Abstract
OBJECTIVE
To determine the feasibility of cervical cancer screening in an urgent care clinic.
DESIGN
Prospective randomized trial.
SETTING
Public teaching hospital.
PATIENTS
Women presenting to the urgent care clinic whose evaluation necessitated a pelvic examination were eligible for participation. Women who had a hysterectomy, had a documented Pap test at our institution in the past year, did not speak English or Spanish, or had significant vaginal bleeding were excluded. Women presenting to the gynecology clinic for a scheduled Pap test were used as a comparison group for rates of follow-up, Pap smear adequacy, and Pap smear abnormalities.
INTERVENTIONS
Women randomized to the intervention group had a Pap test performed as part of their pelvic examination, while women in the usual care group were encouraged to schedule an appointment in the gynecology clinic at a later date. The women in the two groups completed identical questionnaires regarding cervical cancer risk factors and demographic information.
MEASUREMENTS AND MAIN RESULTS
Ninety-four (84.7%) of 111 women in the intervention group received a Pap test, as compared with 25 (29%) of 86 in the usual care group (P < .01). However, only 5 (24%) of 21 women with abnormal Pap smears in the intervention group received follow-up compared with 6 (60%) of 10 women seen during the same time period in the gynecology clinic for self-referred, routine annual examinations (P = .11). Pap smears obtained in the urgent care clinic were similar to those in the gynecology clinic with regard to abnormality rate (22.3% vs 20%; P = .75, respectively) and specimen adequacy (67% vs 72%; P = .54, respectively).
CONCLUSIONS
Urgent care clinic visits can be used as opportunities to perform Pap test screening in women who are unlikely to adhere to cervical cancer screening recommendations. However, to accrue the full potential benefit from this intervention, an improved process to ensure patient follow-up must be developed.
Keywords: cervical cancer screening, urgent care clinic, Pap smears
Cervical cancer is the most common malignancy affecting women worldwide.1 The slow natural history of cervical cancer lends itself well to a screening program that identifies dysplasia and prevents it from developing into invasive carcinoma. A large body of convincing scientific evidence supports the value of the Pap smear for reducing cervical cancer mortality by 20% to 60%.2 With mass screening programs, cervical cancer mortality rates have dropped dramatically.3,4 However, the success of mass screening has not been uniform in the United States. Data from the 1992 National Health Interview Survey showed that only 43% of women had had a recent Pap test.5 Within certain subpopulations the incidence and mortality of invasive cervical cancer notably exceed those for white, higher-income, and better-educated women.6–9 Consistent with this inequity, 38% of women with annual incomes less than $10,000 per year and 42% of women with less than a high school education have not had a Pap test within the preceding 3 years.10 Nevertheless, a high percentage of those not appropriately screened for cervical cancer have received some form of medical care within the previous 5 years.11,12
A few studies have looked at the feasibility of screening women for cervical cancer at the initial point of contact with the health care system. A review of cervical cancer screening studies in sexually transmitted disease (STD) clinics pointed out that these screening trials were successful in detecting and treating precursor lesions of cervical cancer, but follow-up was often poor.13 Studies evaluating the efficacy of performing Pap tests on patients presenting to emergency departments suffered from methodological difficulties, but did find high cervical cancer detection rates.14,15
Uninsured persons are much more likely to have current health care needs, lack a primary care physician, and depend on urgent care clinics and emergency departments for routine health care.16,17 Therefore, we undertook a project in our public hospital's urgent care clinic to evaluate and compare the feasibility of cervical cancer screening in this setting versus referral to a gynecology clinic for screening. In the measurement of feasibility our emphasis was not solely on receipt of Pap test, but focused also on the ability to achieve follow-up on women with abnormal Pap smears.
METHODS
Participants
This was a prospective randomized study conducted at Denver Health Medical Center, an acute care urban public hospital, during the period from October 1997 through December 1997. All female patients aged 18 to 70 years presenting to the urgent care departments, Monday through Friday, 8 amto 8 pm, were eligible. Women who presented to the gynecology clinic for self-scheduled annual examinations during the time of the study were used as a comparison group for Pap smear adequacy, Pap smear abnormality, and follow-up rates.
Women presenting to the urgent care clinic were approached for participation by the study coordinator after they had been assessed in the clinic's triage area and identified as having symptoms for which a pelvic examination is usually recommended, such as vaginal bleeding, vaginal discharge, or lower abdominal or pelvic pain. Providers also advised the study coordinators of women who were undergoing a pelvic examination but had not been previously identified in triage. Women were divided into the intervention and usual care groups by randomization of days at the initiation of the study using a random number table. Women in the intervention group had a Pap test performed as part of their pelvic examination in the urgent care clinic. Those in the usual care group were referred to schedule an appointment at a later date in the gynecology clinic for Pap test screening. Women in all groups were excluded if they spoke a language other than English or Spanish, had a documented Pap test at our institution in the past year, or reported having had a hysterectomy. Women were not excluded for reporting a Pap test within the preceding 12 months if we were unable to verify this information at our institution. Written consent was obtained from each participant as required by the Institutional Review Board owing to the sensitive nature of the information collected in the questionnaire. Consenting women completed a questionnaire that was available in both English and Spanish. This questionnaire contained 20 items eliciting information related to demographics, risk factors for cervical cancer, prior Pap test screening, previous treatment for abnormal Pap smears, education level, prior history of STD, and usual source of care. Only after consent was obtained and the questionnaire was completed were women notified of the group to which they were assigned. Women in both groups were given $5 for their participation in the study but were required to pay for all services that they received, including the Pap test itself and any follow-up care that was necessary. Women were alerted to this financial responsibility before consenting to participate.
Procedures
Pap smears were obtained by the care provider evaluating the patient (nurse practitioner, resident, or attending physician), using a standard single-slide technique with a combination of a cytologic brush for the endocervical component and an Ayres spatula for the exocervical component. The pathology department evaluated the Pap smears in its usual fashion and reported results according to the Bethesda protocol. For purposes of this study a Pap smear was considered abnormal if the result was reported as atypical squamous cells of unknown significance (ASCUS) or any grade of dysplasia. Evidence of infection or inadequate smears were not considered abnormal unless they were accompanied by any of the preceding descriptors. Women in the usual care group underwent a pelvic examination, but did not receive a Pap test. These women were given a card asking them to make an appointment in the gynecology clinic at a later time to have their Pap test. Although they were referred to the gynecology clinic to make their Pap test appointment, they were considered compliant with this recommendation if they had a Pap test in any of the community health clinics within our system. Women in the intervention group who had an abnormal Pap smear were tracked by the gynecology clinic according to its usual notification and treatment protocol. This consists of a tracking system wherein 3 attempts are made by mail to notify each woman with an abnormal Pap smear. The initial letter contains a follow-up appointment as well as information in English and Spanish detailing why follow-up for an abnormal Pap smear is necessary. The third letter is sent by certified mail to the last known address. After clinic visits, charts were abstracted for pregnancy status, culture results, Pap smear results, treatment for infection at the time of the initial visit, subsequent Pap smears after referral, and clinic follow-up for abnormal Pap smears. Insurance information, patient age, and patient ethnicity were taken from hospital registration records. All women were followed for 6 months before being defined as noncompliant with scheduling and attending an appointment for their Pap test or for follow-up of an abnormal Pap smear.
Data Analysis
The main outcomes measured were follow-up rates for an abnormal Pap smear. Receipt of Pap tests and the groups were compared using χ2analysis for the categorical variables or Fisher's exact test when one or more cell size was small. For continuous variables the mean ± SD was reported and compared using a 2-sample t test or nonparametric equivalent Wilcoxon rank sum test. All analyses were performed using SAS software, and statistical significance was defined using α = .05.
RESULTS
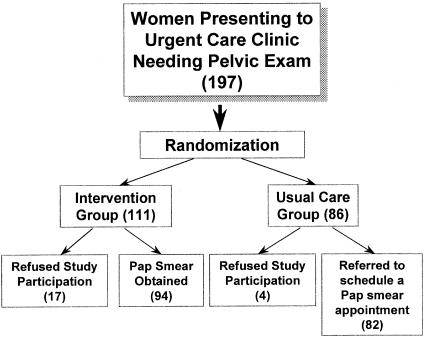
There were 197 eligible women who presented to the urgent care clinic during the study; the allocation of these women to the study groups is shown in Figure 1. Women who refused participation did not differ from women enrolled in the study in age, ethnicity, or insurance status.
FIGURE 1.
Allocation of patients to study groups.
The demographic characteristics of the intervention and usual care groups appear in Table 1. Demographic information, as well as profiles of self-reported cervical cancer risk factors, were available only for those women who consented to participate. Groups were similar with respect to age, insurance status, education, ethnicity, and self-reported history of prior abnormal Pap smears. They were also similar with regard to most of the cervical cancer risk factors, such as age at first intercourse, number of partners, current tobacco use, history of STD, and condom use. Women in the intervention group were more likely to report that they had never had a Pap test or that their last Pap test was more than 3 years ago (28% vs 12%; P = .02) and to self-report their last Pap smear as abnormal (23% vs 8%; P = .03). Women in the usual care group were more likely to report their usual site of care at our institution (74% vs 55%; P = .02).
Table 1.
Characteristics of intervention and usual care groups
| Indicator | Intervention Group* | Usual Care Group† | P value‡ |
|---|---|---|---|
| Mean age ± SD, y | 28 ± 8 | 27 ± 9 | NS |
| Insurance (%) | 19 (20) | 21 (26) | NS |
| Ethnicity, n(%) | NS | ||
| White | 21 (22) | 24 (29) | |
| Black | 23 (24) | 14 (17) | |
| Hispanic | 49 (52) | 43 (52) | |
| Other | 1 (1) | 1 (1) | |
| Last Pap>3 y ago or never, n(%) | 21 (28) | 8 (12) | .02 |
| Last Pap abnormal, n(%) | 16 (23) | 5 (8) | .03 |
| History of abnormal Pap, n(%) | 30 (36) | 18 (24) | NS |
| Last Pap at Denver Health, n(%) | 26 (37) | 19 (33) | NS |
| Record of Pap at Denver Health in last 3 y, n(%) | 12 (13) | 17 (21) | NS |
| Usual site of care is Denver Health, n(%) | 42 (55) | 45 (74) | .02 |
| History of STD, n(%) | 40 (43) | 30 (37) | NS |
| Age 16 y at first intercourse, n(%) | 58 (64) | 42 (53) | NS |
| More than 2 lifetime sexual partners, n(%) | 57 (65) | 51 (66) | NS |
| Condom use, n(%) | 34 (38) | 30 (41) | NS |
| Current tobacco use, n(%) | 44 (48) | 35 (47) | NS |
| Education, high school degree or higher, n(%) | 62 (70) | 52 (68) | NS |
Includes 17 patients who refused participation.
Includes 4 patients who refused participation.
NS indicates not significant.
Of the women initially receiving care in the urgent care clinic, 197 eligible women were included in the intention-to-treat analysis. There were 111 women assigned to the intervention group; a Pap test was performed on 94 of them, for a receipt rate of 84.7%. Of the 86 women assigned to the usual care group, only 25 women (29%) returned for a subsequent Pap test. Thus, there was a statistically significant difference in the rate of receipt of Pap tests between the 2 groups (P < .01).
In the usual care group a woman's compliance with scheduling and attending an appointment for a Pap test was greatly influenced by her pregnancy status. Of the 82 women who were actually referred, 24 (29%) were pregnant. Sixty-three percent of these pregnant women attended an appointment for a Pap test, compared with only 17% of the nonpregnant women (P < .01). When the comparison was limited to nonpregnant women, the rate of Pap test receipt differed even more dramatically between the intervention and usual care groups (100% vs 17%; P < .01). Multivariate analysis for this outcome was not completed owing to substantial missing data on the covariates.
In the intervention group, our ability to obtain follow-up of women with abnormal Pap smears was less than optimal. Twenty-one women in this group had an abnormal Pap smear (22.3%). Of these, only 5 (23.8%) complied with their gynecology clinic follow-up. Again, there was a trend for pregnancy status to predict who would actually present for follow-up. Although the numbers were small, 2 (67%) of 3 pregnant women presented for follow-up, compared with only 3 (17%) of 18 women who were not pregnant (P = .13). When compared with women who had self-referred and kept their appointments for annual examinations in the gynecology clinic, women in the intervention group with abnormal Pap smears had much lower rates of follow-up (23.8% vs 60.0%; P = .11).
There was no difference in the quality of Pap smears obtained from the intervention group as compared with those obtained from the comparison group who attended the gynecology clinic. Of the Pap tests performed in the urgent care clinic, 63 (67%) of 84 were adequate, as compared with 36 (72%) of 50 done in the gynecology clinic (P = .54). In addition, Pap smear abnormality rates did not differ between smears obtained in the urgent care clinic and in the gynecology clinic (rate of abnormal Pap smears, 22.3% vs 20%; P = .75).
DISCUSSION
Our results demonstrate that follow-up for abnormal Pap smears from women examined in the urgent care clinic is less effective than that for women who self-refer and keep their routine gynecology clinic appointments. However, our results are encouraging in that they demonstrate that cervical cancer screening rates can be improved in a public hospital urgent care clinic by performing Pap tests at the time of a pelvic examination for a patient's acute complaints, rather than relying on the referral process. This method increased receipt of Pap tests by over 44%. This is especially significant because 20% of women seen in our urgent care clinic reported not having had a Pap test in the last 3 years. Indeed, women who lack primary care and cite the emergency department or urgent care clinic as their regular place of care are the least likely to receive preventive care services.18,19
We also demonstrated that the Pap smear specimens obtained from our urgent care clinic were equal in quality to those from the gynecology clinic. Despite concerns that vaginal bleeding and cervical infection would obscure Pap smear results, this was not found to be the case. The bias against performing Pap tests in the presence of possible infection or bleeding may cause health care providers to miss valuable opportunities to perform screening because of unfounded concerns regarding smear quality.
A number of caveats in the interpretation of this study deserve mention. First, the number of refusals to participate was greater in the intervention group (15.3%) than in the usual care group (4.7%). Because women were notified of their group assignment only after consent, there is no discernible explanation for this difference other than chance. Second, for those women who consented to participate, there were some differences between the intervention and usual care groups. The usual care group more frequently reported that they were up-to-date in their Pap test screening and that their last Pap smear was normal. Whether these small differences would somehow account for a lower acceptance of scheduling an appointment for a Pap test in the usual care group, thus biasing the results, is unclear. As Pap test receipt was reported in terms of a true intention-to-treat analysis, this inclusion of women who refused participation made it impossible for us to correct the Pap test receipt rates for these observed differences between the intervention and usual care groups.
In addition, it is difficult to generalize our results to other institutions whose patient demographics may differ substantially. However, perhaps the greatest limitation was in screening only women already receiving a pelvic examination. Although this is logical owing to patient and provider acceptability, the majority of women present to the clinic with other complaints. Thus, a large number of women were not offered screening. An emergency department study group who attempted to screen all women who presented regardless of their need for a pelvic examination found they would not reach the majority of eligible women and had difficulty following those with abnormal Pap smear. However, they did detect a high rate of cervical cancer. The National Health Interview Survey data showed that older women were most likely to be inadequately screened, with 16.6% never having had a Pap smear.5 An approach that attempted to screen all presenting women would most likely have a greater impact because it would include these higher-risk women.
Having a regular source of health care is clearly the best predictor for receiving health care maintenance and adequate treatment for common medical problems such as hypertension.20,21 A study evaluating regular source of care and receipt of preventive services found a linear trend in increasing breast and cervical cancer screening rates from those having no usual source of care, to those having a usual source, and to those having a regular clinician at that usual source of care location. That study concluded that increased emphasis on continuity of care may help to bridge the gap in access to cancer prevention services for minority women.22
Our intervention was effective in improving screening, but inadequate follow-up still presented a major barrier to optimal cervical cancer prevention. Previous studies have shown that approximately one third of indigent patients with abnormal Pap smears will not return for colposcopy, despite attempts to increase compliance.20 However, we made no attempt to document whether patients initially referred for a Pap test, or subsequently contacted for follow-up of an abnormal Pap smear, obtained care outside our institution. This was unlikely to be a major factor, as the follow-up rate in both groups was influenced predominantly by pregnancy status. Pregnant women, given their presumptive eligibility for Medicaid, are covered for care at numerous institutions. However, most pregnant women in our study chose to obtain further care at our hospital. If this pattern of behavior were extended to the nonpregnant women in our study, the majority of whom had no insurance, then women of this group who felt it necessary to obtain follow-up care would choose to do so at our institution.
In our study, the patient was given the responsibility to schedule follow-up because we were not able to schedule patient appointments during all hours of operation. However, it has been shown that the most important factor associated with compliance with follow-up referral is scheduling appointments while the patient is still in the walk-in unit.23 Although this could have improved follow-up in the usual care group, the less than optimal rate of follow-up in those women documented to have an abnormal Pap smear would remain.
In the few studies evaluating follow-up for women with abnormal Pap smears, rates varied from a low of 45% among women for whom referral for follow-up was not for a suspected malignancy,24 to 92% for a group of African-American women carefully tracked following an abnormal diagnosis.25 Rates sometimes, but not always, appear to vary by race, socioeconomic status, location of residence, age, availability of payment mechanism, severity of preliminary diagnosis, access to follow-up care, and screening location.24–26 In our study the most significant predictor of follow-up was pregnancy status.
Ideally primary care should be the cornerstone of medical practice, but the reality is that with barriers such as appointment availability and transportation, many patients do not choose to access health care in this mode.27,28 Therefore, urgent care clinics and emergency departments at public hospitals assume an important role in the health care system by virtue of their unique accessibility.29,30 The results of our study support the idea that we should augment preventive services for patients who tend to access their care through urgent care clinic settings. Cancer screening programs in urgent care clinics, such as the Pap test screening we performed, should substantially increase the receipt of these important preventive services by a group of patients who often have unmet health needs and are at risk of experiencing worse health outcomes. However, difficulty with patient follow-up limits the full benefit of these programs. Further study of how to improve compliance with follow-up is necessary in order to realize the full benefit of screening in this manner.
Acknowledgments
Funding for this research was provided by the Division of General Internal Medicine, University of Colorado Health Sciences Center.
REFERENCES
- 1.Centers for Disease Control. Chronic disease reports: deaths from cervical cancer—United States, 1984–1986. Morb Mortal Wkly Rep. 1989;38:650–2. [PubMed] [Google Scholar]
- 2.Brinton LA, Fraumeni Jf., Jr Epidemiology of uterine cervical cancer. J Chronic Dis. 1986;39:1051–65. doi: 10.1016/0021-9681(86)90139-6. [DOI] [PubMed] [Google Scholar]
- 3. Greenwald P, Sondik EJ, eds. Cancer Control Objectives for the Nation: 1985–2000. National Cancer Institute Monograph 2. Washington, DC: Government Printing Office; 1986. NIH publication 86-2880.
- 4.Muir C, Waterhouse J, Powell J, Whelan S. Cancer Incidence in Five Continents. Vol. 88. Lyon, France: IARC; 1987. p. 5. eds. [Google Scholar]
- 5.Martin LM, Calle EE, Wingo PA, Heath CW. Comparison of mammography and Pap test use from the 1987 and 1992 National Health Interview Survey: are we closing the gaps? Am J Prev Med. 1996;12:82–90. [PubMed] [Google Scholar]
- 6.McGinnis JM, Lee PR. Healthy people 2000 at mid-decade. JAMA. 1995;273:1123–9. [PubMed] [Google Scholar]
- 7.Parkin DM, Day NE. Evaluating and planning screening programs. In: Parkin DM, Wagner G, Muir C, editors. The Role of the Registry in Cancer Control. Vol. 66. Lyon, France: IARC; 1985. p. 155. [Google Scholar]
- 8.Parker SL, Tang T, Bolden S, Wingo PA. Cancer statistics, 1997. CA. 1997;47:5–27. doi: 10.3322/canjclin.47.1.5. [DOI] [PubMed] [Google Scholar]
- 9.Kosary CL, Ries LAG, Miller BA, Hankey BF, Harras P, Edwards BK. SEER Cancer Statistics Review, 1973–1992: Tables and Graphs. Bethesda, Md: National Cancer Institute; 1995. eds NIH publication 95-2789. [Google Scholar]
- 10.Makuc DM, Freid VM, Kleinman JC. National trends in the use of preventive health care by women. Am J Public Health. 1989;79:21–6. doi: 10.2105/ajph.79.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Center of Health Statistics. Healthy People 2000. Review, 1993. Hyattsville, Md: Public Health Service; 1994. [Google Scholar]
- 12.Department of Health Us. Healthy People 2000: National Health Promotion Disease Prevention Objectives. Washington, DC: US Government Printing Office; 1990. DHHS Publication 91-50212. and Human Services and Institute of Medicine. [Google Scholar]
- 13.Marcus AC, Crance LA, Kaplan CP, et al. Screening for cervical cancer in emergency centers and sexually transmitted disease clinics. Obstet Gynecol. 1990;75:454–5. [PubMed] [Google Scholar]
- 14.Kamb ML. Cervical cancer screening of women attending sexually transmitted disease clinics. Clin Infect Dis. 1995;20(suppl 1):S98–S103. doi: 10.1093/clinids/20.supplement_1.s98. [DOI] [PubMed] [Google Scholar]
- 15.Hogness CG, Englestad LP, Linck LM, et al. Cervical cancer screening in an urban emergency department. Ann Emerg Med. 1992;21:933–9. doi: 10.1016/s0196-0644(05)82931-2. [DOI] [PubMed] [Google Scholar]
- 16.Cunningham PJ, Kemper P. Ability to obtain medical care for the uninsured. JAMA. 1998;280:921–7. doi: 10.1001/jama.280.10.921. [DOI] [PubMed] [Google Scholar]
- 17.Goldfrank LR. Emergency medicine. JAMA. 1995;273:1673–4. [PubMed] [Google Scholar]
- 18.Mandelblatt J, Freeman H, Winczewski D, et al. Implementation of a breast and cervical cancer screening program in a public health emergency department. Ann Emerg Med. 1996;28:493–8. doi: 10.1016/s0196-0644(96)70111-7. [DOI] [PubMed] [Google Scholar]
- 19.The Medicaid Access Group. Access of medicaid recipients to outpatient care. N Engl J Med. 1994;330:1426–30. doi: 10.1056/NEJM199405193302007. [DOI] [PubMed] [Google Scholar]
- 20.Bindman AB, Grumbach K, Osmond D, Vranizan K, Stewart AL. Primary care and receipt of preventive services. J Gen Intern Med. 1996;11:269–76. doi: 10.1007/BF02598266. [DOI] [PubMed] [Google Scholar]
- 21.Shea S, Misra D, Erlich MH, Field S, Francis CK. Predisposing factors for severe uncontrolled hypertension in an inner city minority population. N Engl J Med. 1996;334:635–41. doi: 10.1056/NEJM199209103271107. [DOI] [PubMed] [Google Scholar]
- 22.Walter SD, Clarke EA, Hatcher J, Stitt LW. A comparison of physician and patient reports of Pap smear histories. J Clin Epidemiol. 1988;41:401–10. doi: 10.1016/0895-4356(88)90148-5. [DOI] [PubMed] [Google Scholar]
- 23.Pinkster J, Phillips RS, Davis RB, Iezzon LI. Use of follow-up services by patients referred from a walk-in unit: how can patient compliance be improved? Am J Med Qual. 1995;10:81–7. doi: 10.1177/0885713X9501000204. [DOI] [PubMed] [Google Scholar]
- 24.Burger RA, Monk BJ, Van Nostrand KM, Greep A, Anton-Culver H, Manetta A. Single-visit program for cervical cancer prevention in a high-risk population. Obstet Gynecol. 1995;86:491–8. doi: 10.1016/0029-7844(95)00204-5. [DOI] [PubMed] [Google Scholar]
- 25.Lacey L, Whitfield J, DeWhite W, et al. Referral adherence in an inner city breast and cervical cancer screening program. Cancer. 1993;72:950–5. doi: 10.1002/1097-0142(19930801)72:3<950::aid-cncr2820720347>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 26.Mandelblatt J, Traxler M, Lakin P, et al. for the Harlem Study Team Breast and cervical cancer screening of poor elderly, black women: Clinical results and implications. Am J Prev Med. 1993;9:133–8. [PubMed] [Google Scholar]
- 27.O'malley AS, Mandelblatt J, Gold K, Cagney KA. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157:1462–70. [PubMed] [Google Scholar]
- 28.Rask KJ, Williams MV, Parker RM, McNagny SE. Obstacles predicting lack of a regular provider and delays in seeking care for patients at an urban public hospital. JAMA. 1994;271:1931–33. [PubMed] [Google Scholar]
- 29.Malone RE. Whither the almshouse? Overutilization of the role of the emergency department. J Health Polit Policy Law. 1998;23:795–832. doi: 10.1215/03616878-23-5-795. [DOI] [PubMed] [Google Scholar]
- 30.Krakau F, Hassler E. Provision for clinic patients in the emergency department produce more nonemergency visits. Am J Emerg Med. 1999;17:18–20. doi: 10.1016/s0735-6757(99)90006-2. [DOI] [PubMed] [Google Scholar]