Abstract
OBJECTIVE
To assess the effect of hospital discharge against medical advice (AMA) on the interpretation of charges and length of stay attributable to alcoholism.
DESIGN
Retrospective cohort. Three analytic strategies assessed the effect of having an alcohol-related diagnosis (ARD) on risk-adjusted utilization in multivariate regressions. Strategy 1 did not adjust for leaving AMA, strategy 2 adjusted for leaving AMA, and strategy 3 restricted the sample by excluding AMA discharges.
SETTING
Acute care hospitals.
PATIENTS
We studied 23,198 pneumonia hospitalizations in a statewide administrative database.
MEASUREMENTS AND MAIN RESULTS
Among these admissions, 3.6% had an ARD, and 1.2% left AMA. In strategy 1 an ARD accounted for a $1,293 increase in risk-adjusted charges for a hospitalization compared with cases without an ARD ( p = .012). ARD-attributable increases of $1,659 ( p = .002) and $1,664 ( p = .002) in strategies 2 and 3 respectively, represent significant 28% and 29% increases compared with strategy 1. Similarly, using strategy 1 an ARD accounted for a 0.6-day increase in risk-adjusted length of stay over cases without an ARD ( p = .188). An increase of 1 day was seen using both strategies 2 and 3 ( p = .044 and p = .027, respectively), representing significant 67% increases attributable to ARDs compared with strategy 1.
CONCLUSIONS
Discharge AMA affects the interpretation of the relation between alcoholism and utilization. The ARD-attributable utilization was greater when analyses adjusted for or excluded AMA cases. Not accounting for leaving AMA resulted in an underestimation of the impact of alcoholism on resource utilization.
Keywords: hospitalization, patient discharge; patient dropouts; alcoholism; pneumonia; fees and charges
Few studies of resource utilization pay particular attention to the relatively small numbers of patients that leave the hospital against medical advice (AMA).1 Discharges AMA can be expected to decrease the duration and cost of a hospitalization. But discharges AMA could affect the interpretation of resource utilization attributable to particular patient characteristics or comorbidities. The impact of discharges AMA is likely to be greater when the goal of an analysis is to understand resource utilization attributable to patient characteristics that are also associated with leaving AMA. Such characteristics might include not having health insurance, or clinical factors such as alcohol or drug abuse.2–8
Many studies have shown that alcoholism is associated with increased health care resource utilization.9–11 Because patients with alcoholism may be more likely to leave the hospital AMA, we hypothesized that resource utilization attributable to alcoholism may be underestimated when AMA discharges are not considered in the analyses. Therefore, to assess the effect of AMA discharge on interpretations of resource utilization attributable to alcoholism, we compared three analytic strategies: (1) no adjustment for AMA, (2) adjustment for AMA, and (3) restriction of the analysis to cases that did not leave AMA. We focused analyses on cases with a common medical diagnosis, pneumonia.
METHODS
Study Population
The study population was selected from the fiscal year 1992 database of the Massachusetts Health Data Consortium, Inc.12 It included (1) all cases with pneumonia admitted to acute care hospitals in Massachusetts, and (2) for Massachusetts residents, all cases with pneumonia admitted to acute care hospitals in the six bordering states (Connecticut, New York, Rhode Island, Vermont, New Hampshire, and Maine). This database consists of hospital discharge abstract data routinely collected by the Massachusetts Rate Setting Commission and includes up to 15 International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coded diagnoses.13 The data are standardized and checked for accuracy to produce a uniform data set.
Cases were included if they were over 17 years of age and had an ICD-9-CM principal diagnosis of pneumonia as defined by Fine et al.14 Cases were excluded when the total charge for a hospitalization was less than or equal to $1 (all excluded hospitalizations were veterans' hospitals or facilities outside Massachusetts). Cases were also excluded when the source of admission was another acute care hospital, an intermediate care facility, or a skilled nursing facility. Cases admitted from these facilities were excluded to create an inception cohort in which patients were at similar stages of their illness. This approach prevented the inclusion of cases for which varying amounts of resource utilization prior to hospitalization might introduce unknown confounding.
Variable Definition
Variables of interest were demographics, alcohol-related diagnoses (ARDs), pneumonia severity, and comorbidity. Demographic variables of interest were age, gender, race, and health insurance. Alcohol-related diagnoses were defined using any listed ICD-9-CM diagnosis codes as previously validated by Adams et al.15,16 These ARDs included the following ICD-9-CM codes and diagnoses: 305.0, alcohol abuse; 303–303.9, alcohol dependence including acute alcohol intoxication, other alcohol dependence, and unspecified alcohol dependence; 291–291.9, alcoholic psychoses including alcohol withdrawal delirium, alcohol amnestic syndrome, other alcoholic dementia, alcohol withdrawal hallucinosis, idiosyncratic alcohol intoxication, alcoholic jealousy, other specified alcoholic psychosis, and unspecified alcoholic psychosis; 571.0–571.3, alcoholic fatty liver, alcoholic hepatitis, acute, alcoholic cirrhosis of the liver, and alcoholic liver damage unspecified; 425.5, alcoholic cardiomyopathy; 535.3, alcoholic gastritis; 357.5, alcoholic polyneuropathy; and 265.2, alcoholic pellagra.
To define pneumonia severity, we identified and grouped pneumonia etiologies by ICD-9-CM diagnosis codes, an approach taken by Fine et al.14 and Saitz et al.9 This allowed identification of the pneumonia etiologies associated with higher resource utilization. Comorbidity variables were identified using any listed ICD-9-CM diagnosis codes according to the coding scheme defined by Deyo et al.17 We entered individual diagnosis codes to adjust for comorbidity in the analyses.
Outcomes
The outcomes of interest were hospital charges and length of hospital stay. Hospital charges were in dollars and represented all charges for the hospitalization including, for example, pharmacy, room, laboratory, and other charges. Length of stay was the time from admission to discharge, in days.
Analysis
All analyses were performed using the SAS System (Release 6.09, SAS Institute, Cary, NC). Analyses focused on multivariate models yielding risk-adjusted charges and length of stay in cases with and without an ARD, and tested different strategies for accounting for leaving AMA. To construct the risk-adjustment models, first bivariate analyses using Wilcoxon testing, analysis of variance (ANOVA), and Pearson or Spearman correlation testing, as appropriate, were performed for demographics, comorbidity, and pneumonia etiology and for the two outcomes, hospital charges and length of stay. Then, multivariate linear regression analyses included all variables associated with either outcome at the p < .20 level in bivariate analyses. These variables were age, gender, insurance, race, and comorbidity and pneumonia etiology (as described previously). All independent variables were dichotomous except age which was a continuous variable.
The models were used to compare any differences in outcome for patients with and patients without an ARD, adjusted for pneumonia severity, comorbidity, and demographics. Three models were constructed for each of the two outcomes, hospital charges and length of stay. In the baseline model, an indicator variable for discharge AMA (dichotomous) was not included. In the second model, we accounted for leaving AMA and the interaction between ARD and leaving AMA. In the third model, the sample was restricted by excluding cases discharged AMA from the analysis. The changes in resource utilization attributable to ARDs by the second and third approaches were compared with the baseline model.
In order to compare the difference in charge and length-of-stay estimates attributable to ARDs in each of the three analyses, we performed a bootstrapping procedure with 80 replications to generate 80 estimates of differences in charges and length of stay attributable to ARDs from each of the three models (i.e., 3 times 80 estimates).18 These estimates of charges and lengths of stay were then compared among analytic strategies using analysis of variance, and Scheffe's multiple comparison procedure with the experimentwise type I error rate set at p = .05 to take into account the multiple (three) comparisons performed. We compared estimates generated from the second and third models with those from the baseline model (two comparisons) using ANOVA, and required a p value of .025 (using Bonferroni's correction for multiple comparisons) for statistical significance.
RESULTS
Of 23,198 cases with pneumonia, the mean age was 68.2 years (SD ± 18.9), 824 (3.6%) had an ARD, and 281 (1.2%) were discharged AMA. Other patient characteristics appear in Table 1.
Table 1.
Characteristics of Hospitalized Cases with Pneumonia (N = 23,198)
| Characteristic | % |
|---|---|
| White | 91.8 |
| Female | 49.7 |
| Health insurance | |
| Any | 96.0 |
| Medicare | 67.2 |
| HMO coverage | 8.5 |
| Medicaid | 7.0 |
| Blue Cross | 6.6 |
| None | 4.0 |
| Alcohol-related diagnosis* | 3.6 |
| Discharge against medical advice | 1.2 |
See “Methods” section for definition.
In bivariate analyses, having an ARD was associated with AMA discharge: 8.5% of cases with an ARD left AMA, while only 0.9% of cases without an ARD left AMA (p < .0001; odds ratio [OR] 9.8; 95% confidence interval [CI] 7.4–12.9). Compared with standard discharges, leaving AMA was associated with lower hospital charges (mean, $5,767 vs $9,976, p = .0001) and shorter length of hospital stay (mean, 5.8 vs 9.6 days, p = .0001). The presence of an ARD was associated with higher hospitalization charges (mean, $11,232 vs $9,877, p = .07) and shorter length of stay (mean, 9.2 vs 9.6, p = .02) compared with cases with no ARD. For the AMA discharges, hospital charges and length of stay did not differ significantly according to the presence (mean charges and stay, $5,992 and 6.4 days) or absence (mean charges and stay, $5,087 and 4.0 days) of an ARD. For standard discharges, hospital charges were higher in cases with an ARD ($11,803 vs $9,913, p = .0003), but length of stay was the same (9.6 days) in cases with and cases without an ARD.
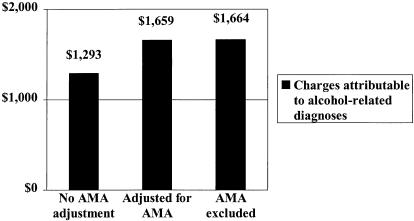
Resource Utilization Attributable to Alcoholism
Multivariate modeling adjusting for demographics, comorbidity, and disease severity yielded significantly higher risk-adjusted hospitalization charges and length of stay for cases with ARDs, regardless of modeling strategy. In the baseline model with no adjustment for AMA discharge (strategy 1), risk-adjusted mean hospital charges were higher for pneumonia cases with ARDs. An ARD accounted for a $1,293 increase in risk-adjusted charges over the $9,886 for a hospitalization without an ARD (p = .012) (Fig. 1), and yielded a total hospitalization charge of $11,179 for a case with an ARD.
FIGURE 1.
Increases in risk-adjusted mean hospital charges for pneumonia hospitalization attributable to the presence of an alcohol-related diagnosis. Three alternative modeling strategies are displayed: no adjustment for leaving against medical advice (AMA), adjustment for leaving AMA, and excluding cases discharged AMA. The differences yielded by the latter two models are larger than the baseline model (no AMA adjustment) (ANOVA p = .0001, Scheffe's test p < .05).
Strategy 2 included adjustment for AMA, and strategy 3 excluded AMA cases from the analysis. In strategy 2 the ARD-attributable increase was $1,659 over $9,873 (p = .002), yielding a total charge of $11,532; and in strategy 3 the increase was $1,664 (p = .002) over the $9,929 for a hospitalization without an ARD, yielding a total charge of $11,593. These charges represent significant increases of 28% and 29%, respectively, compared with strategy 1 (ANOVA p = .0001 for overall comparison of the mean charges for each of the three strategies, p = .0001 for each of the two comparisons between strategies 2 and 3 and strategy 1, and Scheffe's p < .05 for comparison of strategies 2 and 3 with strategy 1).
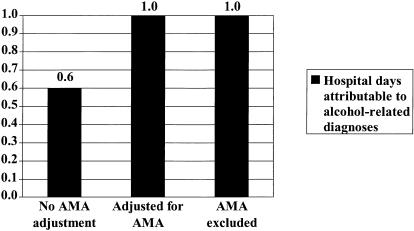
Similarly, using strategy 1, an ARD accounted for a 0.6-day increase in risk-adjusted length of stay over the 9.5 days without an ARD (p = .188) (Fig. 2), yielding a total length of stay of 10.1 days for a case with an ARD. Using strategy 2 there was an increase of 1.0 day over 9.5 days (p = .044) (total, 10.5 days), and using strategy 3, 1.0 day over 9.6 days (p = .027) (total, 10.6 days). These lengths of stay represent significant 67% increases attributable to ARDs compared with strategy 1 (ANOVA p = .0001 for overall comparison of the mean length of stay for each of the three strategies, p = .0001 for each of the two comparisons between strategies 2 and 3 and strategy 1, and Scheffe's p < .05 for comparison of strategies 2 and 3 with strategy 1).
FIGURE 2.
Increases in risk-adjusted mean length of hospital stay for pneumonia attributable to the presence of an alcohol-related diagnosis. Three alternative modeling strategies are displayed: no adjustment for leaving against medical advice (AMA), adjustment for leaving AMA, and excluding cases discharged AMA. The differences yielded by the latter two models are larger than the baseline model (no AMA adjustment) (ANOVA p = .0001, Scheffe's test p < .05).
DISCUSSION
The interpretation of resource utilization attributable to alcoholism varied with the analytic strategy chosen to address hospital discharges AMA. Accounting for discharge AMA in analyses affected the amount of utilization attributed to alcoholism. Alcoholism was associated with discharge AMA and discharge AMA was associated with resource utilization. When discharge AMA was not addressed analytically, the increases in hospitalization charges and length of stay attributable to alcoholism were substantially underestimated.
These findings should be of interest to persons concerned with measuring and understanding health care utilization. For someone interested in per-hospitalization charges only, the base analysis (strategy 1, in which no attention is given to discharges AMA) may be sufficient. This base analysis (and the simpler bivariate analysis of unadjusted charges) yielded the lowest charges and lengths of stay attributable to alcoholism when compared with the alternative analyses. This base analysis yielded the actual total mean charges for a hospital stay with or without an ARD. Hospitalizations ending in discharge AMA were shorter and cost less and hospitalizations of cases with an ARD were more likely to end AMA.
The analyses that account for discharge AMA would be of interest to those wanting to determine resource utilization attributable to specific conditions such as alcoholism and to health providers, health plan administrators, and organizations wanting to determine an individual's utilization beyond a single hospitalization. These analyses would also be of interest to any researcher or health care organization designing an intervention that would reduce discharges AMA. Which of the two analytic strategies is “correct,” however, is not clear, but the results were almost identical. Treating AMA discharge as a confounder may not be a rigorous solution because leaving AMA does not independently affect resource utilization.19 Although AMA discharge is associated with both alcoholism and charges, it is an intermediate step in a causal pathway: the path in which alcoholism results in altered resource utilization. The restriction strategy is also imperfect in that the excluded cases are likely to be quite different (more charges attributable to alcoholism) from those left in the restricted sample.
Discharge AMA is a relatively infrequent occurrence. For a given hospitalization ending in discharge AMA, the resource utilization (costs and length of stay) will be lower. But the estimates of resource utilization attributable to a patient characteristic may be underestimated when the patient is discharged AMA. Also, overall costs of caring for an individual patient over time may be higher for patients who leave the hospital prematurely. The utilization may be shifted from the hospital to other providers and is likely to show up later.1,5,20 In fact, leaving AMA is likely to result in greater subsequent utilization, including more return visits, and perhaps greater costs for the subsequent care of an initially inadequately treated condition. Weingart et al. reported that patients discharged AMA were significantly more likely to be readmitted than patients discharged with approval, and that 54% of patients discharged AMA were hospitalized again.21
Both analyses that in some way accounted for discharges AMA, either by the exclusion of cases discharged AMA or by adjustment for leaving AMA, forecast the resource utilization that would have been seen had the hospitalization not ended prematurely. It is predictable that these hospitalization costs would appear in health systems that were successful at efforts to reduce AMA discharges. For cases that do end in AMA discharge, the costs are likely to appear later for outpatient care. There are three possibilities for the predicted additional amounts attributable to alcoholism accounted for by AMA discharge: one is that the additional charges never appear, another is that some of them do, and the other is that all of the additional charges appear in the future. Because our data are limited to hospitalization, we cannot test hypotheses regarding future care costs. But on the basis of the literature cited above and our risk-adjusted analyses, we feel that the base analysis underestimates the resource utilization attributable to alcoholism. True estimates of resource utilization attributable to alcoholism are higher, and the alternative analyses provide a closer reflection of the utilization attributable to alcoholism.
In a separate multivariate analysis, we also found that younger age, male gender, lack of health insurance, and substance abuse all independently increased the likelihood of AMA discharge.22 We suspect that analyses of resource utilization attributable to patients with these risk factors may be subject to the same difficulty with interpretation as alcoholism when discharge AMA is not accounted for in analyses by either adjustment or restriction. Of note, those discharged AMA did not have less comorbidity, nor did they have significant differences in pneumonia severity as measured by the presence of high-risk etiologies.14,22
The analyses reported are primarily limited by the lack of longitudinal cost data. We speculate that the costs saved during a hospitalization that ends in discharge AMA will appear elsewhere in the system. Also, we used charge data rather than cost data for these analyses. Each hospital has its own cost-to-charge ratio and charges cannot be assumed to reflect actual costs. However, in these analyses, the charges were of interest as they related to ARDs and discharges AMA, not to how they varied from hospital to hospital. Finally, the use of only administrative data may have limited the present study, though it is particularly in analyses of these data sets that our concerns are relevant. This study had sufficient clinical detail so that the analyses could be adjusted for comorbidity and disease severity.
Studies of hospital utilization generally do not account for whether patients left AMA or not. This may be inconsequential, but when one is interested in resource utilization by persons with alcohol problems or in other groups in which AMA discharge is more likely, the impact of discharge AMA on interpretations of utilization analyses may become significant. Our results from a large statewide database, risk-adjusted for demographics, pneumonia etiology, and comorbidity, show that discharge AMA affects the relation between alcoholism and hospital resource utilization. Not accounting for whether or not a hospitalization ends AMA can result in a significant underestimation of resource utilization attributable to alcoholism.
Acknowledgments
Dr. Saitz is a Generalist Physician Faculty Scholar of the Robert Wood Johnson Foundation and was also supported in this work by the Center for Substance Abuse Prevention Faculty Development Program, grant number 1 T15 SP07773-01, Substance Abuse Mental Health Services Administration, Department of Health and Human Services. This work was supported by the Massachusetts Health Data Consortium, which provided the data used in the analyses. Dr. Ghali is supported by a Population Health Investigator Award from the Alberta Heritage Foundation for Medical Research and is now at the Department of Medicine and Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
REFERENCES
- 1.Udvarhelyi IS, Goldman L, Komaroff AL, Lee TH. Determinants of resource utilization for patients admitted for evaluation of acute chest pain. J Gen Intern Med. 1992;7(1):1–10. doi: 10.1007/BF02599092. [DOI] [PubMed] [Google Scholar]
- 2.Smith DB, Telles JL. Discharges against medical advice at regional acute care hospitals. Am J Public Health. 1991;81(2):212–5. doi: 10.2105/ajph.81.2.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Targonski PV, Persky VW, Kelleher P, Addington W. Characteristics of hospitalization for asthma among persons less than 35 years of age in Chicago. J Asthma. 1995;32(5):365–72. doi: 10.3109/02770909509082761. [DOI] [PubMed] [Google Scholar]
- 4.Jeffer EK. Against medical advice, part I: a review of the literature. Mili Med. 1993;158(2):69–73. [PubMed] [Google Scholar]
- 5.Pennycook AG, McNaughton G, Hogg F. Irregular discharge against medical advice from the accident and emergency department—a cause for concern. Arch Emerg Med. 1992;9(2):230–8. doi: 10.1136/emj.9.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ochitill HN, Havassy B, Byrd RC, Peters R. Leaving a cardiology service against medical advice. J Chronic Dis. 1985;38(1):79–84. doi: 10.1016/0021-9681(85)90010-4. [DOI] [PubMed] [Google Scholar]
- 7.Baile WF, Brinker JA, Wachpress JD, Engel BT. Signouts against medical advice. J Behav Med. 1979;2(1):85–92. doi: 10.1007/BF00846565. [DOI] [PubMed] [Google Scholar]
- 8.Jankowski CB, Drum DE. Diagnostic correlates of discharge against medical advice. Arch Gen Psychiatry. 1977;34(2):153–5. doi: 10.1001/archpsyc.1977.01770140043004. [DOI] [PubMed] [Google Scholar]
- 9.Saitz R, Ghali WA, Moskowitz MA. The impact of alcohol-related diagnoses on pneumonia outcomes. Arch Intern Med. 1997;157:1446–52. [PubMed] [Google Scholar]
- 10.Pankrantz L, Jackson J. Habitually wandering patients. N Engl J Med. 1994;331:1752–5. doi: 10.1056/NEJM199412293312606. [DOI] [PubMed] [Google Scholar]
- 11.Forsythe AB, Griffiths B, Reiff S. Comparison of medical services by alcoholics and non-alcoholics. Am J Public Health. 1982;72:600–2. doi: 10.2105/ajph.72.6.600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Densen PM, Fielding JE, Getson J, Stone EM. The collection of data on hospital patients: the Massachusetts Health Data Consortium approach. N Engl J Med. 1980;302:171–3. doi: 10.1056/NEJM198001173020311. [DOI] [PubMed] [Google Scholar]
- 13.Practice Management Information Corp. ICD–9-CM: International Classification of Diseases, 9th revision, Clinical Modification. 4th ed. Los Angeles, Calif: Practice Management Information Corp; 1995. [Google Scholar]
- 14.Fine MJ, Singer DE, Hanusa BH, Lave JR, Kapoor WN. Validation of a prognostic index using the MedisGroups comparative hospital database. Am J Med. 1993;94:153–9. doi: 10.1016/0002-9343(93)90177-q. [DOI] [PubMed] [Google Scholar]
- 15.Adams WL, Yuan Z, Barboriak JJ, Rimm AA. Alcohol-related hospitalizations of elderly people: prevalence and geographic variation in the United States. JAMA. 1993;270:1222–5. [PubMed] [Google Scholar]
- 16.Dufour MC, Fe Caces M. Epidemiology of the medical consequences of alcohol. Alcohol Health Res World. 1993;17:265–71. [Google Scholar]
- 17.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 18.Iezzoni LI. Risk Adjustment for Measuring Health Outcomes. Ann Arbor, Mich: Health Administration Press; 1994. [Google Scholar]
- 19.Rothman KJ, Greenland S. Modern Epidemiology. 2nd ed. Hagerstown, Md: Lippincott–Williams & Wilkins; 1998. [Google Scholar]
- 20.Dalrymple AJ, Fata M. Cross-validating factors associated with discharges against medical advice. Can J Psychiatry. 1993;38(4):285–9. doi: 10.1177/070674379303800411. [DOI] [PubMed] [Google Scholar]
- 21.Weingart SN, Davis RB, Phillips RS. Patients discharged against medical advice from a general medicine service. J Gen Intern Med. 1998;13:568–71. doi: 10.1046/j.1525-1497.1998.00169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saitz R, Ghali WA, Moskowitz MA. Characteristics of patients with pneumonia who are discharged from hospitals against medical advice. Am J Med. 1999;107:507–9. doi: 10.1016/s0002-9343(99)00262-4. [DOI] [PubMed] [Google Scholar]