Abstract
OBJECTIVES
To understand the nature of patients' expectations for parts of the physical examination and for diagnostic testing and the meaning patients ascribe to their desires.
DESIGN
Qualitative inquiry based on patient interviews and focused on perceived diagnostic omissions as “critical incidents.”
SETTING
Three general internal medicine practices (21 practitioners) in one mid-sized northern California city.
PATIENTS
Of 687 patients visiting these practice sites and completing a detailed questionnaire, 125 reported one or more omissions of care and 90 completed an in-depth telephone interview. This study focuses on the 56 patients interviewed who did not receive desired components of the physical examination or diagnostic tests.
MEASUREMENTS
Qualitative analysis of key themes underlying patients' unmet expectations for examinations and tests, as derived from verbatim transcripts of the 56 interviews.
MAIN RESULTS
The 56 patients perceived a total of 113 investigative omissions falling into four broad categories: physical examination (47 omissions), conventional tests (43), high-cost tests (10), and unspecified investigations (13). Patients considered omitted investigations to have value along both pragmatic and symbolic dimensions. Diagnostic maneuvers had pragmatic value when they were seen to advance the technical aims of diagnosis, prognosis, or therapy. They had symbolic value when their underlying purpose was to enrich the patient-physician relationship. Patients in this study were often uncomfortable with clinical uncertainty, distrusted empiric therapy, endorsed early detection, and frequently interpreted failure to examine or test as failure to care.
CONCLUSIONS
When patients express disappointment at failing to receive tests or examinations, they may actually be expressing concerns about the basis of their illness, the rationale for therapy, or the physician-patient relationship.
Keywords: patient perceptions, tests, patient expectations, examinations
Physicians routinely use the physical examination, selected laboratory tests, and imaging studies in medical decision making.1 However, the use of these tools can be costly in terms of time and resources. Physicians are exhorted to employ only the most efficient diagnostic strategies and to avoid unnecessary examinations and tests.2–4 At the same time, broader public awareness of the benefits of medical technology and an increasingly strident consumerist ethos have raised the stakes for physicians committed to cost-effective care.5–7
Despite the gap in medical knowledge between physicians and laypersons, patients can identify specific interventions they consider necessary.8–12 Research suggests that visit satisfaction suffers8 and health-related worry increases13 when desired diagnostic interventions are not received. Nonetheless, uncritical compliance with patients' requests would be unprofessional and arguably unethical.14
Engaging patients in a clinical negotiation in which patients and physicians share their concerns, discuss areas of contention, and reach a mutually agreeable conclusion can enhance the patient-physician relationship and increase patients' participation in their own care.15,16 This process has itself been associated with improved physiological and functional outcomes.17,18 The clinician who is aware of the nature of patients' desires and the personal meaning patients ascribe to them will be in a better position to negotiate productively around visit content. A systematic study of patients' unmet expectations for diagnostic investigations would create a context for understanding this important aspect of the physician-patient relationship.
The current study relies on the same data set as a previously published manuscript.19 In that article, we reported that patients had unmet expectations for care in about 20% of medical encounters and that these expectations could generally be traced to four sources: current somatic symptoms, perceived vulnerability to illness, past experiences, and acquired knowledge. However, that study was broadly focused on the entire spectrum of patients' expectations (ranging from history taking to counseling) and did not address the question that motivates this article: When patients seek investigation of their symptoms by hinting at, requesting, or demanding various diagnostic maneuvers, what are they really after?
We framed the current investigation in terms of the following two research questions. First, what is the nature of patients' unmet expectations for the physical examination and for diagnostic testing in primary care? (In this context, we define “unmet expectations” as medical services patients deem necessary or possibly necessary but which are not received.) Second, what meaning do patients ascribe to these expectations and desires? What value do they place on the desired services and how do they interpret physicians' failure to provide them? Insights gained from pursuing these questions may be useful both to clinicians seeking more effective strategies for clinical negotiation and to administrators contemplating policies that affect delivery of diagnostic services.
METHODS
Sampling of Practices and Patients
The sampling methods used in this study have been described previously.19 Briefly, the study was conducted within three general internal medicine practices in Sacramento, Calif (metropolitan population, 1.6 million). Two practices (employing 13 clinicians) were branch offices of a large group-model HMO. The third practice consisted of eight general internists (two with further subspecialty training) and one nurse practitioner, affiliated with a large nonacademic multispecialty group, working within a single private office, and compensated by a combination of salary and bonuses for productivity. Patients in this practice were insured under a variety of prepaid and fee-for-service plans. All three practices scheduled patients with their own regular practitioner whenever possible.
These practices represent the dominant models of care in northern California, an area heavily penetrated by managed care.20 Because managed care providers may have financial incentives to restrict medical care, managed care settings are potentially ripe for conflict between patients' expectations of receiving potentially costly investigations and the willingness of clinicians to perform or obtain them.7 In addition, time constraints may limit opportunities to meet patients' expectations for more complete physical examinations.21
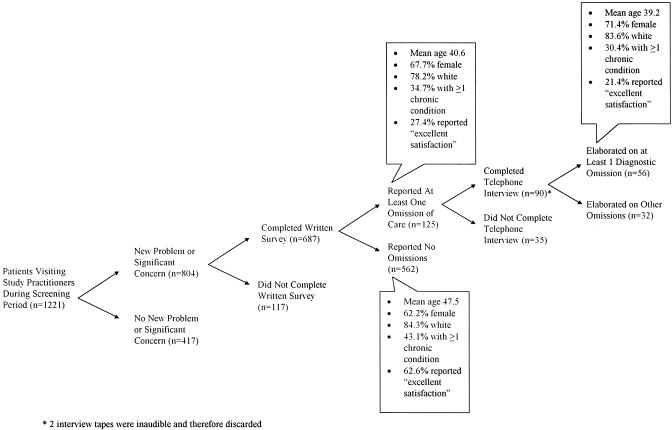
Administration of the Screening Survey
As previously described,18 trained research assistants approached patients in waiting rooms during a total of 36 half-day clinic sessions in late 1994 and encouraged them to complete a brief form. The form asked two questions: (1) Do you have a new or worsening problem that you wish to discuss with the doctor today (yes or no)? and (2) How concerned are you that you might have an undiagnosed serious condition (not at all, not very, somewhat, very, extremely)? The flow of patients through the study is diagrammed in Figure 1. Of 1,221 patients completing the form, 804 reported a new or worsening problem or were at least somewhat concerned about an undiagnosed condition and were thus eligible for further study. Of the eligible patients, 687 (85%) consented to participate further and completed a postvisit questionnaire about demographic characteristics, recent health care utilization, health status, visit satisfaction, and perceived omissions of care. Of respondents, 62% were seeing their own regular provider, while the remainder were seen on an urgent basis by some other practitioner.
FIGURE 1.
Allocation of patients to study groups.
The core of the written survey was a set of eight questions about perceived omissions of care (“things you felt were necessary for the doctor to do today but which, for whatever reason, didn't happen”). Patients could endorse (check off) any of eight categories of putative omissions: preparation for the visit; history taking; physical examination; laboratory testing or diagnostic imaging; medication prescribing; specialty referral; information, counseling, or personal help; and “anything else.”
Of the respondents, 125 (18%) reported one or more omissions; 108 (86%) of these gave written consent for a telephone interview. The lead author interviewed 90 of the 108 patients within 7 days of the visit (the other 18 were telephoned at least four times but could not be reached). The interviewer identified himself as a “researcher from UC Davis” but not as a physician unless specifically asked. Interviewing used the critical incident technique22 to focus on patients' accounts of events that actually happened rather than on speculation or general opinions.23,24 In this case, the critical incident was the perceived omission. Thus, the opening question was, “You mentioned on your questionnaire that you were hoping that the doctor would [perform a particular intervention], but that didn't happen. Can you tell me more about that?” Subsequent questions explored why patients considered the omitted services necessary (including the expected benefits), whether they communicated their desires explicitly, and what they thought motivated the doctor in failing to deliver the desired services. Patient interviews averaged 15 minutes; 88 of the 90 interviews were successfully tape-recorded and transcribed.
Data Transformation
Qualitative analysis of the data was performed in two stages. In the first stage, using coding methods described elsewhere,19 we identified 56 transcripts (64%) in which patients reported on one or more omitted diagnostic maneuvers (i.e., omission of a portion of the physical examination, a laboratory test, an imaging study, or an unspecified diagnostic maneuver). Owing to the structure of the interviews (with a standardized opening question), the type of perceived omission could generally be ascertained by reading the first few lines of each transcript. In a random sample of nine transcripts, the first and second authors reached 100% agreement on the presence or absence of specific perceived diagnostic omissions.
In the second stage of the analysis, both authors re-read all 56 transcripts, noting especially the nature of the perceived omissions and how patients justified their (unmet) expectations. Each author brought the perspectives of his discipline to these readings. Dr. Kravitz is a general internist in academic practice. Dr. Callahan is a clinical psychologist with an academic appointment in a department of family medicine. Both see patients in the highly managed Sacramento, Calif, environment. During a series of meetings conducted over several months, the investigators reached consensus on the interpretation of patients' remarks and the salience of key themes. Neither investigator sought to impose a specific theoretical framework on the data; rather, key themes were grounded in the data and emerged over time via multiple readings. Although formal triangulation was not performed, themes were validated in a series of patient and physician focus groups in November 1995, departmental seminars in 1995–96, and national presentations in 1996–97.
RESULTS
Characteristics of Patients Reporting Omitted Investigations
Among patients completing the written survey (n = 687), those reporting any omission of care (n = 125) were significantly younger (p = .006) and less satisfied (p = .0001) than those who reported no omissions (n = 562) (Fig. 1). The 56 patients who perceived and elaborated on diagnostic omissions were generally indistinguishable from the larger group of 125, except that proportion rating care as “excellent” or better was lower (21% vs 27%, Fig. 1).
Distribution of Perceived Diagnostic Omissions
Fifty-six of the 88 patients for whom usable telephone interviews were available reported a total of 113 diagnostic omissions (Table 1). Nearly four fifths of the 113 complaints alleged failure to perform parts of the physical examination or to order relatively inexpensive laboratory tests or plain radiographs; less than 10% involved omission of higher-cost tests such as magnetic resonance imaging (MRI) scans or cardiac stress tests. Failure to check vital signs; to inspect the eyes, ears, nose and throat; and to auscultate the heart and lungs accounted for 60% of physical examination omissions (Table 1). In just under 10% of reports, patients stated that the physician should have “done more testing” or “looked into my problem more thoroughly” but did not specify the diagnostic omission more precisely.
Table 1.
Prevalence of Perceived Investigative Omissions
| Omission Category | Number of Omitted Investigations (Number of Patients) |
|---|---|
| Physical examination components | 47 (33) |
| HEENT* | 9 |
| Heart | 8 |
| Chest/lungs | 6 |
| Vital signs | 6 |
| Other component (or unspecified) | 14 |
| Complete physical exam | 4 |
| Conventional tests | 43 (36) |
| Plain radiographs | 12 |
| Blood tests | 12 |
| Urine tests | 5 |
| Microbiological cultures | 5 |
| Other or unspecified | 9 |
| Costly tests† | 10 (10) |
| Unspecified diagnostic maneuvers | 13 (13) |
HEENT indicates head, eyes, ears, nose, and throat examination.
Magnetic resonance imaging, computed tomography, and cardiac stress testing (with or without imaging).
Perceived Value of Omitted Investigations
During the telephone interviews, patients were encouraged to describe the perceived diagnostic omission in detail, elaborate on their views of the omitted procedure, and explain why it would have been helpful. In reviewing the transcribed interviews, we analyzed all statements that related to the perceived value, purpose, or function of the alleged diagnostic omission. We sorted the statements into categories, modifying the categories iteratively as more statements were analyzed. After several iterations, we agreed on five domains reflecting two dimensions (Table 2). Summaries of the categories that emerged from study of patient transcripts follow.
Table 2.
Perceived Value of Diagnostic Investigations
| Domain | Value, Purpose, or Function | Example |
|---|---|---|
| Pragmatic | ||
| Prevention | Promote health | ”He didn't suggest blood work or urinalysis of any kind. I am a relatively healthy person but I would like to stay that way.” |
| Detect potentially serious disease before it becomes unmanageable (diffuse concern) | ”He didn't look in my eyes, my fingernails, he didn't check my temperature… Hell, I'm 68 years old and things can happen.” | |
| Detect potentially serious disease before it becomes unmanageable (narrow concern) | ”This is the second time I have had the basal cell problem on my face… and he doesn't check my face.” | |
| Diagnosis | Clarify cause of symptoms | ”The antibiotic would have been the same… So I think the treatment may not have changed, but I wanted a more definitive answer of what was wrong. |
| Define anatomic source of symptoms | ”He didn't look in my ears, which I thought was odd considering it was dizziness.” | |
| Confirm specific diagnostic hypothesis | ”I don't know what kind of checking would be done for migraines, but it should be some kind of test.” | |
| Confirm specific pathophysiologic hypothesis | ”I thought something on x-ray might show some sort of inflammation that is not being tended to.” | |
| Provide an alternative explanation | ”I am getting a lot of leg, foot, and lower back pain and I was hoping she would refer me for an MRI. She seems to attribute the pain to my diabetes but I [doubt it].” | |
| Provide a personal (hypothetico-deductive) rather than statistical (probabilistic) diagnosis | ”I wanted a blood test because how else can you find out what's going on with me personally?” | |
| Disease monitoring | Assess status of chronic condition | ”So I feel that having a heart condition where I take two drugs for it that he automatically should listen to the heart and lungs when I go in.” |
| Monitor chronic therapy | ”You are supposed to have blood work every 3 months if you take this arthritis medicine.” | |
| Disease management | Guide therapy | ”I just figure if you have an infection you would need to know what kind of germs you were dealing with to know the appropriate medication.” |
| Symbolic | Demonstrate interest in the patient's problem | ”It's like he had his mind made up before he even walked into the room.” |
| Validate concerns | ”I was hoping she would do a range of motion exam and actually feel my joints because it is so uncomfortable for me… It warranted more than just, ‘Well, let’s talk about it in 2 weeks.'” | |
| Demonstrate an empathic connection | ”Having my heart and lungs checked is why I go to him… He never did anything! He never touched me in any way.” | |
| Establish clinical credibility | ”The last time I went into the doctor they said I had a little bit of [ear] wax buildup; I went in again and they said it was getting there; this time she didn't even look at it.” | |
| Provide specific reassurance | ”I just want to make sure it's not pneumonia. Walking pneumonia killed my father and I know the best way to tell if I have pneumonia is with a chest x-ray.” | |
| Reduce future “chagrin” | ”I screamed and told them that at work there was a guy that went in for a bunion and he lost the toe 3 months later. I said, ‘You people going to wait until I lose my hearing?’” |
The analysis revealed that patients in our study considered omitted examinations, laboratory tests, and imaging studies to have both pragmatic and symbolic value (Table 2). Maneuvers had pragmatic value when they were perceived to affect the diagnostic process, provide prognostic information, or influence disease outcomes. Patients perceived such interventions to have merit because they advanced practical objectives consistent with the goals of scientific medicine. Interventions had symbolic value when their claim to the patients' attention lay primarily with the physician-patient relationship.
Perceived Value of Omitted Investigations
Pragmatic Dimensions
Patients' views concerning the pragmatic (biomedical) significance of diagnostic maneuvers were classified as pertaining to prevention, diagnosis, disease monitoring, and disease management (Table 2). Patients ascribed to these interventions the power to promote health, detect subclinical disease, define the basis of symptoms, monitor the status of a disease or its therapy, or direct therapeutic decisions. Although patients' suppositions about the role of examinations and tests often aligned with common sense, they were sometimes simplistic (“I thought an x-ray might show some sort of inflammation that is not being tended to”) or dogmatic (“You are supposed to have blood work every 3 months if you take this arthritis medicine”).
One way patients assessed the need for diagnostic and monitoring procedures (especially radiographic procedures) was to create a mental picture based on a mechanical model of disease. These images could be powerful compared with the more abstract formulations common to clinical medicine. For example, one 56-year-old woman reported: “I have degenerative disk disease and the nerves get mashed and it's real painful… Nobody has ever x-rayed it because the doctor said if they x-ray it, that will make me believe that that's why I have the pain and it's not possible… that it's from my spine and it really can't be.” This patient's request flowed out of her understanding of the disease process but conflicted with the physician's recognition that radiographic evidence of degenerative arthritis often coexists with back pain without being causal.
Another crosscutting theme was discomfort with statistical or probabilistic diagnosis. The probabilistic approach—in which the decision to test or treat is determined by the expected utilities of the alternative strategies and thus by their relative benefits and risks—is well supported by the medical decision-making literature,25 but was greeted skeptically by patients. As one put it, “I wanted a blood test because how else can you find out what's going on with me personally?” While the physician may have considered concepts such as sensitivity, specificity, and prior probability in deciding whether to test or treat empirically, the patient wanted a personal diagnosis. Another patient reported that she was told her hand cramps were “maybe a circulation problem…but he [the doctor] wanted to give me some medication. Well, I would like to find out first if this is a circulation problem before I start taking medication for something.” A third individual (a 33-year-old woman with headaches) commented, “I thought maybe if they did blood work they would find something other than just giving me narcotics to kill the pain… Let's do something and figure out why it's happening, as opposed to, ‘Oh, you are getting migraines, so take these drugs.’”
Symbolic Dimensions
In addition to pragmatic dimensions considered above, patients often perceived examinations and tests to have value that transcended their potential contribution to diagnosis, prognosis, and therapy (Table 2). Diagnostic investigations were seen as a way in which clinicians could demonstrate interest in the patients and their problems, validate their concerns, demonstrate an empathic connection, establish clinical credibility, provide specific reassurance, and reduce the odds of future chagrin (Table 2).
Failure to examine a body part or order a laboratory test could suggest lack of interest in the patient as a person. One 38-year-old woman, for example, complained: “My rash was real bad. I think they should have run some tests on me but they didn't… If somebody walks in that a doctor really likes, or a relative or somebody like that, they would give them the shot. They would do more than just say here's some cream… I'm just a patient. Nobody they care about.” Another young woman was more succinct: “I just did not feel like the physician cared about me as an individual.”
For patients seeking validation of their concerns, the physician's failure to probe, test, or examine could mean their concerns were unfounded or illegitimate. As one patient put it, “I was hoping she would do a range-of-motion exam and actually feel my joints because it is so uncomfortable for me… It warranted more than just, ‘Well, let’s talk about it in 2 weeks.'” While this statement reflects pragmatic concerns (the patient thought a joint examination might rule out serious underlying disease), it also highlights the patient's sense that important symptoms were not being taken seriously.
Empathy could be established both verbally and nonverbally. Touch was particularly important, as illustrated in these four brief extracts:
[68-year-old male] “He didn't do anything. He never touched me in any way. Then I brought up the fact that I was sure his nurse had made a mistake on my pulse and he grabbed my wrist and held it for maybe 15 seconds and said, ‘Oh, that feels about right.’”
[47-year-old female] “[He should] at least touch my body in some way.… He was actually very affable; however, he didn't look in my ears, which I thought was odd considering it was dizziness.”
[59-year-old female] “He didn't touch me. I have been having symptoms of dizziness and everything. He came in and talked to me and that was all. He didn't listen to my heart, my lungs, or anything.”
[38-year-old female] “I would get dizzy and my right arm would get numb and strange things like that would happen. So, the guy comes in and looks at me, asks a few questions, and says, ‘I think you have an inner ear problem.’ He didn't even look at me. He didn't even touch my body. He doesn't do anything.”
In examples 2 and 3, touch is explicitly assigned a higher value than relational skills. In these two cases, willingness to talk (even “affably”) is no substitute for a careful viewing of the eardrums and auscultation of the heart and lungs.
Some patients looked to diagnostic maneuvers as evidence of their physician's clinical credibility. For example, a patient seeing an unfamiliar clinician for evaluation of acute back spasms was perturbed that the physician failed to follow-up on a previously noted problem. “The last time I went into the doctor they said I had a little bit of wax buildup and might want to get that scraped out. I went in again, and they checked it again, and they said it was getting there but I didn't need it yet. I went in this time and she didn't even look at it.” Experience during at least two prior visits led the patient to expect that her ears would be checked routinely; in departing from this expected routine, the clinician evoked doubts about her diligence or competence.
Patients sometimes sought specific reassurance that they did not have a dread disease; examinations and tests were a way to rule out particular concerns. For example, a young man with cough wanted a chest x-ray to make sure he was not developing pneumonia, to which his father had recently succumbed (see quote, Table 2).
The “chagrin factor” has been proposed as an explanation for why physicians order tests to detect devastating but unlikely conditions.26 According to this theory, physicians anticipate how badly they will feel if a serious diagnosis is missed, so they order unnecessary tests to minimize the potential psychological discomfort. We found some evidence that patients also try to reduce future chagrin. For example, a 59-year-old woman had to wait 6 weeks before seeing a specialist for pressure in the ears. While the primary care team apparently saw no urgency in referring a case of presumed otitis media with effusion, the patient was obsessed with the possible consequences of delay. “I told them that at work there was a guy that went in for a bunion and they screwed it up so bad that he lost the toe 3 months later. I said, ‘You people going to wait until I lose my hearing and then do something?’”
Expressions of Entitlement
Managed health care has been criticized for promising much to the healthy while delivering relatively less to the sick.27–29 Therefore, we were surprised that only 1 of 56 patients couched concerns about omitted care in the language of entitlement. This patient was upset over his physician's failure to order an MRI scan for chronic back pain. “They have the money already. It's paid through my insurance, but when you go to get something done they refuse to do it.” While other patients commented on the possible role of managed care and health insurance in shaping their physicians' clinical judgments, they always offered an alternative rationale (beyond simple economic entitlement) for seeking diagnostic studies.
Omitted Care and the Dynamics of Human Judgment
Research on patient assessments of care (e.g., patient satisfaction research) often assumes that patients form stable judgments about their care immediately after the visit.30,31 Two patients in our series challenged this assumption. One 32-year-old female patient presented with a sore, swollen cervical lymph node. The physician performed a brief physical examination and ordered a throat culture, and the patient was, by her account, perfectly satisfied. By the time we spoke with her 2 days later, however, the throat culture had returned negative, and the patient was concerned that the examination “should have been more thorough.” In contrast, a patient with symptoms of sinusitis was initially annoyed that the physician failed to examine his nose and sinuses (and conveyed his annoyance on the postvisit questionnaire). However, by the time of our telephone call, his symptoms had resolved in response to a prescribed antibiotic, and he was completely satisfied with his care.
DISCUSSION
In a survey of 687 ambulatory care encounters, we identified 56 patients (about 8%) with unmet expectations for diagnostic tests and examinations. During extended interviews, these patients not only lamented lost opportunities for precise diagnosis (pragmatic dimension) but also expressed unease over the relational implications of the perceived omissions (symbolic dimension). Awareness of both dimensions is necessary to appreciate the patient perspective on the examination or test “not taken.”
Failure to perform part of the physical examination or to obtain relatively inexpensive tests or x-rays accounted for 90 (80%) of 113 reported omissions. Concern about failure to order more costly tests such as computed tomography or MRI were uncommon. As a result, the financial value of disputed resources was relatively small on a per-case basis. Consistent with this observation, patients rarely had their explicit requests refused; rather, most patients failed to articulate to the physician what it was they were hoping to receive.
Patients' perceptions of the pragmatic value of diagnostic studies were generally reasonable and consistent with conventional medical wisdom. For example, the view that early periodic examination or testing can “catch disease early” and avert future complications (a theme sounded repeatedly in our study) is the premise underlying many screening programs and has been advocated fiercely by organizations such as the American Cancer Society. However, patients did not always get the details right.
Many patients constructed pathophysiologic models (“mental representations of illness”)32 as an aid to understanding their symptoms. Although patients' models were frequently plausible, they sometimes conflicted with the scientific evidence, the physicians' interpretation of the evidence, or both. Discordant models appeared to underlie several cases of patient-physician conflict. These observations highlight the difficulty in communicating complex medical information to lay persons,33,34 especially when scientific data or epidemiologic principles are inconsistent with a simple anatomic or mechanical explanation.
From the physician's perspective, the principal value of diagnostic maneuvers is to determine the probability of conditions considered in the differential diagnosis as developed from the clinical interview.1 From the patient's perspective, these maneuvers may simultaneously address factual questions (What do I have?) and psychosocial needs (Does my doctor care about me?). Physicians ignore these symbolic dimensions at their peril because they are powerfully associated with patients' evaluations of their care.35–37
The results must be interpreted in context. The study was done in three practices within two health care systems in one geographic region of the United States. Although neither system linked physician compensation directly to laboratory utilization or referral profiles, cost-effective practice was encouraged through a combination of queuing (in the HMO), internal utilization review (in the private medical group) and cultural norms (in both systems).
In summary, on the basis of our interview findings, we suggest that patients with unmet expectations for diagnostic services in primary care share a belief system organized around three principles:
Doctors ought to know what's wrong before they try to fix it. Some patients had great faith in the power of diagnostic maneuvers to identify the root cause of an illness and a corresponding mistrust of empiric therapy. “You don't doctor the symptoms and don't give me medicine for something that you don't know for sure.” The physician considering initiation of a therapeutic trial in these patients must carefully explain the rationale if he or she expects the patient to embrace the clinical “experiment.” It may be worthwhile to determine the acceptability of a proposed course of treatment by inquiring directly, “How does that seem to you?” By carefully observing the patient's reactions (verbal and nonverbal), the physician can determine how much more explanation (or testing) is necessary.
By the time symptoms appear, it might be too late. The message that early, preclinical detection of disease saves lives and reduces disability has been widely disseminated by public health authorities, self-help organizations, HMOs, and the medical profession. Our data indicate that part of the listening public has taken heed. Implicitly, the “cult of early detection” encourages patients to distrust both their bodies (which may not signal disease through symptoms until serious damage has occurred) and their physicians. Simultaneously, patients may develop unrealistic beliefs about the curative powers of modern medicine (as long as we “catch it early”) and may discount the value of “watchful waiting.” Physicians will have a hard time combating the early detection message for several reasons (not least of which because the message is sometimes appropriate), but they should be aware of its ubiquity and the propensity of patients to misapply it. As has been suggested elsewhere,38 they might also ask their patients about specific diagnostic concerns: for example, “Many patients have ideas about what might be going on with them. Have you had any thoughts or worries about what might be causing your symptoms?”
If my doctor cared enough about me, he/she would investigate my symptoms more thoroughly. Our data clearly illustrate the symbolic, interpersonal functions of the physical examination and diagnostic testing. What remains unclear is whether the dissatisfaction resulting from perceived withholding of diagnostic studies is potentially containable through dialogue. In this study, we were unable to determine whether a more extended clinical interview or a more detailed explanation might have assuaged patients whose ostensible complaint was failure to examine or test; more research is needed. Nevertheless, it may be worthwhile to inquire about patients' unmet expectations by asking, repeatedly, if necessary, “Anything else you were hoping I would do today?” With reticent patients, some persistence may be required, but once the agenda is on the table, clinicians can attempt to negotiate a plan that satisfies the patient's need to feel cared for while avoiding unnecessary or premature testing.
In conclusion, patients' unmet expectations for diagnostic investigations can potentially color their evaluations of the quality of care received and distort the physician-patient relationship. Such clinical discord is likely to increase as patient consumerism continues to meet the imperatives of cost containment. Physicians may be able to handle such potential conflict by inquiring about patients' fears, checking out the acceptability of proposed clinical strategies, and asking directly about possible omissions of care. Even in instances of overt disagreement, understanding the pragmatic and symbolic dimensions of patients' expectations may enhance the process of clinical negotiation by laying bare the sources of conflict.
Acknowledgments
The authors thank Margo DeLong for transcription of the audiotapes; JaNahn Scalapino, MD, Marcia Dunham, MD, and Deirdre Antonius, BS, for help with data collection; Martin Shapiro, MD, PhD, and Benjamin Crabtree, PhD, for helpful comments on an earlier draft of this manuscript; and Charles Lewis, MD, ScD, for general guidance and mentorship. Dr. Kravitz was a Picker/Commonwealth Faculty Scholar at the time this work was initiated.
REFERENCES
- 1.Cutler P. Problem Solving in Clinical Medicine. Baltimore, Md: Williams & Wilkins; 1979. [Google Scholar]
- 2.Praiss I, Gjerde C. Cost containment through medical education. JAMA. 1980;244:53–5. [PubMed] [Google Scholar]
- 3.Eisenberg JM. The internist as gatekeeper: preparing the general internist for a new role. Ann Intern Med. 1985;102:537–43. doi: 10.7326/0003-4819-102-4-537. [DOI] [PubMed] [Google Scholar]
- 4.Shulkin DJ, Rosenstein AH. Promoting cost-effective physician behavior. Healthc Financ Manage. 1993;47:48,50,52–4. [PubMed] [Google Scholar]
- 5.Bastian H. Speaking up for ourselves: the evolution of consumer advocacy in health care. Int J Technol Assess Health Care. 1999;4:127–8. doi: 10.1017/s0266462300010485. [DOI] [PubMed] [Google Scholar]
- 6.Consumerism rampant: a critique of the view of medicine as a commercial enterprise Mt Sinai J Med. 1993;60:15–9. [PubMed] [Google Scholar]
- 7.Gallagher TH, Lo B, Chesney M, Christensen K. How do physicians respond to patients' requests for costly, unindicated services? J Gen Intern Med. 1997;12:663–8. doi: 10.1046/j.1525-1497.1997.07137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kravitz RL, Cope DW, Bhrany V, Leake B. Internal medicine patients' expectations for care during office visits. J Gen Intern Med. 1994;9:75–81. doi: 10.1007/BF02600205. [DOI] [PubMed] [Google Scholar]
- 9.Joos SK, Hickam DH, Borders LM. Patients' desires and satisfaction in general medicine clinics. Public Health Rep. 1993;108:751–9. [PMC free article] [PubMed] [Google Scholar]
- 10.Brody DS, Miller SM, Lerman CE, Smith DG, Lazaro CG, Blum MJ. The relationship between patients' satisfaction with their physicians and perceptions about interventions they desired and received. Med Care. 1989;13:562–9. doi: 10.1097/00005650-198911000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Good MJD, Good BJ, Nassi AJ. Patient requests in primary health care settings: development and validation of a research instrument. J Behav Med. 1983;6:151–68. doi: 10.1007/BF00845378. [DOI] [PubMed] [Google Scholar]
- 12.Marple RL, Kroenke K, Lucey CR, Wilder J, Lucas CA. Concerns and expectations in patients presenting with physical complaints: frequency, physician perceptions and actions, and 2-week outcome. Arch Intern Med. 1997;157:1482–8. [PubMed] [Google Scholar]
- 13.Sox HC, Marguiles I, Sox CH. Psychologically mediated effects of diagnostic tests. Ann Intern Med. 1981;95(6):680–5. doi: 10.7326/0003-4819-95-6-680. [DOI] [PubMed] [Google Scholar]
- 14.LaCombe MA. What is it patients want? Am J Med. 1995;99:588–9. doi: 10.1016/s0002-9343(99)80242-3. [DOI] [PubMed] [Google Scholar]
- 15.Lazare A, Eisenthal S, Frank A. A negotiated approach to the clinical encounter, II: conflict and negotiation. In: Lazare A, editor. Outpatient Psychiatry: Diagnosis and Treatment. Baltimore, Md: Williams & Wilkins; 1979. In: [Google Scholar]
- 16.Botelho RJ. A negotiation model for the doctor-patient relationship. Fam Pract. 1992;9:210–8. doi: 10.1093/fampra/9.2.210. [DOI] [PubMed] [Google Scholar]
- 17.Greenfield S, Kaplan S, Ware JE. Expanding patient involvement in care: effects on patient outcomes. Ann Intern Med. 1985;102:520–8. doi: 10.7326/0003-4819-102-4-520. [DOI] [PubMed] [Google Scholar]
- 18.Bertakis KD, Callahan EJ, Helms LJ, Azari R, Robbins JA, Miller J. Physician practice styles and patient outcomes: differences between family practice and general internal medicine. Med Care. 1998;36:879–91. doi: 10.1097/00005650-199806000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Kravitz RL, Callahan EJ, Paterniti D, Antonius D, Dunham M, Lewis CE. Prevalence and sources of patients' unmet expectations for care. Ann Intern Med. 1996;125:730–7. doi: 10.7326/0003-4819-125-9-199611010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Miller RH, Lipton HL, Duke KS. Health System Change in the Greater Sacramento Area. Sacramento, Calif: Sierra Health Foundation; 1997. June. [Google Scholar]
- 21.Lowes RL. Are you expected to see too many patients? Med Econ. 1995;72:52–3. 57–9. [PubMed] [Google Scholar]
- 22.Flanagan JC. The critical incident technique. Psychol Bull. 1954;51:327–58. doi: 10.1037/h0061470. [DOI] [PubMed] [Google Scholar]
- 23.Bradley CP. Uncomfortable prescribing decisions: a critical incident study. BMJ. 1992;304:294–6. doi: 10.1136/bmj.304.6822.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bradley CP. Turning anecdoetes into data—the critical incident technique. Fam Pract. 1992;9:98–103. doi: 10.1093/fampra/9.1.98. [DOI] [PubMed] [Google Scholar]
- 25.Sox HC, Blatt MA, Higgins MC, Marton KI. Medical Decision Making. Boston, Mass: Butterworth Publications; 1988. [Google Scholar]
- 26.Feinstein AR. The ‘chagrin factor’ and qualitative decision analysis. Arch Intern Med. 1985;145(7):1257–9. [PubMed] [Google Scholar]
- 27.Ware Je, Jr, Brook RH, Rogers WH, et al. Comparison of health outcomes at a health maintenance organisation with those of fee-for-service care. Lancet. 1986;1(8488):1017–22. doi: 10.1016/s0140-6736(86)91282-1. [DOI] [PubMed] [Google Scholar]
- 28.Ware JE, Jr, Bayliss MS, Rogers WH, Kosinski M, Tarlov AR. Differences in 4-year health outcomes for elderly and poor, chronically ill patients treated in HMO and fee-for-service systems: results from the Medical Outcomes Study. JAMA. 1996;276:1039–47. [PubMed] [Google Scholar]
- 29.McCall TB. Some HMOs are bad news. (Is yours?) Redbook. 1996;187(4):47,48. [Google Scholar]
- 30.Rosenthal GE, Shannon SE. The use of patient perceptions in the evaluation of health-care delivery systems. Med Care. 1997;35(11 suppl):NS58–68. doi: 10.1097/00005650-199711001-00007. [DOI] [PubMed] [Google Scholar]
- 31.Kravitz RL. Patients' expectations for medical care: an expanded formulation based on review of the literature. Med Care Res Rev. 1996;53:3–27. doi: 10.1177/107755879605300101. [DOI] [PubMed] [Google Scholar]
- 32.Skelton JA, Croyle RT, editors. Mental Representation in Health and Illness. New York, NY: Springer-Verlag; 1991. [Google Scholar]
- 33.Kee F. Patients' prerogatives and perceptions of benefit. BMJ. 1996;312(7036):958–60. doi: 10.1136/bmj.312.7036.958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mazur DJ, Merz JF. Patients' interpretations of verbal expressions of probability: implications for securing informed consent to medical interventions. Behav Sci Law. 1994;12(4):417–26. doi: 10.1002/bsl.2370120410. [DOI] [PubMed] [Google Scholar]
- 35.Froehlich GW, Welch HG. Meeting walk-in patients' expectations for testing: effects on satisfaction. J Gen Intern Med. 1996;11:470–4. doi: 10.1007/BF02599041. [DOI] [PubMed] [Google Scholar]
- 36.Rose G, Segesten K. Someone who cares—patients' experiences concerning health examinations. Scand J Caring Sci. 1995;9:105–12. doi: 10.1111/j.1471-6712.1995.tb00396.x. [DOI] [PubMed] [Google Scholar]
- 37.McLeod PJ, Tamblyn R, Benaroya S, Snell L. Faculty ratings of resident humanism predict patient satisfaction ratings in ambulatory medical clinics. J Gen Intern Med. 1994;9:321–6. doi: 10.1007/BF02599179. [DOI] [PubMed] [Google Scholar]
- 38.Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood. Arch Gen Psychiatry. 1975;32:553–8. doi: 10.1001/archpsyc.1975.01760230019001. [DOI] [PubMed] [Google Scholar]