virus, was used to place selected ORFs in the sixth, seventh, and eighth genome positions within engineered cDNAs. (C) Gvsv is a chimeric viral membrane glycoprotein consisting of the VSIV G ecto- and transmembrane domains (amino acids 1 to 491) coupled to the CTD of the HRSV F protein (amino acids 553 to 574) via an XbaI site, created by introduction of 3 nt (tct).
Construction of viral cDNAs, recovery and verification of engineered viruses, and production of virus stocks.
A cDNA of the prototype A2 strain of HRSV was generated by reverse transcription (RT)-PCR of HRSV RNAs and cloned into plasmid pBluescript (Stratagene) using conventional cloning techniques. A T7 RNA polymerase promoter followed by three guanosine residues (to enhance transcription) and a T7 RNA polymerase terminator preceded by the hepatitis delta virus (HDV) ribozyme sequence were cloned on either side of the cDNA, such that in the presence of the T7 RNA polymerase, a plus-sense RNA was transcribed (14, 49, 71). This transcript was replicated by the viral polymerase, initiating an authentic viral infection. The above-described HRSV cDNA-containing plasmid was modified by deleting, with the use of PCR, the area from the translation initiation codon of SH to the translation termination codon of F and inserting unique restriction sites (FseI and AscI) in its place (pRSΔsh,g,f in Fig. 1B). A second plasmid vector named pSH/G/F was constructed, containing the exact HRSV genomic region deleted in pRSΔSH,G,F and also flanked by FseI and AscI restriction sites. The three ORFs contained within pSH/G/F were removed and each replaced with a linker containing unique restriction sites, creating construct pBLS-6,7,8 (Fig. 1B). pBLS-6,7,8 thus contained intergenic regions, transcription signals, and 3′ and 5′ untranslated regions that were unaltered from those of virus A2. The indicated glycoprotein and/or marker ORFs were cloned into pBLS-6,7,8, and the resulting shuttle vectors were inserted in the pRSΔSH,G,F backbone via the FseI and AscI sites to generate the final cDNA containing plasmids (Fig. 1A).
Viruses were recovered from the cDNA as follows: HEp-2 cells (0.5 × 106 cells per well), infected with modified vaccinia Ankara-T7 virus (MVA-T7) (73) at a multiplicity of infection of 5 for 1.5 h, were transfected with plasmids containing a modified HRSV cDNA and plasmids encoding each of the proteins required for transcription and replication of viral RNA (nucleocapsid protein [N], phosphoprotein [P], polymerase [L], and transcription factor M2-1), using Lipofectin (Invitrogen) (25). For each transfection, 0.1 μg of cDNA plasmid was used, along with approximately 0.35, 0.2, 0.25, and 0.05 μg, respectively, of plasmids encoding the N, P, M2-1, and L proteins. Cells were incubated at 37°C for 70 h, at which time supernatants were collected and added to fresh Vero cells. After 24 h at 33°C, the supernatant was replaced with fresh medium, and cells were incubated for another 7 days at 33°C. Virus was collected from the supernatants and amplified on Vero cells, and stocks were generated and stored at −80°C. The RNAs of engineered virus stocks between pass 4 and 6 were verified by RT-PCR and sequence analysis across cloning junctions and in modified areas.
Titration of virus stocks.
Virus was adsorbed to cells for 1.5 h at 37°C and then overlaid with 0.5% agar. At 5 days postinfection, 4% formaldehyde in phosphate-buffered saline (PBS) was added to the overlay, and the plates were incubated for 30 min at room temperature. Agar was removed, and the cells fixed for an additional 5 min in methanol. The protocol for visualization of antigens was an adaptation of an existing β-galactosidase detection assay (60). Fixed cells were incubated with either anti-VSIV G antibodies (for viruses RSΔsh,g/Gvsv and RSΔsh,g,f/Gvsv) or anti-F antibodies (for viruses RSΔsh and virus A2), and this was followed by incubation with a β-galactosidase-conjugated goat anti-mouse antibody (Southern Biotechnology Associates, Inc.). After washing with PBS, cells were incubated overnight at 20°C in a solution of 0.5 mM potassium ferricyanide-0.5 mM potassium ferrocyanide-0.1 mM MgSO4-5-bromo-4-chloro-3-indolyl-β-d-galactopyranoside (0.15 mg/ml) in PBS. Samples were washed twice with H2O and dried, and the plaques counted.
RNA analysis.
Vero cells, infected at a multiplicity of infection of 2, were incubated with [3H]uridine (Moravek Biochemicals, Inc.) in the presence of actinomycin D (10 μg/ml), from 16 to 22 h postinfection. Total RNA was isolated using RNeasy columns (Qiagen), and mRNA 3′ poly(A) tails were removed by annealing with oligo(dT) followed by digestion with RNase H (25). RNAs were electrophoresed on 1.75% agarose gels containing 6 M urea and 25 mM citrate and were visualized by fluorography.
Immunofluorescence.
Vero cells were infected at a multiplicity of infection of 2 and fixed at 16 h (for G protein) or 24 h (for proteins Gvsv and F) postinfection with methanol at room temperature. For confocal microscopy, cells were fixed with freshly dissolved 4% paraformaldehyde at 24 h postinfection. Fixed cells were washed, blocked with 2% bovine serum albumin in PBS, and incubated with anti-F, anti-G, or anti-VSIV G antibodies. Next, cells were incubated with either a goat anti-mouse or rabbit anti-human antibody carrying a fluorescent conjugate (Alexa-594 or Alexa-350; Molecular Probes). For confocal microscopy, nuclei of A2-infected cells were visualized with Hoechst stain. Cells were photographed on a Zeiss Axioscope microscope or scanned on a Leica TCS NT confocal microscope system for dual detection of GFP and viral antigens.
Syncytium formation assay.
Vero cells were infected at a multiplicity of infection of 1. At 20 h postinfection, supernatants were removed and cells were incubated in PBS buffered to either pH 7 or 5, for 3 min. PBS was then removed and replaced with fresh medium. Cells were further incubated for 1 h at 37°C, fixed with 4% paraformaldehyde, and photographed on a Zeiss Axiovert microscope using phase contrast or UV light for GFP visualization.
Neutralization of infectivity.
Virus (5 × 104 PFU) was incubated in 250 μl of normal cell growth medium plus 10 mM HEPES for 1 h at room temperature in the presence of anti-VSIV G or anti-VSNJV G antibodies at a range of dilutions. Vero cells were incubated with the pretreated virus for 1.5 h at 37°C, after which cells were washed twice and incubated in normal growth medium at 37°C. At 28 h postinfection, cells were fixed with 4% paraformaldehyde and photographed on a Leica TCS NT confocal microscope.
Ammonium chloride inhibition analysis.
For microscopy analysis, Vero cells were infected at a multiplicity of infection of 0.5. Thirty minutes prior to virus adsorption, ammonium chloride was added to growth medium containing 25 mM HEPES. Concentrations of ammonium chloride were maintained during virus adsorption and postinfection incubation. At 24 h postinfection, cells were fixed with 4% paraformaldehyde, mounted, and photographed on a Leica TCS NT confocal microscope. For flow cytometry analysis, Vero cells were infected at a multiplicity of infection of 1. At 20 h postinfection, cells were trypsinized, resuspended in PBS, and pelleted in a microcentrifuge. Cells were resuspended in 4% paraformaldehyde and incubated for 20 min. Cells were pelleted, resuspended in PBS, and analyzed in a FACSCalibur flow cytometer (Becton Dickinson), using 500,000 events per sample. To calculate relative entry, the number of cells expressing GFP in the presence of ammonium chloride was divided by the number of GFP-expressing cells in the absence of ammonium chloride and multiplied by 100.
Growth curves.
For each virus, a series of 60-mm-diameter dishes of Vero and HEp-2 cells were infected at a multiplicity of infection of 0.1. After virus adsorption, cells were washed once with growth medium. At 0 h postinfection and 24-h intervals for 4 (Vero) or 5 (HEp-2) days, supernatant and cells were harvested separately from one dish of each series and stored at −80°C. Titers of samples were determined by 50% tissue culture infective dose (TCID50) (using 96-well plates with 10-fold dilution series with 12 replicate wells for each dilution). GFP expression was scored at 6 days postinfection. In the case of virus A2, cells were fixed with paraformaldehyde, incubated with a mixture of anti-G and anti-F antibodies followed by a secondary antibody with a fluorescent conjugate, and also scored with a fluorescence microscope. To test whether GFP expression correlated with replicating engineered virus, plaque assays of virus RSΔsh,g,f/Gvsv were first scored for GFP expression, and then the cells were fixed and scored for Gvsv expression via antibodies using a standard plaque assay technique, as described above. Marked plaques expressing GFP overlapped precisely with plaques identified via Gvsv (data not shown). We also compared the results of TCID50 scoring of plates of virus RSΔsh,g/Gvsv either for GFP expression or for expression of viral antigens (i.e., Gvsv or F) after fixation and incubation with anti-GIN or anti-F antibodies. Detection based on GFP, Gvsv, or F yielded identical scores, indicating that scoring on the basis of GFP was an accurate indicator of viral replication and that comparing scores based on GFP and viral antigens detected via immunofluorescence was valid. Log TCID50 scores of the engineered viruses were compared. To determine total virus titers, supernatant- and cell-derived titers were combined.
Scanning electron microscopy (SEM).
Vero cells were infected at a multiplicity of infection of 2 and fixed at 25 h postinfection for 1 h in 2.5% glutaraldehyde-0.1 M cacodylate at room temperature, and this was followed by three washing steps in 0.1 M cacodylate buffer and immersion in 1% osmium tetroxide-0.1 M cacodylate buffer for 1 h. Cells were rinsed three times in cacodylate buffer and once in distilled water and then were dehydrated with ethanol and hexamethyldisilizane. Samples were air dried overnight, coated with gold, and analyzed on an ISI-SX-40 scanning electron microscope (International Scientific Instruments, Inc.).
RESULTS
Construction of cDNAs and recovery of HRSVs with altered glycoprotein gene content.
A plasmid containing a cDNA of the A2 strain of HRSV was constructed as described in Materials and Methods. From this, the SH-G-F region was deleted, generating construct pRSΔsh,g,f (Fig. 1B). Together with a shuttle vector (pBLS-6,7,8), constructed to place ORFs of choice in genome positions six, seven, and eight, pRSΔsh,g,f was used as the basis to engineer cDNAs with an altered glycoprotein gene content. This was done without altering the absolute number of genes or any of the gene junctions, such that untranslated regions as well as the authentic gene start, gene end, and intergenic regions were maintained at every position within the genome in order to maintain wt transcriptional control levels (Fig. 1B). cDNAs were generated that lacked one, two, or all three of the HRSV transmembrane glycoprotein ORFs, and each deleted ORF was replaced as follows: the SH ORF was replaced with that of GFP, the F ORF was replaced with that of marker protein GUS, and the G ORF was replaced with that of a chimeric glycoprotein based on the VSIV G protein. VSIV G contains attachment, fusion, and assembly-exit functions within a single protein and has been successfully used to enhance infectivity of other distantly related viruses (9, 18, 40). However, because the CTD of viral glycoproteins can play a critical role in glycoprotein incorporation and virion budding and morphology, we modified the VSIV G ORF by exchanging the sequence encoding its predicted CTD (amino acids 492 to 512) with that of HRSV F (amino acids 553 to 574) (Fig. 1C) (31, 44, 46, 53, 54, 61). The product of this chimeric ORF was termed Gvsv.
The three cDNAs that were constructed (Fig. 1A) thus varied only in the content of ORFs in genome positions six, seven and eight: (i) pRSΔsh, containing the homologous HRSV G and F ORFs preceded by that of GFP; (ii) pRSΔsh,g/Gvsv, lacking the SH and G ORFs and containing instead those of GFP and Gvsv; and (iii) pRSΔsh,g,f/Gvsv, lacking all three homologous transmembrane glycoprotein ORFs, SH, G, and F, and containing instead those of GFP, Gvsv, and GUS. These engineered cDNAs were transfected into HEp-2 cells previously infected with modified vaccinia Ankara-T7 virus, along with plasmids encoding the N, P, L, and M2-1 proteins, as described in Materials and Methods. Infectious viruses were recovered from all cDNAs and designated RSΔsh, RSΔsh,g/Gvsv, and RSΔsh,g,f/Gvsv, respectively. Virus stocks were generated in Vero cells, yielding titers of approximately 107 PFU/ml. The genomes of virus stocks were verified by RT-PCR across the modified areas followed by sequence analysis at pass 4 to 6 (data not shown).
mRNA expression by the engineered viruses.
The expression of mRNAs by the engineered HRSVs was compared to that of virus A2 by infecting Vero cells at a multiplicity of infection of 2 and labeling with [3H]uridine in the presence of actinomycin D. Total RNA was isolated at 22 h postinfection, and 3′ poly(A) tails were removed by digestion with RNase H after annealing with oligo(dT). The profiles of labeled mRNAs are shown in Fig. 2. The positions of monocistronic A2 mRNAs are indicated on the left (10, 13). The engineered viral genomes all lacked the ORF of the SH gene and hence did not express the SH mRNA; instead, they expressed an mRNA consistent with the size of the GFP ORF inserted in its place (Fig. 2, compare lanes 2 and lanes 3 to 5). Virus RSΔsh,g/Gvsv did not express either the SH or G mRNAs (Fig. 2, lane 4), and virus RSΔsh,g,f/Gvsv expressed neither SH, G, nor F mRNAs (Fig. 2, lane 3). Instead, these viruses expressed the Gvsv mRNA (Fig. 2, lanes 3 and 4), and additionally, in the case of RSΔsh,g,f/Gvsv, an mRNA corresponding to the predicted size of the inserted GUS ORF (Fig. 2, lane 3). In each case, the appropriate mRNA for the deleted ORF was missing, and in its place the appropriate mRNA for the inserted ORF was expressed.
FIG. 2.
RNA synthesis by engineered viruses. Uninfected Vero cells and Vero cells infected with the engineered viruses or virus A2 were subjected to metabolic labeling with [3H]uridine in the presence of actinomycin D from 16 to 22 h postinfection. Total RNA was isolated, 3′ poly(A) tails were removed by digestion with RNase H following annealing with oligo(dT), and RNAs were analyzed by agarose-urea gel electrophoresis. On the left, previously characterized monocistronic mRNAs from wt HRSV are indicated (10, 13). On the right, the positions of transcripts from genes containing introduced ORFs Gvsv, GFP, and GUS are indicated. Lane 1, mock-infected cells; lane 2, wt A2; lane 3, RSΔsh,g,f/Gvsv; lane 4, RSΔsh,g/Gvsv; lane 5, RSΔsh.
Protein expression by the engineered viruses.
Transmembrane glycoprotein expression by each of the viruses was examined by immunofluorescence. Vero cells infected with each of the engineered viruses were fixed with methanol, incubated with antibodies against the HRSV G or F proteins (L9 and MAb19, respectively) or the VSIV G protein (ATCC), and visualized using a secondary antibody carrying a fluorescent conjugate (Fig. 3). In cells infected with virus RSΔsh,g,f/Gvsv, neither the HRSV G nor F proteins were detected; instead the Gvsv protein was detected (Fig. 3). Engineered virus RSΔsh,g/Gvsv also lacked expression of the HRSV G protein but expressed both Gvsv and the HRSV F protein. In cells infected with viruses RSΔsh and A2, which carry wt HRSV G and F genes and no heterologous glycoprotein ORFs, both HRSV G and F proteins were expressed, but not Gvsv (Fig. 3). These results were in agreement with the genome content of each of the viruses and confirmed that in engineered virus RSΔsh,g,f/Gvsv, the only transmembrane glycoprotein expressed was chimeric protein Gvsv.
FIG. 3.
Transmembrane glycoprotein expression by engineered viruses. Vero cells infected with each of the engineered viruses and virus A2 were fixed with methanol at 16 h (for HRSV G) or 24 h (for proteins Gvsv and F) postinfection and incubated with antibody L9 directed against the HRSV G protein (αG), antibody MAb 19 directed against the HRSV F protein (αF), or an anti-VSIV G antibody (αGvsv). After incubation with a secondary antibody carrying an Alexa-594 fluorescent conjugate, samples were examined on a fluorescence microscope and photographed (magnification, ×400). Uninfected Vero cells were included as a control (left panels).
Analysis of Gvsv function.
During entry of VSIV virions via endocytosis, the acidification of endosomes triggers the VSIV G protein to induce virus-cell membrane fusion, which allows entry of the nucleocapsid into the cytoplasm. This capacity to induce membrane fusion can be demonstrated by exposing cells that express VSIV G at the cell surface to low-pH medium, which leads to fusion between adjacent plasma membranes and formation of multinucleated syncytia (21, 40). To examine the membrane fusion capacity of chimeric protein Gvsv, we assayed its ability to induce cell-cell membrane fusion. Vero cells were infected with viruses RSΔsh,g,f/Gvsv, RSΔsh,g/Gvsv, or RSΔsh, at a multiplicity of infection of 1. Infection was allowed to proceed for 20 h, at which time the cells were exposed to PBS at pH 5.0 or 7.0 for 3 min. Cells were then incubated in normal growth medium for 1 h, fixed with 4% paraformaldehyde, and examined by phase-contrast and fluorescence microscopy (Fig. 4). Extensive cell-cell membrane fusion and formation of multinucleated syncytia were observed in RSΔsh,g,f/Gvsv- and RSΔsh,g/Gvsv-infected cells after treatment at pH 5.0 (Fig. 4, lower panels) but not at pH 7.0 (Fig. 4, upper panels). This indicated that chimeric protein Gvsv migrated to the cell surface and was fusion activated by low pH. As expected, low-pH-induced syncytia were not formed in uninfected Vero cells also included in this assay (not shown) or in RSΔsh-infected cells. However, at later times postinfection, multinucleated syncytia appeared gradually in RSΔsh-infected cells in a pH-independent manner, as is typically observed with wt HRSV (data not shown).
FIG. 4.
Analysis of Gvsv fusion capacity by cell-cell membrane fusion assay. Vero cells infected with viruses RSΔsh,g/Gvsv, RSΔsh,g,f/Gvsv, or RSΔsh were exposed for 3 min to pH 7 (top panels) or pH 5 (bottom panels) medium at 20 h postinfection. Cells were further incubated in normal growth medium for 1 h, fixed with 4% paraformaldehyde, and photographed (phase contrast; magnification, ×100). RSΔsh,g,f/Gvsv-infected cells were also photographed on a fluorescence microscope (GFP).
Infectivity of RSΔsh,g,f/Gvsv is neutralized by Gvsv-specific antibodies.
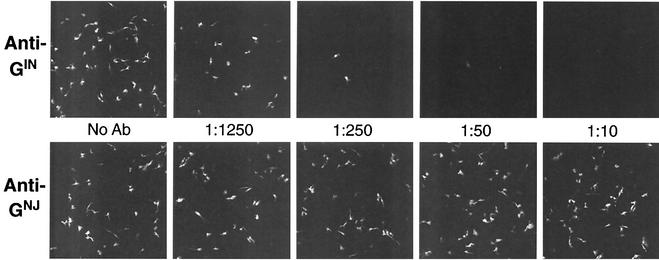
We examined the effect of anti-VSIV G specific antibodies on infectivity of RSΔsh,g,f/Gvsv to Vero cells. As a control, anti-VSNJV G antibodies were included. The anti-VSIV G and -VSNJV G antibodies neutralized their corresponding G proteins at similar concentrations. RSΔsh,g,f/Gvsv virions were preincubated with either antibody in a range of concentrations and assayed for their ability to infect Vero cells. Cells infected with preincubated virus were examined by fluorescence microscopy at 28 h postinfection (Fig. 5). Anti-VSIV G antibodies neutralized infectivity in a concentration-dependent manner (Fig. 5, upper panels). In contrast, even the highest concentrations of anti-VSNJV G antibodies had no effect on RSΔsh,g,f/Gvsv infectivity (Fig. 5, lower panels). To test whether the neutralizing effect could have been due to nonspecific interactions with HRSV or marker proteins expressed by RSΔsh,g,f/Gvsv, the anti-VSIV G antibodies were also used to treat the RSΔsh virus. Preincubated RSΔsh virus was unaffected in its ability to infect Vero cells even at the highest antibody concentrations (data not shown). Together, this indicated that infectivity of virus RSΔsh,g,f/Gvsv was mediated by the Gvsv protein.
FIG. 5.
Neutralization of RSΔsh,g,f/Gvsv infectivity by anti-VSIV G antibodies. Virus RSΔsh,g,f/Gvsv was preincubated with anti-VSIV G (anti-GIN) or anti-VSNJV G (anti-GNJ) antibodies in a range of dilutions. Preincubated virus was used to infect Vero cells for 1.5 h and then removed by wash steps. At 20 h postinfection, cells were fixed and examined by fluorescence microscopy (magnification, ×100). Concentrations of antibodies (Ab) used are indicated.
Virus RSΔsh,g,f/Gvsv utilizes an altered, Gvsv-dependent, entry mechanism.
VSIV virions enter via endocytosis, in which acidification of endosomes triggers the VSIV G protein to induce virus-cell membrane fusion, an event required for entry of the nucleocapsid. The endocytic entry pathway of VSIV virions can be blocked with compounds that buffer the endosomal pH and thus prevent the acidification that induces virus-cell membrane fusion, such as ammonium chloride (26, 43). In contrast to VSIV, HRSV is believed to enter at the plasma membrane in a pH-independent manner, and it was shown previously that entry and replication of a wt HRSV are not affected by ammonium chloride (56). We examined whether entry of virus RSΔsh,g,f/Gvsv was sensitive to ammonium chloride by infecting Vero cells in the presence of a range of ammonium chloride concentrations. Increasing amounts of ammonium chloride progressively inhibited RSΔsh,g,f/Gvsv infectivity (Fig. 6A, upper panels) as measured by the number of cells expressing GFP, while cell viability was unaffected (Fig. 6A, lower panels); a concentration of 20 mM ammonium chloride led to nearly complete inhibition of infectivity, as has been shown for other viruses that utilize this pathway (40, 41, 43). This inhibition appeared to be at a stage beyond viral adsorption, because cells that were incubated with virus in the presence of ammonium chloride but grown in medium without ammonium chloride were efficiently infected (data not shown). This is consistent with the finding that ammonium chloride does not affect virus binding to cells (40). The data presented in Fig. 5 and 6 together show that infectivity of virus RSΔsh,g,f/Gvsv was mediated by the Gvsv protein and required a low-pH activation step.
FIG. 6.
Effect of ammonium chloride (NH4Cl) on virus entry. (A) Vero cells were infected with virus RSΔsh,g,f/Gvsv for 1.5 h at 37°C in the presence of 0, 2, 5, or 20 mM NH4Cl. Cells were then further incubated in the presence of the same NH4Cl concentrations. At 20 h postinfection, cells were fixed with 4% paraformaldehyde and photographed with phase contrast (phase) or in the presence of UV light (GFP) (magnification, ×60). (B) Flow cytometry analysis. Vero cells were infected in the presence or absence of 20 mM NH4Cl with viruses RSΔsh, RSΔsh,g/Gvsv, and RSΔsh,g,f/Gvsv. After infection, cells were washed and further incubated, maintaining the NH4Cl concentrations used during infection. At 20 h postinfection, samples were trypsinized, fixed with paraformaldehyde, and analyzed by flow cytometry. Bars represent the number of GFP-expressing cells in the absence (−) or presence (+) of NH4Cl, relative to the number of GFP-expressing cells in the absence of NH4Cl × 100. Error bars are standard deviations from the mean of duplicate samples.
To determine whether replacement of the SH, G, and F ORFs with that of Gvsv altered the entry pathway from a pH-independent to a pH-dependent mode, we compared the effect of ammonium chloride on entry of virus RSΔsh,g,f/Gvsv to that of virus RSΔsh, which contains the homologous HRSV attachment and fusion proteins G and F (Fig. 6B). Virus RSΔsh,g/Gvsv, containing two fusion-competent glycoproteins (HRSV F and Gvsv), was also included in this experiment. Cells were infected in the presence or absence of ammonium chloride, harvested at 20 h postinfection, fixed, and examined for GFP expression using flow cytometry. Infectivity of RSΔsh,g,f/Gvsv was blocked by 20 mM ammonium chloride as above. In contrast, entry of the RSΔsh virus was unaffected, consistent with previous reports and confirming that RSΔsh and RSΔsh,g,f/Gvsv utilized different entry pathways. Infectivity of engineered virus RSΔsh,g/Gvsv was also severely inhibited by ammonium chloride (Fig. 6B). A similar level of inhibition of RSΔsh,g/Gvsv infectivity was observed by immunofluorescence, in both Vero and HEp-2 cells (data not shown). Apparently, despite the fact that F function was not affected by ammonium chloride (Fig. 6B, virus RSΔsh), the F protein was unable to mediate infectivity in the presence of Gvsv in either Vero or HEp-2 cells.
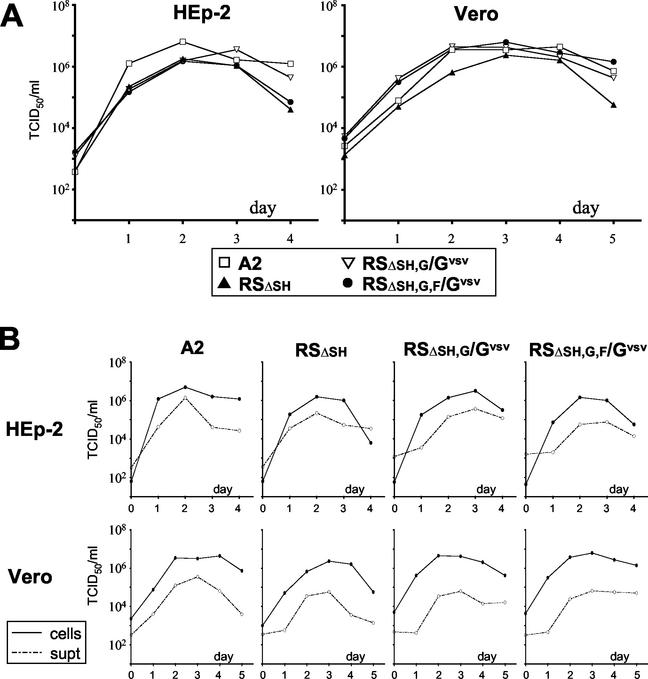
Replication of the engineered viruses in Vero and HEp-2 cells.
To assess the ability of the engineered viruses to replicate in cell culture, multistep growth curves were generated in two different cell types, Vero and HEp-2. These are cell types commonly used for in vitro HRSV studies; however, the glycoprotein requirements for HRSV infectivity in these cell types differ in that G-deleted viruses grow efficiently in Vero cells but are substantially restricted in HEp-2 cells (35, 64). The two cell types were infected with each of the engineered viruses at a multiplicity of infection of 0.1, and viral replication was compared to that of the prototype A2 strain. Cells and supernatants were harvested separately to determine the degree to which the different viruses remained cell associated. Titers were determined by TCID50, in which virus A2 was scored by immunofluorescence with a combination of anti-G and anti-F antibodies, and the engineered viruses were scored using GFP expression as described in Materials and Methods. In either Vero or HEp-2 cells, the RSΔsh virus replicated to levels only slightly lower than those of wt A2 (Fig. 7A). This was consistent with previous findings that absence of SH has only a marginal effect on replication of HRSV in cell culture (8, 62). The viruses RSΔsh,g/Gvsv and RSΔsh,g,f/Gvsv replicated to levels that were similar or slightly lower in HEp-2 cells than those of the A2 virus (Fig. 7A). In Vero cells, onset of RSΔsh,g,f/Gvsv and RSΔsh,g,f/Gvsv progeny virus production appeared somewhat accelerated compared to that of A2, whereas in HEp-2 cells the opposite was observed. Overall, despite the differences in the content of proteins involved in infectivity and the mode of virus entry, relative replication levels between all viruses were similar in both cell types tested.
FIG. 7.
Multistep growth curve analysis of the engineered viruses in HEp-2 and Vero cells. The engineered viruses and prototype virus A2 were used to infect Vero and HEp-2 cells at a multiplicity of infection of 0.1. Cells and supernatants were harvested at 1-day intervals, and titers were determined by TCID50 on the basis of GFP expression (engineered viruses) or indirect immunofluorescence (A2). (A) Total virus growth curves. Data points represent the combined titer of supernatant and cell-derived virus. (B) Comparison of supernatant-derived (dashed lines) and cell-derived (solid lines) virus titers from Vero and HEp-2 cells.
To examine whether the absence of HRSV glycoproteins or the presence of Gvsv had an effect on the degree to which the engineered viruses remained cell associated, titers determined from supernatant and cells were compared. In both Vero and HEp-2 cells, over 90% of infectivity of virus A2 was detected in the cell-associated fraction (Fig. 7B), similar to previous reports with this virus in Vero and HeLa cells (36, 51). With the engineered viruses, no significant changes were observed in either Vero or HEp-2 cells in the ratio of cell-associated to non-cell-associated virus, indicating that neither absence of the various HRSV glycoproteins nor presence of the Gvsv protein significantly altered the proportion of virus released to the supernatant.
Filamentous structures form at the cell surface even when the SH, G, and F proteins are replaced with Gvsv.
Previous work has shown that HRSV infection induces the formation of relatively large (length, 4 to 10 μm), cell-associated filamentous particles at the plasma membrane in various cell types and that the G and F proteins target to these filaments (3, 7, 19, 22, 48, 52, 57). These observations appear to be in agreement with the findings that HRSV infectivity is predominantly cell associated and that the majority of infectivity is lost after passage through 0.45-μm-pore-size filters (47, 51). To determine the effect of the absence of the HRSV membrane glycoproteins on virion morphology, we examined the surface of infected Vero cells by SEM at 25 h postinfection (Fig. 8). In agreement with previous observations, single filaments and bundles of filaments were detected abundantly at the surface of virus A2-infected cells (Fig. 8, panel 2). Also, areas were observed where filament bundles branched off to connect to neighboring bundles, giving the appearance of a dense, highly interconnected network of filaments. Despite the variability in size (approximately 1 to 10 μm) and appearance, the length of these filaments exceeded the length of microvilli (<1 μm) observed at the surface of uninfected Vero cells (Fig. 8, panel 1). Examination of the surface of cells infected by the engineered viruses revealed that in the absence of one, two, or all three of the HRSV transmembrane glycoproteins (Fig. 8, panels 3, 4, and 5, respectively), an abundance of viral filaments with a similar range in size and appearance were detected. These filaments also formed at the surface of HEp-2 cells after infection with each of the engineered viruses or virus A2 (data not shown). Thus, while previous work showed that the HRSV G and F proteins concentrate in virus-induced filaments at the cell surface, neither the SH, G, nor the F protein appears to be essential for the formation of filaments observed with SEM, with the possible exception of the F protein CTD.
FIG. 8.
SEM analysis of the surface of virus-infected cells. Vero cells infected with the engineered viruses (panels 3 to 5) or virus A2 (panel 2), as well as uninfected Vero cells (panel 1), were fixed and processed for SEM at 25 h postinfection and photographed at a magnification of ×5,000. Single filaments (arrowheads) as well as bundles of filaments (arrows) are indicated. Size bar, 2 μm.
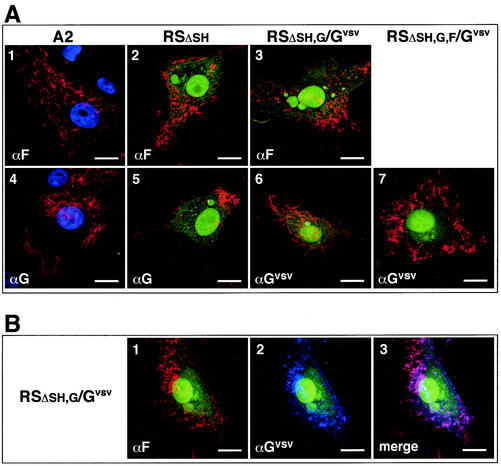
Chimeric glycoprotein Gvsv concentrates in filamentous structures at the cell surface.
To determine whether, as previously reported for the HRSV G and F proteins, chimeric glycoprotein Gvsv targeted to cell surface-associated filaments, we examined virally infected cells by immunofluorescence. Vero cells, infected with the engineered viruses or virus A2 at low multiplicity, were fixed with freshly dissolved 4% paraformaldehyde at 24 h postinfection and incubated with anti-HRSV G or F or anti-VSIV G antibodies. Samples were examined simultaneously for GFP and glycoprotein expression by confocal microscopy (Fig. 9A). GFP expression was detected in cells infected with the engineered viruses, both in the cytoplasm and in the nucleus (Fig. 9A, panels 2, 3, 5, 6, and 7). Virus A2-infected cells, which lack GFP expression, were incubated with Hoechst stain to visualize nuclei (Fig. 9A, panels 1 and 4). The F, G, and Gvsv proteins all concentrated in filamentous structures at or near the cell surface. No differences were observed in the morphology of the filaments between any of the engineered viruses and virus A2, and in each case filaments were heterogeneous in appearance, ranging from discrete rods up to 10 μm long to dense clusters of filaments of highly variable lengths in parallel or perpendicular arrangements. These filaments likely correspond to the aggregates or bundles of filaments observed by SEM (Fig. 8); however, this is difficult to determine due to significant differences between the two techniques in sample treatment and visualization. To examine whether the Gvsv protein would target to the same locations as the authentic HRSV F protein, cells infected with virus RSΔsh,g/Gvsv were similarly fixed, incubated with anti-F and anti-VSIV G antibodies simultaneously, and visualized with, respectively, a red or blue fluorescent conjugate (Fig. 9B, panels 1 and 2). Merging of the images revealed that the Gvsv and HRSV F proteins colocalized in filamentous structures at the surface of infected cells (Fig. 9B, panel 3). Together these data show that Gvsv was efficiently targeted to virus-induced filaments. Whether the F CTD is required for the observed targeting remains to be determined.
FIG. 9.
Cell surface localization of the Gvsv protein and HRSV G and F proteins in virus-infected cells by confocal microscopy. (A) Single antibody incubations for individual detection of G, F, and Gvsv. Vero cells were infected with the engineered viruses or virus A2 and fixed with freshly dissolved 4% paraformaldehyde at 24 h postinfection. G, F, and Gvsv proteins were detected by incubation with anti-VSIV G (αGvsv), anti-HRSV G (αG) or anti-HRSV F (αF) antibodies, followed by incubation with an Alexa-594 (red)-conjugated secondary antibody. A2-infected cells were, in addition, incubated with Hoechst stain to visualize nuclei (panels 1 and 4). Images were generated by sequential scanning for GFP expression (green) or Hoechst stain (blue) and expression of viral antigens (G, F, and Gvsv) (red). For each image, the antibody used is indicated in the lower left corner. Size bar, 20 μm. (B) Double antibody labeling for dual detection of F and Gvsv proteins. Vero cells infected with virus RSΔsh,g/Gvsv were fixed as described above and incubated with anti-HRSV F and anti-VSIV G antibodies simultaneously. The F protein was visualized with an Alexa-594 (red)-conjugated antibody, and Gvsv was visualized with an Alexa-350 (blue)-conjugated antibody. Images were generated by sequential scanning for GFP expression (green), F expression (red), and Gvsv expression (blue). The antibodies used are indicated. Panel 3 is a merged image of panels 1 and 2.
DISCUSSION
The recovery of HRSVs and BRSVs lacking the SH gene, or the SH and G genes combined, has been reported previously (7, 8, 34, 35, 62, 64, 72). Also, the G and F genes of BRSV were successfully cosubstituted with the parainfluenza virus attachment and fusion protein genes (57). These engineered viruses all retained a functional fusion protein gene of the Paramyxoviridae family. In this report, we generated a cDNA from which the ORFs of all three HRSV transmembrane glycoproteins SH, G, and F were deleted. Instead, the ORF of a single chimeric transmembrane glycoprotein based on the VSIV G protein (Gvsv) was added to functionally replace these gene products. Two ORFs encoding marker proteins were added to replace the other two deleted ORFs. The resulting virus, RSΔsh,g,f/Gvsv, did not express any of the homologous HRSV transmembrane glycoproteins yet was infectious to the two different cell types tested here. This feature, together with the generation of viruses lacking either the SH ORF or the SH and G ORFs, allowed us to examine HRSV replication, entry, and morphology in the absence of the SH, G, and F proteins.
Gvsv efficiently mediates infectivity of a virus with SH, G, and F deleted.
The results presented demonstrate that all SH, G, and F functions necessary for infectivity and transmission of HRSV in cell culture can be provided by a single heterologous transmembrane glycoprotein carrying the F protein CTD (Gvsv). Moreover, this functional substitution was efficient, as engineered virus RSΔsh,g,f/Gvsv was infectious to both Vero and HEp-2 cells and replicated in either cell type to titers near the wt level. In contrast, previous work showed that HRSVs lacking the G gene replicated efficiently in Vero cells but were significantly growth impaired in HEp-2 cells (35, 64). Thus, by providing a foreign viral glycoprotein, one can expand the range of cell types in which viruses with G deleted can be propagated. The efficiency of substitution further suggests that beyond providing access to the cell cytoplasm, no additional G and F functions were essential for initiation of infection or for production of infectious progeny virions in cell culture. A possible exception is the F protein CTD, as this domain was included in the chimeric protein used to replace SH, G, and F in virus RSΔsh,g,f/Gvsv.
HRSV can be modified to initiate infection via an endosomal entry route.
Because VSIV and HRSV have different entry mechanisms (16, 43, 56), the strategy of replacing SH, G, and F with a VSIV G-derived membrane glycoprotein provided insight into the ability of HRSV to utilize an alternate entry pathway. Consistent with previous reports, entry of virus RSΔSH, which carries HRSV G and F proteins, was not affected by ammonium chloride, a compound known to block entry of VSIV and other viruses that require an acidification step during entry (40). In contrast, infectivity of virus RSΔsh,g,f/Gvsv was severely inhibited by ammonium chloride, demonstrating that HRSV can be modified to productively infect cells via an alternate (low-pH-dependent) entry mechanism. Because RSΔsh,g,f/Gvsv infectivity was mediated by and dependent on Gvsv and required an acidification step, entry most likely occurs through clathrin-coated vesicles, similar to the entry of VSIV virions (17, 40). This suggests that, when provided with an appropriate receptor binding protein and the means to cross the endosomal membrane, the HRSV ribonucleoprotein can initiate infection after release from endosomes.
Virus RSΔsh,g/Gvsv, which expresses two fusion-competent glycoproteins (Gvsv and HRSV F) that concentrate in virus-induced filaments (Fig. 9B), failed to initiate infection in Vero and HEp-2 cells in the presence of ammonium chloride. This was surprising because previous reports using a virus in which the HRSV SH and G genes were deleted and not replaced showed that F alone was able to mediate efficient propagation in Vero cells (35, 62). However, in these viruses the F gene was now in the seventh position relative to the 3′ end of the genome instead of its wt eighth position, and its expression therefore was likely upregulated (due to the obligatorily sequential transcription with attenuation at each gene junction). The inability of F to mediate RSΔsh,g/Gvsv entry in the presence of ammonium chloride was probably not due to ammonium chloride or the F protein itself, as infectivity of virus RSΔsh was not affected by the same compound (Fig. 6B) and RSΔsh,g/Gvsv-infected cells formed pH-independent syncytia at later time points in the absence of ammonium chloride, indicating fusion competency. Thus, Gvsv appeared to dictate the mode of entry and the HRSV F protein was unable to initiate infection in its presence. It was previously reported that, in HEp-2 cells, the F protein was able to mediate pH-independent entry of a recombinant VSIV which retained its homologous G protein, in the presence of ammonium chloride (33). Although the efficiency of this pH-independent entry process was not directly measured, it raises the possibility that differences exist between the HRSV and VSIV systems that may allow different degrees of F-mediated, pH-independent entry.
Infectivity remains predominantly cell associated in the absence of SH, G, and F proteins.
Budded HRSV virions remain predominantly associated with the cell surface; this is also true for Measles virus (MeV), a Paramyxovirus from the genus Morbillivirus (36, 51, 55). In a similar study, genes encoding attachment protein H and fusion protein F were deleted from the MeV genome and replaced with the VSIV G gene carrying the CTD of MeV F protein. Infectious viruses were recovered, but replication in Vero cells was substantially delayed and viral titers were reduced 10- to 50-fold (55). Notably also, this engineered MeV was now efficiently released to the supernatant of infected cells, instead of being predominantly cell associated. In contrast, replacement of the HRSV SH, G, and F ORFs with that of Gvsv did not increase the proportion of infectious HRSV virions in the supernatant of infected Vero cells, nor did it significantly delay or lower viral yields (Fig. 7). These results indicate that significant differences may exist between HRSV and MeV in the requirements of homologous glycoproteins to drive efficient cell-to-cell transmission, and in the mechanisms by which HRSV and MeV remain associated with the cell surface.
Virus-induced filaments form at the surface of engineered and A2 virus-infected cells.
Filamentous structures are formed at the cell surface after infection of various cell types, both polarized and unpolarized, with HRSV (2, 19, 22, 48, 51). These filaments are sites where the G and F proteins concentrate and vary significantly in length and appearance, ranging from single discrete filaments with a diameter of 0.1 μm and a length between 1 and 10 μm to bundles of filaments of various lengths, often observed as dense clusters. This morphology does not appear to be a consequence of tissue culture adaptation. A predominant filamentous nature was also observed in cells infected with HRSV directly isolated from patients and in autopsy material (4, 5, 32). In both Vero and HEp-2 cells infected with the engineered HRSVs generated here, we observed that filamentous structures, similar to those previously described for a wt HRSV, formed in abundance at the cell surface, even when all three transmembrane glycoproteins were replaced by a single foreign viral glycoprotein carrying the F CTD. Thus, although the virus-induced filaments appear to be sites where the glycoproteins concentrate, the SH and G proteins, as well as the F protein ecto- and transmembrane domains are not essential for the formation or maintenance of these structures.
These results appear consistent with previous findings for VSIV and rabies virus, where the M protein was the predominant determinant of particle morphology (38, 44). In contrast to VSIV, for simian virus 5 (another member of the Paramyxoviridae), coexpression of the N protein, the M protein, and one of the homologous transmembrane glycoproteins was required for efficient particle assembly (53). It is not known whether interactions between the M and F proteins are important for the HRSV assembly process. HRSV M was shown to have independent membrane binding ability, and, in contrast to MeV and Sendai virus, the HRSV M and F proteins did not colocalize in the cytoplasm of infected cells (27). However, the M and F proteins colocalized at the plasma membrane and the F protein had an effect on the degree to which M associated with lipid rafts. Together these findings suggest that the HRSV M protein may be a central organizer of the assembly process and that interactions between M and the glycoproteins also play a role. Whether the F protein CTD is required for efficient incorporation of glycoproteins into virus particles or whether the F protein CTD and M protein are essential components of the observed filamentous structures remains to be established.
In conclusion, our data show that HRSVs having all three transmembrane glycoprotein ORFs, SH, G, and F, deleted and replaced with that of a nonparamyxoviral transmembrane glycoprotein can be recovered. Such viruses are infectious to two different cell types and have an altered entry pathway. These results demonstrate the potential for manipulating HRSV infectivity and transmission for practical applications and as tools to further examine the roles of individual or combinations of HRSV glycoproteins in HRSV biology and pathogenesis.
Acknowledgments
We thank the members of the G. W. Wertz and L. A. Ball laboratories for helpful discussions during preparation of the manuscript and Albert Tousson and Leigh Millican of the UAB imaging facility for technical support.
This work was supported by Public Health Service grants AI20181 from NIH and R37-AI12464 from NIAID.
REFERENCES
- 1.Anderson, K., A. M. King, R. A. Lerch, and G. W. Wertz. 1992. Polylactosaminoglycan modification of the respiratory syncytial virus small hydrophobic (SH) protein: a conserved feature among human and bovine respiratory syncytial viruses. Virology 191:417-430. [DOI] [PubMed] [Google Scholar]
- 2.Bachi, T. 1988. Direct observation of the budding and fusion of an enveloped virus by video microscopy of viable cells. J. Cell Biol. 107:1689-1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bachi, T., and C. Howe. 1973. Morphogenesis and ultrastructure of respiratory syncytial virus. J. Virol. 12:1173-1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bryson, D. G., S. McConnell, M. McAliskey, and M. S. McNulty. 1991. Ultrastructural features of alveolar lesions in induced respiratory syncytial virus pneumonia of calves. Vet. Pathol. 28:286-292. [DOI] [PubMed] [Google Scholar]
- 5.Bryson, D. G., M. F. Platten, S. McConnell, and M. S. McNulty. 1991. Ultrastructural features of lesions in bronchiolar epithelium in induced respiratory syncytial virus pneumonia of calves. Vet. Pathol. 28:293-299. [DOI] [PubMed] [Google Scholar]
- 6.Buchholz, U. J., S. Finke, and K. K. Conzelmann. 1999. Generation of bovine respiratory syncytial virus (BRSV) from cDNA: BRSV NS2 is not essential for virus replication in tissue culture, and the human RSV leader region acts as a functional BRSV genome promoter. J. Virol. 73:251-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Buchholz, U. J., H. Granzow, K. Schuldt, S. S. Whitehead, B. R. Murphy, and P. L. Collins. 2000. Chimeric bovine respiratory syncytial virus with glycoprotein gene substitutions from human respiratory syncytial virus (HRSV): effects on host range and evaluation as a live-attenuated HRSV vaccine. J. Virol. 74:1187-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bukreyev, A., S. S. Whitehead, B. R. Murphy, and P. L. Collins. 1997. Recombinant respiratory syncytial virus from which the entire SH gene has been deleted grows efficiently in cell culture and exhibits site-specific attenuation in the respiratory tract of the mouse. J. Virol. 71:8973-8982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burns, J. C., T. Friedmann, W. Driever, M. Burrascano, and J. K. Yee. 1993. Vesicular stomatitis virus G glycoprotein pseudotyped retroviral vectors: concentration to very high titer and efficient gene transfer into mammalian and nonmammalian cells. Proc. Natl. Acad. Sci. USA 90:8033-8037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Collins, P. L., Y. T. Huang, and G. W. Wertz. 1984. Identification of a tenth mRNA of respiratory syncytial virus and assignment of polypeptides to the 10 viral genes. J. Virol. 49:572-578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collins, P. L., R. A. Olmsted, and P. R. Johnson. 1990. The small hydrophobic protein of human respiratory syncytial virus: comparison between antigenic subgroups A and B. J. Gen. Virol. 71:1571-1576. [DOI] [PubMed] [Google Scholar]
- 12.Collins, P. L., and G. W. Wertz. 1985. The 1A protein gene of human respiratory syncytial virus: nucleotide sequence of the mRNA and a related polycistronic transcript. Virology 141:283-291. [DOI] [PubMed] [Google Scholar]
- 13.Collins, P. L., and G. W. Wertz. 1983. cDNA cloning and transcriptional mapping of nine polyadenylylated RNAs encoded by the genome of human respiratory syncytial virus. Proc. Natl. Acad. Sci. USA 80:3208-3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conzelmann, K. K., and M. Schnell. 1994. Rescue of synthetic genomic RNA analogs of rabies virus by plasmid-encoded proteins. J. Virol. 68:713-719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Couch, R. B., J. A. Englund, and E. Whimbey. 1997. Respiratory viral infections in immunocompetent and immunocompromised persons. Am. J. Med. 102:2-9, 25-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahlberg, J. E. 1974. Quantitative electron microscopic analysis of the penetration of VSV into L cells. Virology 58:250-262. [DOI] [PubMed] [Google Scholar]
- 17.Doxsey, S. J., F. M. Brodsky, G. S. Blank, and A. Helenius. 1987. Inhibition of endocytosis by anti-clathrin antibodies. Cell 50:453-463. [DOI] [PubMed] [Google Scholar]
- 18.Emi, N., T. Friedmann, and J. K. Yee. 1991. Pseudotype formation of murine leukemia virus with the G protein of vesicular stomatitis virus. J. Virol. 65:1202-1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faulkner, G. P., P. V. Shirodaria, E. A. Follett, and C. R. Pringle. 1976. Respiratory syncytial virus ts mutants and nuclear immunofluorescence. J. Virol. 20:487-500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Feldman, S. A., R. M. Hendry, and J. A. Beeler. 1999. Identification of a linear heparin binding domain for human respiratory syncytial virus attachment glycoprotein G. J. Virol. 73:6610-6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Florkiewicz, R. Z., and J. K. Rose. 1984. A cell line expressing vesicular stomatitis virus glycoprotein fuses at low pH. Science 225:721-723. [DOI] [PubMed] [Google Scholar]
- 22.Fuchs, H., and T. Bachi. 1975. Scanning electron microscopical demonstration of respiratory syncytial virus antigens by immunological markers. J. Ultrastruct. Res. 52:114-119. [DOI] [PubMed] [Google Scholar]
- 23.Graham, B. S., J. A. Rutigliano, and T. R. Johnson. 2002. Respiratory syncytial virus immunobiology and pathogenesis. Virology 297:1-7. [DOI] [PubMed] [Google Scholar]
- 24.Han, L. L., J. P. Alexander, and L. J. Anderson. 1999. Respiratory syncytial virus pneumonia among the elderly: an assessment of disease burden. J. Infect. Dis. 179:25-30. [DOI] [PubMed] [Google Scholar]
- 25.Hardy, R. W., S. B. Harmon, and G. W. Wertz. 1999. Diverse gene junctions of respiratory syncytial virus modulate the efficiency of transcription termination and respond differently to M2-mediated antitermination. J. Virol. 73:170-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Helenius, A., M. Marsh, and J. White. 1982. Inhibition of Semliki forest virus penetration by lysosomotropic weak bases. J. Gen. Virol. 58:47-61. [DOI] [PubMed] [Google Scholar]
- 27.Henderson, G., J. Murray, and R. Yeo. 2002. Sorting of the respiratory syncytial virus matrix protein into detergent-resistant structures is dependent on cell-surface expression of the glycoproteins. Virology 300:244-254. [DOI] [PubMed] [Google Scholar]
- 28.Hendricks, D. A., K. Baradaran, K. McIntosh, and J. L. Patterson. 1987. Appearance of a soluble form of the G protein of respiratory syncytial virus in fluids of infected cells. J. Gen. Virol. 68:1705-1714. [DOI] [PubMed] [Google Scholar]
- 29.Huang, Y. T., P. L. Collins, and G. W. Wertz. 1985. Characterization of the 10 proteins of human respiratory syncytial virus: identification of a fourth envelope-associated protein. Virus Res. 2:157-173. [DOI] [PubMed] [Google Scholar]
- 30.Huang, Y. T., and G. W. Wertz. 1983. Respiratory syncytial virus mRNA coding assignments. J. Virol. 46:667-672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jin, H., G. P. Leser, J. Zhang, and R. A. Lamb. 1997. Influenza virus hemagglutinin and neuraminidase cytoplasmic tails control particle shape. EMBO J. 16:1236-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joncas, J., L. Berthiaume, and V. Pavilanis. 1969. The structure of the respiratory syncytial virus. Virology 38:493-496. [DOI] [PubMed] [Google Scholar]
- 33.Kahn, J. S., M. J. Schnell, L. Buonocore, and J. K. Rose. 1999. Recombinant vesicular stomatitis virus expressing respiratory syncytial virus (RSV) glycoproteins: RSV fusion protein can mediate infection and cell fusion. Virology 254:81-91. [DOI] [PubMed] [Google Scholar]
- 34.Karger, A., U. Schmidt, and U. J. Buchholz. 2001. Recombinant bovine respiratory syncytial virus with deletions of the G or SH genes: G and F proteins bind heparin. J. Gen. Virol. 82:631-640. [DOI] [PubMed] [Google Scholar]
- 35.Karron, R. A., D. A. Buonagurio, A. F. Georgiu, S. S. Whitehead, J. E. Adamus, M. L. Clements-Mann, D. O. Harris, V. B. Randolph, S. A. Udem, B. R. Murphy, and M. S. Sidhu. 1997. Respiratory syncytial virus (RSV) SH and G proteins are not essential for viral replication in vitro: clinical evaluation and molecular characterization of a cold-passaged, attenuated RSV subgroup B mutant. Proc. Natl. Acad. Sci. USA 94:13961-13966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levine, S., and R. Hamilton. 1969. Kinetics of the respiratory syncytial virus growth cycle in HeLa cells. Arch. Gesamte Virusforsch. 28:122-132. [DOI] [PubMed] [Google Scholar]
- 37.Levine, S., R. Klaiber-Franco, and P. R. Paradiso. 1987. Demonstration that glycoprotein G is the attachment protein of respiratory syncytial virus. J. Gen. Virol. 68:2521-2524. [DOI] [PubMed] [Google Scholar]
- 38.Lyles, D. S., M. O. McKenzie, P. E. Kaptur, K. W. Grant, and W. G. Jerome. 1996. Complementation of M gene mutants of vesicular stomatitis virus by plasmid-derived M protein converts spherical extracellular particles into native bullet shapes. Virology 217:76-87. [DOI] [PubMed] [Google Scholar]
- 39.Mangor, J. T., S. A. Monsma, M. C. Johnson, and G. W. Blissard. 2001. A GP64-null baculovirus pseudotyped with vesicular stomatitis virus G protein. J. Virol. 75:2544-2556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marsh, M., and A. Helenius. 1989. Virus entry into animal cells. Adv. Virus Res. 36:107-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Martin, K., and A. Helenius. 1991. Transport of incoming influenza virus nucleocapsids into the nucleus. J. Virol. 65:232-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martinez, I., and J. A. Melero. 2000. Binding of human respiratory syncytial virus to cells: implication of sulfated cell surface proteoglycans. J. Gen. Virol. 81:2715-2722. [DOI] [PubMed] [Google Scholar]
- 43.Matlin, K. S., H. Reggio, A. Helenius, and K. Simons. 1982. Pathway of vesicular stomatitis virus entry leading to infection. J. Mol. Biol. 156:609-631. [DOI] [PubMed] [Google Scholar]
- 44.Mebatsion, T., M. Konig, and K. K. Conzelmann. 1996. Budding of rabies virus particles in the absence of the spike glycoprotein. Cell 84:941-951. [DOI] [PubMed] [Google Scholar]
- 45.Murphy, B. R., A. V. Sotnikov, L. A. Lawrence, S. M. Banks, and G. A. Prince. 1990. Enhanced pulmonary histopathology is observed in cotton rats immunized with formalin-inactivated respiratory syncytial virus (RSV) or purified F glycoprotein and challenged with RSV 3-6 months after immunization. Vaccine 8:497-502. [DOI] [PubMed] [Google Scholar]
- 46.Oomens, A. G., and G. W. Blissard. 1999. Requirement for GP64 to drive efficient budding of Autographa californica multicapsid nucleopolyhedrovirus. Virology 254:297-314. [DOI] [PubMed] [Google Scholar]
- 47.Paccaud, M. F., and C. Jacquier. 1970. A respiratory syncytial virus of bovine origin. Arch. Gesamte Virusforsch. 30:327-342. [DOI] [PubMed] [Google Scholar]
- 48.Parry, J. E., P. V. Shirodaria, and C. R. Pringle. 1979. Pneumoviruses: the cell surface of lytically and persistently infected cells. J. Gen. Virol. 44:479-491. [DOI] [PubMed] [Google Scholar]
- 49.Pattnaik, A. K., L. A. Ball, A. W. LeGrone, and G. W. Wertz. 1992. Infectious defective interfering particles of VSV from transcripts of a cDNA clone. Cell 69:1011-1020. [DOI] [PubMed] [Google Scholar]
- 50.Pringle, C. R. 1987. Progress towards control of the acute respiratory viral diseases of childhood. Bull. W. H. O. 65:133-137. [PMC free article] [PubMed] [Google Scholar]
- 51.Roberts, S. R., R. W. Compans, and G. W. Wertz. 1995. Respiratory syncytial virus matures at the apical surfaces of polarized epithelial cells. J. Virol. 69:2667-2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roberts, S. R., D. Lichtenstein, L. A. Ball, and G. W. Wertz. 1994. The membrane-associated and secreted forms of the respiratory syncytial virus attachment glycoprotein G are synthesized from alternative initiation codons. J. Virol. 68:4538-4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schmitt, A. P., G. P. Leser, D. L. Waning, and R. A. Lamb. 2002. Requirements for budding of paramyxovirus simian virus 5 virus-like particles. J. Virol. 76:3952-3964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schnell, M. J., L. Buonocore, E. Boritz, H. P. Ghosh, R. Chernish, and J. K. Rose. 1998. Requirement for a non-specific glycoprotein cytoplasmic domain sequence to drive efficient budding of vesicular stomatitis virus. EMBO J. 17:1289-1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Spielhofer, P., T. Bachi, T. Fehr, G. Christiansen, R. Cattaneo, K. Kaelin, M. A. Billeter, and H. Y. Naim. 1998. Chimeric measles viruses with a foreign envelope. J. Virol. 72:2150-2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Srinivasakumar, N., P. L. Ogra, and T. D. Flanagan. 1991. Characteristics of fusion of respiratory syncytial virus with HEp-2 cells as measured by R18 fluorescence dequenching assay. J. Virol. 65:4063-4069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stope, M. B., A. Karger, U. Schmidt, and U. J. Buchholz. 2001. Chimeric bovine respiratory syncytial virus with attachment and fusion glycoproteins replaced by bovine parainfluenza virus type 3 hemagglutinin-neuraminidase and fusion proteins. J. Virol. 75:9367-9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Stott, E. J., G. Taylor, L. A. Ball, K. Anderson, K. K. Young, A. M. King, and G. W. Wertz. 1987. Immune and histopathological responses in animals vaccinated with recombinant vaccinia viruses that express individual genes of human respiratory syncytial virus. J. Virol. 61:3855-3861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sullender, W. M. 2000. Respiratory syncytial virus genetic and antigenic diversity. Clin. Microbiol. Rev. 13:1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sussman, D. J. 1995. 24-hour assay for estimating the titer of beta-galactosidase-expressing baculovirus. BioTechniques 18:50-51. [PubMed] [Google Scholar]
- 61.Takimoto, T., T. Bousse, E. C. Coronel, R. A. Scroggs, and A. Portner. 1998. Cytoplasmic domain of Sendai virus HN protein contains a specific sequence required for its incorporation into virions. J. Virol. 72:9747-9754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Techaarpornkul, S., N. Barretto, and M. E. Peeples. 2001. Functional analysis of recombinant respiratory syncytial virus deletion mutants lacking the small hydrophobic and/or attachment glycoprotein gene. J. Virol. 75:6825-6834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Teng, M. N., and P. L. Collins. 1998. Identification of the respiratory syncytial virus proteins required for formation and passage of helper-dependent infectious particles. J. Virol. 72:5707-5716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Teng, M. N., S. S. Whitehead, and P. L. Collins. 2001. Contribution of the respiratory syncytial virus G glycoprotein and its secreted and membrane-bound forms to virus replication in vitro and in vivo. Virology 289:283-296. [DOI] [PubMed] [Google Scholar]
- 65.Tripp, R. A., D. Moore, L. Jones, W. Sullender, J. Winter, and L. J. Anderson. 1999. Respiratory syncytial virus G and/or SH protein alters Th1 cytokines, natural killer cells, and neutrophils responding to pulmonary infection in BALB/c mice. J. Virol. 73:7099-7107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Varga, S. M., and T. J. Braciale. 2002. RSV-induced immunopathology: dynamic interplay between the virus and host immune response. Virology 295:203-207. [DOI] [PubMed] [Google Scholar]
- 67.Walsh, E. E., and J. Hruska. 1983. Monoclonal antibodies to respiratory syncytial virus proteins: identification of the fusion protein. J. Virol. 47:171-177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wertz, G. W., P. L. Collins, Y. Huang, C. Gruber, S. Levine, and L. A. Ball. 1985. Nucleotide sequence of the G protein gene of human respiratory syncytial virus reveals an unusual type of viral membrane protein. Proc. Natl. Acad. Sci. USA 82:4075-4079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wertz, G. W., M. Krieger, and L. A. Ball. 1989. Structure and cell surface maturation of the attachment glycoprotein of human respiratory syncytial virus in a cell line deficient in O glycosylation. J. Virol. 63:4767-4776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wertz, G. W., E. J. Stott, K. K. Young, K. Anderson, and L. A. Ball. 1987. Expression of the fusion protein of human respiratory syncytial virus from recombinant vaccinia virus vectors and protection of vaccinated mice. J. Virol. 61:293-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Whelan, S. P., L. A. Ball, J. N. Barr, and G. T. Wertz. 1995. Efficient recovery of infectious vesicular stomatitis virus entirely from cDNA clones. Proc. Natl. Acad. Sci. USA 92:8388-8392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Whitehead, S. S., A. Bukreyev, M. N. Teng, C. Y. Firestone, M. St. Claire, W. R. Elkins, P. L. Collins, and B. R. Murphy. 1999. Recombinant respiratory syncytial virus bearing a deletion of either the NS2 or SH gene is attenuated in chimpanzees. J. Virol. 73:3438-3442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wyatt, L. S., B. Moss, and S. Rozenblatt. 1995. Replication-deficient vaccinia virus encoding bacteriophage T7 RNA polymerase for transient gene expression in mammalian cells. Virology 210:202-205. [DOI] [PubMed] [Google Scholar]