Abstract
OBJECTIVE
Little is known about patients who skip doses or otherwise avoid using their medications because of cost. We sought to identify which elderly patients are at highest risk of restricting their medications because of cost, and how prescription coverage modifies this risk.
DESIGN AND PARTICIPANTS
Cross-sectional study from the 1995–1996 wave of the Survey of Asset and Health Dynamics Among the Oldest Old, a population-based survey of Americans age 70 years and older.
MEASUREMENTS
Subjects were asked the extent of their prescription coverage, and whether they had taken less medicine than prescribed for them because of cost over the prior 2 years. We used bivariate and multivariate analyses to identify risk factors for medication restriction in subjects who lacked prescription coverage. Among these high-risk groups, we then examined the effect of prescription coverage on rates of medication restriction.
MAIN RESULTS
Of 4,896 seniors who regularly used prescription medications, medication restriction because of cost was reported by 8% of subjects with no prescription coverage, 3% with partial coverage, and 2% with full coverage (P < .01 for trend). Among subjects with no prescription coverage, the strongest independent predictors of medication restriction were minority ethnicity (odds ratio [OR], 2.9 compared with white ethnicity; 95% confidence interval [95% CI], 2.0 to 4.2), annual income <$10,000 (OR, 3.8 compared with income ≥$20,000; 95% CI, 2.4 to 6.1), and out-of-pocket prescription drug costs >$100 per month (OR, 3.3 compared to costs ≤$20; 95% CI, 1.5 to 7.2). The prevalence of medication restriction in members of these 3 risk groups was 21%, 16%, and 13%, respectively. Almost half (43%) of subjects with all 3 risk factors and no prescription coverage reported restricting their use of medications. After multivariable adjustment, high-risk subjects with no coverage had 3 to 15 times higher odds of medication restriction than subjects with partial or full coverage (P < .01).
CONCLUSIONS
Medication restriction is common in seniors who lack prescription coverage, particularly among certain vulnerable groups. Seniors in these high-risk groups who have prescription coverage are much less likely to restrict their use of medications.
Keywords: insurance, pharmaceutical services; health services accessibility; prescriptions, drug; fees, pharmaceutical; aged
Prescription drug costs are growing faster than any other segment of health care.1 In turn, many anecdotal reports have surfaced of elderly patients forced to skip doses of their medications, or avoid these medications altogether, because they lack adequate prescription drug coverage and cannot afford the high cost of modern pharmaceuticals.2–4 These stories, and the media interest they have generated, have stimulated calls for a prescription drug benefit for Medicare.4
However, the extent to which different groups of elderly patients skip, avoid, or otherwise restrict their use of prescription medications because of cost is largely unknown. Recent studies show that patients who lack prescription coverage receive fewer prescription medications than those with coverage.5–8 However, it remains unclear to what extent these disparities reflect differential prescribing by physicians, preferential enrollment of sicker patients into plans that provide coverage, or patients restricting their own use of medications because of cost.9 Moreover, little is known about which groups of underinsured patients are at the greatest risk of restricting their use of medications because of cost, and how prescription coverage may attenuate that risk.
We studied these questions in a large, nationally representative cohort of older Americans. First, we compared the rate of medication restriction in patients with different levels of prescription insurance. Next, we determined which seniors who lacked prescription coverage were at highest risk of restricting their use of medications because of cost. Finally, to examine how prescription coverage modified the risk of medication restriction among these vulnerable groups, we compared rates of medication restriction in high-risk seniors who had no, partial, or full coverage.
METHODS
Population
We studied elders who participated in the second wave (1995–1996) of the Survey of Asset and Health Dynamics Among the Oldest Old (AHEAD). AHEAD is a nationally representative, longitudinal survey of noninstitutionalized elders who were at least 70 years old at the cohort's inception in 1993. African-American and Hispanic persons and residents of Florida were oversampled within a multistage area probability sample.10,11
Of 6,237 persons age 70 years and older in the second wave of AHEAD, we limited our analytic sample to the 4,935 who stated that they regularly used prescription medications. An additional 39 were excluded because they did not answer questions about medication restriction, did not state their level of prescription coverage, or had a pharmacy claim under dispute. This left a final sample size of 4,896 subjects.
Measures
Our primary outcome variable was medication restriction because of cost, assessed by the question: “At any time in the last 2 years have you ended up taking less medication than was prescribed for you because of the cost?” Independent (predictor) variables included prescription drug coverage, demographic characteristics, several measures of health status, and monthly out-of-pocket spending on prescription drugs.
Subjects reported whether their insurance covered the costs of their prescription medications not at all, partly, or completely. We measured comorbidity by the number of self-reported diagnoses from a list of 7 conditions (hypertension, diabetes mellitus, cancer, chronic lung disease, ischemic heart disease or heart failure, cerebrovascular disease, psychiatric problems, and arthritis or “rheumatism”). We defined independence in activities of daily living (ADL) as needing no assistance with bathing, dressing, eating, transferring in or out of bed, and toileting.
Income, total assets, and monthly out-of-pocket costs for prescription medications were assessed by self-report. Subjects unable or unwilling to state their exact earnings or out-of-pocket prescription drug costs were given an option of choosing from among several ranges of income and cost.
Ethnicity was determined by self-report. In most of our analyses, point estimates for Hispanic subjects were similar to those of African-American subjects, but were unstable given the low number of Hispanic subjects in the sample. As a result, we collapsed both groups into the ethnic category “minority.” One percent of subjects belonged to other ethnic groups, and were not included in the analysis. Marital status was defined as “spouse at home” for those with a spouse or partner living with them, and “no spouse at home” for all others.
Analyses
For each analysis, we adjusted for survey weights intended to make the AHEAD sample representative of the noninstitutionalized U.S. population age 70 and older.10 This involved the use of 1) sample weights to adjust for the systematic oversampling of select groups and for interviewee nonresponse, and 2) design weights to account for variance intrinsic to the multistage sampling technique used to identify survey households. Repeating the analyses with unweighted data yielded similar results.
We first compared characteristics of subjects who reported no, partial, and full prescription coverage. Continuous variables were compared using 1-way analysis of variance (ANOVA) or the Kruskall-Wallis ANOVA, and categorical variables were analyzed using the χ2test (modified for trend where appropriate). Using the same bivariate analytic techniques, we evaluated which of the subjects who lacked prescription coverage were at increased risk of restricting their medications. We then performed stepwise logistic regression of all variables (see Table 2)) (P < .05 to enter, P < .10 to stay, P < .05 to report) to identify independent predictors of medication restriction in subjects with no prescription coverage. We included indicator variables for income (169 subjects) and comorbidity (151 subjects) when data were missing.
Table 2.
Medication Restriction in Seniors with No Prescription Coverage (N = 1,911)
| Characteristic | Restricted Medications, % | Relative Risk of Medication Restriction (95% Confidence Interval)* |
|---|---|---|
| Age, y | ||
| ≥80 | 6.2 | — |
| <80 | 8.8 | 1.4 (1.0 to 2.0) |
| Gender | ||
| Male | 6.4 | — |
| Female | 8.3 | 1.3 (0.9 to 1.9) |
| Ethnicity | ||
| White | 6.2 | — |
| Minority | 20.9 | 3.4 (2.4 to 4.7) |
| Income | ||
| ≥$20,000 | 3.7 | — |
| $10,000 to $19,999 | 7.6 | 2.1 (1.3 to 3.3) |
| <$10,000 | 15.6 | 4.3 (2.8 to 6.6) |
| Education | ||
| High school or greater | 5.4 | — |
| 9 to 11 years | 9.3 | 1.7 (1.1 to 2.6) |
| <9 Years | 12.6 | 2.3 (1.7 to 3.3) |
| Marital status | ||
| Spouse at home | 6.4 | — |
| No spouse at home | 8.8 | 1.4 (1.0 to 1.9) |
| Self-rated health | ||
| Excellent or very good | 4.4 | — |
| Good or fair | 7.7 | 1.7 (1.1 to 2.7) |
| Poor | 15.7 | 3.5 (2.2 to 5.7) |
| Comorbid conditions | ||
| 0 to 1 | 5.0 | — |
| 2 to 3 | 7.4 | 1.5 (1.0 to 2.3) |
| ≥4 | 16.6 | 3.3 (2.1 to 5.3) |
| ADL | ||
| Independent in all ADLs | 6.1 | — |
| Dependent in ≥1 ADL | 12.4 | 2.0 (1.5 to 2.8) |
| Monthly out-of-pocket prescription drug cost | ||
| ≤$20 | 3.1 | — |
| $21 to $100 | 6.5 | 2.1 (1.1 to 4.0) |
| >$100 | 13.4 | 4.4 (2.4 to 8.1) |
Baseline risk of 1.00 assigned to lowest risk category within each group.
ADL, activities of daily living.
Our next set of analyses assessed how prescription coverage modified the risk of medication restriction in groups found to be at high risk in the absence of coverage. First, for each of these high-risk groups, we used independent samples t tests to compare the rate of medication restriction in subjects with no coverage to the rates in those with partial and full coverage. To determine the independent association between prescription coverage and medication restriction, within each high-risk group we developed a logistic regression model in which the dependent variable was medication restriction, the major independent variable was degree of prescription coverage, and the other independent variables were those found on our prior analyses to be independently associated with medication restriction (excluding out-of-pocket prescription drug costs). We excluded out-of-pocket prescription drug costs from the models because these costs are likely to be a major causal mechanism by which prescription coverage affects medication restriction. Including this causal mechanism would have overadjusted our models, with subsequent misestimation of the true effect of prescription coverage on medication restriction. To evaluate the magnitude of this effect, we added prescription drug costs to the models and repeated the analyses.
RESULTS
Of 4,896 subjects in the analytic cohort, 39% reported no prescription coverage, 44% reported partial coverage, and 17% reported full coverage. Their characteristics are presented in Table 1. Taking less medication than prescribed because of cost was noted by 7.7% of subjects with no prescription coverage, 3.0% of subjects with partial coverage, and 2.0% of subjects with full coverage (P for trend <.01). Out-of-pocket prescription drug costs were substantially higher in those lacking prescription coverage; median and 75th percentile costs were $60 and $119 per month for subjects with no coverage, compared with $24 and $50 per month for those with partial coverage (P < .001 for both comparisons). Of note, full prescription coverage was more common in lower-income subjects than in their wealthier counterparts. This is explained in part by higher rates of Medicaid coverage in those with incomes less than $10,000 (37.1%) than in those with larger incomes (6.5% for income $10,000 to $19,999, 0.8% for income $20,000 or greater, P < .001 for differences).
Table 1.
Characteristics of Subjects
| Extent of Prescription Coverage | |||
|---|---|---|---|
| No Coverage (n = 1,911) | Partial Coverage (n = 2,095) | Full Coverage (n = 890) | |
| Mean age, y ±SD | 79.5 ± 6.6 | 78.9 ± 5.5 | 79.5 ± 6.0 |
| Female, % | 67.7 | 61.3 | 65.1 |
| Ethnicity, % | |||
| White | 89.3 | 87.2 | 73.4 |
| African American | 7.3 | 9.4 | 14.3 |
| Hispanic | 2.5 | 2.5 | 10.4 |
| Income, % | |||
| ≥$20,000 | 41.1 | 47.5 | 35.0 |
| $10,000 to $19,999 | 34.5 | 30.6 | 25.5 |
| <$10,000 | 24.4 | 21.9 | 39.5 |
| Education, % | |||
| High school or greater | 59.6 | 62.2 | 47.4 |
| 9 to 11 years | 18.3 | 15.5 | 16.9 |
| <9 Years | 22.0 | 22.3 | 35.7 |
| Marital status, % | |||
| Spouse at home | 45.1 | 50.6 | 40.8 |
| No spouse at home | 54.9 | 49.4 | 59.2 |
| Self-rated health, % | |||
| Excellent or very good | 30.4 | 28.2 | 24.4 |
| Good or fair | 57.4 | 57.6 | 55.9 |
| Poor | 12.1 | 14.2 | 19.7 |
| Comorbid conditions, % | |||
| 0 to 1 | 30.1 | 25.5 | 24.5 |
| 2 to 3 | 56.2 | 54.8 | 54.0 |
| ≥4 | 13.7 | 19.8 | 21.5 |
| ADL, % | |||
| Independent in all ADLs | 74.1 | 71.3 | 60.6 |
| Dependent in ≥1 ADL | 25.9 | 28.7 | 39.4 |
| Monthly out-of-pocket prescription drug cost, % | |||
| ≤$20 | 19.0 | 47.4 | ** |
| $21 to $100 | 54.7 | 40.5 | ** |
| >$100 | 26.3 | 12.1 | ** |
*Out-of-pocket prescription drug cost not reported for subjects with full coverage.
P < .01 in all groups for difference between insurance cohorts.
ADL, activities of daily living.
We next evaluated the bivariate association between medication restriction and a variety of patient characteristics in seniors with no prescription coverage (Table 2). Medication restriction due to cost was reported by 20.9% of minority subjects, 15.6% of subjects with income less than $10,000, 15.7% of subjects with poor self-rated health, 16.6% of subjects with 4 or more comorbid conditions, and 13.4% of seniors with out-of-pocket prescription drug costs greater than $100 per month. These high-risk seniors were more than 3 times as likely to restrict medications than the lowest risk subjects within each group.
Similar risk factors for medication restriction were observed in seniors with partial coverage, although the absolute magnitude of restriction and the differences within groups were substantially smaller. Subjects with full coverage restricted medications only rarely, and patterns within groups were not readily discernible.
We next used stepwise logistic regression to determine which risk factors independently predicted medication restriction among seniors with no prescription coverage (Table 3). Independent predictors included age less than 80, minority ethnicity, lower or middle income, dependency in activities of daily living, and out-of-pocket prescription drug costs greater than $100 per month.
Table 3.
Medication Restriction in Seniors with No Prescription Coverage: Multivariate Results
| Characteristic | Adjusted Odds Ratio (95% Confidence Interval) |
|---|---|
| Age <80 y (compared to ≥80) | 2.0 (1.4 to 3.0) |
| Minority ethnicity (compared to white) | 2.9 (2.0 to 4.2) |
| Income (compared to ≥$20,000) | |
| $10,000 to $19,999 | 1.8 (1.1 to 3.2) |
| <$10,000 | 3.8 (2.4 to 6.1) |
| Dependent in ≥1 ADL (compared to fully independent) | 1.6 (1.1 to 2.6) |
| Monthly out-of-pocket prescription drug cost (compared to ≤$20) | |
| $21 to $100 | 1.8 (0.9 to 3.7) |
| >$100 | 3.3 (1.5 to 7.2) |
ADL, activities of daily living.
To adjust for interethnic differences in total wealth that are not measured by income,12 we recalculated the multivariate model with a measure of total assets obtained 2 years earlier in the first wave of AHEAD. Our results were unchanged. To further clarify the predictive value of out-of-pocket drug costs, we recalculated the model excluding all clinical variables (self-rated health, number of comorbid conditions, and ADL dependence) that might themselves cause higher drug costs. The odds ratio associated with out-of-pocket prescription drug costs greater than $100 per month increased from 3.3 to 4.5, while the odds ratio for drug costs of $21 to $100 per month increased from 1.8 to 2.1 (P < .05 for both adjusted odds ratios). The odds ratios for all other variables changed by less than 15%.
We next assessed how prescription coverage modified the rate of medication restriction in subjects with minority ethnicity, low income, or high out-of-pocket prescription drug costs (the 3 strongest risk factors identified in our multivariate model;Table 4) Among each of these groups, medication restriction was substantially more common in subjects with no coverage than in those with partial or full coverage (P < .001 by independent samples t tests).
Table 4.
Prevalence of and Adjusted Risk for Medication Restriction among High-Risk Groups, by Prescription Coverage
| Restricting Medications, %* | Adjusted Odds for Medication Restriction (95% Confidence Interval)† | ||||
|---|---|---|---|---|---|
| Characteristic | No Coverage | Partial Coverage | Full Coverage | No vs Full Coverage | No vs Partial Coverage |
| Minority ethnicity | 20.9 | 7.5 | 3.7 | 10.3 (4.4 to 24.4) | 4.3 (2.6 to 7.3) |
| Income <$10,000 | 15.6 | 7.7 | 2.3 | 14.8 (6.7 to 32.6) | 3.2 (2.2 to 4.6) |
| Monthly out-of-pocket prescription drug cost >$100 | 13.4 | 4.3 | ‡‡ | ‡‡ | 3.8 (2.2 to 6.5) |
P < .001 for comparisons within each group by independent samples t tests (no vs partial coverage, no vs full coverage).
Multivariate odds ratio, adjusting for all variables independently associated with medication restriction in seniors without prescription coverage, except out-of-pocket prescription drug cost.
‡Out-of-pocket prescription drug costs not assessed for subjects with full coverage.
Within each high-risk group, we next used a multivariate model to control for the factors found on our previous analyses to be independently associated with medication restriction (except out-of-pocket prescription drug costs). After this adjustment, the odds of medication restriction in minority subjects was 10.3 (95% confidence interval [95% CI], 4.4 to 24.4) times higher in those with no coverage than in those with full coverage. Similarly, the odds of medication restriction was 14.8 (95% CI, 6.7 to 32.6) times higher in low-income subjects with no coverage than in those with full coverage. Drug cost data were not available for patients with full coverage, but subjects with high out-of-pocket drug costs and no coverage were 3.8 (95% CI, 2.2 to 6.5) times more likely to restrict their use of medications than their counterparts with partial coverage.
Out-of-pocket prescription drug costs were excluded from these analyses to avoid overadjustment for this presumably causal link between coverage status and medication restriction. When drug costs were added back to the multivariate model, the association between medication restriction and prescription coverage was substantially attenuated, but did not fully disappear. For example, the odds of medication restriction among those with no coverage compared to full coverage decreased to 5.3 (95% CI, 1.2 to 23.0) for minority subjects and 7.0 (95% CI, 2.0 to 24.4) for subjects with income less than $10,000.
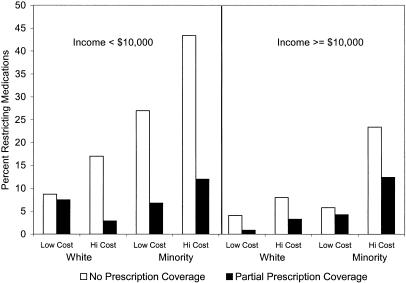
Figure 1 demonstrates the interaction of these 3 risk factors (minority ethnicity, low income, and high out-of-pocket prescription drug costs) among subjects with no coverage and partial coverage. Subjects with full coverage were not asked about out-of-pocket drug costs, so they could not be included in this stratified analysis. Increasing numbers of risk factors were associated with a greater risk of medication restriction. In the highest risk group of all 3 risk factors and no prescription coverage, 43% of subjects restricted their use of medications. In each group, subjects with no coverage were at consistently higher risk of medication restriction than were subjects with partial coverage.
FIGURE 1.
Medication restriction among risk groups, by prescription coverage status. Low cost, monthly out-of-pocket prescription drug cost ≤$100; high cost, monthly out-of-pocket prescription drug cost >$100.
DISCUSSION
Anecdotal reports have brought attention to underinsured patients who restrict their use of medications because of cost.2–4 However, surprisingly little research has assessed the frequency of this behavior, which patients are at the highest risk of medication restriction, and how prescription coverage may modify this risk. Our findings quantify and clarify these relationships. Among seniors with no prescription coverage, medication restriction is common in several vulnerable populations, including ethnic minorities, the poor, the sick and frail, and those with high out-of-pocket drug costs. In contrast, seniors in these high-risk groups who had partial or full prescription coverage were much less likely to restrict their use of medications.
Several of these findings bear further examination. Low income and high out-of-pocket drug costs both play an important role in medication restriction, consistent with basic economic principles. However, the strong association between minority ethnicity and medication restriction was unexpected. This association persisted after adjustment for out-of-pocket drug costs, income, health status, and other risk factors, suggesting that minority patients may be more predisposed to medication restriction when confronted with prescription costs for which they lack insurance. Part of this association may be due to unmeasured economic factors. However, interethnic differences in attitudes and behaviors toward medical decisions, reflecting different experiences with the health care system, may also play a role.13–15 As a result, minority elders may prioritize prescription drug spending differently than whites in the face of competing economic concerns, including such necessities as food and shelter. Whatever the cause, this high risk of medication restriction was very sensitive to prescription coverage, with rates of restriction dramatically lower among minorities who had prescription coverage than in those who lacked it.
Similar factors may also explain why out-of-pocket prescription drug costs, the presumed main causal mechanism linking prescription coverage to medication restriction, only partially explained the relationship between prescription coverage and medication restriction even after adjustment for income, ethnicity, and other variables. Some of the residual association may be due to imprecision of the drug cost variable we used. However, it may be that people with prescription coverage have greater personal investment in the health care system, and that subsidized drug costs make patients more willing to pay their share for medications even if their total out-of-pocket expenditures are equal to patients receiving no such help.
Although scant research has directly addressed medication restriction due to cost, other related studies support our findings. A report from the 1997 National Health Interview Survey found increased rates of medication restriction in Medicare patients who lacked prescription coverage.9 Studies of Medicare beneficiaries show consistently less prescription drug use among patients who lack prescription coverage than among those with coverage.5–8,16,17 These disparities, which are more pronounced in the sickest and poorest patients, have grown in recent years. Overall, those who lack prescription coverage receive 30% fewer prescriptions, yet have nearly twice the out-of-pocket costs, than those with coverage.6,7 Similar associations between medication cost and use have been found with medication copayments.18,19
The effect of medication restriction on the health and welfare of individual patients, and on total health system spending, remains incompletely defined. However, policies designed to limit medication use may have serious consequences for patients' health, resulting in increased emergency department visits, nursing home admissions, use of emergency mental health services, and more.20–24 Further, drug costs savings from such policies can be offset by increased utilization of other health services due to patient underuse of essential medications.1,20,24–27
High drug costs and lack of prescription coverage may have additional consequences. Doctors who know their patients cannot afford high prescription costs may be less likely to prescribe costly but effective medications. Moreover, medication expenses comprise a substantial proportion of the 19% of elderly people's income that is spent on health care, imposing a particularly heavy burden on the poor.9,28,29 As a result, many low-income elderly may be forced to choose between their medications and food, clothing, or telephone service.2 In this way, even those elders who do not restrict their use of medications may be forced to forego other goods and services important to their well-being.
The risk factors for medication restriction that we identified would be less important were they not so common. Half of all Medicare enrollees lack a consistent source of prescription coverage,30 and a disproportionate share of the uncovered live below the poverty line.6 Out-of-pocket prescription drug costs exceeded $100 per month in over one quarter of the elderly subjects with no prescription coverage that we surveyed in 1995–1996. Since the time of the survey, prescription drug expenses have approximately doubled,1 and prescription coverage options have declined for many seniors.9,31
Several methodologic considerations may affect interpretation of this study. Because medication restriction was assessed by self-report, it is subject to questions of validity (i.e., systematic misreporting) and bias (i.e., differential reporting by one group compared with another). We believe the question used in this study has good face and construct validity for the measurement of medication restriction, but we have no data to directly measure the accuracy of this question and the responses it generated. Other studies that have compared patient recall with medical record review document a wide range of accuracy in recalling the use of specific medications and health services.32–36 A handful of studies that examined the effect of socioeconomic factors such as income, education, and race on the accuracy of recall have produced mixed results.33,35,37–41 Thus, while we cannot rule out systematic misreporting of medication restriction, the tendency to underrepresent socially undesirable activities and forget remote events suggests that, to the extent that our data is inaccurate, we likely underestimated the true level of medication restriction.37,38 In addition, while little is known about differential reporting between traditionally disadvantaged versus advantaged groups, the effect would have to be very large to account for the magnitude of differences that we found.
Several other considerations are worth noting. Information on prescription coverage status was also assessed by self-report, the reliability of which has not been fully determined.17,42 Subjects were not provided a standard definition to classify their level of prescription coverage. Also, frequent changes in prescription coverage in the elderly suggests that some subjects with one level of coverage at the time of the survey may have had a different level of coverage in the recent past.6,9 Unmeasured variables, such as depression and personal investment in the health care system, may account for some of the variance in rates of medication restriction. Because medication restriction was assessed in a yes/no format, we could not assess the degree of restriction, nor could we assess the number and types of medications used. Finally, the cross-sectional design precludes us from inferring a causal link between lack of prescription coverage and medication restriction.
The association between prescription coverage and medication restriction, particularly in certain high-risk groups, has important implications for both clinicians and policymakers. Physicians should be alert to the possibility of medication restriction among their elderly patients with no insurance, particularly minority patients and those with low income or high out-of-pocket drug costs. Asking about the impact of medication costs can help physicians identify patients who could benefit from government assistance, industry programs for the medically indigent, or the selection of less-expensive therapeutic alternatives. However, the scope of this problem among vulnerable seniors calls for a broader solution.1 A more comprehensive coverage plan, and policies that limit medication costs, may help reduce medication restriction and with it the clinical, economic, and social morbidity that disproportionately affects our most vulnerable seniors.
Acknowledgments
We thank Kyle Dane (University of California–San Francisco) for his assistance with statistical programming and analysis, and C. Seth Landefeld, MD (San Francisco Veterans Affairs Medical Center and University of California–San Francisco) for his advice on earlier drafts of this manuscript.
Dr. Steinman was supported in part by the VA National Quality Scholars Fellowship Program. Dr. Covinsky was supported in part by an Independent Scientist Award from the Agency for Healthcare Research and Quality (K02HS00006-01) and is a Paul Beeson Faculty Scholar in Aging Research.
REFERENCES
- 1.Soumerai SB, Ross-Degnan D. Inadequate prescription-drug coverage for Medicare enrollees—a call to action (published erratum appears in N Engl J Med 1999;340:976). N Engl J Med. 1999;340:722–8. doi: 10.1056/NEJM199903043400909. [DOI] [PubMed] [Google Scholar]
- 2.Lagnado L. The uncovered; drug costs can leave elderly a grim choice: pills or other needs. Wall Street Journal. November 17 1998:A1. [Google Scholar]
- 3.Dustan HP, Caplan LR, Curry CL, et al. Report of the Task Force on the Availability of Cardiovascular Drugs to the Medically Indigent. Circulation. 1992;85:849–60. doi: 10.1161/01.cir.85.2.849. [DOI] [PubMed] [Google Scholar]
- 4.Drazen JM, Bush GW, Gore A. The Republican and Democratic candidates speak on health care. N Engl J Med. 2000;343:1184–9. doi: 10.1056/NEJM200010193431611. [DOI] [PubMed] [Google Scholar]
- 5.Shih YC. Effect of insurance on prescription drug use by ESRD beneficiaries. Health Care Financ Rev. 1999;20:39–54. [PMC free article] [PubMed] [Google Scholar]
- 6.Poisal JA, Chulis GS. Medicare beneficiaries and drug coverage. Health Aff. 2000;19:248–56. doi: 10.1377/hlthaff.19.2.248. [DOI] [PubMed] [Google Scholar]
- 7.Poisal JA, Murray L. Growing differences between Medicare beneficiaries with and without drug coverage. Health Aff. 2001;20:74–85. doi: 10.1377/hlthaff.20.2.74. [DOI] [PubMed] [Google Scholar]
- 8.Lillard LA, Rogowski J, Kington R. Insurance coverage for prescription drugs: effects on use and expenditures in the Medicare population. Med Care. 1999;37:926–36. doi: 10.1097/00005650-199909000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Department of Health and Human Services. Report to the President: Prescription Drug Coverage, Spending, Utilization, and Prices. 2000 Available at: http://www.aspe.hhs.gov/health/reports/drugstudy. [Google Scholar]
- 10.Soldo BJ, Hurd MD, Rodgers WL, Wallace RB. Asset and health dynamics among the oldest old: an overview of the AHEAD study. J Gerontol B Psychol Sci Soc Sci. 1997;52:1–20. doi: 10.1093/geronb/52b.special_issue.1. [DOI] [PubMed] [Google Scholar]
- 11.Heeringa S. Technical Description of the Asset and Health Dynamics (AHEAD) Survey Sample Design (Public Use Version) Ann Arbor: University of Michigan Institute for Social Research; 1995. [Google Scholar]
- 12.Smith JP. Wealth inequality among older Americans. J Gerontol B Psychol Sci Soc Sci. 1997;52:74–81. doi: 10.1093/geronb/52b.special_issue.74. [DOI] [PubMed] [Google Scholar]
- 13.Hopp FP, Duffy SA. Racial variations in end-of-life care. J Am Geriatr Soc. 2000;48:658–63. doi: 10.1111/j.1532-5415.2000.tb04724.x. [DOI] [PubMed] [Google Scholar]
- 14.McKinley ED, Garrett JM, Evans AT, Danis M. Differences in end-of-life decision making among black and white ambulatory cancer patients. J Gen Intern Med. 1996;11:651–6. doi: 10.1007/BF02600155. [DOI] [PubMed] [Google Scholar]
- 15.Escarce JJ, Epstein KR, Colby DC, Schwartz JS. Racial differences in the elderly's use of medical procedures and diagnostic tests. Am J Public Health. 1993;83:948–54. doi: 10.2105/ajph.83.7.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blustein J. Drug coverage and drug purchases by Medicare beneficiaries with hypertension. Health Aff. 2000;19:219–30. doi: 10.1377/hlthaff.19.2.219. [DOI] [PubMed] [Google Scholar]
- 17.Stuart B, Grana J. Ability to pay and the decision to medicate. Med Care. 1998;36:202–11. doi: 10.1097/00005650-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Stuart B, Zacker C. Who bears the burden of Medicaid drug copayment policies? Health Aff. 1999;18:201–12. doi: 10.1377/hlthaff.18.2.201. [DOI] [PubMed] [Google Scholar]
- 19.Johnson RE, Goodman MJ, Hornbrook MC, Eldredge MB. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Med Care. 1997;35:1119–31. doi: 10.1097/00005650-199711000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Tamblyn R, Laprise R, Hanley JA. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–9. doi: 10.1001/jama.285.4.421. [DOI] [PubMed] [Google Scholar]
- 21.Lurie N, Ward NB, Shapiro MF, Brook RH. Termination from Medi-Cal—does it affect health? N Engl J Med. 1984;311:480–4. doi: 10.1056/nejm198408163110735. [DOI] [PubMed] [Google Scholar]
- 22.Soumerai SB, Avorn J, Ross-Degnan D, Gortmaker S. Payment restrictions for prescription drugs under Medicaid. Effects on therapy, cost, and equity. N Engl J Med. 1987;317:550–6. doi: 10.1056/NEJM198708273170906. [DOI] [PubMed] [Google Scholar]
- 23.Soumerai SB, Ross-Degnan D, Avorn J, McLaughlin T, Choodnovskiy I. Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med. 1991;325:1072–7. doi: 10.1056/NEJM199110103251505. [DOI] [PubMed] [Google Scholar]
- 24.Soumerai SB, McLaughlin TJ, Ross-Degnan D, Casteris CS, Bollini P. Effects of a limit on Medicaid drug-reimbursement benefits on the use of psychotropic agents and acute mental health services by patients with schizophrenia. N Engl J Med. 1994;331:650–5. doi: 10.1056/NEJM199409083311006. [DOI] [PubMed] [Google Scholar]
- 25.Schweitzer SO, Shiota SR. Access and cost implications of state limitations on Medicaid reimbursement for pharmaceuticals. Annu Rev Public Health. 1992;13:399–410. doi: 10.1146/annurev.pu.13.050192.002151. [DOI] [PubMed] [Google Scholar]
- 26.Pedersen TR, Kjekshus J, Berg K, et al. Cholesterol lowering and the use of healthcare resources. Results of the Scandinavian Simvastatin Survival Study (published erratum appears in Circulation 1996;94:849). Circulation. 1996;93:1796–802. doi: 10.1161/01.cir.93.10.1796. [DOI] [PubMed] [Google Scholar]
- 27.Rosenheck R, Cramer J, Allan E, et al. Cost-effectiveness of clozapine in patients with high and low levels of hospital use. Department of Veterans Affairs Cooperative Study Group on Clozapine in Refractory Schizophrenia. Arch Gen Psychiatry. 1999;56:565–72. doi: 10.1001/archpsyc.56.6.565. [DOI] [PubMed] [Google Scholar]
- 28.Gross DJ, Alecxih L, Gibson MJ, Corea J, Caplan C, Brangan N. Out-of-pocket health spending by poor and near-poor elderly Medicare beneficiaries. Health Serv Res. 1999;34:241–54. [PMC free article] [PubMed] [Google Scholar]
- 29.Rogowski J, Lillard LA, Kington R. The financial burden of prescription drug use among elderly persons. Gerontologist. 1997;37:475–82. doi: 10.1093/geront/37.4.475. [DOI] [PubMed] [Google Scholar]
- 30.Stuart B, Shea D, Briesacher B. Dynamics of drug coverage of Medicare beneficiaires: finders, losers, switchers. Health Aff. 2001;20:86–99. doi: 10.1377/hlthaff.20.2.86. [DOI] [PubMed] [Google Scholar]
- 31.McArdle F, Cappock S, Yamamoto D, Zebrak A. Retiree Health Coverage: Recent Trends and Employer Perspectives on Future Benefits. Menlo Park, Calif: The Henry J. Kaiser Family Foundation; 1999. [Google Scholar]
- 32.Sjahid SI, van der Linden PD, Stricker BH. Agreement between the pharmacy medication history and patient interview for cardiovascular drugs: the Rotterdam Elderly Study. Br J Clin Pharmacol. 1998;45:591–5. doi: 10.1046/j.1365-2125.1998.00716.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rost K, Roter D. Predictors of recall of medication regimens and recommendations for lifestyle change in elderly patients. Gerontologist. 1987;27:510–5. doi: 10.1093/geront/27.4.510. [DOI] [PubMed] [Google Scholar]
- 34.West SL, Savitz DA, Koch G, Strom BL, Guess HA, Hartzema A. Recall accuracy for prescription medications: self-report compared with database information. Am J Epidemiol. 1995;142:1103–12. doi: 10.1093/oxfordjournals.aje.a117563. [DOI] [PubMed] [Google Scholar]
- 35.McKenna MT, Speers M, Mallin K, Warnecke R. Agreement between patient self-reports and medical records for Pap smear histories. Am J Prev Med. 1992;8:287–91. [PubMed] [Google Scholar]
- 36.Brown JB, Adams ME. Patients as reliable reporters of medical care process. Recall of ambulatory encounter events. Med Care. 1992;30:400–11. doi: 10.1097/00005650-199205000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Evans C, Crawford B. Patient self-reports in pharmacoeconomic studies. Their use and impact on study validity. Pharmacoeconomics. 1999;15:241–56. doi: 10.2165/00019053-199915030-00004. [DOI] [PubMed] [Google Scholar]
- 38.Coughlin SS. Recall bias in epidemiologic studies. J Clin Epidemiol. 1990;43:87–91. doi: 10.1016/0895-4356(90)90060-3. [DOI] [PubMed] [Google Scholar]
- 39.Norrish A, North D, Kirkman P, Jackson R. Validity of self-reported hospital admission in a prospective study. Am J Epidemiol. 1994;140:938–42. doi: 10.1093/oxfordjournals.aje.a117182. [DOI] [PubMed] [Google Scholar]
- 40.Yaffe R, Shapiro S, Fuchseberg RR, Rohde CA, Corpeno HC. Medical economics survey-methods study: cost-effectiveness of alternative survey strategies. Med Care. 1978;16:641–59. doi: 10.1097/00005650-197808000-00003. [DOI] [PubMed] [Google Scholar]
- 41.Cleary PD, Jette AM. The validity of self-reported physician utilization measures. Med Care. 1984;22:796–803. doi: 10.1097/00005650-198409000-00003. [DOI] [PubMed] [Google Scholar]
- 42.McCall N, Rice T, Sangl J. Consumer knowledge of Medicare and supplemental health insurance benefits. Health Serv Res. 1986;20:633–57. [PMC free article] [PubMed] [Google Scholar]