Abstract
OBJECTIVE
To evaluate the effect of primary care coordination on utilization rates and satisfaction with care among public hospital patients.
DESIGN
Prospective randomized gatekeeper intervention, with 1-year follow-up.
SETTING
The Adult General Medical Clinic at San Francisco General Hospital, a university-affiliated public hospital.
PATIENTS
We studied 2,293 established patients of 28 primary care physicians.
INTERVENTION
Patients were randomized based on their primary care physician's main clinic day. The 1,121 patients in the intervention group (Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare [APPROACH] group) required primary care physician approval to receive specialty and emergency department (ED) services; 1,172 patients in the control group did not.
MEASUREMENTS AND MAIN RESULTS
Changes in outpatient, ED, and inpatient utilization were measured for APPROACH and control groups over the 1-year observation period, and the differences in the changes between groups were calculated to estimate the effect of the intervention. Acceptability of the gatekeeping model was determined via patient satisfaction surveys.
RESULTS
Over the 1-year observation period, APPROACH patients decreased their specialty use by 0.57 visits per year more than control patients did ( P =.04; 95% confidence interval [CI]−1.05 to −0.01). While APPROACH patients increased their primary care use by 0.27 visits per year more than control patients, this difference was not statistically significant (P =.14; 95% CI, −0.11 to 0.66). Changes in low-acuity ED care were similar between the two groups (0.06 visits per year more in APPROACH group than control group, P =.42; 95% CI, −0.09 to 0.22). APPROACH patients decreased yearly hospitalizations by 0.14 visits per year more than control patients (P =.02; 95% CI, −0.26 to −0.03). Changes in patient satisfaction with care, perceived access to specialists, and use of out-of-network services between the 2 groups were similar.
CONCLUSIONS
A primary care model of health delivery in a public hospital that utilized a gatekeeping strategy decreased outpatient specialty and hospitalization rates and was acceptable to patients.
Keywords: primary care, coordination, public hospital patients, gate keeping, utilization
Most prepaid health plans organize health care via primary care physicians who directly deliver services to enrollees and coordinate a vast array of health services including specialty, emergency, hospital, home-health, and other expensive care. In spite of recent trends to the contrary,1,2 most managed care plans and contracting physician groups continue to rely on such a designated gatekeeper.3–5 The use of gatekeepers is increasingly common among the growing number of Medicaid managed care health plans6–8 and county-organized health services for the uninsured.9 Despite this increasing use, however, little is known about the extent to which gatekeeping can actually achieve its main goals — to increase coordination and continuity, improve access and quality, and control costs.10 Even less is known about what effect gatekeeping has on public sector patients. The few studies of Medicaid managed care demonstration projects report conflicting results with regard to changes in patterns of use and continuity of care.8,11,12 In addition, most studies of gatekeeping have been limited by the fact that the gatekeeping function is nearly always confounded by financial arrangements such as capitation or incentives that may themselves affect outcomes.8,11,13–18
In an attempt to assess some of the implications that managed care strategies may have for patients cared for at a public hospital, we collaborated with the San Francisco Department of Public Health in evaluating a managed care project called the Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare (APPROACH). The main goal of the APPROACH Project was to assess the effect of a managed care intervention — in this case, the primary care coordination or gatekeeping model facilitated by a customized computer authorization system — on utilization rates and satisfaction with care among a cohort of publicly insured and uninsured adult patients cared for at a public hospital.
METHODS
Setting and Study Participants
The APPROACH Project took place between April 1, 1997, and March 31, 1998, in the General Medical Clinic (GMC) at San Francisco General Hospital (SFGH), the acute care public hospital serving the city and county of San Francisco. Approximately half of San Francisco's 130,000 uninsured residents and one quarter of its Medicaid population make at least 1 visit to SFGH each year. The GMC is a hospital-based, adult, primary care clinic that serves a patient population that is medically complex, ethnically diverse, and of low socioeconomic status. The approximately 5,000 patients followed in GMC are cared for in a continuity fashion by attending general internist faculty who are assigned to SFGH but employed by the University of California, San Francisco (UCSF), or by SFGH-based UCSF medical residents with attending oversight.
In order to be eligible for the study, patients were required to have been followed in GMC, as determined by having made at least 1 visit to their primary care physician in GMC within 12 months and at least 1 visit to any SFGH clinic (specialty or primary care) within 6 months prior to the April 1, 1997, start date. These criteria increased our confidence that patients were actively using the SFGH system. We randomly assigned patients by virtue of the main clinic day of their primary care physician. Patients cared for by physicians whose main clinic day was on Thursday were assigned to the intervention arm (APPROACH group), while patients cared for by physicians whose main clinic day was on either Tuesday or Wednesday served as controls. The two groups of physicians and their patients were mutually exclusive.
Intervention
The intervention entailed primary care approval for all specialty and nonurgent emergency department care. All APPROACH patients received a brochure, written at the fifth-grade level, also available in Spanish and Cantonese translations, that introduced them to the APPROACH Project. The brochure included the name of their regular physician, oriented them to the necessity of coordinating all of their care through this physician, and provided them with important clinic telephone numbers. APPROACH patients were permitted to disenroll at any time. Control patients did not receive any new information.
Starting April 1, 1997, all APPROACH patients required prior approval from their primary care physician in order to receive specialty care at SFGH, a policy achieved by way of a computer screen that blocked the scheduling of unapproved specialty visits. In order to generate a specialty referral, APPROACH primary care physicians were instructed to complete a standard consultation form that included clinical information as well as the number of visits requested. No guidelines were given regarding the number of specialty visits recommended, and there was no external utilization management process. All APPROACH consultations originating from a resident's patient required the signature of the resident's supervising attending physician. Receipt of this form allowed GMC staff to “unlock” the scheduling system for the number of visits requested, and schedule the initial appointment for the patient.
Specialty physicians or other hospital staff attempting to electronically schedule an unauthorized visit for an APPROACH patient were informed on the computer screen that the patient required the approval of his/her primary care physician prior to receiving the service. The screen also listed the name, voicemail number, and beeper number of the patient's primary care physician, the APPROACH back-up nurse, and the GMC physician on call, all of whom could unlock the system if the appointment was deemed appropriate. All patients in the control group were able to receive specialty services as usual, without limitations, through self-referral or referral from primary care physicians, specialists, ED staff, nursing staff, discharging physicians, and others.
Less-urgent visits to the ED (low-acuity triage codes 3, 4, and 5 on a 5-point scale, as determined by ED triage nurse; protocols available on request) made by APPROACH patients also were supposed to require prior authorization from the primary care physician or GMC physician on call. Although the ED computer screen informed registration staff about the need to obtain authorization, it did not block the electronic recording of visit, a priori. Patients in the control group did not require prior authorization to receive emergency care. Finally, no prior authorization was needed to obtain hospitalization, diagnostic testing, primary care, mental health care, or family planning care for patients in either group.
APPROACH physicians and those working in specialty clinics and the ED were oriented to the goals and processes of the project by way of a packet that explained the prior authorization process described above. APPROACH physicians were asked to deliver optimal health care, facilitate provision of all appropriate care, authorize all needed medical services, avoid unnecessary or duplicative services, enhance communication with specialists and ED physicians, and assume responsibility for coordinating the care of their patients. APPROACH physicians were informed that neither they nor their patients would be subject to incentives or penalties for either “desired” or “undesired” patterns of use. To minimize bias, primary care physicians did not receive feedback about their patients' utilization or learn the results of the study until the end of the 1-year project.
Data Sources
Patients' demographic information, derived from the hospital's information system, included age, gender, primary language, race/ethnicity, insurance status, APPROACH status (enrolled, not enrolled, or disenrolled), as well as a running tally of International Classification of Diseases, Ninth Revision (ICD-9), codes generated from billing records.
Utilization data were obtained via the hospital's encounter-based billing system that records all SFGH outpatient and inpatient visits, with the exception of outpatient psychiatric services. We excluded all psychiatric hospitalizations and hospitalizations for labor and delivery.
We obtained data regarding patients' experiences with the gatekeeping model by directly surveying a group of patients at baseline (96 APPROACH patients and 105 control patients) by means of a confidential questionnaire administered by a research assistant, by telephone or in person. We attempted to readminister the survey to patients after the 1-year observation period. Respondents were given $5 for their participation in each survey. The survey instrument, translated from English into Spanish and back-translated into English, consisted of 30 items that explored numerous domains of care, including self-rated health, satisfaction with care, access to primary and specialty care, and loci of care, including receipt of medical care outside SFGH.
Measurements
The main outcomes of the study were changes from the previous year to the study year in rates of utilization of SFGH inpatient and outpatient services. Secondary outcomes, including coordination of care, access to specialty care, and acceptability of the gatekeeping model to patients, were measured only during the study year.
Visits were categorized into primary care, specialty, low-acuity ED, or inpatient use. A patient's yearly rates of utilization were measured on a monthly basis for each service category by counting visits during each of the 12 months of study. If before the end of the study patients changed their primary care physician or clinic (34 APPROACH patients and 34 control patients), disenrolled from the APPROACH Project (38 patients), or died (4 APPROACH patients and 11 control patients), we extrapolated a 12-month rate from use during the period of time before dropout. We similarly calculated a patient's baseline use by counting visits during the 12 months prior to the beginning of the study. The baseline rates of each patient were then subtracted from the rates during the study, and the results were used to compare average change in utilization between APPROACH and control groups.
Extent of primary care coordination was assessed during the study year by measuring the percentage of patients who returned to GMC within a month of an ED visit. We assumed that differences in the frequency of this pattern of care between APPROACH and control patients reflected differences in coordination and timely follow-up between the ED and the primary care physician. In addition, among users of specialty care, we compared the percentage of APPROACH and control patients who experienced at least 1 occurrence of consecutive visits to different specialties before returning to GMC. Though this pattern might, in part, reflect multiple referrals simultaneously generated by a primary care physician, we reasoned that differences in the frequency of this pattern between APPROACH and control patients might be attributable to specialty-to-specialty referrals. For example, a primary care physician might refer a patient to a cardiologist for chest pain; the cardiologist, feeling that the pain is due to reflux esophagitis, might then bypass the primary care physician and refer the patient directly to a gastroenterologist. In contrast, sequential visits to 1 specialist (several orthopedic visits in a row) would not represent a pattern of consecutive visits to different specialties.
To assess whether the intervention was associated with an inappropriate reduction in access to specialty care, we chose to evaluate access to a type of specialty care for which there is national consensus. It is generally accepted that every diabetic patient should receive a retinal examination annually. We compared the percentage of diabetics (all patients with an ICD-9 code of 250.XX) in each group who made at least 1 visit to a SFGH ophthalmologist over the course of the study year. We also analyzed the extent to which patients' perceived access to all specialty care, gathered from the patient survey, changed from baseline to the end of the 1-year observation period in both groups.
Acceptability of the gatekeeping model was assessed in 3 ways. First, we measured the number of active disenrollments from the APPROACH Project. Second, we measured the degree to which patients were nonusers of our system, by comparing the percentage of patients in each group without any visits to SFGH each month. Third, we measured the degree to which patients' reports of out-of-network use changed in each group from baseline to the end of the 1-year observation period.
Statistical Analysis
For the main outcome measures, the change from the previous year to the study year was calculated for each patient and then analyzed by mixed effects models that included a random physician effect,19 in order to account for possible lack of independence or clustering between patients of the same physician. Because residuals from these models did not follow normal distributions, a bootstrapping strategy was used to obtain valid confidence intervals and P values.20 This involved randomly resampling residuals with replacement and adding them to each patient's fitted change, then reestimating the original model on these simulated data. This was done 2,000 times, with confidence intervals then obtained by the bias-corrected accelerated method and P values defined as 1 minus the highest confidence level that excluded 0. To control these comparisons for differences in the 2 groups that could affect utilization, we also fit models controlling for the covariates age, race, gender, insurance status, and type of provider (resident vs attending physician).
As a rough estimate of the magnitude of the effect of the intervention, we also calculated a percentage change in utilization within each service category for the APPROACH group relative to the control group, by dividing the difference in change between APPROACH and control groups (accounting for clustering) by the baseline use in the APPROACH group.
All secondary, dichotomous outcomes, including coordination of care, access to ophthalmologic care, and acceptability of the gatekeeping model, were analyzed by logistic models with generalized estimating equations to account for possible lack of independence between patients of the same physician.
The evaluation of the APPROACH Project was approved by the UCSF Committee on Human Research.
RESULTS
A total of 1,121 patients cared for by 12 physicians (4 attending physicians and 8 residents) were assigned to the APPROACH group, and 1,172 patients cared for by 16 physicians (6 attending physicians and 10 residents) were assigned to the control group. Together, these patients comprised approximately one half of the active GMC patient panel.
The baseline characteristics for patients in both groups are shown in Table 1). There were no statistically significant differences between the 2 groups with regard to gender, race/ethnicity, language capabilities, prior outpatient and inpatient utilization, proportion with attending-level primary care physicians, distance from the hospital (ZIP codes), or the prevalence of chronic medical conditions. In the control group, the mean age was higher, the percentage of Medicare patients was higher, and the percentage of Medicaid patients was lower.
Table 1.
Baseline Characteristics of Patients*
| Characteristic | APPROACH (n=1,121) | Control (n=1,172) | P Value† |
|---|---|---|---|
| Mean age, y | 53.3 | 54.6 | .02 |
| Male, % | 52.9 | 52.1 | .68 |
| Race/ethnicity, % | |||
| African American | 25.6 | 27.4 | |
| Asian/Pacific Islander | 20.8 | 21.9 | |
| White | 28.5 | 26.0 | |
| Hispanic | 23.6 | 22.0 | |
| Other | 1.5 | 2.7 | |
| Language, % English | 75.1 | 76.8 | .35 |
| Insurance status, % | <.01 | ||
| Medi-Cal (Medicaid) | 29.9 | 29.7 | |
| Medicare | 23.1 | 29.8 | |
| Uninsured | 40.1 | 34.1 | |
| Other | 3.1 | 2.6 | |
| Prior year SFGH utilization (mean visits/y) | |||
| Primary care (GMC) | 4.8 | 4.8 | .81 |
| Specialty care | 4.3 | 4.6 | .21 |
| Total emergency care | 1.3 | 1.2 | .70 |
| Low-acuity emergency care | 0.7 | 0.6 | .70 |
| Hospital (inpatient) care | 0.48 | 0.44 | .41 |
| Patients with 1 or more hospitalizations, % | 16.6 | 14.5 | .17 |
| Attending-level primary care physician, % | 49.9 | 49.5 | .86 |
| Medical conditions, % | |||
| Hypertension | 64.9 | 64.8 | .93 |
| Diabetes mellitus | 29.4 | 31.7 | .23 |
| Congestive heart failure | 12.9 | 12.1 | .60 |
| Asthma | 11.2 | 13.7 | .07 |
| Chronic obstructive lung disease | 12.7 | 12.0 | .64 |
| HIV disease | 3.9 | 4.3 | .68 |
APPROACH indicates Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare; SFGH, San Francisco General Hospital; GMC, General Medical Clinic.
Unclustered t tests.
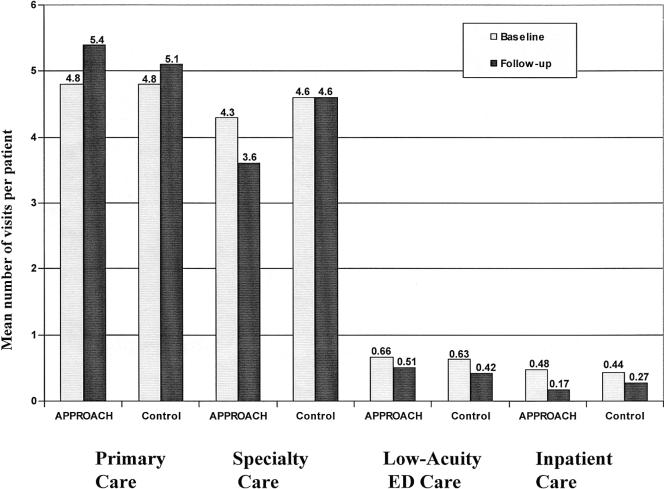
The crude means for utilization within each category of care in the baseline year and the 1-year observation period for APPROACH and control groups are shown in Figure 1. Table 2 shows the estimated APPROACH effects across all service categories, after accounting for clustering between patients of the same physician, and after adjustment. During the study year, APPROACH patients had 0.57 fewer specialty visits than control patients (P = .04; 95% confidence interval [CI]−1.05 to −0.01), representing approximately 13% fewer visits. APPROACH patients had 0.27 more primary care visits per year than control patients, although this difference was not statistically significant (P = .14; 95% CI, −0.11 to 0.66). Changes in low-acuity ED care were similar in the 2 groups (0.06 visits per year more in the APPROACH group than the control group; P = .42; 95% CI, −0.09 to 0.22). Results remained similar after adjusting for age, sex, race, financial class, language, type of provider, and prior outpatient utilization.
FIGURE 1.
Annual utilization of San Francisco General Hospital services by service category, at baseline and after 1-year observation period, for intervention (APPROACH) and control groups. APPROACH indicates Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare; ED, emergency department.
Table 2.
Changes in Hospital Utilization over the One-Year Observation Period, for APPROACH and Control Groups,* and Differences in These Changes Between Groups†
| Utilization | Change in APPROACH | Change in Control | Difference in Change Unadjusted (P Value; 95% CI) | Difference in Change Adjusted‡(P Value; 95% CI) |
|---|---|---|---|---|
| Primary care | 0.60 | 0.33 | 0.27 (.14; −0.11 to 0.66) | 0.28 (.16; −0.11 to 0.66) |
| Specialty care | −0.48 | 0.09 | −0.57 (.04; −1.05 to −0.01) | −0.53 (.05; −1.05 to 0.01) |
| Low-acuity ED care | −0.15 | −0.21 | 0.06 (.42; −0.09 to +0.22) | 0.06 (.42; −0.09 to +0.22) |
| Inpatient care | −0.31 | −0.17 | −0.14 (.02; −0.26 to −0.03) | −0.14 (.01; −0.26 to −0.03) |
Calculated for each service category as: Change =(Baseline Use)−(Observation Period Use). Results may not exactly coincide with the crude means from Figure 1, as this calculation accounts for the clustering effect. APPROACH indicates Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare; CI, confidence interval.
These results, calculated as (Change in APPROACH)−(Change in Control), represent the main effect of the intervention.
Adjusted for age, sex, race, financial class, language, and level of provider.
Over the course of the year, there were a total of 286 hospitalizations, with 120 in the APPROACH group and 166 in the control group. Patients in the APPROACH group had 0.14 fewer hospitalizations per year than controls (P = .02; 95% CI, −0.26 to −0.03), representing 29% fewer hospitalizations than in the control group. The distributions of admitting diagnoses were similar in APPROACH and control patients, as were the proportions of elective admissions (data not shown). After adjustment for age, race, sex, insurance status, type of provider, and prior hospital utilization, the difference in change in inpatient utilization between the APPROACH and control groups persisted.
We observed similar patterns in the difference in change in utilization between APPROACH and control patients across the 3 major insurance categories (Medicare, Medicaid, and uninsured). Because of the smaller sample sizes, none of these differences reached statistical significance.
To explore the possibility that the reduction in specialty care observed in the APPROACH group was simply a function of delay in accessing care, we examined whether the specialty use differences between APPROACH and control groups varied by month and found that the differences were present each month, suggesting a sustained effect (data not shown).
With regard to coordination of outpatient care, among users of the ED (n = 734), a greater percentage of APPROACH patients returned to GMC within a month of an ED visit, when compared with control patients (61% vs. 52%, P < .01), a difference that persisted after adjustment for age, sex, race, financial class, language, and type of provider (P < .01). Among patients with visits to at least 2 different specialties (n = 1,007), a smaller percentage of APPROACH patients made consecutive visits to different specialties before returning to the primary care physician, when compared with control patients (53% vs 59%, P < .01), a difference that persisted after adjustment for age, sex, race, financial class, language, and type of provider (P < .01).
To assess whether the intervention was associated with a reduction in one aspect of appropriate specialty care, we compared the percentage of diabetic patients (n = 651) in each of the groups who had made at least 1 visit to the ophthalmologist. We found no difference between APPROACH and control groups in the percentage of patients who had made an ophthalmology visit at SFGH during the year of study (38% vs 38%, P = .94). After adjustment for age, gender, race, financial class, language, and type of provider, the difference was still not statistically significant (P = .72).
Thirty-eight APPROACH patients (3%) explicitly disenrolled from the project. The percentages of patients who did not make any visit to SFGH on a monthly basis in the APPROACH and control groups were similar (data not shown), suggesting that APPROACH patients were not preferentially leaving the SFGH system over the course of the year.
Seventy-three APPROACH patients (76%) and 78 control patients (75%) completed surveys at baseline and at the end of the 1-year observation period. The groups appeared to be similar at baseline with regard to patients' ratings of their health, satisfaction with care, access to primary care, access to specialty care, or experience of their physician being unwilling to refer them to a specialist. At the end of the one year observation period, we found similar changes between the 2 groups across these domains (Table 3) None of the patients in either group described their physician as being unwilling to refer them to a specialist during the year of study. Among respondents, 20% of APPROACH patients and 16% of control patients reported on the baseline survey that they had physician visits outside SFGH. The percentages of patients in both groups who reported visits to physicians outside SFGH declined by similar amounts over the year of study.
Table 3.
Baseline and Follow-up Patient Surveys and Relative Change Between APPROACH and Control Groups*
| Measure | Baseline | One Year | Relative Change†(95% CI) | P Value | ||
|---|---|---|---|---|---|---|
| APPROACH (n=73) | Control (n=78) | APPROACH (n=73) | Control (n=78) | |||
| Self-rated health‡ | 3.67 | 3.69 | 3.51 | 3.62 | 0.09 (−0.28 to 0.43) | .68 |
| Satisfaction with care§ | 4.14 | 3.97 | 4.14 | 3.95 | −0.02 (−0.41 to 0.36) | .89 |
| Access to primary care‖ | 4.21 | 4.00 | 4.39 | 4.16 | −0.02 (−0.43 to 0.38) | .90 |
| Access to specialty care¶ | 3.78 | 3.74 | 4.27 | 4.31 | 0.08 (−0.48 to 0.63) | .79 |
| Physician unwilling refer,#% | 0 | 3 | 0 | 0 | −1.0** | 1.0 |
| Visits outside SFGH,††% | 20 | 16 | 16 | 12 | 0.3 (−12 to 13) | 1.0 |
APPROACH indicates Ambulatory Patient–Physician Relationship Organized to Achieve Coordinated Healthcare; CI, confidence interval.
The change from baseline to one year in each group (A1 − A0 for APPROACH group) and (C1 − C0 for control group) was first calculated for each measure. The relative change between the two groups was then determined by subtracting the change in the control group from the change in the APPROACH group (A1–A0) – (C1–C0).
Health status (“In general, would you say your health is:”) was rated on a 5-point scale, with 1 = “excellent” and 5 = “poor.”
Satisfaction with care (“Overall, how would you rate the care you have received at the General Medical Clinic over the past 6 months?”) was rated on a 5-point scale, with 1 = “poor” and 5 = “excellent.”
Access to primary care (“Overall, how difficult is it for you to get medical care at the General Medical Clinic when you need it?”) was rated on a 5-point scale, with 1 = “extremely difficult” and 5 = “not difficult at all.”
Access to specialty care (“Overall, how difficult is it for you to see a specialist outside of the General Medical Clinic, such as a foot doctor, eye doctor, or heart doctor? Would you say it is:”) was rated on a 5-point scale, with 1 = “extremely difficult” and 5 = “not difficult at all.”
Dichotomous question: “In the past 6 months, was your primary care doctor at the General Medical Clinic ever unwilling to make a referral that you requested?”
Small and zero cells prevent calculation of 95% confidence interval.
Dichotomous question: “In the past 6 months, have you had any visits with dorctors or health professionals not at San Francisco General Hospital?”
DISCUSSION
As health care financing for public sector patients has become more competitive, public hospitals have come under increasing pressure to provide efficient, high-quality, cost-effective care.6,7 Many patients cared for in institutions that serve as medical safety nets possess a complex set of medical, psychological, and social problems that may tend to make their care costly, fragmented, and difficult to manage. Strategies applied in the private sector to change patient and physician behavior (restricting benefits packages, imposing financial penalties for undesired patterns of use, requiring copayments, and providing incentives to physicians to limit care) may be problematic or undesirable in the public sector. Patients in our public hospital who were cared for in a primary care gatekeeping model had significantly lower specialty use, similar rates of primary care and nonurgent emergency department use, and fewer hospitalizations, when compared with a control group of primary care patients without such an explicit model of care. In addition, patients in the gatekeeping model displayed patterns of care that suggest enhanced coordination, and continued to receive similar access to at least one type of appropriate specialty care, when compared with the control group. Patients' health status, satisfaction, and perceived access to primary and specialty care were also similar.
The extent of the reduction in specialty care observed in our study is similar to that in the few previously published studies of gatekeeping that explored this issue.8,13 The failure of our intervention to reduce low-acuity ED care speaks to the complexities of this pattern of utilization among the urban poor,21 the fact that ED use for nonurgent complaints is primarily a patient-driven rather than a physician-driven pattern, and the fact that the computer screens used in our intervention merely informed ED staff of the primary care physician approval process, but did not enforce it by preventing access to the ED for unauthorized visits.
The lower rate of hospitalizations associated with the gatekeeping intervention is consistent with findings of some previous private sector studies. A prior randomized controlled trial of gatekeeping found a trend toward a reduction in hospital use for enrollees in the gatekeeping model,13 and a study of enrollees in an HMO that converted its payment method to primary care physicians from a fee-for-service to a capitated model found that hospital admissions declined by 16%.17 The RAND Health Insurance Experiment found that persons enrolled in a group-model HMO experienced 41% fewer hospital days and incurred 28% lower total expenses than those who received care in a fee-for-service model.14
The reduction in hospitalizations observed in our study may be due to greater primary care linkage, follow-up, and continuity experienced by APPROACH patients. Unfortunately, the number of admissions was too small to allow for an analysis of specific types of admissions such as avoidable hospitalizations. Alternatively, the reduction may simply be a function of the lower rate of outpatient specialty utilization and the fact that, as was suggested in a prior study of primary care and hospital readmissions, reducing the number of encounters and diagnostic studies experienced by a patient lowers the likelihood that the patient will be admitted.22
The few studies of Medicaid managed care demonstration projects report conflicting results with regard to changes in patterns of use and continuity of care, with the direction of change often correlated with the type of financial incentive applied to participating primary care physician gatekeepers. Fee-for-service arrangements appear to lead to increased primary care use, with no change in specialty or ED use11,12; capitation arrangements with incentives to limit referrals lead to a reduction in the use of specialty services without a corresponding increase in primary care use8; and fee-for-service arrangements augmented by a gatekeeper case management fee lead to greater reliance on primary care physicians relative to specialists, a reduction in ED use, and an increase in the proportion of enrollees receiving care from 1 physician.8 Our study is unique by virtue of its public hospital setting and its ability to separate the administrative function of gatekeeping from the financial incentives with which it is often confounded. Our findings suggest that such incentives were not necessary in shifting care to the primary care site.
In designing our evaluation of the APPROACH Project, we attempted to capture the primary care coordination function embedded in gatekeeping. Our measures of primary care coordination were based on comparisons of rates of patterns of care, such as the presence of a primary care visit after an ED visit, or the absence of a primary care visit between visits to 2 different specialties (the presence of specialty-to-specialty referrals). Patients in the APPROACH group displayed patterns of care suggesting enhanced coordination, but the limitations of such an approach are obvious and speak to the need for more sophisticated, validated measures of primary care coordination that go beyond locus of utilization.23 There are several reasons, however, to consider our measures justified in the setting of the visit-based, fragmented care typical of a public hospital. At SFGH, primary care physicians do not receive computerized clinical information regarding their patients' visits to specialty clinics. As such, a primary care visit often serves to provide communication and information to the primary care physician to assist in coordinating the care of his/her patient. Such visits may also reinforce the concept of a “medical home” and promote continuity of care, arguably an important part of providing care to vulnerable, public-sector patients.24 In addition, patients cared for at SFGH have complex medical conditions, often in the context of complicated social conditions and language barriers, which make transmittal and clarification of information (e.g., what medications to take, or where the ultrasound suite is located) an important component of primary care, usually delivered in person to facilitate comprehension and adherence.
We could not directly assess the degree to which patients in either group were receiving care through other health systems or other hospitals. We attempted to indirectly measure this phenomenon by measuring the percentage of patients who did not make any visits to SFGH on a monthly basis and asking a sample of patients about their out-of-network use, and we found similar results, suggesting that out-of-network use occurred, but did not preferentially affect one of the groups. In addition, we neither restricted nor measured use of the mental health system, arguably a significant component of health service delivery to a public sector population.
In measuring the degree to which the gatekeeping model affected access to specialty care, we found no differences in the level of eye care afforded to diabetic patients and no changes in patients' perceptions of access to specialty care. Though these findings suggest that appropriate care was preserved in the APPROACH intervention, we did not have an encompassing method for assessing appropriateness.
Our study involved patients who were already in established relationships with primary care physicians before the initiation of the gatekeeping intervention. As such, the results may not be generalizable to all public hospital patients.
Our study does not answer all of the questions raised by primary care gatekeeping, especially those having to do with quality of care and clinical outcomes. It does suggest, however, that when the medical management function of gatekeeping is separated from the financial incentives with which it is often confounded, utilization can still be influenced, coordination enhanced, and patient satisfaction maintained. These conclusions challenge the assumption that financial incentives are the key element in explaining the success of managed care plans in reducing the utilization of services.11,18,25 Our findings also suggest that health care delivery systems that utilize a primary care gatekeeper can be effective and acceptable to patients in public settings.
Acknowledgments
The authors thank Diane Miller and Phil Hopewell, MD, for their support, Anna Napoles-Springer and Anita Stewart, PhD, for their assistance with the patient survey, Kim Tally for her technical assistance, Kevin Grumbach, MD, and Jennifer Haas, MD, for their editorial comments, and Chris Rusev, RN, Roberto Alaniz, MPH, and the entire staff of the General Medical Clinic at SFGH for their contributions that led to the preparation of this manuscript.
REFERENCES
- 1.Kreier R. HMOs without gatekeepers. Am Med News. 1996;39(29):1. [Google Scholar]
- 2.Freudenheim M. Medical insurers revise cost-control efforts. 1999. New York Times. December 3, A1.
- 3.Grembowski D, Cook K, Patrick D, Roussel A. Managed care and physician referral. Med Care Res Rev. 1998;55:3–31. doi: 10.1177/107755879805500101. [DOI] [PubMed] [Google Scholar]
- 4.Kerr E, Mittman B, Hays R, Siu A, Leake B, Brook R. Managed care and capitation in California: how do physicians at financial risk control their own utilization? Ann Intern Med. 1995;123:500–4. doi: 10.7326/0003-4819-123-7-199510010-00004. [DOI] [PubMed] [Google Scholar]
- 5.Felt-Lisk S. How HMOs structure primary care delivery. Managed Care Q. 1996;4:96–105. [PubMed] [Google Scholar]
- 6.Rosenbaum S. A look inside Medicaid managed care. Health Aff. 1997;16:266–71. doi: 10.1377/hlthaff.16.4.266. [DOI] [PubMed] [Google Scholar]
- 7.Rowland D, Hanson K. Medicaid: moving to managed care. Health Aff. 1996;15:150–2. doi: 10.1377/hlthaff.15.3.150. [DOI] [PubMed] [Google Scholar]
- 8.Hurley R, Freund D, Gage B. Gatekeeper effects on patterns of physician use. J Fam Pract. 1991;32:167–73. [PubMed] [Google Scholar]
- 9.National Public Health and Hospital Institute. Survey of Managed Care Programs for the Indigent. Washington, DC: National Public Health and Hospital Institute; 1996. [Google Scholar]
- 10.Sisk J, Gorman S, Reisinger A, Glied S, DuMouchel W, Hynes M. Evaluation of Medicaid managed care. JAMA. 1996;276:50–5. [PubMed] [Google Scholar]
- 11.Long S, Settle R. An evaluation of Utah's primary care case management program for Medicaid recipients. Med Care. 1988;26:1021–32. doi: 10.1097/00005650-198811000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Schoenman J, Evans W, Schur C. Primary care case management for Medicaid recipients: evaluation of the Maryland Access to Care program. Inquiry. 1997;34:155–70. [PubMed] [Google Scholar]
- 13.Martin D, Diehr P, Price K, Richardson W. Effect of a gatekeeper plan on health services use and charges: a randomized trial. Am J Public Health. 1989;79:1628–32. doi: 10.2105/ajph.79.12.1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Manning W, Leibowitz A, Goldberg G, Rogers W, Newhouse J. A controlled trial of the effect of a prepaid group practice on use of services. N Engl J Med. 1984;310:1505–10. doi: 10.1056/NEJM198406073102305. [DOI] [PubMed] [Google Scholar]
- 15.Rice T. Physician payment policies: impacts and implications. Annu Rev Public Health. 1997:549–65. doi: 10.1146/annurev.publhealth.18.1.549. [DOI] [PubMed] [Google Scholar]
- 16.Hillman A, Pauly M, Kerstein J. How do financial incentives affect physicians' clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989;321:86–92. doi: 10.1056/NEJM198907133210205. [DOI] [PubMed] [Google Scholar]
- 17.Stearns S, Wolfe B, Kindig D. Physician response to fee-for-service and capitation payment. Inquiry. 1992;29:416–25. [PubMed] [Google Scholar]
- 18.Hellinger F. The impact of financial incentives on physician behavior in managed care plans: a review of the evidence. Med Care Res Rev. 1996;53:294–314. doi: 10.1177/107755879605300305. [DOI] [PubMed] [Google Scholar]
- 19.Cary, NC: Sas Institute Inc.; 1997. SAS/STAT Software: Changes and Enhancements through Release 6.12; pp. 571–701. [Google Scholar]
- 20.Efron B, Tibshirani RJ. An Introduction to the Bootstrap. London, UK: Chapman and Hall; 1993. pp. 178–88. 214–8, 398–403. [Google Scholar]
- 21.The Medicaid Access Study Group: access of Medicaid recipients to outpatient care. N Engl J Med. 1994:1426–30. doi: 10.1056/NEJM199405193302007. [DOI] [PubMed] [Google Scholar]
- 22.Weinberger M, Oddone E, Henderson W, et al. Does increased access to primary care reduce hospital readmissions? N Engl J Med. 1996;334:1441–7. doi: 10.1056/NEJM199605303342206. [DOI] [PubMed] [Google Scholar]
- 23.Bodenheimer T, Lo B, Casalino L. Primary care physicians should be coordinators, not gatekeepers. JAMA. 1999;281:2045–8. doi: 10.1001/jama.281.21.2045. [DOI] [PubMed] [Google Scholar]
- 24.Blumenthal D, Mort E, Edwards J. The efficacy of primary care for vulnerable population groups. Health Serv Res. 1995;30:253–73. [PMC free article] [PubMed] [Google Scholar]
- 25.Conrad D, Maynard C, Cheadle A, et al. Primary care physician compensation methods in medical groups. JAMA. 1998;279:853–8. doi: 10.1001/jama.279.11.853. [DOI] [PubMed] [Google Scholar]