Abstract
OBJECTIVE
To examine factors associated with variation in the quality of care for women with 2 common breast problems: an abnormal mammogram or a clinical breast complaint.
DESIGN
Cross-sectional patient survey and medical record review.
SETTING
Ten general internal medicine practices in the Greater Boston area.
PARTICIPANTS
Women who had an abnormal radiographic result from a screening mammogram or underwent mammography for a clinical breast complaint (N = 579).
MEASUREMENTS AND MAIN RESULTS
Three measures of the quality of care were used: (1) whether or not a woman received an evaluation in compliance with a clinical guideline; (2) the number of days until the appropriate resolution of this episode of breast care if any; and (3) a woman's overall satisfaction with her care. Sixty-nine percent of women received care consistent with the guideline. After adjustment, women over 50 years (odds ratio [OR], 1.58; 95%[CI], 1.06 to 2.36) and those with an abnormal mammogram (compared with a clinical breast complaint: OR, 1.75; 95% CI, 1.16 to 2.64) were more likely to receive recommended care and had a shorter time to resolution of their breast problem. Women with a managed care plan were also more likely to receive care in compliance with the guideline (OR, 1.72; 95% CI, 1.12 to 2.64) and have a more timely resolution. There were no differences in satisfaction by age or type of breast problem, but women with a managed care plan were less likely to rate their care as excellent (43% vs 53%,P < .05).
CONCLUSIONS
We found that a substantial proportion of women with a breast problem managed by generalists did not receive care consistent with a clinical guideline, particularly younger women with a clinical breast complaint and a normal or benign-appearing mammogram.
Keywords: quality of care, mammography, guidelines
With the growth of managed care, primary care physicians are playing a central role in the management of common women's health problems, including the evaluation of abnormal mammograms and clinical breast complaints (e.g., breast lumps or pain). Though the vast majority of women seen for these problems do not have breast cancer, a delay in diagnosis can be catastrophic. Over the past decade, several noninvasive or minimally invasive tests (e.g., ultrasound and fine-needle aspiration) have been added to the diagnostic armamentarium for breast problems, but it is unclear whether these tests have been integrated into the evaluation of women with breast problems in a coherent manner, or rather have fostered confusion about what constitutes an appropriate evaluation.
For these reasons the management of breast problems is complicated for primary care physicians. This challenge is reflected by the observation that failure to diagnose breast cancer in a timely manner is currently the leading cause of malpractice claims in the United States.1 It is also the most costly claim made against physicians. Reflecting these trends, breast cancer claims filed against physicians insured by the Harvard University malpractice insurer, CRICO, have increased dramatically in recent years.2 In general, the most common claim involves a premenopausal woman with a self-identified breast complaint, a normal or probably benign mammogram result, and no further evaluation. The principal allegation is failure to diagnose breast cancer.2
Because of the growing liability associated with breast problems and the potential for variation in the evaluation of these problems, the goal of this study, conducted at 10 Harvard-affiliated primary care practices, was to examine factors associated with variation in the quality of care for women with the 2 most common breast problems managed by general internists: an abnormal mammogram result or a clinical breast concern.
METHODS
Setting
Women were recruited from 1 of 10 participating general internal medicine practices in the Greater Boston area. Participating sites all received malpractice coverage through the Harvard University–affiliated insurance program (CRICO), but were diverse in location, structure, and the degree of academic affiliation. Participation of the clinical sites in this project was encouraged by CRICO as part of the risk management activities conducted at all of its insured institutions. The sites included 5 hospital-based practices, 1 university health service, 1 large group-model HMO, 2 neighborhood health centers in disadvantaged communities, and 1 suburban group practice. The study was approved by the institutional review board of each institution.
Patients
The goal of the study was to examine the care that women received for 2 common breast problems managed by general internists. Women were eligible for this study if (1) they received an abnormal radiographic result from a screening mammogram (i.e., the results were indeterminate or aroused suspicion of cancer, or there was a recommendation for nonroutine follow-up including additional or magnification views, mammography within the following 12 months, ultrasound examination, fine-needle aspiration, or biopsy), or (2) they underwent mammography for a clinical breast concern (i.e., lump, thickening, breast pain that persisted for longer than 1 menstrual cycle) regardless of the result of the mammogram. Women were initially identified by reviewing the mammogram reports from each of the participating facilities. Because our study question focused on the management of these women by general internists, patients were eligible for the study if they (1) had had at least 1 visit to their attending-level primary care physician during the year prior to their index mammogram, (2) fit 1 of the 2 eligibility categories defined above, (3) underwent mammography at the principal radiology site used by that practice, (4) were English or Spanish speaking, (5) had not previously been diagnosed with breast cancer, and (6) had not been evaluated for an abnormal mammogram or breast complaint within the preceding year.
Data Collection
Eligible women were sent an informational letter about the study and asked to return an “opt-out” postcard if they did not want to participate. Attempts were made to contact women who did not return a postcard by telephone to complete a “baseline” telephone survey within 6 to 8 weeks of their index mammogram. All of the baseline surveys were conducted between June 1996 and June 1997. Women who agreed to participate in the baseline survey were also contacted for a “follow-up” telephone survey 7 to 8 months after their index mammogram. All of the follow-up surveys were conducted between November 1996 and November 1997. The medical records of all eligible women (i.e., survey respondents and nonrespondents) were reviewed after the time indicated for the follow-up survey.
The baseline telephone survey included questions about sociodemographic characteristics, risk factors for breast cancer, degree of worry about breast cancer before the index mammogram, type of subsequent evaluation (if any), and overall satisfaction with their subsequent medical care for their breast problem (rated as poor to excellent on a 5-point scale). The follow-up survey asked about their overall satisfaction with their medical care for their breast problem and about evaluation completed since the baseline interview. Women who reported a diagnosis of breast cancer at the time of the baseline interview were not recontacted for a follow-up survey. Trained nurse reviewers abstracted medical records for information about the type of subsequent evaluation for the breast problem, the date of subsequent tests, and their results.
Analytic Variables
Our principal interest was to examine what factors affect the quality of care for women with an abnormal mammogram or a breast complaint. We focused on 3 measures of the quality of care. One measure was whether or not a woman had received an evaluation that was in compliance with a guideline for the management of common breast problems published by the Harvard Risk Management Foundation (a CRICO subsidiary) in its quarterly newsletter circulated to all of its insured physicians (summarized in Table 1)2,3 If a woman reported care consistent with this guideline during the baseline survey, or a consistent evaluation was noted on review of her medical records, her care was judged to be in compliance with these recommendations. Another measure was the number of days from the time of the index mammogram until the appropriate resolution of this episode of breast care (if any). For women diagnosed with breast cancer, this was calculated using the date of diagnosis. For other women, it was calculated using the date of the final test that was done for the breast problem if her evaluation was consistent with the guideline described in Table 1. For women who did not receive care consistent with the guideline, the date of the chart review was used as the date of censoring in the Cox models described below. The third measure was a woman's overall satisfaction with the quality of care that she received for her breast problem, both at the baseline and at the follow-up surveys. For ease of presentation this is categorized as excellent versus other responses.
Table 1.
Compliance with Algorithm for Common Breast Problems(3)*
| Clinical Problem | Appropriate Evaluation |
|---|---|
| Mammographic abnormality on screening exam with no history or physical exam findings of a breast lump | |
| Biopsy recommended | Biopsy (open, core) |
| Additional imaging | Clinical breast exam within the 12 mo prior to the index mammogram and the additional imaging suggested by the radiologist (e.g., magnification views, ultrasound, follow-up mammogram) |
| Palpable breast mass or lump with normal or probably benign mammogram result | Ultrasound demonstrating a cyst, or aspiration of fluid, and follow-up breast exam or ultrasound to exclude persistence or recurrence of the finding. (if there is recurrence or persistence of the finding, the patient should be referred to a surgeon), or |
| Follow-up breast exam documenting resolution, or | |
| Biopsy (i.e., open, core) of any persistent mass or nodularity | |
| Breast pain persisting for more than 1 mo (without lump) | Clinical breast exam within 12 mo of the index mammogram and a normal or probably benign mammogram result |
The source of the algorithm was Smith (1995).3
Predictor variables examined included a woman's age at the time of the index mammogram, any family history of breast cancer, race or ethnicity, level of education, insurance status, radiographic result of the index mammogram, the degree of a woman's worry about breast cancer before the time of the index mammogram (5-point scale from not at all worried to extremely worried), and site of care.
Statistical Analysis
The analysis was based on women who responded to the baseline survey. Descriptive statistics were used to examine the association between potential independent variables and the outcomes of interest. Initial comparisons were made using a χ2test for categorical data and the Wilcoxon rank sum test for continuous data. Logistic regression models were used to examine factors that were independently associated with compliance with the guideline.4 Cox models were used to examine factors associated with the time to resolution of the breast complaint.5 For these models, we assigned censored values to women who did not have a date of resolution noted at the end of the chart review period.
Associations were examined for the overall sample and then separately for the subgroups of women with an abnormal mammogram result or a clinical breast complaint. Since the multivariate models were descriptive, independent variables were selected based on a priori decisions (e.g., family history of breast cancer) or significant univariate associations. Because there were few eligible women from the 2 community health centers and the results from these sites were similar, data from these 2 sites were aggregated.
RESULTS
Response Rates
Of the 751 women who were eligible to participate, 579 (77%) completed the baseline telephone survey, 97 (13%) refused to participate, and 75 (10%) could not be reached by telephone after at least 10 attempts. Of the 579 women who completed the baseline survey, 26 were diagnosed with breast cancer and therefore were not eligible for the follow-up survey, and 447 (77%) completed the follow-up survey.
Some demographic information was available from medical record review to compare the survey respondents with the nonrespondents. There were no differences between these groups for age, eligibility group (i.e., abnormal mammogram vs breast lump), whether a woman received care in compliance with the clinical guideline (based on chart review data only), degree of mammographic abnormality, payer, or site of care. Among women who had responded to the first survey, there were no differences in age, eligibility group, degree of worry about breast cancer, family history, level of education, or site of care between women who responded to the follow-up survey and those who did not. Women who responded to both surveys were more likely to be white (80% vs 69%; P = .005) than women who responded only to the baseline survey.
Characteristics of the Participants
Overall, 68% of participants were eligible for the study because of an abnormal screening mammogram and 32% were eligible because of a clinical breast concern. The characteristics of the study population are displayed in Table 2). Women with a clinical breast complaint were younger and more likely to be worried about the possibility of breast cancer than women eligible because of an abnormal screening mammogram. Women with a clinical breast complaint also were more likely to be diagnosed with breast cancer as a result of their evaluation.
Table 2.
Characteristics of the Study Population
| Eligibility Group, n(%) | ||
|---|---|---|
| Characteristic | Abnormal Screening Mammogram (N = 392) | Clinical Breast Complaint (N = 187) |
| Age, y | ||
| <50 | 179 (45.7) | 114 (61.0)* |
| ≥50 | 213 (54.3) | 73 (39.0) |
| Race | ||
| White | 295 (76.0) | 136 (72.7) |
| African American | 60 (15.5) | 24 (12.8) |
| Hispanic | 16 (4.1) | 17 (9.1) |
| Other, nonwhite | 17 (4.4) | 10 (5.4) |
| Education | ||
| High school or less | 83 (21.6) | 44 (23.8) |
| Some college | 190 (49.4) | 96 (51.8) |
| Beyond college | 112 (29.1) | 45 (24.3) |
| Payer | ||
| Managed care | 241 (62.3) | 107 (57.2) |
| Commercial | 101 (26.1) | 51 (27.3) |
| Medicaid | 11 (2.8) | 7 (3.7) |
| Medicare | 18 (4.7) | 15 (8.0) |
| Uninsured | 16 (4.1) | 7 (3.7) |
| Family history of breast cancer | 102 (26.2) | 54 (29.4) |
| Degree of worry about breast cancer prior to mammogram | ||
| Not at all worried/a little worried | 335 (85.5) | 134 (71.7)* |
| Very/somewhat worried | 57 (14.5) | 53 (28.3) |
| Radiologist's recommendation for further care based on index mammogram | ||
| Biopsy | 51 (13.0) | 19 (10.2)* |
| Nonroutine follow-up mammogram (<12 mo) | 115 (29.3) | 11 (5.9) |
| Routine or 12-mo follow-up† | 165 (42.1) | 81 (43.3) |
| Follow-up as clinically indicated | 61 (15.6) | 76 (40.6) |
| Diagnosed with breast cancer during the 6 mo following the index mammogram | 13 (3.3) | 14 (7.5)‡ |
P,.005 for comparison between women with an abnormal mammogram and those with a clinical breast complaint.
Women in the abnormal mammogram group with the recommendation of routine follow-up were included in this study because of the performance of additional compression or magnification views, ultrasound, or other additional testing by the radiologist at the time of the index mammogram.
P <.05 for comparison between women with and abnormal mammogram and those with a clinical breast complaint.
Factors Associated with Compliance with the Guideline
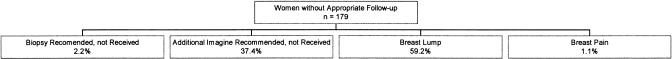
Overall, only 69.1% of women received care that was consistent with the recommendations of the breast care guideline. Figure 1 shows the general categories of breast problems that did not receive follow-up that was in compliance with the algorithm. The majority of women who did not receive care in compliance with this clinical algorithm had a palpable breast lump (59.2%). Few women received care that was noncompliant with the algorithm because a biopsy was recommended but not received (2.2%) or because of breast pain (1.1%).
FIGURE 1.
Reasons for noncompliance with the breast care algorithm.
Table 3 shows the relation between patient characteristics, compliance with the breast care guideline, and the timeliness of the resolution of the breast problem. After adjustment for family history of breast cancer, race, severity of mammographic abnormality, degree of worry about breast cancer, eligibility category, insurance status, and site of care, women who were older than 50 years were more likely to receive care that complied with the guideline than were younger women. Women with an abnormal mammogram were more likely to receive care that was consistent with the guideline than were women with a clinical breast complaint. Women with a managed care plan were also more likely to receive care in compliance with guideline than were women with other payers. Over 90% of women with a mammogram result suggesting the need for biopsy received one. After adjustment, 1 study site was statistically more likely to provide care in compliance with the clinical guideline.
Table 3.
Compliance with Breast Care Guideline and Timeliness of Resolution of Breast Problem
| Characteristic | Compliance with Breast Care Guideline, % | Adjusted* Odds Ratio for Compliance (95% Confidence Interval) | Adjusted* Hazard Ratio for Days Until Resolution of Breast Problem (95% Confidence Interval) |
|---|---|---|---|
| Eligibility criteria | |||
| Abnormal mammogram (n = 392) | 74.0† | 1.75 (1.16 to 2.64) | 1.07 (0.84 to 1.35) |
| Clinical breast complaint (n = 187) | 58.8 | — | — |
| Age, y | |||
| <50 (n = 293) | 63.8† | — | — |
| ≤50 (n = 286) | 74.5 | 1.58 (1.06 to 2.36) | 1.23 (1.01 to 1.51) |
| Race/ethnicity | |||
| White (n = 431) | 71.0 | — | — |
| African American (n = 84) | 59.5 | 0.67 (0.42 to 1.07)‡ | 0.92 (0.71 to 1.20)‡ |
| Hispanic (n = 33) | 75.8 | ||
| Other (n = 27) | 55.6 | ||
| Family history of breast cancer | |||
| Yes (n = 156) | 69.2 | 1.08 (0.70 to 1.67) | 1.01 (0.80 to 1.27) |
| No (n = 417) | 68.8 | — | — |
| Payer | |||
| Managed care (n = 348) | 73.3† | 1.72 (1.12 to 2.64) | 1.32 (1.05 to 1.67) |
| Other payer (n = 226) | 62.0 | — | — |
| Degree of worry | |||
| Not at all/a little worried (n = 469) | 70.2 | — | — |
| Very/somewhat worried (n = 110) | 64.6 | 0.79 (0.48 to 1.29) | 1.11 (0.84 to 1.46) |
| Radiologist's recommendation for further care based on index mammogram | |||
| Biopsy (n = 70) | 94.3† | 10.77 (3.71 to 31.25) | 3.69 (2.74 to 4.98) |
| Other (n = 509)§ | 65.7 | — | — |
| Site of primary care | |||
| A (n = 55) | 63.6‖ | — | — |
| B (n = 49) | 59.2 | 1.29 (0.54 to 3.11) | 1.15 (0.69 to 1.91) |
| C (n = 97) | 68.0 | 1.25 (0.58 to 2.69) | 0.99 (0.65 to 1.51) |
| D (n = 90) | 61.1 | 1.28 (0.60 to 2.74) | 1.01 (0.65 to 1.57) |
| E (n = 28) | 75.0 | 2.24 (0.75 to 6.70) | 1.49 (0.85 to 2.60) |
| F (n = 48) | 70.8 | 1.95 (0.79 to 4.81) | 1.20 (0.74 to 1.97) |
| G (n = 114) | 72.8 | 1.59 (0.72 to 3.53) | 1.21 (0.79 to 1.85) |
| H (n =80) | 83.8 | 4.03 (1.69 to 9.61) | 1.79 (1.17 to 2.75) |
| I (n = 18) | 55.6 | 1.28 (0.38 to 4.29) | 0.90 (0.43 to 1.90) |
Adjusted for age, family history of breast cancer, race, severity of mammographic abnormality, degree of worry about breast cancer, eligibility category, insurance status, and site of care.
P < .005 for comparison within characteristic.
Comparison is for nonwhite compared with white patients.
Includes 6-month follow-up, 12-month (routine) follow-up, follow-up as clinically indicated.
P < .05 for comparison within characteristic
Among women with a date of resolution noted, the median number of days to resolve the episode of breast care was 61 (range, 0 – 289). Women received a more timely evaluation for their breast problem if they were older, belonged to a managed care plan, or had a more significant radiographic abnormality. For example, on a given day, older women were 23% more likely to have had their breast problem resolved than were younger women.
In our principal analysis, we did not include information from the follow-up survey because we were concerned that women who did not respond to the second survey would bias our conclusions. In a secondary analysis, we included women's reports of care from the follow-up survey to capture information that may not have been available from chart review (e.g., off-site care). Including the follow-up survey data only increased the compliance rate from 69.1% to 69.4%.
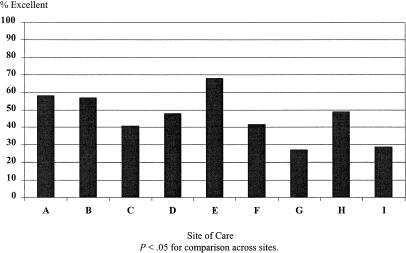
Patient-Reported Quality of Breast Care
Satisfaction with the quality of breast care was modest. Overall, 46.8% reported excellent care during the baseline survey and 45.8% noted excellent care during the follow-up survey. White women were significantly more satisfied with the quality of their breast care than women of other racial groups (Table 4). Despite greater compliance with the breast care guideline noted above, women with a managed care plan were less likely to report excellent satisfaction with the quality of their breast care at the time of the baseline survey. There was also significant variation in patient-reported quality of care by site at the time of the follow-up survey (Fig. 2). Compliance with the breast care guideline was not associated with patient-reported quality of care at either the baseline or follow-up interview (P = .41 for both comparisons).
Table 4.
Patient-Reported Quality of Breast Care*
| Women Reporting Excellent Overall Quality of Breast Care | ||
|---|---|---|
| Characteristic | Baseline Survey (N = 579) | Follow-up Survey (N = 447) |
| Eligibility criteria | ||
| Abnormal mammogram | 46.6 | 44.9 |
| Clinical breast complaint | 47.2 | 47.5 |
| Age, y | ||
| <50 | 44.4 | 46.6 |
| ≥50 | 49.3 | 44.9 |
| Race/ethnicity | ||
| White | 51.9† | 49.8‡ |
| African American | 35.9 | 35.6 |
| Hispanic | 33.3 | 25.0 |
| Other | 18.5 | 35.7 |
| Family history of breast cancer | ||
| Yes | 47.1 | 52.0 |
| No | 46.3 | 43.4 |
| Payer | ||
| Managed care | 42.9‡ | 42.4 |
| Other payer | 52.8 | 50.7 |
| Degree of worry | ||
| Not at all/a little worried | 48.2 | 46.6 |
| Very/somewhat worried | 40.7 | 42.5 |
| Radiologist's recommendation for further care based on index mammogram | ||
| Biopsy | 45.7 | 49.9 |
| Other§ | 47.0 | 45.3 |
Unadjusted P < .05 for comparison within characteristic.
Unadjusted P < .005 for comparison within characteristic.
Includes recommendation for additional imaging, follow-up as clinically indicated, and routine follow-up.
Note: Some categories include missing data.
FIGURE 2.
Patient-reported quality of care for breast problem.
Women with an Abnormal Mammogram
Among the subgroup of women with an abnormal mammogram, women who were at least 50 years old (odds ratio [OR], 1.76; 95% confidence interval [CI], 1.06 to 2.92), those with a managed care plan (OR, 2.49; 95% CI, 1.41 to 4.36), and women with a more significant mammographic abnormality (OR, 6.04; 95% CI, 2.01 to 18.19) were more likely to receive care that was in compliance with the clinical guideline. Nonwhite women were less likely than white women to receive care in compliance with the guideline (OR, 0.54; 95% CI, 0.30 to 0.97). Among women with an abnormal mammogram result and a date of resolution noted (i.e., not censored), the unadjusted median time to resolution was 159 days (range, 0–260 days).
Women with a Clinical Breast Complaint
Among the subgroup of women with a clinical breast complaint, no factors were significantly associated with compliance with the clinical guideline or the timelines of resolution. Among women with a clinical breast complaint and a date of resolution recorded (i.e., not censored), the unadjusted median time to resolution was 28 days (range, 0–289 days).
Women Diagnosed with Breast Cancer
Twenty-seven women were diagnosed with breast cancer during the course of this study. Women with a clinical breast complaint were more likely to be diagnosed with breast cancer than women with an abnormal mammogram (Table 2). Women over 50 years of age were more likely to be diagnosed with breast cancer than younger women (7.3% vs 2.1%, P = .003). There were no differences in the rate of breast cancer by race, education, insurance status, family history, or site of care, although the small number of women with breast cancer limits our conclusions about these associations.
DISCUSSION
The evaluation of women with an abnormal mammogram or a breast complaint is a common clinical problem faced by primary care providers. Our work suggests that a substantial proportion of women with a breast problem managed in these general internal medicine practices did not receive care consistent with a locally disseminated clinical guideline, particularly younger women with a clinical breast complaint and a normal or probably benign mammogram result. Women with managed care insurance were more likely to receive care consistent with the guideline. There were no associations between patient-reported satisfaction with care and compliance with the guideline. Minority women and those with managed care reported being less satisfied. Finally, there was significant variation in quality of care by practice site.
Our work offers some explanation as to why failure to diagnose breast cancer has become the leading, and most costly, cause of malpractice claims in the United States.6 Although the degree to which delayed diagnosis of breast cancer affects survival is controversial,7,8 most malpractice claims for failure to diagnose breast cancer allege a significant and avoidable delay. Paralleling national and local claim trends, in our study it is younger women with clinical breast complaints and “reassuring” mammograms who are less likely to receive care that is consistent with the clinical guideline. These findings suggest that the growth of claims among younger women is not solely related to biologic differences in the aggressiveness of tumors in younger versus older women,9 or to the lower sensitivity of screening mammography for younger women,10 but is at least in part due to problems with the quality of care.
Recent studies question whether malpractice litigation is a deterrent to poor quality care.11,12 Although our finding that younger women with clinical breast complaints were less likely to receive care consistent with a clinical guideline parallels the growth of malpractice claims among such women, our findings suggest that “substandard” care is more prevalent than the claims alone would suggest. The observed variation in care and satisfaction by practice site also suggests that efforts should be taken to ensure standard care for these women.
Why did many women with these common breast complaints not receive care consistent with this local clinical guideline? Although the guideline was distributed to all of the providers at these sites in an issue of a newsletter devoted to the management of breast problems,2,3 it is unknown whether these physicians were familiar with the guideline. A proliferation of diagnostic tests may leave general internists confused as to how to coherently integrate these tests into practice. Primary care physicians may be wary of the significant “false-positive” rate of screening mammography. One recent study demonstrated that over a 10-year period one third of women screened in a community setting had an abnormal mammogram requiring further evaluation without documented breast cancer.13 Conversely, both physicians and patients may be falsely reassured by a normal or benign-appearing mammogram in the setting of a clinical breast complaint and not pursue further evaluation even though it may be warranted. This study suggests that this group should be targeted for interventions to improve the quality of their care. In particular, the potential for “false-negative” diagnostic tests in the setting of a clinical breast complaint should be better understood by patients and physicians.
Though women with a clinical breast complaint were less likely to receive care consistent with the clinical guideline than women with an abnormal mammogram, this sample of general internists saw more women with abnormal mammogram results than with a clinical breast complaint. Among the subgroup of women with an abnormal mammogram result, older women, those with managed care, and those with a more troubling radiographic finding were more likely to receive care consistent with the guideline. The majority of women with an abnormal finding were interpreted as needing further evaluation. Though the likelihood that a woman has breast cancer after this type of finding is mostly determined by her age-specific risk,14 that younger women were less likely to receive recommended follow-up is of concern.
As part of a quality improvement initiative directed at women with common breast problems at these primary care practices, follow-up of women who received care that does not meet the standard defined by this clinical algorithm is being conducted. These sites have been instituting and evaluating local quality improvement initiatives for women with common breast problems, particularly focusing on women with a breast complaint and a reassuring mammogram.
It is unlikely that the providers at these sites actively disregarded this clinical algorithm because they disagreed with the management recommended. The guideline used to measure the quality of care for these common breast problems, developed using a multidisciplinary panel of local clinical experts, is similar to the evaluation recommended by a national consensus panel.15 Clinical guidelines have been thought of as an important tool for standardizing the quality of care and also protecting physicians against liability claims by defining a standard of care.16 Though this guideline does not recommend a target benchmark, the moderate rates of compliance observed in this study suggest that there are barriers to dissemination and implementation. Future efforts to improve the care of women with breast problems should examine barriers to the implementation of clinical guidelines.
Better compliance with the guideline was not associated with better satisfaction. Of note, women with a managed care plan received care more consistent with the guideline, but were less satisfied. These observations highlight the importance of examining “quality” using an integrated approach that includes measuring process of care and patient-reported outcomes. The small number of women diagnosed with breast cancer during the period of this study limits our ability to examine the relation between the quality of care and the timely diagnosis of breast cancer.
Other studies have suggested that nonwhite women may experience delayed resolution of an abnormal mammogram result.17 Though our study did not show differences in guideline compliance or timeliness of care by race, African-American women were less satisfied, perhaps creating barriers to future care. As the mortality rate from breast cancer is higher for African-American women than for white women,18 at least in part because African-American women present with more advanced disease,19,20 future work should address racial differences in satisfaction with care and barriers to seeking care.
Our study was designed to look at the evaluation of women with a variety of common breast problems from the perspective of the general internist, not to look at the predictive value of any specific physical finding or diagnostic test. We used a local clinical guideline, with recommendations similar to those of a national consensus panel, for the management of a variety of breast problems seen by primary care providers as our standard. Like most clinical guidelines, it is based on clinical judgment. Although the guideline was published in a newsletter received by all of the physicians practicing at the study sites, we do not know whether all physicians were familiar with it or agreed with its recommendations. Our principal analysis of whether a woman had received care consistent with the guideline does not include information from the follow-up patient survey because of concern about potential bias introduced by the nonrespondents. A secondary analysis including this information suggests that women seeking follow-up care at other sites did not explain the modest compliance with the algorithm that we observed. Our sites were all located in the Greater Boston area and all received malpractice coverage through the malpractice insurer for the Harvard-affiliated institutions and therefore may not be generalizable to other settings. These primary care practices, however, are diverse in size, organizational structure, and degree of academic affiliation.
Our work suggests that there is substantial variation in the quality of care for women with breast complaints evaluated by general internists. In particular, younger women and those with a clinical breast complaint and a normal or benign-appearing mammogram may be at risk of receiving substandard care. These findings parallel the recent growth of liability claims filed by younger women with clinical breast complaints. Interventions directed at primary care providers should be designed to improve the quality of care for women with common breast problems.
Acknowledgments
We gratefully acknowledge the programming assistance of Karen Vranizan and Jane Soukup. The authors thank Martha Byington, Christopher Coley, MD, Priscilla Dasse, RN, Mark Eisenberg, MD, Alan Jacobson, MD, Betsy Johnson, MD, Randy Stafford, MD, Robert Hartley, MD, Sherry Haydock, MD, Phyllis Jen, MD, Risa Korn, MD, Gila Kriegel, MD, Richard Parker, MD, Russell Phillips, MD, and Linda Temte, MD for their support of this project.
This work was supported by a grant from the Harvard Risk Management Foundation. Dr. Haas was the recipient of a Clinical Investigator Award from the National Institute of Child Health and Human Development (K08-HD01029) when this work was conducted.
REFERENCES
- 1.Diercks DB, Cady B. Lawsuits for failure to diagnose breast cancer. Surgi Oncol Clin Am. 1994;3(1):125–36. [Google Scholar]
- 2.Schaefer MA, editor. Risk Management and Breast Cancer. Cambridge, Mass: 1998. Vol 19. ed. [Google Scholar]
- 3.Smith B. Forum: Harvard Risk Management Foundation. 1995. Algorithms for management of common breast complaints; pp. 1–5. [Google Scholar]
- 4.Hosmer DW, Lemeshow S. Applied Logistic Regression. New York, NY: John Wiley and Sons; 1989. [Google Scholar]
- 5.Cox DR. Regression models and life tables. J R Stat Soc B. 1972;34:187–220. [Google Scholar]
- 6.Dewar MA, Love N. Legal issues in managing breast disease. Postgrad Med. 1992;92(5):137–51. doi: 10.1080/00325481.1992.11701489. [DOI] [PubMed] [Google Scholar]
- 7.Spratt JS, Spratt SW. Medical and legal implications of screening and follow-up procedures for breast cancer. Cancer. 1990;66(6 suppl):1351–62. doi: 10.1002/1097-0142(19900915)66:14+<1351::aid-cncr2820661410>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 8.Plotkin D, Blankenberg F. Breast cancer: biology and malpractice. Am J Clin Oncol. 1991;14(3):254–66. doi: 10.1097/00000421-199106000-00014. [DOI] [PubMed] [Google Scholar]
- 9.Moskowitz M. Breast cancer: age-specific growth rates and screening strategies. Radiology. 1986;161:37–41. doi: 10.1148/radiology.161.1.3532183. [DOI] [PubMed] [Google Scholar]
- 10.Kerlikowske K, Grady D, Barclay J, Sickles EA, Ernster V. Effect of age, breast density and family history on the sensitivity of first screening mammography. JAMA. 1996;276(1):33–8. [PubMed] [Google Scholar]
- 11.Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence. N Engl J Med. 1991;325:245–51. doi: 10.1056/NEJM199107253250405. [DOI] [PubMed] [Google Scholar]
- 12.Brennan TA, Localio AR, Leape LL, et al. Identification of adverse events occurring during hospitalization: a cross-sectional study of litigation, quality assurance, and medical records at two teaching hospitals. Ann Intern Med. 1990;112:221–6. doi: 10.7326/0003-4819-112-3-221. [DOI] [PubMed] [Google Scholar]
- 13.Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Ten-year risk of false positive screening mammograms and clinical breast examinations. N Engl J Med. 1998;338(16):1089–96. doi: 10.1056/NEJM199804163381601. [DOI] [PubMed] [Google Scholar]
- 14.Kerlikowske K, Grady D, Barclay J, Sickles EA, Ernster V. Likelihood ratios for modern screening mammography: risk of breast cancer based on age and mammographic interpretation. JAMA. 1996;276:39–43. doi: 10.1001/jama.276.1.39. [DOI] [PubMed] [Google Scholar]
- 15.Cady B, Steele Gd, Jr, Morrow M, et al. Evaluation of common breast problems: guidance for primary care providers. CA Cancer J Clin. 1998;48(1):49–63. doi: 10.3322/canjclin.48.1.49. [DOI] [PubMed] [Google Scholar]
- 16.King JY. Practice guidelines and medical malpractice litigation. Med Law. 1997;16(1):29–39. [PubMed] [Google Scholar]
- 17.Chang SW, Kerlikowske K, Napoles-Springer A, Posner SF, Sickles EA, Perez-Stable EJ. Racial differences in timeliness of follow-up after abnormal screening mammography. Cancer. 1996;78:1395–402. doi: 10.1002/(SICI)1097-0142(19961001)78:7<1395::AID-CNCR5>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 18.Howard J, Hankey BF, Greenberg RS, et al. A collaborative study of differences in the survival rates of black patients and white patients with cancer. Cancer. 1992;69(9):2349–60. doi: 10.1002/1097-0142(19920501)69:9<2349::aid-cncr2820690925>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 19.Eley JW, Hill HA, Chen VW, et al. Racial differences in survival from breast cancer. JAMA. 1994;272:947–54. doi: 10.1001/jama.272.12.947. [DOI] [PubMed] [Google Scholar]
- 20.Mandelblatt J, Andrews H, Kerner J, Zauber A, Burnett W. Determinants of late stage diagnosis of breast and cervical cancer. Am J Public Health. 1991;81:646–9. doi: 10.2105/ajph.81.5.646. [DOI] [PMC free article] [PubMed] [Google Scholar]